Abstract
Aims and Objectives:
To evaluate the influence of indirect chair-side polymerization of resin composite cores on the fracture resistance of overlaying IPS e.max Press crowns.
Materials and Methods:
Root canals of 60 extracted premolars were prepared to receive #2 fiber posts after the crowns were sectioned 2 mm above the cervical line. In Groups 1–3 (n = 10 each), posts were luted to the prepared dowel spaces using self-adhesive resin cement. Resin composite cores were then bonded and incrementally built-up using Filtek Z250 XT, Filtek P60, and Filtek P90 resin composites. In Groups 4–6 (n = 10 each), the fabricated post-core systems were subjected to post-curing heat and pressure treatment before cementation to their respective teeth using self-adhesive resin cement. Another 10 sound premolars served as control. All teeth in the test and control groups were then subjected to standardized preparation to receive IPS e.max Press crowns before testing their fracture resistance and the mode of restorations' failure. The collected results were statistically analyzed using ANOVA, Kruskal–Wallis, and Tukey's tests on the past software used at α = 0.05 to stand on the significance of the detected differences.
Results:
Significant differences were detected between the fracture resistance of teeth in different groups (ANOVA, P = 2.857E-35). Crowns in Groups 4–6 provided higher fracture resistance than those in Groups 1–3 (Tukey's test, P < 0.05). Crowns in Groups 4 and 6 provided higher fracture resistance than the control, while those in Groups 2 and 3 provided lower fracture resistance than the control (Tukey's test, P < 0.05).
Conclusion:
Indirect composite cores improved the fracture resistance of IPS e.max Press crowns when compared to directly fabricated post and cores. The directly and indirectly polymerized nanohybrid, methacrylate-based composite (Filtek Z250 XT) cores yielded the highest fracture resistance for the utilized all-ceramic crowns.
KEYWORDS: Ceramic crowns, composite cores, fiber post, fracture resistance, indirect polymerization
INTRODUCTION
The need to retain natural teeth, even when a significant portion of the crown has been lost, has dramatically increased through the few past decades. Endodontic treatment allows for the placement of posts and cores whose preparation yields studies which indicate more brittle teeth.[1,2] Investigators[2,3,4] have reported minor to no reduction in tooth hardness and resiliency in response to the expected change in the moisture content of dentin. Others[5,6] attributed the questionable biomechanical behavior of the endodontically treated teeth to the significant loss of tooth coronal substrates. At the same time, the remaining cervical tooth structure and the restorative approach also influence the clinical survival of treated teeth.[6,7,8,9] Therefore, the use of endodontic posts is recommended to retain, support, and anchor cores.[7,8,10] Many researchers[11,12] considered the inherent biomechanical character, retention, and stability of post-core systems crucial for the success and longevity of final restorations. Metal posts were standardly employed for many years; however, the incompatibility of their biomechanical properties with those of dentin led to develop the fiber-reinforced composite (FRC) posts. This alternative in terms of the elastic modulus, optical properties, and tensile strength added its ability to retain cores when used in conjunction with both resin-based cements and composite build-up materials.[12,13,14,15] Many types of the composite resins have been used as direct core build-up materials; however, recently developed materials that tout minimal shrinkage, improved bonding, and mechanical behaviors have been reported. These results could potentially affect the clinical survival of the final ceramic restoration.[16,17]
Normally, the success of the final crown restoration is greatly dependent on the long-term ability of the core material to resist complex intraoral stresses.[15] To achieve that goal, indirect ceramic post-core systems have been suggested, but their cost together with the time-consuming and complicated fabrication techniques limit their application in spite of the reported success.[18,19] The indirect chair-side composite restoratives normally present equivalent compositions to that of the direct materials, but their processing methods are different. Post-curing additional light and/or heat application is a relatively quick and easy technique that has been reported to increase the degree of conversion and improve the composites' mechanical characteristics and color stability.[20,21,22] This approach may present a viable alternative for both direct composite and indirect ceramic core build-up materials with better biomechanical behavior. Therefore, the current in vitro study aimed to evaluate the fracture resistance of pressed ceramic crowns supported with indirect chair-side fabricated resin composite cores.
MATERIALS AND METHODS
Seventy extracted single-rooted maxillary premolars were collected at the Orthodontic clinic, College of Dentistry, King Khalid University, upon the registration and approval of the research idea with the Scientific and Research Committee (SRC/REG/2013-2014/13), College of Dentistry, King Khalid University (The post-hoc power [OSP = 0.9074] was calculated to assure the reliability of the selected sample size) The collected teeth were cleaned up to remove both hard and soft deposits and thoroughly inspected to exclude the cracked ones before their inclusion in the current study. Ten of the selected teeth served as control following their standardized preparation (Axial reduction with 1.2 mm shoulder finish line located 1 mm above the cervical line, flat occlusal reduction, and final occluso-gingival height of 6 mm) using diamond burs (FG 846012, White Diamonds, Lakewood, NJ, USA) on a lathe to receive IPS e.max Press (Ivoclar Vivadent, Schaan, Liechtenstein) crowns. Crowns of the remaining teeth were sectioned 2 mm above the cervical line, and root canals were prepared to receive size 2 resin-impregnated endodontic glass fiber post (RelyX Fiber Post, 3M ESPE, St. Paul, MN, USA) using the enclosed series of drills to the matched size. This rotary process achieved a standardized 10-mm long dowel space. The teeth were then divided into six test groups (n = 10 each) according to the protocol selected for post and core construction [Figure 1].
Figure 1.
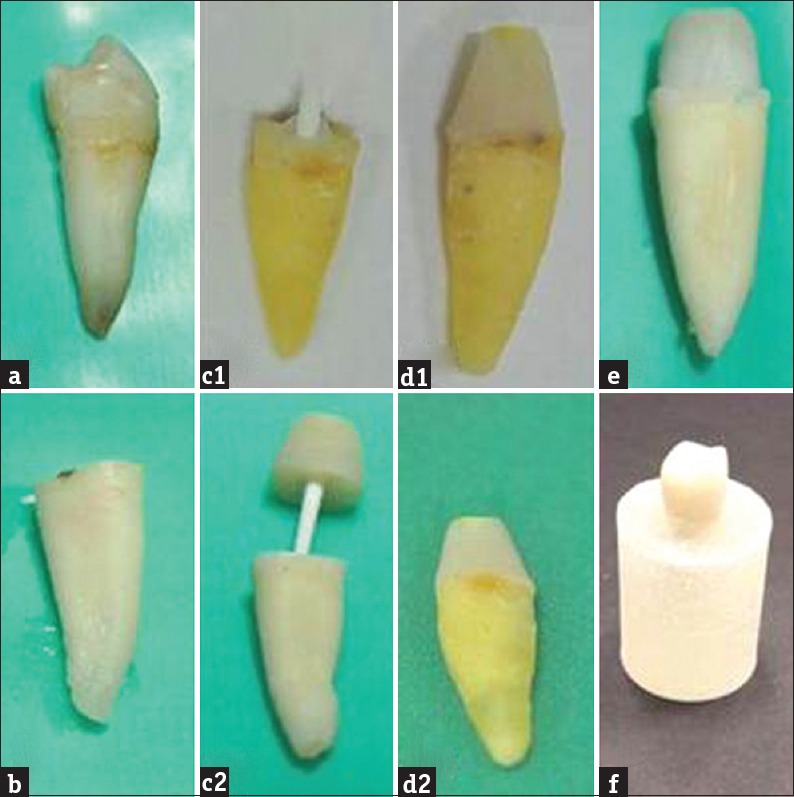
Construction of test specimens: (a) extracted premolar, (b) sectioning the crown, (c1) cementation of fiber post for direct core build-up, (c2) fabricating indirect chair-side post and core, (d1) direct composite core, (d2) cementation of indirect chair-side post and core, (e) standard preparation of cores to receive ceramic crowns, and (f) cemented ceramic crown in place
The length of posts utilized in all test groups was first adjusted using diamond discs (EDENA, Au/SG, Switzerland) in a low-speed handpiece to have only 3 mm extension above the flat coronal surface of each tooth. In groups 1–3, the entire bodies of the selected posts were meticulously cleaned up and dried. Two coats of Adper Single Bond Plus adhesive (3M ESPE, St. Paul, MN, USA) were then agitated against the apical 12 mm of post length and light cured for 10 s (Elipar FreeLight 2, 3M ESPE AG, Seefeld, Germany). All posts were then cemented to their respective dowel spaces using self-adhesive resin cement (RelyX Unicem 2 Automix, 3M ESPE, St. Paul, MN, USA). The auto-mixed cement was injected into the prepared dowel spaces and the posts were then introduced to the full depth. The excess cement was gently swabbed away and the margins exposed around the cemented post were then light-cured for 20 s.
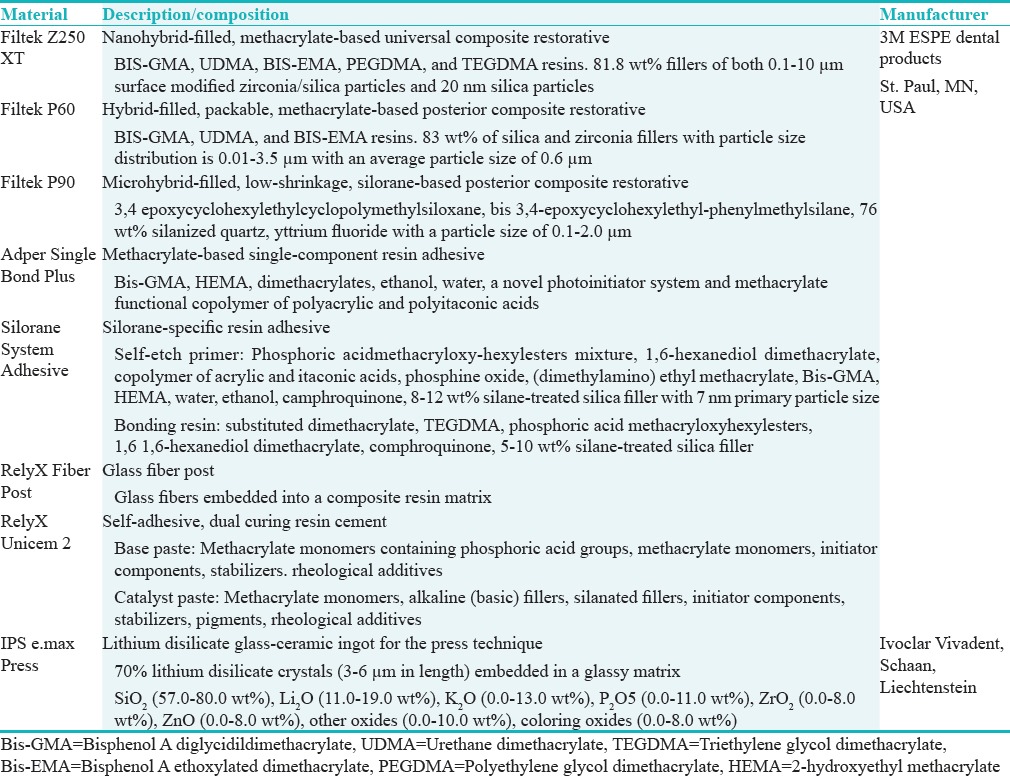
In Groups 1–3, three different composite restorative materials (Filtek Z250 XT, Filtek P60, and Filtek P90, 3M ESPE, St. Paul, MN, USA) were used to directly build the composite cores up. The details of the materials used in this study are listed in Table 1. The dentin first was etched for 15 s (Scotchbond Universal Etchant, 3M, ESPE, St. Paul, MN, USA), washed up, and plot dried to remain moist. In Groups 1 and 2 where the methacrylate-based composites (Filtek Z250 XT and Filtek P60) were hired for core building up, two coats of Adper Single Bond Plus adhesive (3M ESPE, St. Paul, MN, USA) were agitated and light cured for 10 s against the etched tooth surfaces together with the exposed 3 mm of the cemented posts. However, in Group 3 where the silorane-based composite (Filtek P90) was hired for core building up, two coats of the compatible silorane-specific adhesive were agitated and light-cured for 10 s against the etched tooth surfaces together with the exposed 3 mm of the cemented posts. The direct composite cores were built up in two successive increments; each was cured for 20 s, to be 1 mm above the exposed posts and to the full circumference of the remaining coronal tooth structure.
Table 1.
Materials used
In Groups 4–6, all posts were first introduced to the full depth of their respective dowel spaces with no cementation. The exposed parts of the utilized posts were coated with the resin adhesive that is compatible with the same Filtek Z250 XT, Filtek P60, and Filtek P90 composite core materials. The composite cores in Groups 4–6 were built up and bonded only against the exposed resin-coated parts of the fiber posts but with no bonding to the tooth surfaces. The constructed post-core systems were then removed out of their teeth and subjected to post-curing heat and pressure treatment in an autoclave (Type B Lisa autoclave, W and H Sterilization Srl., Brusaporto [BG], Italy) using B-Universal 121 cycle for 41 min at 122.5°C and a pressure of 1.16 bars (116 kPa).[23,24] Before cementing each onto its corresponding tooth, two escape grooves were prepared on the basal surface of each composite core using diamonds #FG 846012 to allow the excess cement to escape. The basal surface of each core surface was then subjected to 30 s of sandblasting with 110 μm alumina particles bombarded at 10.3 kPa. Following the ultrasonic cleaning and air drying, the roughened core surface together with the exposed post was coated with two layers of Adper Single Bond Plus adhesive and cured for 15 s. The prepared dowel space and the top coronal surface of each tooth were thoroughly cleaned and dried before using the self-adhesive resin cement (RelyX Unicem 2 Automix) to lute the indirectly prepared post-core systems in place.
Teeth in all test groups were also prepared following the previously mentioned criteria to receive IPS e.max Press crowns. Standardized anatomical wax patterns of the designed crowns were first constructed by the aid of medium-body polyvinyl index (Imprint, 3M ESPE, St. Paul, MN, USA) and wax sprues 3 mm in diameter were then attached to each at 45°. The constructed patterns were invested in Empress 2 speed investment material (Ivoclar Vivadent, Schaan, Liechtenstein). The set investment blocks were preheated at 850°C for 60 min, before press filling with the softened ceramic material in an Empress furnace at 910° for 20 min. After divesting, finishing, and staining of the constructed crowns, their intaglio surfaces were etched with 9.5% hydrofluoric acid (Porcelain etchant, Bisco Inc., Schaumburg, IL, USA), silanated (ESPE Sil, 3M ESPE), and left to dry for 5 min. All the constructed crowns were cemented onto their corresponding teeth using the same self-adhesive resin cement under pressure after sandblasting the outer surfaces of the indirect cores in Groups 4–6. The excess cement was light-cured for 5 s before its removal with sharp scaler, and the crown margins were then subjected to additional exposure to the curing light for 15 s.
Roots of all specimens were dipped once in light viscosity vinyl polysiloxane impression material (Imprint II Garant, 3M ESPE, Seefeld, Germany) to receive a single coat in representation of the periodontal ligament. After setting of this coating, all roots were embedded into acrylic blocks (Hygienic, Coltene/Whaledent AG. Altstatten, Switzerland) 1.0 mm apical to the cervical line.
To simulate normal oral functions, all specimens were subjected to further cyclic fatigue loading at 50 N for 240,000 cycles[25] and thermocycling at 5°C–55°C (MSCT-1, São Carlos, SP, Brazil) following ISO-TR 11405 Standard for 3500 cycles with a dwell time of 30 s[26,27] before testing their fracture resistance on a universal testing machine (Model 5965, Instron, Grove City, PA, USA). A metal rod running at crosshead speed of 0.5 mm/min was used to stress all crowns to failure. The maximum load at failure ( first audible cracking sound) was recorded for each crown. The data recorded for the test groups (Groups 1–6) were first analyzed using 2-way ANOVA to detect any source of interaction between the two test variables. All the collected data, including those of the control, were then subjected to statistical analysis using 1-way ANOVA and Tukey's comparisons at α = 0.05 to test the significance of differences detected between groups. The mode of failure in each of the tested specimens was also assessed and ranked according to the severity as 1 for dislodged post-core-crown restoration, 2 for the fracture in ceramic crown, 3 for the fracture in both composite core and the overlaying ceramic crown, and 4 for the nonrestorable root fracture. The collect failure mode data were then statistically analyzed using Kruskal–Wallis test at α = 0.05 to detect any significant differences between the tested groups.
RESULTS
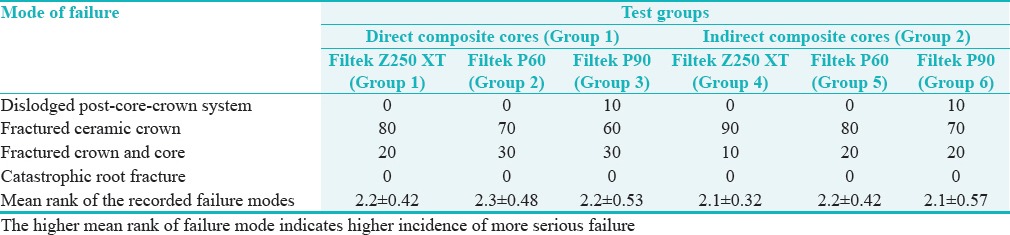
Mean fracture loads and standard divisions of teeth in different groups are listed in Table 2. The 2-way ANOVA indicated significant differences between different types of resin composite cores (P < 0.0001) and between the different polymerization modes (P < 0.0001). However, no interaction between the two variables was detected (P = 0.1041). On the other hand, after inclusion of the control group, significant differences were detected between the fracture resistance of teeth in different groups (ANOVA, P = 2.857E-35). Crowns supported with indirect cores in Groups 4–6 showed higher fracture resistance than those supported with direct cores in Groups 1–3 (Tukey's test, P < 0.05). Crowns in Groups 4 and 6 provided higher fracture resistance than those of the control group (Tukey's test, P = 0.0001309 and 0.0002512), while those in Groups 2 and 3 provided lower fracture resistance than the control (Tukey's test, P = 0.0001309 and 0.0001313). Only those teeth of Group 5, restored using indirect hybrid composite (Filtek P60) cores, showed comparable fracture resistance to the control (Tukey's test, P = 0.4047). The majority of the restored teeth in all subgroups showed a favorable mode of failure, where the catastrophic fracture of the ceramic crowns was dominant [Table 3]. Statistical analysis of the ranked failure data showed no difference between the tested groups (Kruskal–Wallis test, P = 0.9374).
Table 2.
Mean fracture loads (n) and standard divisions of restored teeth in different groups
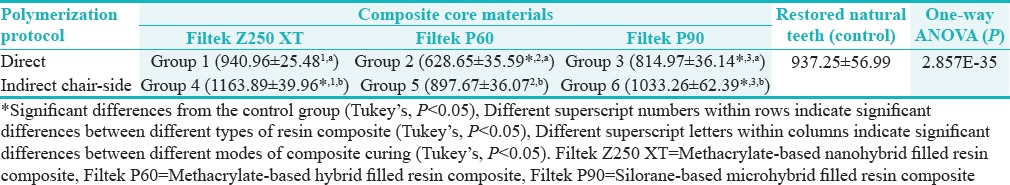
Table 3.
Incidences (%) of different modes of failure
DISCUSSION
The altered biomechanical behavior of endodontically treated teeth with compromised clinical crowns[5,6] often necessitates the use of endodontic posts to retain, support, and anchor cores built up at the time of restoration.[7,8,10] The use of FRC posts, with mechanical and esthetic advantages, combined with a core of resin composite is currently a popular choice.[12,13,14,15] This kind of post-core system can be adhesively bonded to the tooth structure with a direct impact on the clinical longevity of the final ceramic restoration.[6,17] The long-term ability of the core material to resist complex intraoral stresses has also been reported to influence the survival of the overlaying crown restorations.[15,28] Indirect metallic or ceramic post-core systems have been suggested; however, their cost and time-consuming and complicated fabrication procedure have limited their routine application.[18,19,28] On the other hand, post-curing treatment has been reported to improve the mechanical properties of direct resin composite restoratives since they display the same basic composition as those designed for indirect applications.[24,29,30] The curing technique employing additional heat and pressure was used in this study to fabricate indirect chair-side composite cores that hypothesized to add support to yield improved fracture strength to the overlaying ceramic restoration.
IPS e.max Press was selected to present an important category (lithium disilicate glass-ceramic) of the currently available ceramic materials. This material can offer full-size ceramic restorations with improved flexure strength (360–400 MPa) and excellent esthetics with no need for a veneering material.[31] The supporting core build-ups were made of resin composites commonly available in practice. These materials represent composites with different resin formulations and filler characteristics normally utilized for direct restorative applications [Table 1].
In this in vitro study, the stated null hypothesis was rejected as both factors significantly affected the fracture resistance of the IPS e.max Press crowns with no interaction. Significant differences were observed between the fracture resistance values of crowns supported with different types of resin composite cores [Table 2]. Regardless of the employed curing technique, crowns supported with nanohybrid composite cores (Filtek Z250 XT) registered the highest fracture resistance among all test groups. This result may be related to the composition and the degree of conversion effects on the materials' mechanical properties.[32]
Boaro et al.[33] reported higher degree of conversion and higher mechanical properties of Filtek Z250 in comparison to the silorane-based resin composites (Filtek LS) although both having hybrid-filled nature. However, each of those materials has different resin base offering different degrees of conversion, in addition to different filler characteristics and loadings (Filtek Z250, 78.7 wt% of zirconia and silica fillers with a particle size distribution of 0.01–3.5 μm and Filtek LS, 76 wt% of quartz and yttrium fluoride fillers with a particle size distribution of 0.1–2.0 μm). The recent modification of Filtek Z250 by adding nanofillers (20 nm in diameter) to its composition [Table 1] increased the filler loading to 81.8 wt%, and the manufacturer reports better adaptation of the fillers infiltrated by the methacrylate resin base and this may be responsible for the reported improvement in this material's mechanical properties.[32] Although Filtek P60 has a very high filler content (83 wt% of zirconia and silica fillers), the reported size and shape of those fillers may not optimize adaptation leaving larger resin-filled spaces when compared to the nanofilled composites. This structural nature may be the source of the lower final fracture resistance of the material in the present study, including its ultimate strength and modulus of elasticity.[34,35,36]
Based on the aforementioned analysis, composite materials with higher strengths and moduli of elasticity are expected to offer higher resistance to deformation and better support to overlaying ceramic crowns which, in turn, may reflect on crowns' fracture resistance. This explanation could support the recorded higher fracture resistance of ceramic crowns supported with Filtek Z250 XT cores when compared to those supported with Filtek P60 and Filtek P90 cores. D'Alpino et al.[37] and Bechtold et al.[38] also reported lower degrees of conversion and lower mechanical properties of silorane-based composite (Filtek LS) when compared with a hybrid-filled methacrylate (Filtek P60). They related their results to the difference in the materials' filler types and loadings. Although their findings could be contradicting with the finding of the current study that indicated better support of the microhybrid silorane-based composite cores for the overlaying crowns than the hybrid-filled methacrylate-based cores, the difference size, shape, and arrangement of filler particles within the cured structure of both composite materials and the amount of the existing inter-particular resin base may attribute to and explain the recorded results.[34,35,36]
Higher fracture resistance of ceramic crowns was obvious in all specimens restored with indirect chair-side cores in Groups 4–6. Regardless the type of resin composite employed, all indirectly polymerized post and cores were almost equivalent in strength to restored natural teeth. The noticed improvement (23% for Filtek Z250XT, 42% for Filtek P60, and 27% for Filtek P90, respectively), resulted in specimens having fracture resistance comparable to (Filtek P60) or higher than (Filtek Z250 XT and Filtek P90) the control [Table 2]. This significant improvement in the fracture resistance reflects the potential for post-curing to provide improved support to the overlaying ceramic crowns that, in this study, reflected positively on their fracture resistance. This postulation can be supported with the documented fact that increased degree of conversion is observed following post-curing application of heat, pressure, or high-intensity light.[24,39] The increased degree of conversion together with potential relief of internal shrinkage stresses has often been reported to improve mechanical properties, including the modulus of elasticity.[24,40,41] Almeida-Chetti et al.[42] and Jacobsen and Darr[43] reported a significant improvement in the modulus of elasticity of resin composites subjected to post-curing treatment. That improvement would consequently increase the resistance of the indirect chair-side cores to deflection/deformation under the applied occlusal forces. At the same time, it was obvious that the tested specimens mostly showed favorable/restorable mode of failure with no statistical significant differences between different test groups. This finding could be a true reflection of the ability of composite core materials, regardless their mode of polymerization, together with the fiber post to favorably transfer the loading stresses throughout the restoration–root complex.[44,45]
Although testing specimens under oblique occlusal stresses could be relevant from a clinical point of view, results of the current study implicated that the indirect cores have the potential to optimize mechanical properties of the composites tested and represent a viable chair-side technique for build-ups prior to restoration with e.max Press crowns.
CONCLUSION
Indirect composite cores improved the fracture resistance of IPS e.max Press crowns when compared to directly fabricated post and cores. The directly and indirectly polymerized nanohybrid, methacrylate-based composite (Filtek Z250 XT) cores yielded the highest fracture resistance for the all-ceramic crowns used in this study.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Helal MA, Wang Z. Biomechanical assessment of restored mandibular molar by endocrown in comparison to a glass fiber post-retained conventional crown: 3D finite element analysis. J Prosthodont. 2017 doi: 10.1111/jopr.12690. doi: 101111/jopr12690. [DOI] [PubMed] [Google Scholar]
- 2.Slutzky-Goldberg I, Slutzky H, Gorfil C, Smidt A. Restoration of endodontically treated teeth review and treatment recommendations. Int J Dent 2009. 2009:150251. doi: 10.1155/2009/150251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewinstein I, Grajower R. Root dentin hardness of endodontically treated teeth. J Endod. 1981;7:421–2. doi: 10.1016/S0099-2399(81)80042-8. [DOI] [PubMed] [Google Scholar]
- 4.Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992;18:332–5. doi: 10.1016/S0099-2399(06)80483-8. [DOI] [PubMed] [Google Scholar]
- 5.Gholami F, Kohani P, Aalaei S. Effect of nickel-chromium and non-precious gold color alloy cast posts on fracture resistance of endodontically treated teeth. Iran Endod J. 2017;12:303–6. doi: 10.22037/iej.v12i3.10586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature – Part 1.Composition and micro- and macrostructure alterations. Quintessence Int. 2007;38:733–43. [PubMed] [Google Scholar]
- 7.Lazari PC, de Carvalho MA, Del Bel Cury AA, Magne P. Survival of extensively damaged endodontically treated incisors restored with different types of posts-and-core foundation restoration material. J Prosthet Dent. 2017 doi: 10.1016/j.prosdent.2017.05.012. pii: S0022-3913(17)30368-2. [DOI] [PubMed] [Google Scholar]
- 8.Santos-Filho PC, Veríssimo C, Raposo LH, Noritomi MecEng PY, Marcondes Martins LR. Influence of ferrule, post system, and length on stress distribution of weakened root-filled teeth. J Endod. 2014;40:1874–8. doi: 10.1016/j.joen.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Kar S, Tripathi A, Trivedi C. Effect of different ferrule length on fracture resistance of endodontically treated teeth: An in vitro study. J Clin Diagn Res. 2017;11:ZC49–52. doi: 10.7860/JCDR/2017/24669.9675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung W. A review of the management of endodontically treated teeth. Post, core and the final restoration. J Am Dent Assoc. 2005;136:611–9. doi: 10.14219/jada.archive.2005.0232. [DOI] [PubMed] [Google Scholar]
- 11.Bitter K, Perdigão J, Exner M, Neumann K, Kielbassa A, Sterzenbach G, et al. Reliability of fiber post bonding to root canal dentin after simulated clinical function in vitro. Oper Dent. 2012;37:397–405. doi: 10.2341/11-066-L. [DOI] [PubMed] [Google Scholar]
- 12.Othman HI, Elshinawy MI, Abdelaziz KM. Retention of fiber posts to the optimally and over-prepared dowel spaces. J Adv Prosthodont. 2013;5:16–20. doi: 10.4047/jap.2013.5.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choudhary S, Begum Z, Choudhary P, Tripathi S. Comparative evaluation of retention of prefabricated and conventional cast post: An in vitro study. J Int Soc Prev Community Dent. 2014;4:87–91. doi: 10.4103/2231-0762.137635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duret B, Duret F, Reynaud M. Long-life physical property preservation and postendodontic rehabilitation with the composipost. Compend Contin Educ Dent Suppl. 1996;20:S50–6. [PubMed] [Google Scholar]
- 15.Panitiwat P, Salimee P. Effect of different composite core materials on fracture resistance of endodontically treated teeth restored with FRC posts. J Appl Oral Sci. 2017;25:203–10. doi: 10.1590/1678-77572016-0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azer SS, Drummond JL, Campbell SD, El Moneim Zaki A. Influence of core buildup material on the fatigue strength of an all-ceramic crown. J Prosthet Dent. 2001;86:624–31. doi: 10.1067/mpr.2001.120656. [DOI] [PubMed] [Google Scholar]
- 17.Agrawal A, Mala K. An in vitro comparative evaluation of physical properties of four different types of core materials. J Conserv Dent. 2014;17:230–3. doi: 10.4103/0972-0707.131782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vinothkumar TS, Kandaswamy D, Chanana P. CAD/CAM fabricated single-unit all-ceramic post-core-crown restoration. J Conserv Dent. 2011;14:86–9. doi: 10.4103/0972-0707.80730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ozcan N, Sahin E. In vitro evaluation of the fracture strength of all-ceramic core materials on zirconium posts. Eur J Dent. 2013;7:455–60. doi: 10.4103/1305-7456.120671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ritter AV, Fahl N, Jr, Vargas M, Maia RR. The direct-indirect technique for composite restorations revisited. Compend Contin Educ Dent. 2017;38:e9–12. [PubMed] [Google Scholar]
- 21.Terry DA, Touati B. Clinical considerations for aesthetic laboratory-fabricated inlay/onlay restorations: A review. Pract Proced Aesthet Dent. 2001;13:51–8. [PubMed] [Google Scholar]
- 22.Cesar PF, Miranda WG, Jr, Braga RR. Influence of shade and storage time on the flexural strength, flexural modulus, and hardness of composites used for indirect restorations. J Prosthet Dent. 2001;86:289–96. doi: 10.1067/mpr.2001.114513. [DOI] [PubMed] [Google Scholar]
- 23.Nandini S. Indirect resin composites. J Conserv Dent. 2010;13:184–94. doi: 10.4103/0972-0707.73377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soares CJ, Pizi EC, Fonseca RB, Martins LR. Mechanical properties of light-cured composites polymerized with several additional post-curing methods. Oper Dent. 2005;30:389–94. [PubMed] [Google Scholar]
- 25.Heintze SD, Faouzi M, Rousson V, Ozcan M. Correlation of wear in vivo and six laboratory wear methods. Dent Mater. 2012;28:961–73. doi: 10.1016/j.dental.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 26.Subramanian D, Sivagami G, Sendhilnathan D, Rajmohan C. Effect of thermocycling on the flexural strength of porcelain laminate veneers. J Conserv Dent. 2008;11:144–9. doi: 10.4103/0972-0707.48835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Critchlow S. Ceramic materials have similar short term survival rates to other materials on posterior teeth. Evid Based Dent. 2012;13:49. doi: 10.1038/sj.ebd.6400860. [DOI] [PubMed] [Google Scholar]
- 28.Rouvinen E, Näpänkangas R, Raustia A. A report on materials used by dental students for core restorations in single and multiunit crowns. Int J Prosthodont. 2014;27:73–5. doi: 10.11607/ijp.3609. [DOI] [PubMed] [Google Scholar]
- 29.Kildal KK, Ruyter IE. How different curing methods affect the degree of conversion of resin-based inlay/onlay materials. Acta Odontol Scand. 1994;52:315–22. doi: 10.3109/00016359409029044. [DOI] [PubMed] [Google Scholar]
- 30.Tanoue N, Matsumura H, Atsuta M. Properties of four composite veneering materials polymerized with different laboratory photo-curing units. J Oral Rehabil. 1998;25:358–64. doi: 10.1046/j.1365-2842.1998.00241.x. [DOI] [PubMed] [Google Scholar]
- 31.Culp L, McLaren EA. Lithium disilicate: The restorative material of multiple options. Compend Contin Educ Dent. 2010;31:716. [PubMed] [Google Scholar]
- 32.Kim KH, Ong JL, Okuno O. The effect of filler loading and morphology on the mechanical properties of contemporary composites. J Prosthet Dent. 2002;87:642–9. doi: 10.1067/mpr.2002.125179. [DOI] [PubMed] [Google Scholar]
- 33.Boaro LC, Gonçalves F, Guimarães TC, Ferracane JL, Pfeifer CS, Braga RR, et al. Sorption, solubility, shrinkage and mechanical properties of “low-shrinkage” commercial resin composites. Dent Mater. 2013;29:398–404. doi: 10.1016/j.dental.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Manhart J, Kunzelmann KH, Chen HY, Hickel R. Mechanical properties and wear behavior of light-cured packable composite resins. Dent Mater. 2000;16:33–40. doi: 10.1016/s0109-5641(99)00082-2. [DOI] [PubMed] [Google Scholar]
- 35.Oberholzer TG, Grobler SR, Pameijer CH, Hudson AP. The effects of light intensity and method of exposure on the hardness of four light-cured dental restorative materials. Int Dent J. 2003;53:211–5. doi: 10.1111/j.1875-595x.2003.tb00747.x. [DOI] [PubMed] [Google Scholar]
- 36.Peris AR, Mitsui FH, Amaral CM, Ambrosano GM, Pimenta LA. The effect of composite type on microhardness when using quartz-tungsten-halogen (QTH) or LED lights. Oper Dent. 2005;30:649–54. [PubMed] [Google Scholar]
- 37.D'Alpino PH, Bechtold J, dos Santos PJ, Alonso RC, Di Hipólito V, Silikas N, et al. Methacrylate- and silorane-based composite restorations: Hardness, depth of cure and interfacial gap formation as a function of the energy dose. Dent Mater. 2011;27:1162–9. doi: 10.1016/j.dental.2011.08.397. [DOI] [PubMed] [Google Scholar]
- 38.Bechtold J, Dos Santos PJ, Anido-Anido A, Di Hipólito V, Alonso RC, D'Alpino PH, et al. Hardness, polymerization depth, and internal adaptation of class II silorane composite restorations as a function of polymerization protocol. Eur J Dent. 2012;6:133–40. [PMC free article] [PubMed] [Google Scholar]
- 39.Park SH. Comparison of degree of conversion for light-cured and additionally heat-cured composites. J Prosthet Dent. 1996;76:613–8. doi: 10.1016/s0022-3913(96)90439-4. [DOI] [PubMed] [Google Scholar]
- 40.de Gee AJ, Pallav P, Werner A, Davidson CL. Annealing as a mechanism of increasing wear resistance of composites. Dent Mater. 1990;6:266–70. doi: 10.1016/S0109-5641(05)80008-9. [DOI] [PubMed] [Google Scholar]
- 41.Loza-Herrero MA, Rueggeberg FA, Caughman WF, Schuster GS, Lefebvre CA, Gardner FM, et al. Effect of heating delay on conversion and strength of a post-cured resin composite. J Dent Res. 1998;77:426–31. doi: 10.1177/00220345980770021201. [DOI] [PubMed] [Google Scholar]
- 42.Almeida-Chetti VA, Macchi RL, Iglesias ME. Effect of post-curing treatment on mechanical properties of composite resins. Acta Odontol Latinoam. 2014;27:72–6. doi: 10.1590/S1852-48342014000200005. [DOI] [PubMed] [Google Scholar]
- 43.Jacobsen PH, Darr AH. Static and dynamic moduli of composite restorative materials. J Oral Rehabil. 1997;24:265–73. doi: 10.1046/j.1365-2842.1997.d01-288.x. [DOI] [PubMed] [Google Scholar]
- 44.Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence ofvertical root fracture of pulpless teeth restored with six post-and-coresystems. J Prosthet Dent. 1999;81:262–9. doi: 10.1016/s0022-3913(99)70267-2. [DOI] [PubMed] [Google Scholar]
- 45.Pilo R, Cardash HS, Levin E, Assif D. Effect of core stiffness on the in vitro fracture of crowned, endodontically treated teeth. J Prosthet Dent. 2002;88:302–6. doi: 10.1067/mpr.2002.127909. [DOI] [PubMed] [Google Scholar]


