Abstract
Background: We hypothesized that polymicrobial posttraumatic osteomyelitis (PTO) may be associated with worse outcomes when compared to monomicrobial PTO. We therefore attempted to show the outcomes and predisposing factors associated with polymicrobial PTO.
Methods: A single-center case-control study was carried out from 2007 to 2012. The outcome variables analyzed were: the need for additional surgical and antibiotic treatments, rates of amputation, and mortality associated with the infection. Univariate and multivariable analyses using multiple logistic regression were performed to identify risk factors associated with polymicrobial PTO, and p < 0.05 was considered significant.
Results: Among the 193 patients identified, polymicrobial PTO was diagnosed in 37.8%, and was significantly associated with supplementary surgical debridement (56.1% vs. 31%; p < 0.01), a higher consumption of antibiotics, and more amputations (6.5% vs 1.3%; p < 0.01). Factors associated with polymicrobial PTO in the multivariable analysis were older age (odds ratio [OR] = 1.02, 95% confidence interval [CI] = 1.01 to 1.03, p = 0.04), working in agriculture (OR = 2.86, 95% CI = 1.05 to 7.79, p = 0.04), open fracture Gustilo type III (OR = 2.38, 95% CI = 1.02 to 5.56, p = 0.04), need for blood transfusion (OR = 2.15, 95% CI = 1.07 to 4.32, p = 0.03), and need for supplementary debridement (OR = 2.58, 95% CI = 1.29 to 5.16, p = 0.01).
Conclusions: PTO is polymicrobial in more than one-third of patients, associated with extra surgical and clinical treatment, and worse outcomes including higher rates of amputation.
Keywords: Chronic osteomyelitis, polymicrobial infection, monomicrobial infection, posttraumatic osteomyelitis, risk factors, Staphylococcus aureus
Introduction
Posttraumatic osteomyelitis (PTO) is an increasingly prevalent public health problem, especially in low- and middle-income countries, in which the injury rates associated with falls, self-harm, interpersonal violence and road traffic accident are increasing 1. Even with systemic antimicrobial therapy being applied soon after the trauma, open fracture-associated infections can be expected to occur just after the surgical procedures or later on, depending upon the complexity and severity of the soft tissue and bone damage 2-4. Unfortunately, there have been few studies addressing the epidemiology and clinical outcomes of soft tissue and bone infections following non-fatal injuries, even though the average cost of combined medical and surgical treatment for PTO is estimated to be US$15,000 in developing countries 5. In a single center retrospective study, the development of surgical site infection (SSI) soon after management of the trauma was the only risk factor in a multivariate analysis associated with 30-days hospital readmission 6.
Inoculation of microorganisms into the bone may happen soon after the trauma, from adjacent soft tissue contamination or pre- and intra-operatively during bone surgeries 7-9. In a previous study, we found a rate of 20.8% of polymicrobial osteosynthesis-associated infections in a young Brazilian population following trauma (mainly motorcycle accidents) and orthopedic surgery 2-3. Similarly, in a Chinese retrospective study of difficult-to-treat chronic osteomyelitis, 66.5% of infections were secondary to trauma, of which polymicrobial PTO accounted for at least 20% of cases 3. Additionally, a population-based historical cohort study carried out in United States identified a rate of 35% of polymicrobial contiguous osteomyelitis resulting from trauma or surgery 10.
Predisposing factors for PTO have been classically sub-divided in patient-related (increased age; comorbidities including diabetes mellitus, obesity, poor nutrition, malignancy; and smoking), injury-related (grade of trauma energy, severity of soft tissue damage, wound contamination, and complexity of fracture), and surgery-related (time period from trauma to surgery, duration of surgery, need for blood transfusion, and empirical antibiotic therapy) 11-13. Nevertheless, microorganism-related factors, including the presence of multiple pathogens on the affected bone and soft tissue, must also be addressed by clinical studies. To the best of our knowledge, the role of polymicrobial etiology as an independent factor for poor outcomes after PTO, as opposed to monomicrobial infection, has not been investigated 2-3, 10-11. Therefore, we hypothesized that polymicrobial PTO may be associated with worse outcomes when compared to monomicrobial PTO, including the need for additional orthopedic surgeries and increased use of broad-spectrum antibiotics, more amputations and higher mortality rates. We also aimed to identify the risk factors for polymicrobial deep infections following PTO. The identification of risk factors may help to reduce the frequency of polymicrobial infections and the associated costs.
Patients and Methods
Study Design
We performed a single-center observational case-control study of data collected from August 2007 through August 2012, with subjects diagnosed with osteomyelitis following orthopedic surgery for closed and open fractures, performed at the Orthopedics and Traumatology Unit of Hospital de Base, a tertiary public teaching hospital in São José do Rio Preto, São Paulo, Brazil. The study included patients older than 12 years old and with at least 2 years of follow-up after the surgical procedures. The standard of care for orthopedic assistance for Gustilo II and III open fractures is currently external fixation for bone stabilization followed by internal fixation with plates and screws or intramedullary nails. Regarding antibiotic prophylaxis and therapy, cefazolin has been indicated for closed fractures and Gustilo I and II open fractures for 24 hours. Clindamycin and gentamicin are prescribed empirically for Gustilo III open fractures for as long as seven days. The following criteria were used to exclude subjects from the study: having had orthopedic surgical procedures performed primarily in an institution other than ours, unavailability of medical records, follow-up shorter than 12 months, amputation after trauma and a previous history PTO. The local Institutional Review Board (Fundação Faculdade Regional de Medicina S J Rio Preto) approved the study, under the protocol number: 234.654.
Identification of post-traumatic osteomyelitis (PTO)
We defined PTO according to the criteria of the Center for Disease Control and Prevention (CDC)/National Healthcare Safety Network (NHSN) guidelines, in which at least one of the following criteria was present: any growth of organism in bone and soft tissue culture; evidence of osteomyelitis on gross anatomic or histopathologic exam; and at least two of the following signs and symptoms of inflammation: fever (>38.0°C), swelling, pain, redness, heat, drainage and delayed wound closure with exposed bone or osteosynthesis; plus at least one of the following: a) organisms identified from blood by culture or a non-culture based microbiologic testing method in a patient with imaging test evidence suggestive of infection, which if equivocal is supported by clinical correlation; b) imaging test evidence suggestive of infection, which if equivocal is supported by clinical correlation 14. Acute bone infection was defined when diagnosis was performed up to 30 days after surgery for the fracture 15. A diagnosis of polymicrobial PTO was made when either the bone or surrounding soft tissue cultures yielded at least two different microorganisms. Low- virulence microorganisms such as coagulase-negative staphylococci were considered pathogens when the same organism was phenotypically identified (e.g., S. epidermidis) in at least two different tissue samples, and when at least one additional criterion for PTO was also fulfilled. For the purpose of study analysis, we included only the first diagnosis of osteomyelitis and subsequent episodes were further excluded.
Outcome and potential risk factors for polymicrobial PTO
A worse outcome was defined as the need for additional orthopedic surgeries, increased use of broad-spectrum antibiotics, amputations and higher mortality rates. Medical, intra-operative, and microbiological records were reviewed for potential risk factors associated with polymicrobial PTO. We searched for demographic variables (age, gender, occupational status, educational level), comorbidities (smoking, alcoholism, and diabetes), and the patient's pre-surgery clinical condition according to the American Society of Anesthesiologists (ASA) classification. Injury-associated variables assessed were: time elapsed from admission to the first dose of antibiotic and to surgery, anatomical site of fracture, the mechanism of trauma - whether a low-energy (fall height < 1 m) or high-energy injury (car, motorcycle, bicycle accident or fall from a height above 1 m), and Gustilo open fracture classification. Surgery-related factors analyzed were type of surgery procedure (open reduction and internal fixation or two-stage temporary external fixator), duration of surgery, and the need for blood transfusion. Furthermore, we also assessed the need to perform supplementary surgical debridement for infected wounds.
Specimen collection and microbiology
In the surgical ward, at least three tissue samples from infected bone and soft tissues were collected during surgical debridement, and then processed for microbiology and histopathology. Tissue was homogenized in 3 ml of brain-heart infusion (BHI) broth for 1 min and inoculated onto aerobic sheep blood agar, chocolate agar, anaerobic blood agar and into thioglycolate broth (BD Diagnostic Systems, Sparks, MD). The time limit for processing samples was 6 hours. Aerobic and anaerobic plates were incubated aerobically at 35° to 37°C in 5 to 7% CO2 for 7 days, and anaerobically at 37°C for 14 days, respectively. Additionally, 0.5 ml of tissue homogenate was inoculated in thioglycolate broth, incubated for 14 days, and the thioglycolate broth was sub-cultured on blood agar plates when cloudy. Colonies of microorganisms growing on the plates were identified, and their susceptibility to antibiotics was tested according to standard microbiologic techniques.
Statistical analysis
For statistical analysis, the overall sample and the groups assigned as monomicrobial and polymicrobial PTO were described as frequencies and percentages for qualitative variables, and median and standard deviation (SD) for quantitative variables. The association between qualitative variables was analyzed using the chi-square test and Fisher's exact test, as indicated, while the Mann-Whitney or t-test were used for quantitative variables. The risk estimates were calculated on the variables associated with risk factors for PTO and reported as an odds ratio with respect to a 95% confidence interval (CI). We used the multiple logistic regression model to investigate independent risk factors for polymicrobial PTO by selecting the variables with significance levels lower than 0.20 on bivariate analysis (p < 0.20); only variables with p-values lower than 0.5 (p < 0.05) remained in the final model. We used the Epi-Info® Version 3.22 software for the data tabulation and SPSS version 20.0 (SPSS, Chicago, IL, USA) for statistical analysis.
Results
Study population and aspects of trauma
During the study period of 2007-2012, we included 205 patients with PTO, of whom 12 (5.9%) subjects were excluded due to a previous history of PTO (7), or to incomplete medical information availability (5). Therefore, one-hundred ninety-three patients with PTO were analyzed, 110 (57%) presenting monomicrobial PTO and 73 (37.8%) polymicrobial PTO. Negative- culture osteomyelitis was diagnosed in 10 (5.2%) patients and they were included in the clinical and epidemiological description. In general, the PTO rate during the study period was 2.5%. Mean age was 50 (± 16-88) years, 68.9% were male, and 34.7% had poor educational status (schooling level <8 years). 30.5% of the patients reported smoking, 22.8% worked in construction and 30.5% in household activities. High-energy trauma due to road traffic accidents occurred in the majority (57.0%) of our study population, and consequently, femur (30.5%) and tibia (29.0%) fractures were the most frequently diagnosed. 9.3% of patients undergoing surgery for fracture stabilization were assigned as having an ASA grade higher than II, and 34.2% received blood transfusion during surgery. Gustilo type II and III open fractures were diagnosed in 11.9% and 18.6% of patients, respectively. The clinical characteristics and comorbidities are shown in Table 1.
Table 1.
Demographic and injury characteristics of 193 patients presenting posttraumatic osteomyelitis (PTOa).
| Demographic data | N=193 (%) |
| Age (mean [range]) (years) | 50 (16-88) |
| Male sex (no. [%]) | 133 (68.9) |
| Schooling level ≤8 years | 67 (34.7) |
| Comorbidities (no. [%]) | |
| Alcohol abuse | 35 (18.1) |
| Smoking | 59 (30.5) |
| Intraoperative hyperglycemia | 58 (30.0) |
| Occupation (no. [%]) | |
| Agriculture worker | 26 (13.5) |
| Driver (car, motorcycle, truck) | 24 (12.5) |
| Construction / Machine Operation | 44 (22.8) |
| Business | 40 (20.7) |
| Household activities | 59 (30.5) |
| Types of injury (no. [%]) | |
| Car crash | 110 (57.0) |
| Fall from height (< 1m) | 57 (29.5) |
| Football related injury | 3 (1.5) |
| Stairs fall | 13 (7.0) |
| Horse fall | 5 (2.6) |
| Firearm injury | 2 (1.0) |
| Penetrating injury by a wooden foreign body | 3 (1.5) |
| High-energy injury | 133 (68.9) |
| Gustilo & Anderson Classification for open fractures | 73 (37.8) |
| Type-I (no. [%]) | 14 (19.2) |
| Type-II (no. [%]) | 23 (31.5) |
| Type-III (no. [%]) | 36 (49.3) |
| Closed fracture | 120 (62.1) |
| More of one surgical debridement | 77 (39.9) |
| Polytrauma | 46 (23.8) |
| American Society of Anesthesiologists score (no. [%]) | |
| ASAb I - II (1 or 2) | 166 (90.7) |
| ASAb III - IV (>2) | 17 (9.3) |
| Intraoperative blood transfusion | 66 (34.2) |
| Duration of surgery (media [range]) (hours) | 2.61 (1-8) |
| Infected Fracture Location (no. [%]) | |
| Upper limbs | 44 (22.8) |
| Lower limbs | 154 (79.2) |
| Collarbone | 7 (3.6) |
| Humerus | 12 (6.2) |
| Radium | 13 (6.7) |
| Ulna | 16 (8.2) |
| Hands | 3 (1.5) |
| Femur | 59 (30.5) |
| Knee | 9 (4.6) |
| Tibia | 56 (29) |
| Fibula | 11 (5.7) |
| Feet | 19 (9.8) |
a PTO-posttraumatic polymicrobial osteomyelitis; b ASA-American Society of Anesthesiologists score.
Outcome and potential risk factors for polymicrobial PTO
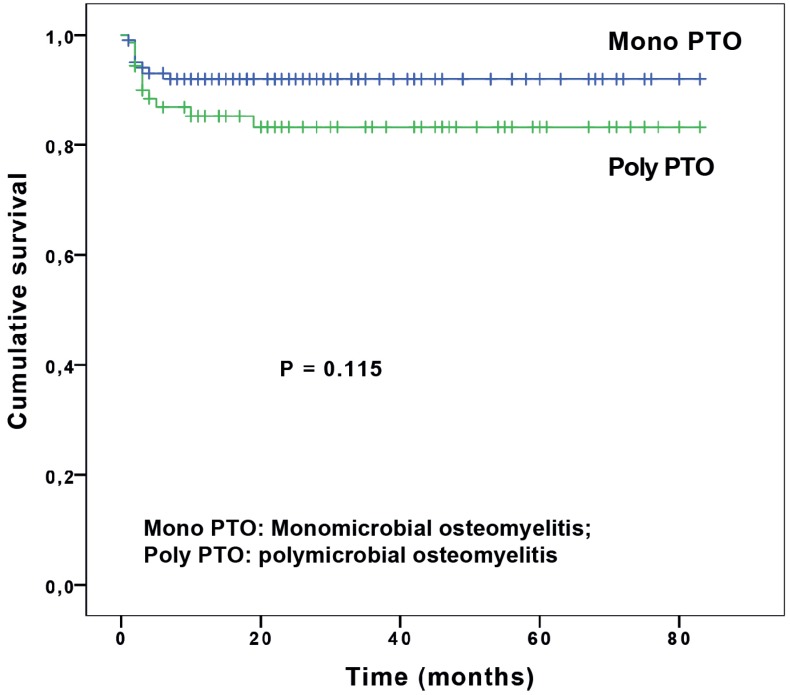
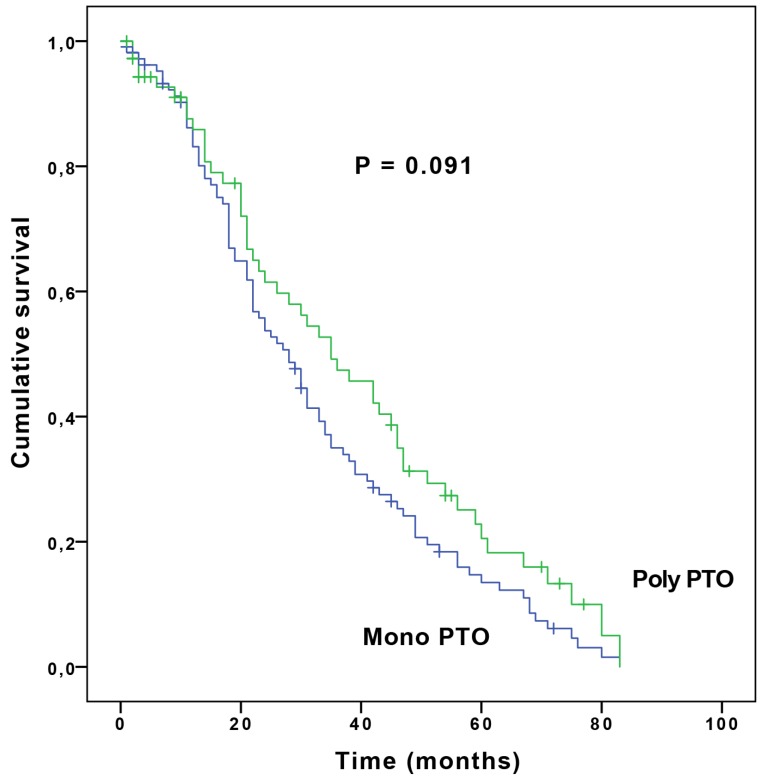
Compared to monomicrobial osteomyelitis, polymicrobial PTO was significantly associated with supplementary surgical debridement (31.0% vs. 56.1; p < 0.001) and a higher consumption of broad-spectrum antibiotics including quinolones (39.7% vs. 24.3; p = 0.029), cephalosporins (21.9% vs. 4.9; p < 0.001), carbapenems (31.5% vs. 3.9; p < 0.001) and glycopeptides (49.3% vs. 27.2; p = 0.003). Polymicrobial PTO and amputations were statistically significant (6.5% vs 1.3%; p < 0.001) with an OR = 11.5 (95 % CI = 1.3-96.1). The 2-year cumulative survival rate of polymicrobial and monomicrobial PTO was 84.5% and 91.8%, respectively (p = 0.115) (Figure 1). Another Kaplan-Meier curve was plotted showing no difference of upper and lower limb survival rates between monomicrobial and polymicrobial PTO (p = 0.091) (Figure 2). There were eight deaths from polymicrobial, and one from monomicrobial PTO.
Fig 1.
Kaplan-Meier estimate of cumulative survival rate showing no difference between two-year survival rate between monomicrobial osteomyelitis (Mono PTO) and polymicrobial osteomyelitis (Poly PTO).
Fig 2.
Kaplan-Meier curve showing no difference of upper and lower limb survival between monomicrobial and polymicrobial PTO (p = 0.091). Mono PTO: Monomicrobial osteomyelitis; Poly PTO: polymicrobial osteomyelitis
The patient, injury, and surgical factors that were investigated for possible association with an increased risk for polymicrobial PTO in the univariate analysis are described in Table 2. Variables showing statistical significance and with clinical importance in the univariate analysis have been added to the multivariate model (Table 3). Predisposing factors associated with polymicrobial PTO in the multivariable analysis were older age (OR = 1.02, 95% CI = 1.01 - 1.03, p = 0.040), open fracture, Gustilo type III (OR = 2.38, 95% CI = 1.02 - 5.56, p = 0.044), a need for intraoperative blood transfusion (OR = 2.15, 95% CI = 1.07 - 4.32, p = 0.031), working in agriculture (OR = 2.86, 95% CI = 1.05 - 7.79, p = 0.040) and the need for supplementary surgical debridement (OR = 2.58, 95% CI = 1.29 - 5.16, p = 0.007).
Table 2.
Univariate analysis of risk factors associated with polymicrobial PTO (Polya) and monomicrobial PTO (Monob) following trauma, among 183c patients.
| Characteristics | Monoa Patients No. (%) (N = 110) |
Polyb Patients No. (%) (N = 73) |
P valued |
|---|---|---|---|
| Demographic data | |||
| Age (median [range]) (yr) | 40.5 (11 - 87) | 50 (16 - 88) | 0.017 |
| Male sex (no. [%]) | 76 (69.0) | 53 (72.6) | 0.610 |
| Schooling level ≥8 years (no. [%]) | 47 (42.7) | 20 (27.3) | 0.035 |
| Agriculture worker (no. [%]) | 9 (8.2) | 16 (22.0) | 0.008 |
| Comorbidities (no. [%]) | |||
| Smoking | 33 (30.0) | 26 (23.6) | 0.426 |
| Intraoperative hyperglycemia | 29 (26.3) | 27 (37.0) | 0.127 |
| High-energy injury (no. [%]) | 79 (71.8) | 50 (68.5) | 0.629 |
| Fall from height (no. [%]) | 29 (26.4) | 22 (30.1) | 0.577 |
| Grade-III open fracture (no. [%]) | 15 (13.6) | 21 (28.7) | 0.012 |
| Admission to surgery t >3h (no. [%]) | 103 (93.6) | 62 (85.0) | 0.053 |
| Duration of surgery (median [range]) (hr) | 2 (1-8) | 2 (1-7) | 0.738 |
| Admission to first antibiotic (hr) | 60 (54.5) | 26 (23.6) | 0.062 |
| Follow-up (range) (days) | 728 (38 - 2539) | 690 (22 - 2526) | 0.980 |
| >1 surgery debridement (no. [%]) | 34 (31.0) | 41 (56.1) | 0.001 |
| Need for blood transfusion (no. [%]) | 26 (23.6) | 38 (52.0) | <0.0001 |
| Femoral fractures (no. [%]) | 26 (23.6) | 31 (42.5) | 0.007 |
| ≥3 samples for bone culture (no. [%]) | 59 (53.6) | 51 (69.8) | 0.028 |
| ≥3 samples of soft tissue (no. [%]) | 12 (11.0) | 20 (27.4) | 0.004 |
| ASA score | |||
| ASA I - II (no. [%]) | 102 (92.7) | 64 (87.7) | 0.249 |
| ASA III - IV (no. [%]) | 8 (7.3) | 9 (12.3) |
a Poly-polymicrobial osteomyelitis; b Mono-monomicrobial osteomyelitis; cTen patients (5.2%) were excluded from this analysis since they presented negative-culture osteomyelitis; d The patient characteristics were summarized as frequencies and percentages or median values and compared using the Pearson chi-square test or Fisher's exact test, as appropriate, with nominal variables and the Mann-Whitney test or t test, as appropriate, with continuous variables (SPSS version 19.0). All tests were two sided, and P values of <0.05 were considered statistically significant.
Table 3.
Multivariate logistic regression analysis of risk predictors PTOa, among 183 patientsb.
| Variables | Monoa Patient No. (%) (N = 110) |
Polyb Patient No. (%) (N = 73) |
Odds Ratio CI (95%) |
P Valuec |
|---|---|---|---|---|
| Age (median [range]) (yr) | 40,5 (11 - 87) | 50 (16 - 88) | 1.02 (1.01 - 1.03) | 0.040 |
| Need for blood transfusion | 26 (40.6%) | 38 (59.4%) | 2.15 (1.07 - 4.32) | 0.031 |
| Gustilo Type-III open fracture | 15 (41.7%) | 21 (58.3%) | 2.38 (1.02 - 5.56) | 0.044 |
| Agriculture workers | 9 (8.2%) | 16 (22.0%) | 2.86 (1.05 - 7.79) | 0.002 |
| >1 surgery debridement (no. [%]) | 34 (31. %) | 41 (56.1%) | 2.58 (1.29 - 5.16) | 0.007 |
a Poly-polymicrobial osteomyelitis; b Mono-monomicrobial osteomyelitis; cP values of <0.05 were considered statistically significant.
Microbial identification
Microbiological diagnosis of PTO using intraoperative bone and soft tissue cultures identified bacteria in 94.8%. Cultures yielded gram-negative bacilli (GNB) and gram- positive cocci (GPC) in 51.8% and 48.2% of samples, respectively. Table 4 shows the frequencies of microorganisms isolated from bone and soft tissue cultures among patients presenting polymicrobial and monomicrobial PTO.
Table 4.
Frequency of microorganisms yielded from cultures of monomicrobial and polymicrobial PTOa patients.
| Micro-organisms | N = 110 | N = 73 |
|---|---|---|
| Monomicrobial | Polymicrobial | |
| Staphylococcus aureus | 69 (62.7) | 35 (47.9) |
| MRSAb | 22 (31.9) | 15 (42.9) |
| MSSAc | 47 (68.1) | 20 (55.1) |
| Pseudomonas aeruginosa | 8 (7.30) | 23 (31.5) |
| Acinetobacter baumannii | 2 (1.80) | 21 (28.8) |
| Enterococcus sp. | 2 (1.80) | 20 (27.4) |
| Citrobacter sp. | 7 (6.40) | 14 (19.2) |
| Klebsiella pneumoniae | 4 (3.60) | 16 (21.9) |
| CoNSd | 8 (7.30) | 11 (15.1) |
| Escherichia coli | 2 (1.80) | 12 (16.4) |
| Proteus sp. | 2 (1.80) | 12 (16.4) |
| Candida tropicalis | 0 (0.00) | 2 (2.7) |
Categorical Variables are expressed as number and proportions.
aPTO-posttraumatic osteomyelitis; bMRSA-Methicillin-resistant Staphylococcus aureus; cMSSA-Methicillin-sensitive Staphylococcus aureus; dCoNS-Coagulase-negative Staphylococci.
Discussion
We performed a 5-year case-control study of trauma care in a Brazilian tertiary hospital, in which PTO was diagnosed in only 2.5% of patients admitted with fractures, but polymicrobial osteomyelitis accounted for 37.8%. Interestingly, polymicrobial PTO was statistically associated with additional orthopedic surgeries for bone and soft tissues, debridement and increased use of broad-spectrum antibiotics - including combination therapy. In addition, higher rates of amputations were statistically associated with polymicrobial infection with an OR of 11.5 (95 % CI = 1.3-96.1). It may be surprising, but data investigating the outcomes and risk factors associated with polymicrobial PTO are scarce, although a few previous case-series associated polymicrobial osteomyelitis among patients with uncontrolled chronic diseases (diabetes mellitus), worse outcomes and treatment failure 10, 16. We speculate the association between devitalized bone and soft tissue following high-energy open or closed fractures with local contamination by a higher inoculum of multiple species of pathogenic bacteria may increase local and systemic inflammatory response and influence the higher rates of amputations. However, in our case-series the outcomes for polymicrobial and monomicrobial PTO in respect of 2-year cumulative survival rate were similar. Even though PTO is frequently associated with higher morbidity but lower mortality, the impact of polymicrobial infection on the outcome of patients with PTO could be better studied by using a quality-of-life measurement, such as SF-36, which includes physical functioning, physical limitations, pain and patient`s general health.
Several risk factors independently associated with polymicrobial PTO were identified in the present study. Older age, agricultural workers, complex lower limb Gustilo III open fractures, intra-operative blood transfusion and the number of debridement procedures, were significantly associated with polymicrobial osteomyelitis in the multivariable analysis. Interestingly, agricultural employment was found to be a potent risk for polymicrobial PTO, showing a 2.86-fold higher risk and reaching statistical significance in the multivariable-adjusted analysis. Ali et al., have previously shown a strong association between open, agricultural upper extremities injuries and PTO (18.7%), with 37.5% having polymicrobial infection 17. Gustilo III fractures of the lower limb are life-threatening injuries, in which inoculation of microorganisms into the bone commonly happen soon after trauma from soft tissue contamination or during surgery 7-9. Recipients of blood transfusion during surgery had a 2.15-fold higher risk of polymicrobial infection. The need for allogeneic blood transfusion may reflect the severity of the injury itself, with extensive soft tissue damage and severe bleeding due to high-energy trauma. Albeit, by controlling the Gustillo classification effect on the multivariable analysis, one may also raise the hypothesis of an independent effect of blood transfusion on the polymicrobial PTO outcome. Previous investigations have shown increased risk of bacterial infection following blood transfusion, possibly associated with an immunomodulatory effect of blood transfusion 18. In a retrospective cohort study performed among patients undergoing hip fracture repair, blood transfusion was associated with a 35% and 52% greater risk of serious bacterial infection and pneumonia, respectively 19. Based on our findings, we have taken some measures to prevent polymicrobial PTO among those with severe open fractures or presenting heavily soiled wounds. This includes more thorough and radical debridement, and the use of more broad-spectrum antibiotic prophylaxis directed at gram-positive, gram-negative and anaerobic bacteria, including activity against staphylococci, Pseudomonas aeruginosa and Acinetobacter baumannii by using single-dose gentamicin and clindamycin.
The spectrum of microorganisms isolated from the bone and soft tissues samples from patients with PTO was different from that reported by other authors, in which Gram-positive cocci, especially staphylococci species are the predominant bacteria 20-21. Indeed, the microbiological findings of the present study added new information to the epidemiology of PTO, because GNB were slightly more prevalent than GPC (51.8% vs. 48.2%, respectively). Among the GNB, Pseudomonas aeruginosa (10.3%) and Acinetobacter baumannii (7.6%) were the commonest in our results. These organisms have frequently been associated with PTO, especially in chronic osteomyelitis of the tibia following high-energy injuries, such as motorcycle accidents and combat-associated fractures 20-22. In respect of this intriguing result, we speculated if previous use of broad-spectrum systemic antibiotics during a prolonged course of therapy might also have had some impact on the high frequency of GNB-PTO. Staphylococcus aureus was still the most commonly isolated pathogen in our cases (34.7%) even though, we noticed a considerably lower yield compared to other PTO series 21. Despite this, staphylococci will continue to play a major role in the pathogenesis of posttraumatic infection due to its incredible ability not only colonize skin and invade deep tissues, but also to survive intracellularly in osteoblasts and forming biofilm 23-24. Only one-third of our positive cultures yielding S. aureus were MRSA strains, which was considered a low incidence due to its high frequency within many Latin America hospitals 3, 25.
We are aware that the retrospective design of our study has potential limitations. First, the study was carried out at a single, large urban public teaching center which offers a specialized orthopedic care for the local population, located in a medium-sized city in a developing country, and the results may not be applicable to other hospitals. Another limitation was the lack of a clear definition of PTO. CDC/NHSN-guidelines do not specifically address the complexity of PTO patients presenting open fractures with soft tissue contamination, and no consensus definition is currently accepted for fracture-related infection 26. In addition, in the polymicrobial PTO group, more bone and soft tissue samples were obtained for cultures, which could have biased our results. We are aware that organisms growing on cultures resulting from soft tissue samples may not directly reflect polymicrobial osteomyelitis, but one can expect that bacterial contamination of soft tissues during open fractures may lead to high rates of bone infection. Furthermore, sonication of the retrieved implants (screws and plates) for the identification of sessile microorganisms was not performed, thus probably influencing the total number of polymicrobial PTO cases studied 2. We concluded that polymicrobial PTO occurred in more than one-third of patients, and was associated with extra surgical and clinical treatment, and worse outcomes, including higher rates of amputation. Besides, higher age, working in agriculture, Gustilo III open fractures, supplementary debridement, and blood transfusion during surgery were independently associated with polymicrobial infection. These findings may prompt clinicians to implement infection control measures, including appropriate empirical antibiotic therapy for these patients. Further studies addressing polymicrobial PTO should be encouraged to confirm our results.
Acknowledgments
We thank the Orthopedics and Traumatology Unit, Hospital de Base de São José do Rio Preto for access to the patient archives, and Patricia Fucuta for her support in the statistical analysis.
References
- 1.Zhou J, Li Y, Wang QK. et al. Status of road safety and injury burden: China. J Orthop Trauma. 2014;28(Suppl 1):S41–2. doi: 10.1097/BOT.0000000000000111. [DOI] [PubMed] [Google Scholar]
- 2.Yano MH, Klautau GB, da Siva CB. et al. Improved diagnosis of infection associated with osteosynthesis by use of sonication of fracture fixation implants. J Clin Microbiol. 2014;52(12):4176–82. doi: 10.1128/JCM.02140-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang N, Ma YF, Jiang Y. et al. Clinical Characteristics and Treatment of Extremity Chronic Osteomyelitis in Southern China. Medicine (Baltimore) 2015;94(42):e1874. doi: 10.1097/MD.0000000000001874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gosselin RA, Roberts I, Gillespie WJ. Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst Rev. 2004;(1):1–27. doi: 10.1002/14651858.CD003764.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darouiche RO. Treatment of Infections Associated with Surgical Implants. N Engl J Med. 2004;350:1422–9. doi: 10.1056/NEJMra035415. [DOI] [PubMed] [Google Scholar]
- 6.Morris DS, Rohrbach J, Sandaram LMT. et al. Early hospital readmission in the trauma population: Are the risk factors different? Injury. 2014;45(1):56–60. doi: 10.1016/j.injury.2013.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trampuz A, Zimmerli W. Diagnosis and treatment of infections associated with fracture- fixation devices. Injury. 2006;37:S59–S66. doi: 10.1016/j.injury.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Gustilo RB, Merkow RL, Templeman D. The management of open fractures. J Bone Joint Surg Am. 1990;72(2):299–304. [PubMed] [Google Scholar]
- 9.Brady RA, Leid JG, Costerton JW. et al. Osteomyelitis: Clinical Overview and Mechanisms of Infection Persistence. Clin Microbiol News. 2006;28(9):65–72. [Google Scholar]
- 10.Kremers HM, Nwojo ME, Ransom JE. et al. Trends in the Epidemiology of Osteomyelitis. J Bone Joint Surg Am. 2015;97:837–45. doi: 10.2106/JBJS.N.01350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazzarini L, Mader JT, Calhoun JH. Osteomyelitis in long bones. J Bone Joint Surg Am. 2004;86(10):2305–18. doi: 10.2106/00004623-200410000-00028. [DOI] [PubMed] [Google Scholar]
- 12.Uçkay I, Hoffmeyer P, Lew D. et al. Prevention of surgical site infections in orthopaedic surgery and bone trauma: state-of-the-art update. J Hosp Infect. 2013;84:5–12. doi: 10.1016/j.jhin.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 13.Li G, Guo F, Ou Y. et al. Epidemiology and outcomes of surgical site infections following orthopedic surgery. Am J Infect Control. 2013;41:1268–71. doi: 10.1016/j.ajic.2013.03.305. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. CDC/NHSN Surveillance Definitions for Specific Types of Infections [access on February 14, 2016] https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf.
- 15.Lipsky BA, Berendt AR. Osteomyelitis. ACP Medicine; 2010. Decker Intellectual Properties; p.1-20. Doi:10.2310/7900.1137. [Google Scholar]
- 16.Sheehy SH, Atkins BA, Bejon P. et al. The microbiology of chronic osteomyelitis: prevalence of resistance to common empirical anti-microbial regimens. J Infect. 2010;60:338–43. doi: 10.1016/j.jinf.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Ali MH, Hoekzema NA, Bakleh M. et al. The microbiology and risk of infection following open, agricultural upper extremity injuries. J Hand Surg Am. 2008;33(1):87–93. doi: 10.1016/j.jhsa.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Tartter PI. Blood transfusion and postoperative infections. Transfusion. 1989;29(5):456–9. doi: 10.1046/j.1537-2995.1989.29589284149.x. [DOI] [PubMed] [Google Scholar]
- 19.Carson JL, Altman DG, Duff A. et al. Risk of bacterial infection associated with allogeneic blood transfusion among patients undergoing hip fracture repair. Transfusion. 1999;39(7):694–700. doi: 10.1046/j.1537-2995.1999.39070694.x. [DOI] [PubMed] [Google Scholar]
- 20.Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg. 2005;13(6):417–27. doi: 10.5435/00124635-200510000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Glass GE, Barrett SP, Sanderson F. et al. The microbiological basis for a revised antibiotic regimen in high-energy tibial fractures: preventing deep infections by nosocomial organisms. J Plast Reconstr Aesthet Surg. 2011;64(3):375–80. doi: 10.1016/j.bjps.2010.05.037. [DOI] [PubMed] [Google Scholar]
- 22.Johnson EN, Burns TC, Hayda RA. et al. Infectious complications of open type III tibial fractures among combat casualties. Clin Infect Dis. 2007;45(4):409–15. doi: 10.1086/520029. [DOI] [PubMed] [Google Scholar]
- 23.Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364(9431):369–79. doi: 10.1016/S0140-6736(04)16727-5. [DOI] [PubMed] [Google Scholar]
- 24.Hudson MC, Ramp WK, Nicholson NC. et al. Internalization of Staphylococcus aureus by cultured osteoblasts. Microbial Pathogenesis. 1995;19:409–19. doi: 10.1006/mpat.1995.0075. [DOI] [PubMed] [Google Scholar]
- 25.Guzmán-Blanco M, Mejía C, Isturiz R. et al. Epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) in Latin America. Int J Antimicrob Agents. 2009;34(4):304–8. doi: 10.1016/j.ijantimicag.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Metsemakers WJ, Kortram K, Morgenstern M. et al. Definition of infection after fracture fixation: A systematic review of randomized controlled trials to evaluate current practice. Injury. 2017;20:pii. doi: 10.1016/j.injury.2017.02.010. S0020-1383(17)30081-5. [DOI] [PubMed] [Google Scholar]