Abstract
Background:
Uncontrolled hemorrhage still remains a major cause of trauma-associated mortality. The events resulting in acute traumatic coagulopathy, particularly hypofibrinogenemia, make control of bleeding difficult. It is essential to timely predict, diagnose, and manage trauma-induced coagulopathy.
Aims:
The aim of this study is to determine clinical and easily available laboratory variables that are predictive of hypofibrinogenemia in acute trauma patients.
Settings and Design:
This 2-year retrospective work examined the data of major trauma patients that were referred to Shahid Rajaee Hospital's emergency room in hemorrhagic shock condition.
Materials and Methods:
Fibrinogen level was assessed for these patients on their arrival at our facility. Along with clinical and routine paraclinical variables, we evaluated the predictive value of these variables for a fibrinogen level below 100 mg/ml.
Results:
A total of 855 cases were included (females: 16.4%; and males: 83.6%) in the study. The mean ± SD age was 36 ± 17.9 years, and the mean ± SD injury severity score was 12.2 ± 9. Motor vehicle accident was the most common cause of injury. Three factors, including arterial pH (cut off point = 7.34; area under the curve [AUC]: 0.59), base excess (cutoff point = −4.3; AUC: 0.60), and patients' gender had a significant association with the fibrinogen level under 100 mg/ml. When three factors of pH, BE, and patients' gender are being assessed simultaneously, the AUC became 0.62 (the predictive ability improved).
Conclusions:
Variables, including arterial pH, BE level, and patients' gender have predictive value for fibrinogen transfusion in trauma.
Keywords: Blood component transfusion, fibrinogen, hemorrhage, shock
INTRODUCTION
Trauma is currently a leading cause of mortality and morbidity worldwide, leading to more than 4 million deaths per year.[1,2] Uncontrolled hemorrhage is a major, but preventable cause of these trauma-related deaths. In spite of various improvements made in the care of trauma patients, uncontrolled bleeding is still responsible for about 40% of trauma-associated mortality.[3,4,5]
An important phenomenon that occurs after trauma and worsens these patients' outcome is the lethal complex of hypothermia, acidosis, and coagulopathy.[6] It is well-known that the events resulting in acute coagulopathy of trauma begin early after severe injury. This problem is already present in about 25%–30% of trauma cases at the time of their admission to the emergency room (ER).[4,7,8] Acute coagulopathy of trauma is associated with increased amount of bleeding, increased transfusion requirements, and increased mortality rate in this group of patients.[7,9]
Hypofibrinogenemia is an important component of acute traumatic coagulopathy. Previous studies have shown that fibrinolytic activity increases in trauma patients after injury, an event that results in impairment of the critical role of this plasma protein in clot formation and bleeding control.[7,10] The process of fibrinogen depletion progresses during trauma-hemorrhage.[5] Fibrinogen and factor V are two most consumed coagulation factors following injury.[1]
Timely and aggressive hemostatic therapy is known as two major measures for improving the patients' survival.[9] Considering the important role of fibrinogen depletion in the occurrence of acute traumatic coagulopathy, timely replacement of this blood product can affect trauma patients' outcome. Nevertheless, presently there are ongoing discussions about the time to start, the amount, and the ratio of blood products transfusion (particularly fibrinogen) in trauma patients.[4,5,11] In this respect, some previous works suggested the use of thromboelastography (TEG) or rotational thromboelastography (ROTEM) to assess plasma fibrinogen level and the need for its transfusion. However, these laboratory facilities are not available widely, and their use will result in significant costs compared with other simple and available clinical or laboratory tests.[5,12]
Keeping in mind the above-mentioned facts, in this study, we examined the feasibility of the use of different clinical and para-clinical variables in predicting the need for fibrinogen replacement therapy in acute trauma patients.
MATERIALS AND METHODS
This retrospective work was performed at Shahid Rajaee (Emtiaz) Trauma Hospital, a high turn-over center that is affiliated with Shiraz University of Medical Sciences (SUMS), Shiraz city, Fars province, Iran. The Institutional Review Board of SUMS approved this research. This work was in accordance with the Helsinki Declaration.
Data were extracted from the Shahid Rajaee Hospital's database. Medical records of those patients that were referred to the aforementioned hospital's ER from January 2014 to December 2015 were assessed (a total of 2 years). The study included cases of major trauma who were referred to the hospital's ER in hemorrhagic shock state. The study cases were older than 16 years. Those patients' whose medical records were incomplete were excluded from the study.
According to the Shahid Rajaee Hospital's local algorithms, plasma fibrinogen level is being checked (using Clauss test) for all the referred cases that have a hemorrhagic shock at the time of their ER admission. If the patients' fibrinogen level is <100 mg/ml, he/she will receive 1–4 g of fibrinogen concentrate (Hemocomplettan®, CSL Behring). The dosage will be determined according to the patients' clinical conditions and the severity of blood fibrinogen depletion. Subsequently, the fibrinogen level will be checked every 3–6 h, until it becomes normal. At the same time, patients' shock state is being evaluated and managed using the guides of Trauma Associated Severe Hemorrhage score. In our center, we transfuse fresh frozen plasma (FFP) and packed red blood cells with a ratio of 1:2 to reduce the possibility of adverse consequences associated with the use of FFP.
We evaluated the predictive value of various factors for a fibrinogen level below than 100 mg/ml. The examined clinical and paraclinical variables were as follows: systolic (SBP) and diastolic blood pressure levels, pulse rate (PR), respiratory rate, patients' age and gender, hemoglobin and hematocrit levels, patients' injury severity score (ISS) and Glasgow Coma scale (GCS) at the time of ER admission, prothrombin time, international normalized ratio, and partial thromboplastin time levels, and arterial blood gas examination (PO2, PCO2, pH, HCO3, and base excess [BE]). We defined massive bleeding as hemorrhage that resulted in the hemodynamic instability (PR >100 beats/min or SBP <90 mmHg).
Data analysis
Data analysis was performed using SPSS Analytical (version 16.0; SPSS Inc., Chicago, IL., USA) and MedCalc softwares. At first, we used t-test and Chi-square test for finding significant variables (P < 0.1). Then, we used logistic regression model using the significant variables to determine those ones that have an association with a fibrinogen level fewer than 100 mg/ml. P <0.05 was considered as statistically significant.
RESULTS
Overall, a total number of 855 cases were included in the study. 140 (16.4%) of the patients were female and 715 (83.6%) of them were male. The mean ± SD age was 36 ± 17.9 (ranging from 7 to 94 years). The mean ± SD ISS value was 12.2 ± 9 (12.85 (standard deviation (SD): 8.18) for men and 12.10 (SD: 9.10) for women), without any significant difference (P = 0.3). Motor vehicle accident was the most prevalent mechanism of trauma.
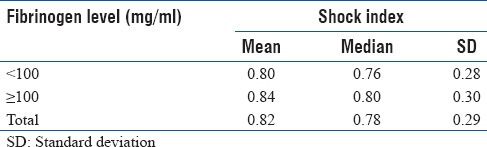
Fibrinogen level was evaluated in male and female patients [Table 1]. After the univariate analysis of the studied factors (assessment of the association of each one with fibrinogen level separately), those variables that had a P < 0.1 were entered in the logistic regression model. According to the Forward method, from among different assessed clinical and para-clinical variables, three factors, including pH (P = 0.046; cutoff point: 7.34), BE (P = 0.001; cutoff point: −4.3), and patients' gender (P = 0.002) had a significant association with the fibrinogen level under 100 mg/ml [Table 2]. The study results showed that the chance of having a fibrinogen level <100 mg/ml is 0.4 times higher in men as compared to women. We also evaluated patients' shock index [Table 3]. The mean value of ISS in the patients with fibrinogen level <100 mg/dL was 11.76 (SD: 8.67) and that of the cases with fibrinogen level ≥100 mg/dL was 11.76 (SD: 8.67), without any significant difference (P = 0.1).
Table 1.
Analysis of fibrinogen level in male and female patients
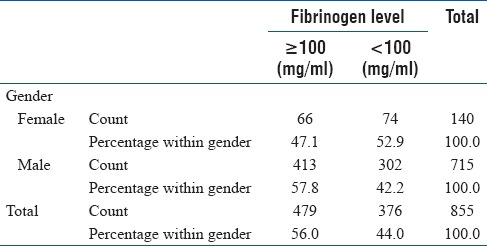
Table 2.
Results of logistic regression
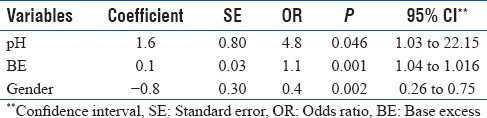
Table 3.
Patient's shock index
For the two factors of pH and BE, the area under the curve (AUC) were 0.59 and 0.60, respectively. However, when three factors of pH, BE, and patients' sex is being assessed together each other, the AUC became 0.62 [Figure 1], which shows that the use of three factors simultaneously will improve the predictive ability for a plasma fibrinogen level below than 100 mg/ml. According to our work, other examined variables, like GCS, had no predictive value for a decreased level of fibrinogen in acute trauma patients.
Figure 1.
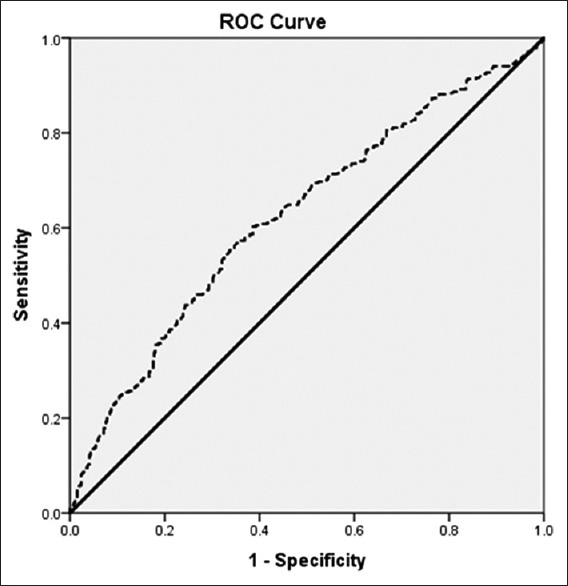
The receiver operating characteristic curve of three examined variables, including pH, base excess, and patients' gender
The overall accuracy of this classification was 63.4% for a fibrinogen level <100 mg/ml. Of note, for model assessment, the Hosmer– Lemeshow goodness of fit index has been used and showed that our model fits well (P = 0.305).
DISCUSSION
This study examined the value of various clinical and simple available para-clinical tests for predicting the need to fibrinogen transfusion in acute major trauma patients. According to our results, three variables, including pH, BE (as an indicator of shock state), and patients' gender had this ability, especially when they are being used simultaneously.
Fibrinogen is a plasma protein that has a critical role in clot formation and hemostasis. The plasma concentration level of this clotting factor ranges from 1.5 to 4.0 gr/L; however, it may be higher in some conditions, like pregnancy, or may show decreased levels, as following major traumas.[1,7,10]
After traumatic injuries, coagulopathy occurs for various reasons. Among these causes are loss of blood clotting factors (to variable degrees) following major hemorrhage, massive tissue factor release from the injury site (an event that will lead to activation of blood coagulation cascades and consumption of clotting factors, particular fibrinogen), and an increased fibrinolytic activity (hyperfibrinolysis).[7,10,13] In addition, the use of plasma volume expanders (which are essential for restoration of patients' hemodynamics), especially when bleeding continues simultaneously, will aggravate the reduction in platelet and plasma clotting factors (including fibrinogen) concentrations, a matter which has a prognostic value for this group of patients.[10] The occurrence of the triad of hypothermia, acidosis, and hypovolemia (and the consequent tissue hypoperfusion) is the other reason that deteriorates of the coagulation process.[13] It has been shown that a decreased level of fibrinogen following trauma is associated with poor patients' outcomes. This is while it is suggested that with increasing total amounts of fibrinogen administered, the outcomes tend to improve.[5] Therefore, the prediction of hypofibrinogenemia possibility, its early diagnosis, and its proper management in trauma.
In the management of acute traumatic coagulopathy, goal-directed transfusions are necessary. One main reason is to minimize the probability of various adverse effects associated with the administration of blood products, such as transfusion-related acute lung injury, and immunosuppression.[14] In addition, this approach will reduce the number of blood products used.
To achieve this goal and reduce the need to allogenic blood products transfusions (and their associated adverse effects), some previous studies recommend ROTEM®-guided/TEM-guided hemostatic therapy using fibrinogen concentrate and prothrombin complex concentrate (PCC).[12,15,16] However, as explained above, facilities such as ROTEM and TEG, in spite of their ability in providing a real-time view of global clot formation and dissolution, are not widely available worldwide, as in countries like ours, Iran.[17] In addition, these tests are expensive,[18] a matter that will be more problematic in high turn-over and busy trauma centers, like that of us.
Considering the above-mentioned facts, to move a step forward, we tried to find clinical/paraclinical variables that have a predictive value for the need to fibrinogen transfusion. This matter was the subject of some previous studies. Previous work by Rourke et al. showed that a decreased fibrinogen level at the time of hospital admission was independently associated with patients' ISS (on admission), the presence of shock state (on admission), and higher volumes of pre-hospital fluid therapy. According to them, cryoprecipitate administration improved patients' survival. The other important finding of this aforementioned study was the predictive value of fibrinogen level for patients' mortality, as they reported fibrinogen level as an independent predictor of mortality at 24 h and 28 days postinjury.[5] Schlimp concluded that hemoglobin and BE levels (on admission) can be used as two helpful variables for identification major trauma patients who are at risk of acquired hypofibrinogenemia.[19] According to them, early ISS calculation and addition of it to the two aforementioned variables can improve their predictive ability for a decreased plasma fibrinogen level in major trauma cases.[19]
The current study had some limitations: This was retrospective. For this reason, we were unable to precisely evaluate other factors, including patients' comorbidities or their medication use, which may affect the results of our examined tests. We did not compare our results to that of a standard control method, like ROTEM/TEG due to the lack of our access to these aforementioned facilities.
CONCLUSION
Three variables of arterial pH and BE levels (at the time of hospital admission), and patients' gender (more chance in the male group) can be used for prediction of trauma cases' need to fibrinogen transfusion. However, due to our study's limitations, we recommend future multicenter studies be conducted to examine this issue.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Professor S. Gando for his contribution in editing the manuscript.
REFERENCES
- 1.Cap A, Hunt B. Acute traumatic coagulopathy. Curr Opin Crit Care. 2014;20:638–45. doi: 10.1097/MCC.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 2.Paydar S, Ahmadi A, Dalfardi B, Shakibafard A, Abbasi H, Bolandparvaz S, et al. Clinical and economic effects of selective radiological evaluation of high-energy trauma patients: A prospective experience of a level 1 busy trauma centre. Emerg Med J. 2015;32:535–8. doi: 10.1136/emermed-2014-204083. [DOI] [PubMed] [Google Scholar]
- 3.Stinger HK, Spinella PC, Perkins JG, Grathwohl KW, Salinas J, Martini WZ, et al. The ratio of fibrinogen to red cells transfused affects survival in casualties receiving massive transfusions at an army combat support hospital. J Trauma. 2008;64:S79–85. doi: 10.1097/TA.0b013e318160a57b. [DOI] [PubMed] [Google Scholar]
- 4.Schöchl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert G, et al. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care. 2010;14:R55. doi: 10.1186/cc8948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rourke C, Curry N, Khan S, Taylor R, Raza I, Davenport R, et al. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. J Thromb Haemost. 2012;10:1342–51. doi: 10.1111/j.1538-7836.2012.04752.x. [DOI] [PubMed] [Google Scholar]
- 6.Martini WZ. Coagulopathy by hypothermia and acidosis: Mechanisms of thrombin generation and fibrinogen availability. J Trauma. 2009;67:202–8. doi: 10.1097/TA.0b013e3181a602a7. [DOI] [PubMed] [Google Scholar]
- 7.Brohi K, Cohen MJ, Davenport RA. Acute coagulopathy of trauma: Mechanism, identification and effect. Curr Opin Crit Care. 2007;13:680–5. doi: 10.1097/MCC.0b013e3282f1e78f. [DOI] [PubMed] [Google Scholar]
- 8.Brohi K, Cohen MJ, Ganter MT, Schultz MJ, Levi M, Mackersie RC, et al. Acute coagulopathy of trauma: Hypoperfusion induces systemic anticoagulation and hyperfibrinolysis. J Trauma. 2008;64:1211–7. doi: 10.1097/TA.0b013e318169cd3c. [DOI] [PubMed] [Google Scholar]
- 9.Schöchl H, Schlimp CJ, Maegele M. Tranexamic acid, fibrinogen concentrate, and prothrombin complex concentrate: Data to support prehospital use? Shock. 2014;41(Suppl 1):44–6. doi: 10.1097/SHK.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 10.Levy JH, Szlam F, Tanaka KA, Sniecienski RM. Fibrinogen and hemostasis: A primary hemostatic target for the management of acquired bleeding. Anesth Analg. 2012;114:261–74. doi: 10.1213/ANE.0b013e31822e1853. [DOI] [PubMed] [Google Scholar]
- 11.Shaz BH, Dente CJ, Nicholas J, MacLeod JB, Young AN, Easley K, et al. Increased number of coagulation products in relationship to red blood cell products transfused improves mortality in trauma patients. Transfusion. 2010;50:493–500. doi: 10.1111/j.1537-2995.2009.02414.x. [DOI] [PubMed] [Google Scholar]
- 12.Hunt H, Stanworth S, Curry N, Woolley T, Cooper C, Ukoumunne O, et al. Thromboelastography (TEG) and rotational thromboelastometry (ROTEM) for trauma induced coagulopathy in adult trauma patients with bleeding. Cochrane Database Syst Rev. 2015;2:CD010438. doi: 10.1002/14651858.CD010438.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schöchl H, Frietsch T, Pavelka M, Jámbor C. Hyperfibrinolysis after major trauma: Differential diagnosis of lysis patterns and prognostic value of thrombelastometry. J Trauma. 2009;67:125–31. doi: 10.1097/TA.0b013e31818b2483. [DOI] [PubMed] [Google Scholar]
- 14.Schöchl H, Forster L, Woidke R, Solomon C, Voelckel W. Use of rotation thromboelastometry (ROTEM) to achieve successful treatment of polytrauma with fibrinogen concentrate and prothrombin complex concentrate. Anaesthesia. 2010;65:199–203. doi: 10.1111/j.1365-2044.2009.06188.x. [DOI] [PubMed] [Google Scholar]
- 15.Schöchl H, Nienaber U, Maegele M, Hochleitner G, Primavesi F, Steitz B, et al. Transfusion in trauma: Thromboelastometry-guided coagulation factor concentrate-based therapy versus standard fresh frozen plasma-based therapy. Crit Care. 2011;15:R83. doi: 10.1186/cc10078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grassetto A, De Nardin M, Ganzerla B, Geremia M, Saggioro D, Serafini E, et al. ROTEM®-guided coagulation factor concentrate therapy in trauma: 2-year experience in Venice, Italy. Crit Care. 2012;16:428. doi: 10.1186/cc11322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whiting D, DiNardo JA. TEG and ROTEM: Technology and clinical applications. Am J Hematol. 2014;89:228–32. doi: 10.1002/ajh.23599. [DOI] [PubMed] [Google Scholar]
- 18.Davenport R, Brohi K. Fibrinogen depletion in trauma: Early, easy to estimate and central to trauma-induced coagulopathy. Crit Care. 2013;17:190. doi: 10.1186/cc13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlimp CJ, Voelckel W, Inaba K, Maegele M, Ponschab M, Schöchl H, et al. Estimation of plasma fibrinogen levels based on hemoglobin, base excess and Injury Severity score upon emergency room admission. Crit Care. 2013;17:R137. doi: 10.1186/cc12816. [DOI] [PMC free article] [PubMed] [Google Scholar]


