Abstract
Corticosteroids are potent anti-inflammatory and anti-allergic agents used in the treatment of various inflammatory diseases, including allergic disease. They are frequently considered the therapy-of-choice for many skin diseases. However, allergic reactions caused by corticosteroids have been reported. Among these, delayed reactions to topical steroids are more common, whereas immediate reactions to systemic steroids are rare. Herein, we report the case of a 32-year-old woman with triamcinolone-induced immediate hypersensitivity reaction, in which the patient had a positive prick test result with triamcinolone. She has had atopic dermatitis (AD) for three years. She had used systemic steroid, cyclosporine, and antihistamine with topical steroids for AD. In clinic, approximately 10 minutes after intralesional injection of triamcinolone, she complained of erythematous patches with slight elevation and itching on the face, trunk, and both hands. After intravenous injection of dexamethasone, her symptoms got worse. After treatment with epinephrine, all symptoms resolved within two hours. We performed an open test and skin prick test. She had a positive result only from the prick test with triamcinolone; all other steroids showed negative results from the open tests. Dermatologists should be aware of the possibility of anaphylaxis or other allergic hypersensitivity in response to corticosteroids.
Keywords: Steroid, Hypersensitivity, Skin Prick Test, Open Test
INTRODUCTION
Corticosteroids have immunosuppressive, anti-proliferative, anti-inflammatory, and anti-allergic effects, and are used in the management of numerous conditions, including malignancy, transplantation, autoimmune, and allergic disease.1,2 Corticosteroids have a wide range of adverse effects, but considering the frequent use of corticosteroids, hypersensitivity reactions are rare.3 It may be paradoxical that corticosteroids, potent anti-inflammatory agents and immunomodulators used in the treatment of allergic manifestations, can produce immediate or delayed allergic hypersensitivity reactions.1 Among these, delayed reactions to topical steroids are more common (0.5%–5%), whereas immediate reactions to systemic steroids are rare (0.1%–0.3%).3,4 Herein, we report the case of a 32-year-old, female patient with atopic dermatitis (AD) exhibiting a triamcinolone-induced immediate hypersensitivity reaction.
CASE DESCRIPTION
A 32-year-old woman presented to the dermatology department for treatment for AD one year ago (in January 2015). She had had AD for three years. Measurement of serum food-specific immunoglobulin E levels (MAST) was negative and total immunoglobulin E (IgE) level was normal. She had no history of food or drug allergy, no suggestive family history, and no other systemic diseases. She typically used oral antihistamine and intermittent oral corticosteroid (methylprednisolone) and cyclosporine with topical steroids for the AD.
She was given intermittent intramuscular injections with antihistamine and dexamethasone, and intralesional injections with triamcinolone. During previous intermittent treatment with methylprednisolone tablets (4 mg Methylon; Albogen Korea, Seoul, Korea), dexamethasone injection 5 mg/mL (Dexa-S; Ilsung Pharmaceuticals, Seoul, Korea), and triamcinolone acetonide injection 2.5 mg/mL (TRIAM®; Shin Poong Pharmaceuticals, Seoul, Korea), there had been no adverse reaction. We used triamcinolone solution, made of only triamcinolone and normal saline, which the concentration is 2.5 mg/mL. In her case, no other agents, including lidocaine, were inserted.
In clinic (in December 2015), approximately 10 minutes after intralesional injection of triamcinolone on her dorsum of both hands, she complained of erythematous patches with slight elevation and itching on the face, trunk, and both hands (Fig. 1). Totally, 0.7 mL of triamcinolone solution, which the concentration was 2.5 mg/mL, was injected divided into two severe sites of her hands. Intravenous injection of dexamethasone was done 5 minutes after her symptoms occurred. Even after intravenous injection of dexamethasone, her symptoms got worse. After treatment with epinephrine, all symptoms resolved within two hours.
Fig. 1.

Clinical images of the 32-year-old patient with atopic disease. Well-demarcated erythematous wheals on the (A) face, (B) both hands, and (C, D) trunk, 30 and 20 minutes after intralesional triamcinolone injection and intramuscular dexamethasone injection, respectively.
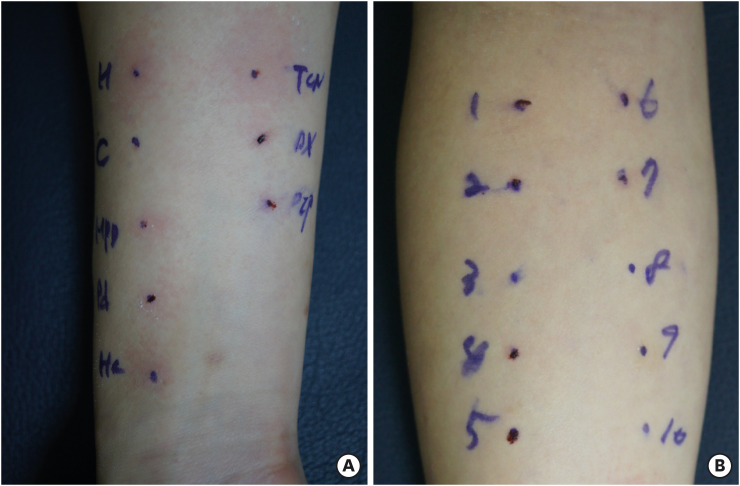
To confirm the causal relationship between the symptoms and corticosteroid, four weeks after the hypersensitivity reaction, we performed an open test and skin prick test (SPT). We performed these tests for hydrocortisone, mometasone furoate, prednicarbate, desonide, desoxymethasone, prednisolone valerate, triamcinolone acetonide, clobetasol propionate, methylprednisolone, and prednisolone. A positive response was only observed after the prick test with triamcinolone, 20 × 23 mm at 15 minutes and at 45 minutes, maximum reaction was observed, 20 × 25 mm; no other steroid prick tests gave positive results, including dexamethasone (Fig. 2). In SPT with steroid, it is known that the reactions might be a maximum after around 30 minutes and the reactions reduce with time after that, at around 60 minutes. We observe time-course results every 15 minutes.1,5 All steroids showed negative open test results after 30 minutes (Fig. 2). For definitive diagnosis, an intravenous or oral provocation test was planned. She refused permission for these tests because she had become pregnant four months after the skin tests.
Fig. 2.
Skin prick tests (SPTs) and topical provocation test were done and we observed the results every 15 minutes. (A) SPTs showed positive reaction to triamcinolone, but not to other steroids, after 30 minutes. (B) All steroids showed negative results for an open test after 30 minutes.
1 = hydrocortisone, 2 = mometasone furoate, 3 = prednicarbate, 4 = desonide, 5 = desoxymethasone, 6 = prednisolone valerate, 7 = triamcinolone acetonide, 8 = clobetasol propionate, 9 = methylprednisolone, 10 = prednisolone, TCN = triamcinolone acetonide, DX = dexamethasone, PIP = piprinhydrinate.
Finally, we diagnosed the patient with immediate hypersensitivity reactions induced by triamcinolone and recommended avoidance of this drug. During the next six months, she did not experience any recurrence.
DISCUSSION
It is possible to identify hypersensitivity reactions to corticosteroids with skin prick and intradermal tests, but many cases will only be diagnosed correctly by intravenous or oral challenge tests.3 There are several invasive/non-invasive epicutaneous tests to diagnose immediate skin responses.2,6 We chose the invasive SPT and non-invasive open test for diagnosis.
In our patient, the SPT with triamcinolone showed positive. The SPT was done to evaluate type I IgE-mediated allergy by confirming allergen-specific IgE.5 It was done on the volar aspect of the forearm, using commercially available topical steroids.5,7 A 1-mm single-peak lancet with shoulder was used. This test breaks the skin barrier and changes skin permeability so haptens of high molecular weight can penetrate and induce hypersensitivity reactions. Histamine was assumed to be released from mast cells in response to exposure to an eliciting substance. Meanwhile, the open test showed a negative result. An open test is usually done to diagnose contact urticaria.8 Contact urticaria is classified as non-immunological/irritant or immunological/allergic, according to the underlying mechanism, which is incompletely understood.9 It has been assumed non-immunologic urticaria is the commonest form, which might be mediated by prostaglandins. Release of prostaglandin D2 without concomitant histamine release has been demonstrated.9 However, immunological contact urticaria is due to immediate-type hypersensitivity, medicated primarily by histamine and confirmed by simple investigations such as skin prick testing or measurement of specific IgE.9 The mechanism following skin challenge involves allergen penetration through the epidermis, then binding to IgE on mast cells, causing degranulation and release of histamine and other vasoactive substances.9 When a hypersensitivity reaction simply occurs by epicutaneous absorption, which means haptens might be small enough to penetrate the skin, the open test can be helpful. However, in a case of haptens related to systemic absorption, the agents producing the hypersensitivity reaction have comparatively higher molecular weight. An open test could also be helpful, but may be negative unless the substance is applied against broken or eczematous skin.9 Skin permeability may be increased because of AD with abnormal skin barrier function.10 The open test can be negative when the skin has healed.10 Our case might also show a negative result for the open test after the skin has healed. Due to these differences between mechanisms, our patient might show different results in the SPT and open test. According to the patient's history and the results of tests, there appears to be a high probability of systemic hypersensitivity reaction due to intravenous or intralesional injections, not contact urticaria. Further testing (intravenous or oral provocation) is needed for a definitive diagnosis.
Due to anti-inflammatory properties of corticosteroids, the clinical signs of allergy may be masked and the results of skin tests are difficult to interpret. It often mimics the symptoms of the underlying disease so that it often likely remains undiagnosed.
Early studies did not identify significant host factors associated with corticosteroid allergy, but more recent work has found several risk factors, which include renal transplant or history of asthmatic disease (especially for those who are aspirin sensitive),11,12,13 hypersensitivity to nonsteroidal drugs,4 a history of nephritis, and high percutaneous absorption caused by sweat, cutaneous infections, and AD. However, this impression might be related more to the frequent use of corticosteroids, than to the disease itself.4,11 The factors associated with individual characteristics include the immune system's ability to identify the antigen, the enzymatic ranges and activity producing metabolites that may exert a different sensitizing capacity, as well as genetic predisposition.1,14 It has also become clear the allergen that triggers an immune reaction may be a by-product of corticosteroid metabolism, not by corticosteroid itself.1,15
Our patient was at high risk of corticosteroid allergy, having AD with frequent corticosteroid use and repeated intralesional triamcinolone injections.16 High percutaneous absorption caused by AD could be another risk factor.
Our patient's symptoms got worse even after the dexamethasone injection. She had no cross-reaction to other steroids, which was confirmed by results from open test and SPT. So, we thought the dose of dexamethasone was not enough for relieving her symptoms and the improvement of symptoms might take some time. The courses of cutaneous reactions due to systemic corticosteroid have been variable in previous cases, from rapid improvement to requiring several months.17
Although the Coopman classification (the cross-reactivity spectrum of topical corticosteroids based on molecular structure) does not apply to systemic corticosteroids and is not necessarily pertinent in immediate hypersensitivity reactions,18 it could provide guidance to doctors for how to choose a replacement corticosteroid. However, cases of cross-reactivity have shown that hypersensitivity to a corticosteroid in one group does not rule out the safe use of other corticosteroids in the same group.19 Therefore, such loose guidance cannot replace a systematic evaluation of the individual patient's sensitivity and tolerability.3 Graded challenge is recommended to ensure tolerance of the alternative preparation4; our patient refused the challenge by intravenous or oral provocation test, so we could not determine a replacement corticosteroid. Finally, we recommended that she avoid steroids, and we have not prescribed any steroids for her to date.
We report a unique case of triamcinolone-induced hypersensitivity with a positive SPT result. Immediate hypersensitivity reactions are possibly underdiagnosed, particularly because corticosteroids are common therapy for hypersensitivity disorders. Physicians should be aware of the possibility of anaphylaxis or other allergic hypersensitivity in response to corticosteroids. It should be taken into consideration in the differential diagnosis of patients receiving corticosteroid.
Footnotes
Funding: This study was supported by grants of the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT & Future Planning (NRF-2017R1A2B4006252), Korea Healthcare Technology R & D project, funded by Ministry of Health & Welfare, Republic of Korea (HI17C0597), and the Hallym University Research Fund (HURF-2017-35, HURF-2017-52).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Park CW.
- Data curation: Son JH, Park SY.
- Investigation: Cho YS, Son JH.
- Writing - original draft: Son JH, Chung BY.
- Writing - review & editing: Son JH, Park SY, Cho YS, Chung BY, Kim HO, Park CW.
References
- 1.Baeck M, Marot L, Nicolas JF, Pilette C, Tennstedt D, Goossens A. Allergic hypersensitivity to topical and systemic corticosteroids: a review. Allergy. 2009;64(7):978–994. doi: 10.1111/j.1398-9995.2009.02038.x. [DOI] [PubMed] [Google Scholar]
- 2.Rietschel RL. Contact dermatitis and diagnostic techniques. Allergy Proc. 1989;10(6):403–411. doi: 10.2500/108854189778935782. [DOI] [PubMed] [Google Scholar]
- 3.Knarborg M, Bendstrup E, Hilberg O. Increasing awareness of corticosteroid hypersensitivity reactions is important. Respirol Case Rep. 2013;1(2):43–45. doi: 10.1002/rcr2.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel A, Bahna SL. Immediate hypersensitivity reactions to corticosteroids. Ann Allergy Asthma Immunol. 2015;115(3):178–182.e3. doi: 10.1016/j.anai.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Ahn YH, Koh YI, Kim JH, Ban GY, Lee YK, Hong GN, et al. The potential utility of iodinated contrast media (ICM) skin testing in patients with ICM hypersensitivity. J Korean Med Sci. 2015;30(3):245–251. doi: 10.3346/jkms.2015.30.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hannuksela M. Epicutaneous testing. Allergy. 1979;34(1):5–10. doi: 10.1111/j.1398-9995.1979.tb01994.x. [DOI] [PubMed] [Google Scholar]
- 7.Kekki OM, Turjanmaa K, Isolauri E. Differences in skin-prick and patch-test reactivity are related to the heterogeneity of atopic eczema in infants. Allergy. 1997;52(7):755–759. doi: 10.1111/j.1398-9995.1997.tb01234.x. [DOI] [PubMed] [Google Scholar]
- 8.Lahti A. In: Contact Urticaria Syndrome. Amins S, Lahti A, Maibach HI, editors. Boca Raton, FL: CRC Press; 1997. Nonimmunologic contact urticaria. Chapter 3. [Google Scholar]
- 9.Wakelin SH. Contact urticaria. Clin Exp Dermatol. 2001;26(2):132–136. doi: 10.1046/j.1365-2230.2001.00780.x. [DOI] [PubMed] [Google Scholar]
- 10.Helaskoski E, Kuuliala O, Aalto-Korte K. Occupational contact urticaria caused by cyclic acid anhydrides. Contact Dermat. 2009;60(4):214–221. doi: 10.1111/j.1600-0536.2009.01526.x. [DOI] [PubMed] [Google Scholar]
- 11.Vatti RR, Ali F, Teuber S, Chang C, Gershwin ME. Hypersensitivity reactions to corticosteroids. Clin Rev Allergy Immunol. 2014;47(1):26–37. doi: 10.1007/s12016-013-8365-z. [DOI] [PubMed] [Google Scholar]
- 12.Dajani BM, Sliman NA, Shubair KS, Hamzeh YS. Bronchospasm caused by intravenous hydrocortisone sodium succinate (Solu-Cortef) in aspirin-sensitive asthmatics. J Allergy Clin Immunol. 1981;68(3):201–204. doi: 10.1016/0091-6749(81)90184-6. [DOI] [PubMed] [Google Scholar]
- 13.Partridge MR, Gibson GJ. Adverse bronchial reactions to intravenous hydrocortisone in two aspirin-sensitive asthmatic patients. BMJ. 1978;1(6126):1521–1522. doi: 10.1136/bmj.1.6126.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkinson SM, Morrey K, Hollowood K, Heagerty AH, English JS. HLA-A, -B and -DR antigens in hydrocortisone contact hypersensitivity. Contact Dermat. 1993;28(5):295–297. doi: 10.1111/j.1600-0536.1993.tb03439.x. [DOI] [PubMed] [Google Scholar]
- 15.Bundgaard H. The possible implication of steroid-glyoxal degradation products in allergic reactions to corticosteroids. Arch Pharm Chem Sci Ed. 1980;8:83–90. [Google Scholar]
- 16.Kim JE, Kim HJ, Lew BL, Lee KH, Hong SP, Jang YH, et al. Consensus guidelines for the treatment of atopic dermatitis in Korea (part II): systemic treatment. Ann Dermatol. 2015;27(5):578–592. doi: 10.5021/ad.2015.27.5.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitmore SE. Delayed systemic allergic reactions to corticosteroids. Contact Dermat. 1995;32(4):193–198. doi: 10.1111/j.1600-0536.1995.tb00668.x. [DOI] [PubMed] [Google Scholar]
- 18.Coopman S, Degreef H, Dooms-Goossens A. Identification of cross-reaction patterns in allergic contact dermatitis from topical corticosteroids. Br J Dermatol. 1989;121(1):27–34. doi: 10.1111/j.1365-2133.1989.tb01396.x. [DOI] [PubMed] [Google Scholar]
- 19.Aranda A, Mayorga C, Ariza A, Doña I, Blanca-Lopez N, Canto G, et al. IgE-mediated hypersensitivity reactions to methylprednisolone. Allergy. 2010;65(11):1376–1380. doi: 10.1111/j.1398-9995.2010.02386.x. [DOI] [PubMed] [Google Scholar]