Inactivation of Ebola virus by 0.1% Triton X-100 or sodium dodecyl sulfate is annulled by serum. Although this treatment does not interfere with clinical chemistry tests, it is not a safe way to inactivate blood samples from Ebola virus–infected patients.
Keywords: Ebola, inactivation, Triton, sodium dodecyl sulfate (SDS), detergent
Abstract
Background
Treatment of blood samples from hemorrhagic fever virus (HFV)–infected patients with 0.1% detergents has been recommended for virus inactivation and subsequent safe laboratory testing. However, data on virus inactivation by this procedure are lacking. Here we show the effect of this procedure on diagnostic test results and infectious Ebola virus (EBOV) titers.
Methods
Serum and whole-blood samples were treated with 0.1% or 1% sodium dodecyl sulfate (SDS) or 0.1% Triton X-100 and assayed for clinical chemistry and malaria antigen detection. Infectious EBOV titers were determined in SDS-treated plasma and whole blood from EBOV-infected nonhuman primates (NHPs). Infectious titers of EBOV or herpes simplex virus type 1 (HSV-1) in detergents-treated cell culture medium containing various serum concentrations were determined.
Results
Laboratory test results were not affected by 0.1% detergent treatment of blood samples, in contrast with 1% SDS treatment. However, 0.1% detergent treatment did not inactivate EBOV in blood samples from infected NHPs. Experiments with cell culture medium showed that virus inactivation by detergents is annulled at physiological serum concentrations.
Conclusions
Treatment of blood samples with 0.1% SDS or Triton X-100 does not inactivate EBOV. Inactivation protocols for HFV should be validated with serum and whole blood.
Possibilities to perform regular clinical laboratory tests are limited when dealing with samples from patients infected with hemorrhagic fever viruses (HFVs) due to biosafety issues. This again became painfully clear during the Ebola virus (EBOV) outbreak in West Africa. Ebola virus disease (EVD) is characterized by a gastrointestinal stage with profound diarrhea and vomiting leading to hypovolemia, systemic hypoperfusion, and electrolyte imbalances [1]. Although there are currently no approved antiviral therapies for EVD, aggressive fluid resuscitation, restoration of electrolyte imbalances, and treatment of coinfections are likely to improve survival of EVD patients [1–5]. During this outbreak, basic laboratory tests for infectious diseases and clinical chemistry parameters were sorely missed. This was not simply an issue for field settings; even in specialized laboratories, basic tests for disease management were unavailable or could not be performed due to safety issues. Such diagnostic tests are normally performed in laboratories with a lower biosafety level than is required for safe handling of EBOV-infected samples. In theory, tests could be performed in these laboratories after inactivation of EBOV. However, current tested and proven EBOV inactivation protocols, such as heat inactivation, gamma irradiation, or photoinducible alkylating agents, result in erroneous clinical chemistry test results, or specialized equipment that is often not available is needed [6–10]. In addition, the use of commercial lysis buffers containing guanidinium isothiocyanate in combination ethanol, a procedure to inactivate EBOV and extract EBOV RNA from blood samples prior to polymerase chain reaction analysis, would also result in erroneous clinical chemistry test results.
Ebola viruses are enveloped viruses and should be susceptible to inactivation by envelope-destroying detergents like Triton X-100 and sodium dodecyl sulfate (SDS) under certain conditions. These detergents have long shelf-life at room temperature, are cheap, and are relatively nontoxic to humans. Previously it was shown that treatment of blood samples with 0.1% Triton X-100 does not affect results of clinical chemistry tests, malaria rapid diagnostic tests (RDTs), and several hematology tests [9, 11–13]. Some have recommended this procedure to inactivate HFVs, including EBOV, in blood samples prior to diagnostic testing [9–15]. However, data on EBOV inactivation by 0.1% Triton X-100 are currently lacking. This prompted the US Centers for Disease Control and Prevention to state that 100% efficacy in inactivating EBOV by this procedure cannot be assumed [16]. Sodium dodecyl sulfate , another commonly used detergent for virus inactivation, has proven activity against enveloped viruses at concentrations of ≤0.1% and, in contrast to Triton X-100, even nonenveloped viruses [17–21]. Preliminary data suggest that EBOV in culture medium is inactivated by 0.1% SDS treatment [22]. These studies reported on inactivation of viruses present in culture medium containing low serum concentrations, but whole-blood or pure serum samples were not included. It is currently not known whether this procedure inactivates EBOV in pure serum or whole blood, nor is the effect of this procedure on diagnostic test results known.
In this study, we show the effect of treatment of serum and whole-blood samples with 0.1% SDS or Triton X-100 on results of clinical chemistry tests, malaria RDTs, and rapid blood-typing tests, as well as on infectious EBOV titers in blood samples from EBOV-infected nonhuman primates (NHPs). In addition, we performed EBOV inactivation experiments using cell culture medium mixed with serum at various ratios to delineate the effect of serum on the capacity of detergents to inactivate EBOV. To make more general statements on the inactivation of enveloped viruses in whole blood and serum, we included herpes simplex virus type 1 (HSV-1) in these experiments because ample data are available on the inactivation of this virus using detergents at concentrations of 0.1% [17–21].
METHODS
Ethics and Biosafety Statement
All animal work was performed in strict accordance with the Guide for the Care and Use of Laboratory Animals, Office of Laboratory Animal Welfare, National Institutes of Health and the Animal Welfare Act, United States Department of Agriculture. Animal procedures were conducted under anesthesia by trained personnel under supervision of veterinary staff. All efforts were made to promote welfare and to minimize animal distress in accordance with recommendations from the Weatherall report for the use of NHPs. All work with infectious material was performed in the maximum containment laboratory at the Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, Hamilton, Montana, applying standard operating protocols approved by the Institutional Biosafety Committee. Materials from human subjects used in this study were from EBOV-negative patients. These materials were obtained for routine patient care. Leftovers of these materials were anonymized and used for this study. Informed consent for use of anonymized leftover patient material was waived. This procedure has been approved by the Medical Ethical Committee of the Erasmus MC (MEC-2015–306), as well as by Dutch law.
Inactivation Chemicals
Triton X-100 and ultrapure 10% (w/v) SDS aqueous solution were obtained from Sigma-Aldrich and Invitrogen, respectively. A 10% (v/v) Triton X-100 working solution was prepared by mixing pure Triton X-100 with distilled water.
Clinical Chemistry
Serum samples were mixed 99:1 (v/v) with 10% SDS (final concentration 0.1%), 9:1 (v/v) with 10% SDS (1%), 99:1 (v/v) with 10% Triton X-100 (0.1%), or were not mixed (controls) and were incubated for 0, 30, or 60 minutes at room temperature and subsequently assayed for concentration of sodium, potassium, chloride, calcium, alanine transaminase, aspartate transaminase, gamma-glutamyl transferase, alkaline phosphatase, creatinine, blood urea nitrogen, ureic acid, amylase, albumin, total protein, and C-reactive protein (Piccolo Xpress analyzer, Abaxis, Union City, USA). For each parameter, 10 serum samples spanning the clinically relevant range for that particular parameter were used. Test results were corrected for the dilution factor caused by addition of Triton X-100 or SDS, and sodium test results were corrected for the amount of sodium present in SDS.
Malaria Rapid Antigen Test
Stored ethylenediaminetetraacetic acid (EDTA) whole-blood samples from 3 Plasmodium falciparum–positive patients were serially diluted in freshly collected malaria-negative EDTA whole blood. Malaria-free EDTA whole blood was used as a negative control. Samples were treated as described above and analyzed using the ICT Malarial Dual Test (cassette) (ICT Diagnostics, Cape Town, South Africa) according to the manufacturer’s instruction. Two technicians interpreted the test results independently (1 blinded and 1 not blinded), and intensities of the visible histidine-rich protein 2 (HRP-2) and Plasmodium lactate dehydrogenase (pLDH) bands of a positive test were scored using a subjective scale ranging from ± (weakly positive) to 3+ (strongly positive).
Blood Group Typing
MDmulticard ABO-D CONFIRM blood typing cards (Medion Grifols Diagnostics AG, Düdingen, Switzerland) were used for blood group typing of 38 whole-blood samples treated with 1% SDS for 1 hour at room temperature, 0.1% SDS for 1 hour at room temperature, or not treated (controls). Blood types of the 38 samples were blood group A-positive, RhD-positive (A+RhD+; n = 5); A+RhD− (n = 5), B+RhD+ (n = 5), B+RhD− (n = 5), AB+RhD+ (n = 6), AB+RhD− (n = 2), O+RhD+ (n = 5), and O+RhD− (n = 5) as determined by the ABO/Rh blood group reference method AutoVue Innova system (Ortho Clinical Diagnostics, Tilburg, The Netherlands) [23]. MDmulticards were used according to the manufacturer’s instructions, except that SDS-treated samples were mixed with 100 µL of diluent F instead of 200 µL because this resulted in slightly better diffusion of the samples on the MDmulticard. Four persons scored the results independently (2 blinded and 2 not blinded).
Inactivation of Ebola Virus in Serum and Whole Blood from Ebola Virus–Infected Nonhuman Primates
Heparinized whole blood was collected and pooled from 3 rhesus macaques that were used as control animals for a previous vaccine study and euthanized due to EVD. The animals were challenged via intramuscular injection of 1000 PFUs of Ebola virus H.sapiens-tc/GUI/2014/Makona-WPGC07 [24]. One portion of pooled blood was used to generate plasma, and the remainder was used as whole blood. Plasma and whole blood were each divided into 3 aliquots for testing. Prior to addition of SDS, a 100-µL sample of blood and plasma was diluted in 900 µL of Dulbecco’s modified Eagle’s medium (DMEM; T0 control sample). Nineteen microliters of 10% SDS was added to each blood and serum sample, and 100-µL samples were removed at 10, 30, and 60 minutes, diluted in 900 µL of DMEM (Sigma, St. Louis, USA) with 2% fetal bovine serum (Gibco, Life Technologies Corporation, New York, USA), 2 mM of L-Glutamine (Gibco), 50 U/mL of penicillin (Gibco), and 50 µg/mL of streptomycin (Gibco). The 10-fold diluted sample was used as primary dilution in the titration procedure described below.
Quantitative Ebola Virus Infectivity Assay
Vero cells were seeded in 48-well flat-bottom plates (28080 cells/well) and cultured for 24 hours. Dilution plates were made by placing 900 µL of DMEM supplemented with 2% FBS, 1% L-Glutamine, and 1% pen/strep into each well of a 48-well plate. One hundred–microliter samples, taken at appropriate time points, were transferred to a well in the top row of the dilution plate (1:10 dilution). A dilution series was carried out by passing 100 µL sequentially down the plate. One hundred micoliters from each column of the dilution series was transferred to each of 4 columns of the cell plate. Plates were incubated at 37°C for 1 hours and washed twice with phosphate-buffered saline (PBS); 200 µL of DMEM with 2% FBS, 2 mM of L-Glutamine, 50 U/mL of penicillin, and 50 µg/mL of streptomycin was added per well; and plates were cultured at 37°C for 14 days. After 14 days, wells were scored for presence of cytopathic effect (CPE), and the 50% Tissue Culture Infectious Dose (TCID50) was calculated (Spearman-Karber method).
Quantitative Herpes Simplex Virus Type 1 Infectivity Assay
A cell-free HSV-1 stock (passage 4, clinical HSV-1 isolate) was prepared on Vero cells cultured in DMEM (Lonza, Breda, The Netherlands) supplemented with 2 mM of L-glutamin (Lonza), 0.08% sodium bicarbonate (Lonza), 2% 2-[4-(2-hydroxyethyl)piperazin-1-yl]ethanesulfonic acid (HEPES) (Lonza), 100 U/mL of penicillin (Lonza), 100 µg/mL of streptomycin (Lonza), and 2.5 µg/mL of amphotericin B (Department of Pharmacy, ErasmusMC, Rotterdam, the Netherlands) and 1% FBS (Greiner Bio-One, Kremsmuenster, Austria). Vero cells were seeded in 96-well flat-bottom plates (20000 cells/well) and cultured for 24 hours. Virus stocks (starting dilution 1/50) were diluted using 5-fold dilution steps in DMEM supplemented with 1% FBS and tested in 8 replicates per dilution step. Plates were incubated at 36.5°C for 1 hour and washed twice with PBS, 200 µL of medium containing 10% FBS was added per well, and plates were cultured at 36.5°C for 7 days. After 7 days, wells were scored for presence of CPE, and the TCID50 was calculated (Spearman-Karber method).
Effect of Serum Concentration on Herpes Simplex Virus Type 1 and Ebola Virus Inactivation by Detergents
Herpes simplex virus type 1 was spiked in culture medium containing 0.98%, 9.8%, or 98% FBS prior to treatment with Triton X-100 (0.1%) or SDS (0.1%). Herpes simplex virus type 1 in 9.8% FBS and spiked with PBS served as control. Samples were incubated for 1 hour at room temperature, and subsequently infectivity in TCID50 was determined as described above. Experiments were performed in triplicate.
Ebola virus/Makona-C07 was spiked in culture medium containing 1%, 10%, or 95% FBS and Triton X-100 (0.1%), SDS (0.1%), or water in triplicate. Additionally, 1%, 10%, or 95% FBS containing Triton X-100 (0.1%), SDS (0.1%), or water without virus were run in triplicate to control for detergent effects on cells used in the titration. Samples were incubated for 1 hour at room temperature. To remove the detergent, 1 mL of each sample was loaded into a 100 K MWCO Amicon Ultra Centrifugal filter (Merck Millipore, Billerica, MA) and spun at 14000 × g for 10 minutes. The samples were then rinsed 3 times by adding 1 mL of PBS then spinning at 14000 × g for 10 minutes before adding 1 mL of DMEM with 2% FBS, 2 mM of L-Glutamine, 50 U/mL of penicillin and 50 µg/mL of streptomycin, inverting the filter tube into a collection tube, and spinning at 1000 × g for 1 minute. The virus titer was determined out as described above with the following exception; 500 µL of the resulting viral suspension was placed undiluted in the top row of the dilution plate without dilution.
Statistical Analyses
Bland-Altman plots were constructed and linear regression curves were fitted through the data points (GraphPad Prism version 5). Proportional error was considered when the slope of the regression curve deviated significantly (P < .05) from zero. Positive percentage agreement (PPA) and negative percentage agreement (NPA) were calculated using Microsoft Excel 2010, and Cohen’s kappa coefficient was calculated with GraphPad QuickCalcs.
RESULTS
Diagnostic Test Results of Blood Samples Treated With Sodium Dodecyl Sulfate or Triton X-100
Mean test results for 0.1% SDS-treated samples deviated from the untreated test results by ≤ 10% except for alanine transaminase (−11%) after 30 minutes. Treatment with 1% SDS profoundly affected most test results (Table 1). Mean test results for 0.1% Triton X-100–treated samples deviated from the untreated test results by ≤ 10% (Table 2). Incubation of serum with 0.1% SDS or 0.1% Triton X-100 for 30 or 60 minutes did not result in proportional errors of clinical chemistry test results.
Table 1.
Effect of 0.1% SDS and 1% Sodium Dodecyl Sulfate on Clinical Chemistry Test Results
| clinical chemistry parameter | Baseline values | 1% SDS | 0.1% SDS | ||||
|---|---|---|---|---|---|---|---|
| 0 min | 30 min | 60 min | 0 min | 30 min | 60 min | ||
| Sodium | 131–158 mmol/L | 111% (109%–114%) | 112% (110%–114%) | 112% (110%–114%) | 102% (101%–103%) | 102% (101%–102%) | 102% (101%–103%) |
| Potassium | 3.0–6.0 mmol/L | 80% (77%–83%) | 81% (78%–85%) | 81% (78%–85%) | 99% (96%–101%) | 98% (96%–99%) | 99% (97%–101%) |
| Chloride | 93–109 mmol/L | 100% (99%–100%) | 100% (99%–102%) | 100% (99%–102%) | 100% (99%–101%) | 100% (98%–100%) | 100% (99%–101%) |
| Calcium | 1.70–2.57 mmol/L | 100% (97%–105%) | 99% (95%–101%) | 100% (97%–102%) | 99% (95%–102%) | 99% (95%–105%) | 100% (97%–104%) |
| Albumin | 14–48 g/L | 25% (15%–37%) | 26% (15%–36%) | 26% (12%–39%) | 100% (93%–111%) | 99% (93%–107%) | 91% (88%–101%) |
| Total protein | 30–71 g/L | 99% (98%–104%) | 100% (98%–104%) | 100% (98%–104%) | 100% (98%–110%) | 101% (98%–100%) | 100% (97%–110%) |
| Creatinine | 51–1095 µmol/L | 97% (95%–98%) | 98% (96%–100%) | 97% (96%–98%) | 96% (95%–98%) | 96% (95%–98%) | 96% (95%–98%) |
| Urea | 1.4–48.5 mmol/L | 13% (3%–24%) | 12% (2%–16%) | 12% (2%–16%) | 96% (94%–99%) | 96% (94%–98%) | 96% (94%–98%) |
| ALT | 17–868 U/L | not detected | not detected | not detected | 91% (87%–95%) | 89% (83%–94%) | 90% (86%–93%) |
| AST | 21–700 U/L | 86% (59%–95%) | 76% (-5%–97%) | 84% (58%–98%) | 100% (97%–102%) | 98% (91%–101%) | 101% (98%–111%) |
| GGT | 17–982 U/L | 80% (68%–109%) | 74% (63%–99%) | 73% (61%–92%) | 98% (97%–101%) | 98% (97%–101%) | 98% (96%–101%) |
| ALP | 75–477 U/L | 99% (96%–105%) | 98% (96%–105%) | 98% (96%–104%) | 99% (97%–100%) | 99% (98%–101%) | 99% (97%–100%) |
| Amylase | 16–856 U/L | 98% (97%–99%) | 98% (97%–104%) | 98% (97%–99%) | 98% (95%–99%) | 98% (95%–101%) | 98% (95%–99%) |
| Uric acid | 0.24–0.90 mmol/L | 97% (95%–100%) | 98% (95%–102%) | 98% (95%–100%) | 97% (95%–99%) | 98% (95%–99%) | 98% (96%–101%) |
| CRP | 0.9–337.8 mg/L | 94% (80%–99%) | 92% (78%–99%) | 90% (78%–99%) | 97% (90%–102%) | 95% (90%–101%) | 95% (88%–101%) |
Test values of the treated samples are reported as mean percentage of the nontreated samples (recovery; ie, 100% means no difference in test result of treated samples compared with untreated samples). Range is shown within parentheses. For each parameter, 10 samples were tested. Baseline values are the range of baseline values for each analyte before inactivation procedure. Test results were corrected for the dilution factor caused by adding sodium dodecyl sulfate (SDS), and sodium test results were corrected for the amount of sodium present in SDS.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate transaminase; CRP, C-reactive protein; GGT, gamma-glutamyl transferase; SDS, sodium dodecyl sulfate.
Table 2.
Effect of 0.1% Triton X-100 on Clinical Chemistry Test Results
| clinical chemistry parameter | Baseline values | 0.1% Triton X-100 | ||
|---|---|---|---|---|
| 0 min | 30 min | 60 min | ||
| Sodium | 131–158 mmol/L | 100% (99%–100%) | 100% (99%–101%) | 100% (99%–100%) |
| Potassium | 3.0–6.0 mmol/L | 99% (98%–101%) | 99% (98%–101%) | 100% (98%–101%) |
| Chloride | 93–109 mmol/L | 99% (98%–100%) | 99% (98%–101%) | 99% (98%–101%) |
| Calcium | 1.70–2.57 mmol/L | 100% (96%–102%) | 101% (97%–105%) | 100% (96%–104%) |
| Albumin | 14–48 g/L | 98% (94%–108%) | 98% (88%–105%) | 96% (79%–105%) |
| Total protein | 30–71 g/L | 102% (99%–111%) | 102% (99%–110%) | 101% (99%–110%) |
| Creatinine | 51–1095 µmol/L | 95% (93%–98%) | 96% (95%–97%) | 97% (93%–98%) |
| Urea | 1.4–48.5 mmol/L | 97% (94%–100%) | 98% (94%–102%) | 97% (94%–99%) |
| ALT | 17–868 U/L | 97% (93%–101%) | 96% (93%–101%) | 95% (89%–99%) |
| AST | 21–700 U/L | 99% (97%–101%) | 100% (94%–106%) | 100% (98%–104%) |
| GGT | 17–982 U/L | 99% (95%–101%) | 99% (95%–100%) | 100% (99%–101%) |
| ALP | 75–477 U/L | 99% (97%–100%) | 99% (98%–101%) | 99% (97%–100%) |
| Amylase | 16–856 U/L | 100% (98%–101%) | 100% (99%–102%) | 100% (99%–101%) |
| Uric acid | 0.24–0.90 mmol/L | 98% (96%–99%) | 98% (96%–101%) | 98% (96%–101%) |
| CRP | 0.9–337.8 mg/L | 99% (96%–102%) | 98% (96%–103%) | 93% (87%–97%) |
Test values of the treated samples are reported as mean percentage of the nontreated samples (recovery; ie, 100% means no difference in test result of treated samples compared with untreated samples). Range is shown within parentheses. For each parameter, 10 samples were tested. Baseline values are the range of baseline values for each analyte before inactivation procedure. Test results were corrected for the dilution factor caused by adding Triton X-100.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate transaminase; CRP, C-reactive protein; GGT, gamma-glutamyl transferase; SDS, sodium dodecyl sulfate.
The malaria RDT relies on the capture of the malarial antigen HRP-2 (Plasmodium falciparum–specific) and the malarial antigen pLDH (pan-Plasmodium) by dye-labeled antibodies to produce a visible band on a strip of nitrocellulose. The intensities of these visible bands were slightly affected by 0.1% SDS treatment (Table 3), but this hardly affected the performance of the malaria RDT as 0.1% SDS-treated whole-blood samples provided similar results to those of untreated samples (PPA, 93.3%; NPA, 100%; Cohen’s kappa coefficient, 0.875). The intensities of the visible bands were not affected by 0.1% Triton X-100 treatment, and identical results were obtained for 0.1% Triton X-100–treated whole blood samples compared with untreated samples (PPA, 100%; NPA, 100%; Cohen’s kappa coefficient, 1).
Table 3.
Reactivity of Antigen Bands of Malaria Rapid Antigen Test for Triton and Sodium Dodecyl Sulfate Inactivated Samples
| whole blood sample dilutions | Patient 1 parasitemia 826800 trof/μL |
Patient 2 parasitemia 29400 trof/μL |
Patient 3 parasitemia 102 trof/μL |
Negative control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | 0.1% SDS | 0.1% Triton | Control | 0.1% SDS | 0.1% Triton | Control | 0.1% SDS | 0.1% Triton | Control | 0.1% SDS | 0.1% Triton | |
| Undiluted | 3+/2+ | 3+/1+ | 3+/2+ | 3+/2+ | 3+/2+ | 3+/2+ | ± / ± | ± / ± | ± / ± | -/- | -/- | -/- |
| 1:2 | 3+/1+ | 3+/1+ | 3+/1+ | 3+/2+ | 3+/2+ | 3+/2+ | ± / ± | ± / - | ± / ± | -/- | -/- | -/- |
| 1:4 | 3+/1+ | 3+/1+ | 3+/1+ | 3+/2+ | 3+/1+ | 3+/2+ | ± /± | ± / - | ± / - | -/- | -/- | -/- |
| 1:8 | 3+/1+ | 3+/± | 3+/1+ | 3+/1+ | 3+/1+ | 3+/2+ | ± / - | ± / - | ± / - | -/- | -/- | -/- |
| 1:16 | 3+/1+ | 3+/± | 3+/1+ | 3+/1+ | 3+/1+ | 3+/1+ | ± / - | -/- | ± / - | -/- | -/- | -/- |
Table shows the detection of HRP-2 antigen (Plasmodium falciparum–specific) and pLDH antigen (pan-Plasmodium), respectively, in undiluted and diluted whole blood samples from 3 P. falciparum–positive patients and 1 negative control donor using no inactivation procedure (control), 0.1% sodium dodecyl sulfate inactivation procedure, or 0.1% Triton inactivation procedure. Dilution of blood samples containing P. falciparum parasites was performed in uninfected control blood. Trof/μL is the number of P. falciparum trophozoites per microliter of whole blood. A negative test result is indicated by “-”, whereas positive test results are indicated by “±”, “1+”, “2+”, or “3+” (scale from weakly positive test to strongly positive test).
Abbreviaton: SDS, sodium dodecyl sulfate.
All 38 untreated whole blood samples were typed correctly using ABO-D CONFIRM MDmulticards. Treatment of blood samples with 0.1% SDS resulted in severe but incomplete hemolysis and weaker bands of the MDmulticard (Figure 1). Still, all 38 SDS-treated blood samples were typed correctly. Results could not be interpreted when blood samples were treated with 1% SDS (data not shown).
Figure 1.
Blood group typing using the MDmulticards ABO-D CONFIRM. The upper left panel shows the results of a representative untreated AB-positive, RhD-positive whole-blood sample. The upper right panel shows the results for the same AB-positive, RhD-positive whole-blood sample when treated with 0.1% sodium dodecul sulfate (SDS) for 1 hour. The lower left panel shows the results of a representative untreated O-positive, RhD-negative whole-blood sample. The lower right panel shows the results for the same O-positive, RhD-negative whole-blood sample when treated with 0.1% SDS for 1 hour.
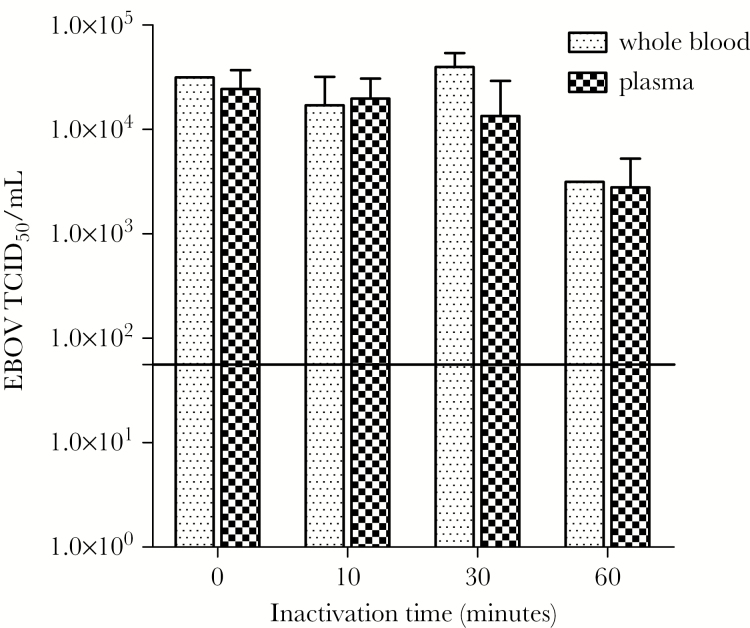
Ebola Virus Inactivation in Serum and Whole Blood From Infected Nonhuman Primates by 0.1% Sodium Dodecyl Sulfate
Serum and whole blood from 3 EBOV-infected rhesus macaques were treated with 0.1% SDS for 10, 30, and 60 minutes and were assayed for infectious EBOV titers. Initial titers of untreated serum and whole-blood samples were 2.44 × 104 TCID50/mL and 3.16 × 104 TCID50/mL, respectively. Previous studies have demonstrated that EBOV is extremely stable in blood matrix with calculated log10 reduction times of up to 20 days [25]. Treatment of serum or whole blood with 0.1% SDS for 10 minutes or 30 minutes did not significantly decrease infectious EBOV titers in the samples, and prolonging the incubation time to 60 minutes only marginally decreased infectious EBOV titers (Figure 2).
Figure 2.
Inactivation of Ebola virus (EBOV) by 0.1% sodium dodecyl sulfate (SDS) in serum and whole blood from EBOV-infected nonhuman primates (NHPs). Addition of 0.1% SDS to blood or plasma of experimentally infected NHPs had little effect on the EBOV titers when incubated at room temperature. After 60 minutes the viral titer in blood and plasma had decreased by approximately 1 log10 to 3.2 × 103 and 2.8 × 103, respectively. The initial titers of the blood and plasma were 3.2 × 104 and 2.4 × 104, respectively. The solid line represents the limit of detection of the assay (5.62 × 101). Abbreviations: EBOV, Ebola virus; TCID50, 50% Tissue Culture Infectious Dose.
Effect of Serum Concentration on Inactivation of Ebola Virus and Herpes Simplex Virus Type 1
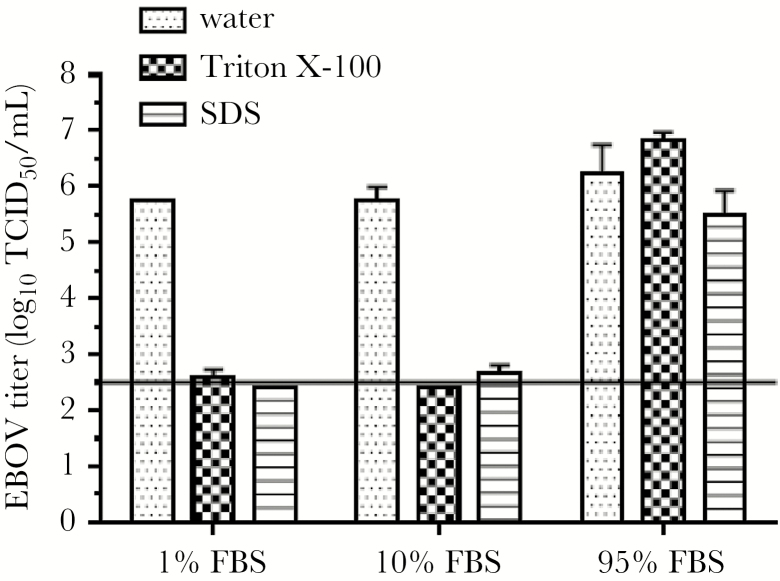
Incubation of samples with 0.1% SDS or 0.1% Triton X-100 for 1 hour reduced the infectious titer of 5.62 × 105 TCID50/mL of EBOV by more than 3 log10 when EBOV was present in medium with 1% FBS or 10% FBS (Figure 3). However, complete inactivation of EBOV was not observed: One of the 3 samples with 1% FBS contained 5.62 × 102 TCID50/mL of infectious EBOV after treatment with 0.1% Triton X-100, and 2 of the 3 samples with 10% FBS contained 5.62 × 102 TCID50/mL of infectious EBOV after treatment with 0.1% SDS. The titers of infectious EBOV in all other replicate samples were below the limit of detection (LOD) of the assay of 3.16 × 102 TCID50/mL. Treatment of 1.78 × 106 TCID50/mL of EBOV in cell culture medium containing 95% FBS with 0.1% SDS or 0.1% Triton X-100 did not result in a statistically significant reduction in EBOV titers.
Figure 3.
Inactivation of Ebola virus (EBOV) by 0.1% sodium dodecyl sulfate (SDS) and 0.1 Triton X-100 and the effect of increasing serum concentrations. Reduction in EBOV titers in culture supernatant containing various fetal bovine serum concentrations after treatment with 0.1% SDS or 0.1% Triton X-100 for 1 hour at room temperature. Ebola virus titers are presented as mean log10 TCID50/mL and standard deviation of 3 experiments. Ebola virus–containing samples spiked with water instead of detergents were used as control. The solid line represents the limit of detection of the assay. Despite rinsing with phosphate-buffered saline to remove the detergent, the first 2 rows of the titration plate demonstrated cell toxicity, resulting in the higher limit of detection. Abbreviations: EBOV, Ebola virus; FBS, fetal bovine serum; SDS, sodium dodecyl sulfate; TCID50, 50% Tissue Culture Infectious Dose.
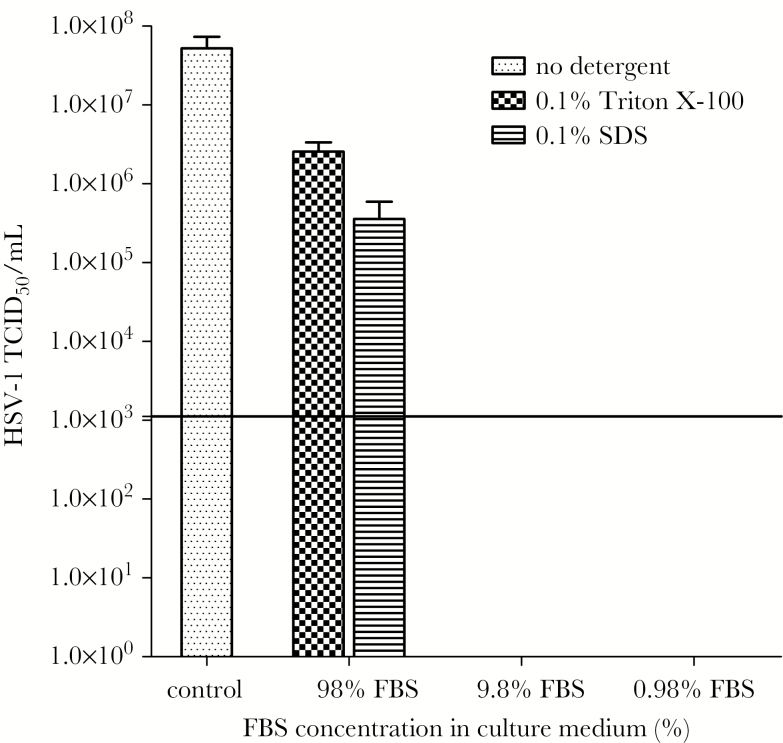
The infectious titers of 5.25 × 107 TCID50/mL of HSV-1 were reduced to below the LOD of the assay when samples containing 1% and 10% FBS were incubated with 0.1% SDS or 0.1% Triton X-100 (> 4 log10 reduction) (Figure 4). However, treatment with 0.1% Triton X-100 or 0.1% SDS reduced HSV-1 titers only by 1 log10 and 2 log10, respectively, when samples contained 98% FBS.
Figure 4.
Inactivation of herpes simplex virus type 1 (HSV-1) by 0.1% sodium dodecyl sulfate (SDS) and 0.1 Triton X-100 and the effect of increasing serum concentrations. Reduction in HSV-1 titers in culture medium containing various fetal bovine serum (FBS) concentrations after treatment with 0.1% SDS or 0.1% Triton X-100 for 1 hour at room temperature. Presented are the mean TCID50/mL titers + standard deviation (n = 3, control n = 6). Control in culture supernatant with 9.8% FBS (no detergent added). The solid line represents the limit of detection of the assay. The first rows of the titration plate demonstrated cell toxicity due to residual detergent present in the samples, resulting in the higher limit of detection. Abbreviations: FBS, fetal bovine serum; HSV-1, herpes simplex virus type 1; SDS, sodium dodecyl sulfate; TCID50, 50% Tissue Culture Infectious Dose.
DISCUSSION
During the Ebola outbreak in West Africa, blood work-up was difficult due to lack of protocols for safe handling of specimens outside high-containment facilities. Some recommend that HFV in blood samples be inactivated with detergents prior to diagnostic testing, although validation of this procedure is lacking [9, 11–15]. This prompted us to study the effect of detergents on diagnostic test results, as well as on EBOV inactivation. Our results show that 0.1% SDS does not affect diagnostic test results in contrast with 1% SDS. In addition, in line with previous reports, we show that treatment of serum samples with 0.1% Triton X-100 is compatible with reliable clinical chemistry testing and malaria antigen detection [9, 11–15]. However, 0.1% SDS treatment of plasma and whole blood from EBOV-infected NHPs did not inactivate EBOV. These results were unexpected in view of published literature reporting that SDS at concentrations ≤ 0.1% completely inactivated the enveloped viruses human immunodeficiency virus type 1, herpes simplex virus, hepatitis C virus, and vesicular stomatitis virus, as well as some nonenveloped DNA viruses [17–21]. A clear difference in methodology between these studies and ours is that virus inactivation protocols were validated with samples in which serum concentration was < 10%, whereas we used serum, plasma, and whole-blood samples as well as samples with lower serum concentrations. Our results show that treatment with 0.1% Triton X-100 or 0.1% SDS inactivates enveloped viruses in samples containing low serum concentrations, whereas virus inactivation is annulled at physiological serum concentration.
The American Society for Testing and Materials (ASTM International) recommends that if a soil load is required to demonstrate virucidal activity of test substances with viruses in suspension, 5% bovine serum can be added to the virus suspension or a tripartite mixture resembling the protein content in 5% serum [26]. We show that validation of virucidal activities in this way cannot be extrapolated to whole-blood, plasma, and serum samples, and this methodology should not be used to validate inactivation protocols for HFV. This is in line with the World Health Organization guideline on viral safety testing of blood products, which recommends for virus inactivation experiments that the virus spike should not alter the characteristics of human blood plasma products, and typically a spike of 5%–10% of the total volume is used [27].
The novelty of this study is that validation of virus inactivation protocols was tested with plasma and whole blood from EBOV-infected NHPs, enabling us to draw conclusions on whether detergent treatment of blood samples prior to diagnostic testing would inactivate EBOV in real-life settings. We did not include other HFVs in this study, but similar results were found for HSV-1. This implies that our findings can be extrapolated to other enveloped viruses such as HFV. A downside of this study is that we were not able to pinpoint which component(s) in serum annulled virus inactivation. It is tempting to speculate that the high lipid and/or protein content in serum and whole blood acts as scavenger for detergents, thereby annulling virus inactivation, but further research is warranted.
In conclusion, treatment of whole blood and serum samples with 0.1% SDS or Triton X-100 does not inactivate HFV, and this procedure cannot be used to provide safe diagnostic testing for clinical decision making. Hemorrhagic fever virus inactivation protocols should be validated with serum and whole-blood samples.
Notes
Acknowledgments. The authors are grateful to Andrea Marzi (National Institute of Allergy and Infectious Diseases [NIAID], National Institutes of Health [NIH]) for providing the nonhuman primate samples.
Financial support. P. L. A. F., M. P. G. K., and M. D. d. J. received funding from EU FP7 project PREPARE (602525). The study was funded in part by the Intramural Research Program of the NIAID, NIH.
Potential conflicts of interest. P. L. A. F. reports grants from EU FP7 project PREPARE (602525) during the conduct of the study and personal fees from Speakers Fee GSK outside the submitted work. M. P. G. K. reports other than from Erasmus MC, grants from the European Union and the Dutch government, outside the submitted work. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Hunt L, Gupta-Wright A, Simms V et al. . Clinical presentation, biochemical, and haematological parameters and their association with outcome in patients with Ebola virus disease: an observational cohort study. Lancet Infect Dis 2015; 15:1292–9. [DOI] [PubMed] [Google Scholar]
- 2. Bah EI, Lamah MC, Fletcher T et al. . Clinical presentation of patients with Ebola virus disease in Conakry, Guinea. N Engl J Med 2015; 372:40–7. [DOI] [PubMed] [Google Scholar]
- 3. Chertow DS, Kleine C, Edwards JK, Scaini R, Giuliani R, Sprecher A. Ebola virus disease in West Africa—clinical manifestations and management. N Engl J Med 2014; 371:2054–7. [DOI] [PubMed] [Google Scholar]
- 4. Leligdowicz A, Fischer WA 2nd, Uyeki TM et al. . Ebola virus disease and critical illness. Crit Care 2016; 20:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Uyeki TM, Mehta AK, Davey RT Jr et al. ; Working Group of the U.S.–European Clinical Network on Clinical Management of Ebola Virus Disease Patients in the U.S. and Europe Clinical management of Ebola virus disease in the United States and Europe. N Engl J Med 2016; 374:636–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elliott LH, McCormick JB, Johnson KM. Inactivation of Lassa, Marburg, and Ebola viruses by gamma irradiation. J Clin Microbiol 1982; 16:704–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Warfield KL, Swenson DL, Olinger GG et al. . Ebola virus inactivation with preservation of antigenic and structural integrity by a photoinducible alkylating agent. J Infect Dis 2007; 196(suppl 2):S276–83. [DOI] [PubMed] [Google Scholar]
- 8. Mitchell SW, McCormick JB. Physicochemical inactivation of Lassa, Ebola, and Marburg viruses and effect on clinical laboratory analyses. J Clin Microbiol 1984; 20:486–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hersberger M, Nusbaumer C, Scholer A, Knöpfli V, von Eckardstein A. Influence of practicable virus inactivation procedures on tests for frequently measured analytes in plasma. Clin Chem 2004; 50:944–6. [DOI] [PubMed] [Google Scholar]
- 10. Chong YK, Ng WY, Chen SP, Mak CM. Effects of a plasma heating procedure for inactivating Ebola virus on common chemical pathology tests. Hong Kong Med J 2015; 21:201–7. [DOI] [PubMed] [Google Scholar]
- 11. Mifsud A, Peelen D, Brincat P et al. . A feasibility study on the effects of Triton X-100 for the in vitro inactivation of Ebola virus on haematological assays. J Clin Pathol 2016; 69:637–42. [DOI] [PubMed] [Google Scholar]
- 12. Loutfy MR, Assmar M, Hay Burgess DC, Kain KC. Effects of viral hemorrhagic fever inactivation methods on the performance of rapid diagnostic tests for Plasmodium falciparum. J Infect Dis 1998; 178:1852–5. [DOI] [PubMed] [Google Scholar]
- 13. Tempestilli M, Pucci L, Notari S et al. . Diagnostic performances of clinical laboratory tests using Triton X-100 to reduce the biohazard associated with routine testing of Ebola virus–infected patients. Clin Chem Lab Med 2015; 53:1967–73. [DOI] [PubMed] [Google Scholar]
- 14. Mabey D, Gill G, Parry E, Weber MW, Whitty CJM, eds. Principles of Medicine in Africa. 4th ed, Table 34.3. Cambridge, UK: Cambridge University Press, 2013. [Google Scholar]
- 15. Warrell DA, Cox TM, Firth JD, Török E, eds. Oxford Textbook of Medicine: Infection. 5th ed, Table 5.17.1. Oxford, UK; Oxford University Press, 2012. [Google Scholar]
- 16. Centers for Disease Control and Prevention. Update: management of patients with suspected viral hemorrhagic fever—United States. MMWR Morb Mortal Wkly Rep 1995; 44:475–9. [PubMed] [Google Scholar]
- 17. Krebs FC, Miller SR, Malamud D, Howett MK, Wigdahl B. Inactivation of human immunodeficiency virus type 1 by nonoxynol-9, C31G, or an alkyl sulfate, sodium dodecyl sulfate. Antiviral Res 1999; 43:157–73. [DOI] [PubMed] [Google Scholar]
- 18. Howett MK, Neely EB, Christensen ND et al. . A broad-spectrum microbicide with virucidal activity against sexually transmitted viruses. Antimicrob Agents Chemother 1999; 43:314–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gong Y, Wen A, Cheung D, Wong M, Sacks SL. Preclinical evaluation of docusate as protective agent from herpes simplex viruses. Antiviral Res 2001; 52:25–32. [DOI] [PubMed] [Google Scholar]
- 20. Song H, Li J, Shi S, Yan L, Zhuang H, Li K. Thermal stability and inactivation of hepatitis C virus grown in cell culture. Virol J 2010; 7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zimmer B, Summermatter K, Zimmer G. Stability and inactivation of vesicular stomatitis virus, a prototype rhabdovirus. Vet Microbiol 2013; 162:78–84. [DOI] [PubMed] [Google Scholar]
- 22. Haddock E, Feldmann F, Feldmann H.. Efficacy testing of inactivation methods for filoviruses. Joint conference of “German symposium on zoonosis research 2014” and “7th international conference on emerging zoonosis”, 2014:82, Berlin, Germany https://www.google.nl/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0ahUKEwjJ1NmD1JfWAhVJa1AKHQxgDioQFggoMAA&url=https%3A%2F%2Fwww.zoonosen.net%2FDesktopmodules%2FBring2Mind%2FDMX%2FDownload.aspx%3FEntryId%3D26011%26PortalId%3D24&usg=AFQjCNGhEgXg18BOp8eOcIzdf92YqFMuvg. [Google Scholar]
- 23. Shin SY, Kwon KC, Koo SH et al. . Evaluation of two automated instruments for pre-transfusion testing: AutoVue Innova and Techno TwinStation. Korean J Lab Med 2008; 28:214–20. [DOI] [PubMed] [Google Scholar]
- 24. Marzi A, Hanley PW, Haddock E, Martellaro C, Kobinger G, Feldmann H. Efficacy of vesicular stomatitis virus-Ebola virus postexposure treatment in rhesus macaques infected with Ebola virus Makona. J Infect Dis 2016; 214:360–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fischer R, Judson S, Miazgowicz K, Bushmaker T, Prescott J, Munster VJ. Ebola virus stability on surfaces and in fluids in simulated outbreak environments. Emerg Infect Dis 2015; 21:1243–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Standard designation E1052-11. Standard Test Method to Assess the Activity of Microbicides against Viruses in Suspension. West Conshohocken: ASTM International, 2011.
- 27. Guidelines on viral inactivation and removal procedures intended to assure the viral safety of human blood plasma products. In: WHO Expert Committee on Biological Standardization: fifty-second report (Annex 4, WHO Technical Report Series, No. 924). Geneva: World Health Organization, 2004. http://www.who.int/bloodproducts/publications/WHO_TRS_924_A4.pdf. Accessed 9 September 2017.