Abstract
Aims:
The aim of the study was to evaluate the effect of 10% sodium ascorbate (SA),10% hesperidin, 1% riboflavin 5-phosphate, collagen cross-linkers, on the pushout bond strength of the fiber resin postluted to the radicular dentin.
Materials and Methods:
Twenty-eight, single-rooted extracted human teeth were collected. The cleaning shaping and obturation was done followed postspace preparation which was etched with 37% phosphoric acid for 15 s and then rinsed with normal saline. The specimens were divided into four groups and postspaces were irrigated, respectively with. (i) Group 1: Normal saline for 4 min, (ii) Group 2: 10% SA for 4 min, (iii) Group 3: 10% hesperidin for 4 min, and (iv) Group 4: 1% riboflavin 5 phosphate (RFV) for 4 min. The pushout bond strength of fiber postluted to root dentin, of all the above groups, was compared. Posts were luted using Rely X Arc luting cement. Each root was horizontally sectioned to obtain 2 mm thick, 28 dentinal disks, per group. The pushout bond strength test was carried out using Universal Testing Machine. The scores were statistically analyzed using Student's Unpaired “t” and ANOVA test.
Results:
Comparison of different collagen crosslinker showed that the highest pushout bond strength value was recorded with 10% hesperidin, followed by 1% RFV and 10% SA.
Conclusion:
All collagen cross-linkers so used, increased the bond strength. The highest push-out bond strength was achieved with 10% hesperidin.
Keywords: Hesperidin, push-out bond strength, riboflavin 5 phosphate, sodium ascorbate
INTRODUCTION
Mutilated endodontically treated teeth are often restored with posts and cores. Adhesive resins have become widely accepted for the cementation of posts in root canals.[1] But failure of the bond is the most common cause of failure of resin luted fiber posts.
Organic component of dentin also undergoes degradation by the use of NaOCl (most common root canal irrigant).[2]
Recent studies have suggested that the eventual bond failure may be due to the release of matrix metalloproteinases (MMPs) from dentin because of the use of acids during adhesive procedures. MMPs causes hybrid layer disintegration by collagen fibril degradation.[3]
One of the techniques to improve bond strengths involves the use of natural crosslinkers which have shown to increase dentin stiffness by increasing the number of intramolecular collagen crosslinks.[4]
Some antioxidants which are extracted from the plants are known to inhibit MMPs. A number of citrus flavonoids, such as grapefruit seed extract and hesperidin (HPN) when used on root caries, showed and rendered made collagen matrix more stable by crosslinking effects on demineralized dentin.[5]
Several recent studies have shown that the application of sodium hypochlorite results in reduced bond strength which can be increased by the use of sodium ascorbate (SA) and Vitamin C.[6]
Riboflavin is another naturally occurring Vitamin (B2) which produces free oxygen radicals that lead to crosslinking collagen through a photooxidation pathway.[7]
Since the mechanical strength of dentin is dependable on the collagen fibrillar network, so the aim and objective of this study were to evaluate the effect of 10% SA,10% hesperidin, 1% riboflavin 5-phosphate, collagen crosslinkers, on the push-out bond strength of the fiber resin postcemented to radicular dentin and their comparison.
MATERIALS AND METHODS
Twenty-eight single rooted, noncarious, freshly extracted human teeth, indicated for extraction, were collected. The root portions were obtained by sectioning at cement-enamel junction.
The cleaning and shaping were done initially with k files till #20 followed by canal preparation with protapers till F2, within between usage of 3% sodium hypochlorite and normal saline as an irrigant. The prepared canals were obturated using guttapercha and AH Plus sealer™. After 24 h, roots were prepared for postinsertion.
The canal space was prepared by corresponding drill for Hi-Rem posts size #1, (made available by the manufacturer). Postspace was etched with 37% phosphoric acid for 15 s, and then, rinsed with normal saline. The specimens were then divided into four groups with 7 teeth in each group, and the postspaces were irrigated, respectively, with:
Group 1: Control group.(n = 7 teeth; 28 dentinal discs), normal saline
Group 2: (n = 7 teeth; 28 dentinal discs), 8 ml 10% SA for 4 min
Group 3: (n = 7 teeth; 28 dentinal discs), 8 ml of 10% hesperidin for 4 min
Group 4: (n = 7 teeth; 28 dentinal discs), 8 ml of 1% riboflavin 5 phosphate (RFV) for 4 min followed by blue light activation for 20 s for each sample.
All the samples were finally irrigated with normal saline. The postspace was dried with paper points. Fifth generation bonding agent was used as an adhesive agent which was applied to the canal wall with a microbrush and cured for 20 s. Hi-Rem Fiber posts of size #1 were used. They were treated with silane coupling agent and luted into the postspace with Rely X Arc resin luting cement. The root was horizontally sectioned into 2 mm thick slices with a diamond blade. 28 dentinal disks were obtained for each group. Each disk was embedded in cold cure acrylic resin in such a way that the top and the bottom surface were left uncovered. After measuring the thickness of each sample, the pushout bond strength test was carried out on each sample using Universal Testing Machine, at a crosshead speed of 1 mm/min.
Pushout bond strength was calculated using formula:
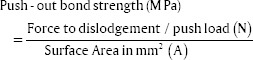
Where, A = 2 Π rh, r = radius of perforated cross-section, h = height of perforation
RESULTS
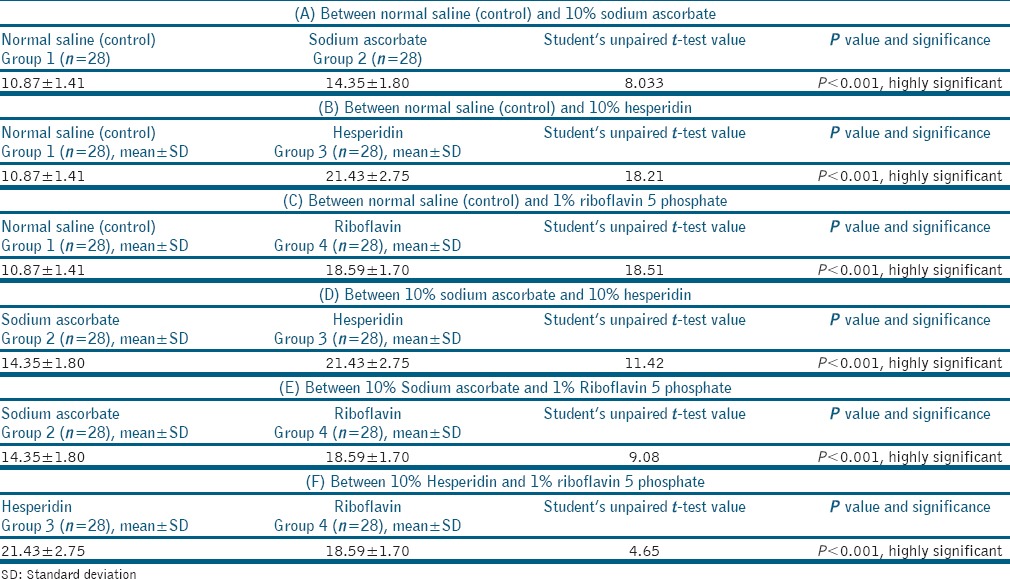
In the present study, statistical analysis was done by comparison of mean and standard deviation values of push out bond strength (MPa) among normal saline (control), 10% SA, 10% hesperidin, and 1% RFV group [Table 1]. Comparison of groups was done by applying Student's Unpaired “t” test [Table 2]. The result of the study revealed that the mean pushout bond strength values for the study groups were as follows:
Table 1.
Comparison of mean and standard deviation values of push out bond strength (MPa) among normal saline (control), 10% sodium ascorbate, 10% hesperidin and 1% riboflavin 5 phosphate group
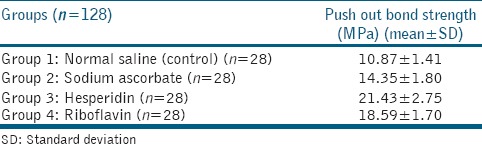
Table 2.
Student's unpaired t-test value-comparisons
Group 1: (normal Saline) 10.87 ± 1.41 MPa,
Group 2: (10% SA) 14.35 ± 1.80 MPa,
Group 3: (10% HPN) 21.43 ± 2.75 MPa,
Group 4: (1% RFV) 18.59 ± 1.70 MPa.
Which is statistically significant with P value<0.001. There was a significant increase in the mean push out bond strength as compared to Group 1 (control group) (P < 0.001). Comparison of different collagen crosslinker showed that the highest pushout bond strength with root canal dentin was found to be in Groups 3 (10% HPN), i.e., 21.43 ± 2.75 MPa, followed by Group 4 (1% RFV) 18.59 ± 1.70 MPa and Group 2 (10% SA) 14.35 ± 1.80 MPa.
DISCUSSION
Long-term survival of the destructed tooth depends on the postretention.[8] Clinical study done by Ebert J et al. showed a success rate of 95%–97% when glass or quartz fiber-reinforced resin posts were used.[8]
One of the factors to increase the retention of fiber posts and improve the fracture resistance of the bonded structures, is the use of resin cements,[9] however, debonding of resin from dentin leads to failure of adhesively luted fiber post.[3] If the collagen is not fully enveloped by adhesive or hybrid layer shows porosity, micro- and nano-pathways are formed which promotes interface degradation.,[10] which exposes collagen fibrils, making them available to dentin MMPs.[11] The acidic nature of adhesive systems and resin cements leads to the activation of MMPs.[3] Studies have shown that modifying the collagen by altering the number of cross-links, improves its mechanical properties and lowers the enzymatic degradation rate.[12]
Naturally occurring collagen crosslinkers such as SA, hesperidin, RFV, chlorhexidine,[13] etc., have been reported to increase the collagen cross-linking.[14] Hence, here in this study, 10% SA, 10% hesperidin and 1% riboflavin 5 phosphate were selected as crosslinking agents, and the push out the bond strength of fiber postcemented to radicular dentin was evaluated. The mean pushout strength values (± standard deviations) for the study groups so obtained were Group 1(normal Saline) 10.87 ± 1.41 MPa, Group 2 (10% SA) 14.35 ± 1.80 MPa, Group 3 (10% HPN) 21.43 ± 2.75 MPa, and Group 4 (1% RFV) 18.59 ± 1.70 MPa. With significantly improved bond strength values as compared to control group and significant difference among all the groups (P <0.001).
SA is an antioxidant and helps in the synthesis of hydroxyproline and hydroxylysine in collagen. Hydroxyproline stabilizes the collagen triple helix and hydroxylysine forms intermolecular collagen crosslinks.[15] In studies conducted by Lai et al., Srinivas Panchjanya, Kato, Nakabayashi, and Pashley et al., ascorbate improved the compromised bond after sodium hypochlorite usage. Significant improvement in the bond strength was seen by Srinivasulu et al. between resin composite to deep dentin, after bonding with a self-etch adhesive system.[14] This explains the improved bond strength value obtained with ascorbate as compared to the control group.
Ten percent SA's pushout bond strength (14.35 ± 1.80MPa) when was compared with 1% RFV (18.59 ± 1.70 MPa), was found to be lower and highly significant (P < 0.001). This could be because RFV is a potent producer of oxygen free radicals,[16] and it promotes telopeptidase activity (inhibits collagenase activity), leading to the strengthening of collagen fibrils.[17] Photoactivated RFV has been known to increase the resistance to biodegradation, the mechanical and physical properties, and the stabilizes the dentin matrix (Pashley et al.).
And also, 10% SA's pushout bond strength (14.35 ± 1.80MPa) was found to be lower than 10% HPN with significant P < 0.001. In a study done by Khoroushi and Kachuei, SA, however, showed better results than 10% HPN. This might be due to short irrigation period of 2 min and also 10% HPN was prepared as a hydroalcoholic gel which led to the adhesive failure due to bubbles formation on the cement surface.[18] However, in this study, 10% HPN solution was prepared by mixing it in DSMO solution and was used in solution form for 4 min. This shows that the irrigation time, volume, and the formulation of the irrigant may have an affect on the outcome of bond strength, which requires further detailed studies.
Group 4 that is 1% RFV showed higher pushout bond strength (18.59 ± 1.70 MPa) as compared to the control group (10.87 ± 1.41 MPa) with statistically significant P value of < 0.001.
RFV is (Vitamin B2). It has been used in inflammatory disorders of cornea and cross-linking and is known to increase the biomechanical rigidity by 4.5 times.[19] This property has been utilized on tooth dentin to improve collagen stability and strength. It is highly unstable and undergoes photoreduction to form singlet oxygen[20] and is an attractive crosslinker.[21] Riboflavin can inactivate MMPs due to direct MMP crosslinking.[22]
Study done by Fawzy et al. revealed that though ultraviolet A (UVA) light most effectively activate riboflavin, however, visible blue light showed to be a promising substitute for UVA. In studies done by Daood et al. and Fawzy et al., the effective concentrations of riboflavin to be used were found to be 1% and 3%. Hence, here in this study, 1% riboflavin was used for 4 min as irrigant followed by blue light activation for 20 s.
Group 3 (10% HPN) had the highest push out bond strength, 21.43 ± 2.75MPa, as compared to all the other groups and was statistically significant (P < 0.001).
HPN, is a citrus flavonoid.[23] Demineralized dentine collagen matrix treated with flavonoids enhance ultimate tensile strength (Bedran-Russo et al., 2007). Proanthocyanidin creates bridge-type hydrogen bonds between hydroxyl groups and carboxyl terminals of the amide band of the collagen fibrils (Hagerman and Butler, 1981; Han et al., 2003). This could probably explain the action of citrus flavonoids, and hence, the highest bond strength obtained with citrus flavanoid. In this study, however, 10% HPN was preferred over proanthocyanidin because it has a lower molecular weight. A recent study showed positive effects of several lower molecular weight flavonoids such as HPN, genipin, etc., (Hiraishi et al., 2013). HPN has various medical benefits such as antioxidative, anti-inflammatory and anticarcinogenic property.[18] HPN (HPN), has been used to study its collagen matrix stabilization effect on demineralized root caries.[5]
Limitation
Since the bond strengths were for a short period of timer, so the effect of collagen crosslinkers in long-term needs to be evaluated. There is a need to evaluate the durability of the adhesive interface in THE future studies. We also need to evaluate the biochemical properties of collagen crosslinkers so as to use them as root canal irrigants.
CONCLUSION
Within the limitations of this in vitro study, results showed that all the collagen crosslinkers used in the study, significantly increased the pushout bond strength of the fiber postluted to radicular dentin. 10% HPN for 4 min showed maximum strength followed by 1% RFV and 10% SA. However, further long-term studies are still required to check for their efficacy, long-term stability, and their concentrations for their formulations to be used in dentistry.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Raj M, Kumar S, Alagarsamy V, Charkravathy D. Evaluation of effect of various endodontic irrigants and intra canal medicaments on push out bond strength to root canal dentin – An in vitro study. IJCD. 2011;2:128–39. [Google Scholar]
- 2.Mohammadi Z. Sodium hypochlorite in endodontics: An update review. Int Dent J. 2008;58:329–41. doi: 10.1111/j.1875-595x.2008.tb00354.x. [DOI] [PubMed] [Google Scholar]
- 3.Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E, et al. Dental adhesion review: Aging and stability of the bonded interface. Dent Mater. 2008;24:90–101. doi: 10.1016/j.dental.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Joseph VM, Thomas MS. Effect Of 3% riboflavin on the adhesion of dental composite resin to etched dentin. Res J Pharm Biol Chem Sci. 2016;7:1829–34. [Google Scholar]
- 5.Islam SM, Hiraishi N, Nassar M, Sono R, Otsuki M, Takatsura T, et al. In vitro effect of hesperidin on root dentin collagen and de/re-mineralization. Dent Mater J. 2012;31:362–7. doi: 10.4012/dmj.2011-203. [DOI] [PubMed] [Google Scholar]
- 6.Prasansuttiporn T, Nakajima M, Kunawarote S, Foxton RM, Tagami J. Effect of reducing agents on bond strength to NaOCl-treated dentin. Dent Mater. 2011;27:229–34. doi: 10.1016/j.dental.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Liu X, Zhou J, Chen L, Yang Y, Tan J. UVA-activated riboflavin improves the strength of human dentin. J Oral Sci. 2015;57:229–34. doi: 10.2334/josnusd.57.229. [DOI] [PubMed] [Google Scholar]
- 8.Ebert J, Leyer A, Günther O, Lohbauer U, Petschelt A, Frankenberger R, et al. Bond strength of adhesive cements to root canal dentin tested with a novel pull-out approach. J Endod. 2011;37:1558–61. doi: 10.1016/j.joen.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Pallottini S, Llukacej A, Monaco C, Baldissara P. Fiber post bonding using self-etching and resin cements. J Dent Res. 2010;89:3. [Google Scholar]
- 10.dos Santos PH, Karol S, Bedran-Russo AK. Nanomechanical properties of biochemically modified dentin bonded interfaces. J Oral Rehabil. 2011;38:541–6. doi: 10.1111/j.1365-2842.2010.02175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carrilho MR, Carvalho RM, de Goes MF, di Hipólito V, Geraldeli S, Tay FR, et al. Chlorhexidine preserves dentin bond in vitro. J Dent Res. 2007;86:90–4. doi: 10.1177/154405910708600115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castellan CS, Bedran-Russo AK, Antunes A, Pereira PN. Effect of dentin biomodification using naturally derived collagen cross-linkers: One-year bond strength study. Int J Dent 2013. 2013 doi: 10.1155/2013/918010. 918010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Islam S, Hiraishi N, Nassar M, Yiu C, Otsuki M, Tagami J, et al. Effect of natural cross-linkers incorporation in a self-etching primer on dentine bond strength. J Dent. 2012;40:1052–9. doi: 10.1016/j.jdent.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 14.Srinivasulu S, Vidhya S, Sujatha M, Mahalaxmi S. Effect of collagen cross-linkers on the shear bond strength of a self-etch adhesive system to deep dentin. J Conserv Dent. 2013;16:135–8. doi: 10.4103/0972-0707.108194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murad S, Grove D, Lindberg KA, Reynolds G, Sivarajah A, Pinnell SR, et al. Regulation of collagen synthesis by ascorbic acid. Proc Natl Acad Sci U S A. 1981;78:2879–82. doi: 10.1073/pnas.78.5.2879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Radovic I, Monticelli F, Goracci C, Vulicevic ZR, Ferrari M. Self-adhesive resin cements: A literature review. J Adhes Dent. 2008;10:251–8. [PubMed] [Google Scholar]
- 17.Okada Y, Naka K, Kawamura K, Matsumoto T, Nakanishi I, Fujimoto N, et al. Localization of matrix metalloproteinase 9 (92-kilodalton gelatinase/type IV collagenase 5 gelatinase B) in osteoclasts: Implications for bone resorption. Lab Invest. 1995;72:311–22. [PubMed] [Google Scholar]
- 18.Khoroushi M, Kachuei M. Pull-out bond strength of a self-adhesive resin cement to NaOCl-treated root dentin: Effect of antioxidizing agents. Restor Dent Endod. 2014;39:95–103. doi: 10.5395/rde.2014.39.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wollensak G, Spoerl E, Seiler T. Stress-strain measurements of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking. J Cataract Refract Surg. 2003;29:1780–5. doi: 10.1016/s0886-3350(03)00407-3. [DOI] [PubMed] [Google Scholar]
- 20.Oster G, Holmstrom B. Riboflavin as an electron donor in photochemical reactions. J Am Chem Soc. 1961;83:1867–71. [Google Scholar]
- 21.Edwards AM, Silva E. Effect of visible light on selected enzymes, vitamins and amino acids. J Photochem Photobiol B. 2001;63:126–31. doi: 10.1016/s1011-1344(01)00209-3. [DOI] [PubMed] [Google Scholar]
- 22.Tezvergil-Mutluay A, Agee KA, Hoshika T, Carrilho M, Breschi L, Tjäderhane L, et al. The requirement of zinc and calcium ions for functional MMP activity in demineralized dentin matrices. Dent Mater. 2010;26:1059–67. doi: 10.1016/j.dental.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guardia T, Rotelli AE, Juarez AO, Pelzer LE. Anti-inflammatory properties of plant flavonoids.Effects of rutin, quercetin and hesperidin on adjuvant arthritis in rat. Farmaco. 2001;56:683–7. doi: 10.1016/s0014-827x(01)01111-9. [DOI] [PubMed] [Google Scholar]


