Abstract
Objective:
To evaluate whether there are significant differences between contrast-enhanced fat-saturated T1 weighted imaging and non-enhanced fat-suppression imaging for diagnosing sacroiliitis in patients with inflammatory back pain.
Methods:
92 patients, consisting of 46 males and 46 females (mean age: 34 years; range: 15–63 years), who met at least 4 out of 5 Assessment in SpondyloArthritis international Society criteria for inflammatory low back pain were enrolled in this study. All patients underwent MRI consisting of a coronal short tau inversion recovery (STIR) sequence, axial fat-saturated T2 weighted imaging (T2FS), and coronal and axial contrast-enhanced fat-saturated T1 weighted imaging (c & a T1CE). Two observers independently reviewed an image set of coronal STIR with axial T2FS, and an image set of c & a T1CE, at separate times. The degree of bone marrow edema and osteitis was evaluated from each image set. A decision for sacroiliitis positivity for each image set was made based on the findings. The presence of additional active inflammatory findings of spondyloarthropathy such as synovitis, enthesitis and capsulitis were also evaluated.
Results:
Interobserver and intersequence agreement for the degree of bone marrow edema and osteitis were good or excellent in all quadrants. Cohen’s kappa coefficients for sacroiliitis positivity between the two observers were 0.978 and 0.956, and Cohen’s kappa coefficients between the two image sets for each observer were 0.892 and 0.870, respectively. The intersequence agreement of additional active inflammatory findings was substantial, and the interobserver agreement was almost perfect or substantial.
Conclusion:
STIR with T2FS image is comparable to T1CE image for diagnosing spondyloarthropathy. T1CE images may have a role in evaluating additional active inflammatory findings of spondyloarthropathy such as synovitis, enthesitis and capsulitis.
Advances in knowledge:
Coronal STIR with axial T2FS may be sufficient for diagnosis spondyloarthropathy without use of contrast administration.
INTRODUCTION
Early detection of active sacroiliitis in patients with suspected spondyloarthropathy is important because early treatment can improve the course of immunologically mediated diseases.1 The diagnosis of spondyloarthropathy mainly depends on clinical findings associated with laboratory and image findings.2–4 Accordingly, a new classification criteria proposed by the Assessment in SpondyloArthritis international Society (ASAS) in 2009 includes MRI as one of two arms for classification of axial spondyloarthropathy.5 These classification criteria consist of an imaging arm and a clinical arm. To meet the criteria of the imaging arm, positivity for sacroiliitis on MRI or plain radiographs in addition to at least one feature of spondyloarthropathy is needed. To meet the criteria of the clinical arm, HLA-B27 positivity and at least two other features of spondyloarthropathy are needed.6
The MRI sequence short tau inversion recovery (STIR) or T1 weighted images after administration of the contrast agent can be used for evaluation of bone marrow edema or osteitis. Most studies on the diagnostic value of MRI sequence in sacroiliitis have used the oblique coronal plane only.5,7–9 However, the axial plane, perpendicular to the oblique coronal plane, provides obvious advantages as it allows visualization of the ventral and dorsal margins of the cartilaginous portion of the joint and characterization of the ligamentous portion of the sacroiliac joint (SIJ).10–13 Both fat-saturated T2 weighted image (T2FS) and STIR are useful for evaluation of bone marrow edema. Each sequence has its advantages and both sequences are complementary to each other. According to our knowledge, there was no study in the literature comparing coronal STIR combined with axial T2FS and T1CE in diagnosing axial spondyloarthropathy.
The aim of this study was to evaluate whether there are significant differences between coronal STIR with axial T2FS and coronal and axial contrast enhanced fat-saturated T1 weighted image (c & a T1CE) in diagnosing sacroiliitis in patients with inflammatory back pain (IBP). An additional purpose was to determine the value of contrast-enhanced study for evaluation of active sacroiliitis.
METHODS AND MATERIALS
Study population
This retrospective study was approved by our institutional review board, and informed consent for enrollment was waived. From January 2012 to December 2015, 105 patients at our rheumatology and rehabilitation medicine outpatient clinic presenting with IBP underwent sacrum MRI under the impression of spondyloarthropathy. In all cases, patients had no previous history of spondyloarthropathy evaluation. Four of the following five ASAS International Society criteria for inflammatory low back pain had to be fulfilled for IBP: onset of symptoms before the age of 40, insidious onset, improvement with exercise, no improvement with rest and pain at night with improvement on getting up.14 Twelve patients finally diagnosed with degenerative osteoarthritis of SIJs were excluded from the study. One patient diagnosed with infectious sacroiliitis was also excluded. Finally, 92 patients were enrolled into this study (46 males and 46 females; mean age: 34 years; range: 15–63 years).
MRI examinations
MRI was performed using a 3 T unit (Achieva, Philips Healthcare, Best, the Netherlands; Ingenia, Philips Healthcare, Best, the Netherlands; Magnetom Skyra, Siemens Healthcare, Erlangen, Germany). Imaging was performed with the patient in the supine position using a high-resolution body phased-array coil. Acquired sequences are as follows:
Coronal short tau inversion recovery sequence (TR = 3900–5300 ms, TE = 70–80 ms, section thickness = 4 mm, intersection gap = 0.4 mm, field of view = 250 mm, matrix = 208–332 × 205–252, echo train length = 15, excitation number = 1)
Axial T2 weighted sequence with fat-saturation (TR = 3300–5200 ms, TE = 80 ms, section thickness = 5 mm, intersection gap = 1 mm, field of view = 250 mm, matrix = 380–500 × 250–300, echo train length = 15, excitation number = 1)
Axial T1 weighted sequence with fat-saturation after contrast administration (TR = 500–700 ms, TE = 10–20 ms, section thickness = 5 mm, intersection gap = 1 mm, field of view = 250 mm, matrix = 300–500 × 200–256, echo train length = 3, excitation number = 1)
Coronal T1 weighted sequence with fat-saturation after contrast administration (TR = 500–700 ms, TE = 15–25 ms, section thickness = 4 mm, intersection gap = 0.4 mm, field of view = 250 mm, matrix = 300–500 × 200–256, echo train length = 3, excitation number = 1).
Coronal images were taken in the oblique coronal plane which was oriented along the long axis of the sacral bone, and axial images were taken in the oblique axial plane which is perpendicular to the oblique coronal plane.
Image analysis and scoring
Two radiologists evaluated the imaging studies independently. Analyses were performed by a fourth-year radiology resident (observer 1) and by a musculoskeletal radiologist (observer 2) with 11 years of experience in the interpretation of sacrum MRI; both were blinded to the diagnoses. Presence of bone marrow edema was defined as depiction of a hyperintense signal on coronal STIR image or axial T2FS, and presence of osteitis was defined as a hyperintense signal on coronal or axial contrast-enhanced fat-saturated T1 weighted images (T1CE), according to the ASAS/Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) working group definition.5 For analysis, each SI joint was divided into four quadrants based on the coronal image (Figure 1), and the Hermann-Braun scoring system was used for the evaluation of active sacroiliitis.9,15 The reference line dividing upper and lower quadrants at the ilium and sacrum was drawn on the oblique coronal section, which cuts the mid portion of both SI joints. The line was parallel to the end plate of the L5 vertebral body, and the level of the reference line was half of synovial SI joint. Each quadrant was graded with an activity score from 0 to 4; Grade 0: no inflammatory changes or subtle subchondral signal change; Grade 1: linear or dotty subchondral signal change along the joint (signal intensity changes confined to the joint space or the joint capsule); Grades 2–4: bone marrow edema of para-articular bone marrow involving 33%, 34–66%, or over 66% of the quadrant area, respectively.9 Coronal STIR and axial T2FS were analysed as an image set for the evaluation of bone marrow edema. Axial and coronal images of T1CE were analysed as another image set for the evaluation of osteitis. Bone marrow edema and osteitis were evaluated separately. In cases in which the results of axial and coronal images were not concordant, the greater score was taken as the result. Before reviewing images, each reader was shown five example cases to establish the grading scale. These examples were not included in the analysis of this study.
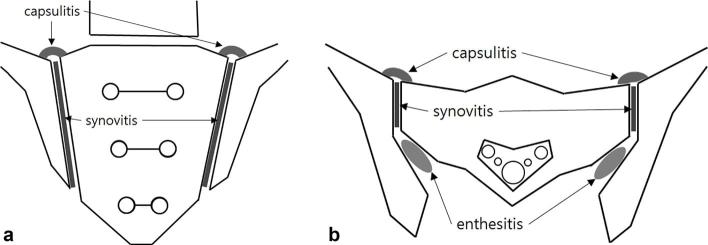
Figure 1.
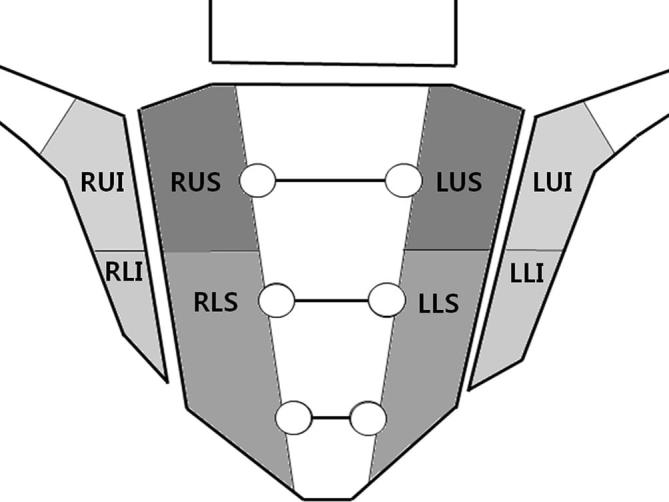
MRI grading of bone marrow edema/osteitis—H/B score. Each sacroiliac joint (SIJ) was divided into 4 quadrants and the severity of inflammatory changes in each quadrant was assigned a score of 0–4. H/B, Hermann-Braun; SIJ, sacroiliac joint.
As the ASAS/OMERACT working group definition, findings of MRI were considered as positive for sacroiliitis when at least one lesion was present in at least two consecutive slices, or when at least two lesions were found in one slice.5,8
Both radiologists determined the presence of additional active inflammatory findings based on coronal STIR with axial T2FS images and c & a T1CE images. Only bone marrow edema on STIR or osteitis on contrast enhanced sequence is considered for the definition of active sacroiliitis according to the ASAS/OMERACT consensus.5,12 Therefore, we defined synovitis, enthesitis and capsulitis as additional active inflammatory findings of spondyloarthropathy in this study (Figure 2). The ASAS/OMERACT working group definition was used for these additional active inflammatory findings.5 Depiction of a hyperintense signal on coronal STIR with axial T2FS or c & a T1CE images at sites where ligaments and tendons attach to bone was defined as enthesitis on each coronal SITR with axial T2FS or c & a T1CE images. Synovitis was defined as hyperintense signal in the synovial portion within the SIJ. Capsulitis was defined as hyperintense signal around the anterior or posterior SIJ capsule. Hyperintense signal on c & a T1CE was defined as similar to blood vessel,5 and on coronal STIR with axial T2FS was defined as hyperintense signal not considered normal joint fluid. Additional active inflammatory findings were evaluated on each side, left and right joint, and quadrants were not used.
Figure 2.
Enthesitis, synovitis and capsulitis. (a, b) Enthesitis was defined as depiction of a hyperintense signal at sites where ligaments and tendons attach to bone (interosseous ligament). Synovitis and capsulitis were defined as hyperintense signal at the synovial or capsular portions of the SIJ, respectively. SIJ, sacroiliac joint.
Statistical analysis
All statistical analyses were performed with SPSS 22.0 software (SPSS, Chicago, IL). Cohen’s kappa coefficient was calculated to determine the concordance of positivity of sacroiliitis. For analysis, we defined interobserver agreement and intersequence agreement. Interobserver agreement was agreement between two observers on the same image set. Intersequence agreement was agreement between coronal STIR with axial T2FS and c & a T1CE images for each observer. The interobserver and intersequence agreement of scores of each quadrant were determined by intraclass correlation coefficients (ICCs). Cohen’s kappa coefficient was calculated for interobserver and intersequence agreement of the result of positivity for sacroiliitis. Cohen’s kappa coefficient was also calculated for interobserver and intersequence agreement of the result of additional active inflammatory findings of each joint. Interobserver and intersequence agreement were considered less than chance agreement when κ was less than 0 (κ < 0), slight agreement when 0.01 < κ < 0.20, fair agreement when 0.20 ≤ κ < 0.40, moderate agreement when 0.40 ≤ κ < 0.60, substantial agreement when 0.60 ≤ κ < 0.80, and almost perfect agreement when 0.81 < κ < 0.99.16 For the ICC, agreement was considered as poor when ICC < 0.5, moderate when 0.5 ≤ ICC < 0.75, good when 0.75 ≤ ICC < 0.9 and excellent when 0.9 ≤ ICC.17–19
RESULTS
Among the 92 patients included in this study, 72 patients (78%) had positive HLA-B27. According to the ASAS classification criteria, 57 patients (62.0%) were diagnosed as an axial spondyloarthropathy. Among the 57 patients, 22 patients (38.6%) had radiographic changes and could be diagnosed as ankylosing spondylitis by modified New York criteria, and the other 35 patients (61.4%) had non-radiographic spondyloarthropathy. Three patients (3.3%) were diagnosed as osteitis condensans ilii, and 32 patients (34.8%) had non-specific lower back pain, clinically.
Interobserver agreement for both image sets were good or excellent in all quadrants (0.878 < ICC <0.964) (Figure 3) (Table 1). Intersequence agreement were also good or excellent for both observers in all quadrants (0.781 < ICC <0.914) (Table 1). Of note, ICCs for interobserver agreement were higher than the ICCs for intersequence agreement. Considering the disparity of experience of the two observers in this study, this result suggests constant interpretation, regardless of experience, would be possible. Except for the result in the left lower sacrum from observer 1, the ICC for intersequence agreement was greater than 0.8. The interobserver agreements of positivity for sacroiliitis were almost perfect for coronal STIR with axial T2FS (κ = 0.978) and for c & a T1CE images (κ = 0.956) (Table 2). The intersequence agreement of positivity for sacroiliitis were also nearly perfect for both radiologists (κ = 0.870 and 0.891) (Table 2).
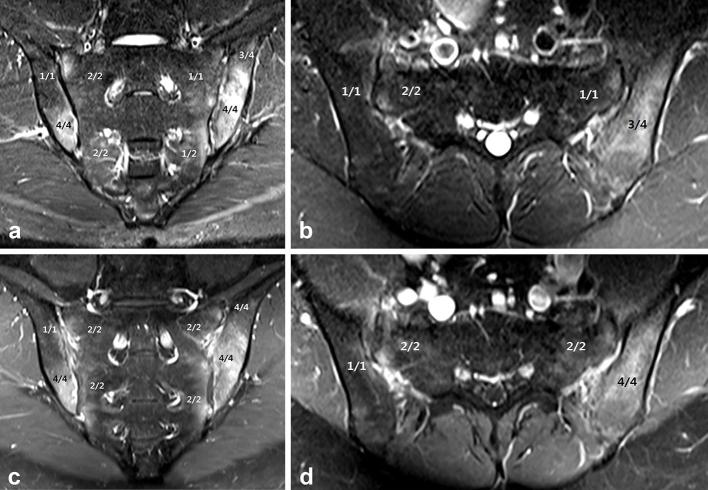
Figure 3.
Spondyloarthropathy in a 26-year-old male. (a, b) Coronal short tau inversion recovery (STIR) imaging shows increased signal intensity at the right lower and left upper and lower ilium. The area of involvement is considered more than two-thirds at the right lower and left upper and lower ilium (Grade 4). Axial T2FS imaging shows increased signal intensity at the left upper ilium (Grade 4). Except for the left upper sacrum, increased signal intensities at the bilateral sacrum involving less than one-third the area are seen (Grade 2). Linear increased signal intensity at the left upper sacrum is seen (Grade 1). (c, d) Coronal T1CE imaging of the same patient shows increased signal intensity and similar patterns to STIR imaging. However, the area of involvement at the left upper sacrum is larger than on STIR imaging (Grade 2). Synovitis and enthesitis are more prominent on T1CE compared with STIR with T2FS.
Table 1.
Intraclass correlation coefficient for interobserver agreement and intersequence agreement of grading scores of each quadrant
| Quadrant | Interobserver agreement | Intersequence agreement | ||
|---|---|---|---|---|
| STIR & T2FS | T1CE | Observer 1 | Observer 2 | |
| RUS | 0.924 | 0.907 | 0.884 | 0.855 |
| RLS | 0.903 | 0.916 | 0.849 | 0.867 |
| RLI | 0.964 | 0.942 | 0.889 | 0.893 |
| RUI | 0.937 | 0.952 | 0.868 | 0.825 |
| LUS | 0.880 | 0.919 | 0.822 | 0.879 |
| LLS | 0.878 | 0.920 | 0.781 | 0.840 |
| LLI | 0.882 | 0.918 | 0.864 | 0.857 |
| LUI | 0.941 | 0.904 | 0.882 | 0.914 |
LLI, left lower ilium; LLS, left lower sacrum; LUI, left upper ilium; LUS, left upper sacrum; RLI, right lower ilium; RLS, right lower sacrum; RUI, right upper ilium; RUS, right upper sacrum; STIR, short tau inversion recovery; T1CE, contrast-enhanced fat-saturated T1 weighted imaging; T2FS, fat-saturated T2weighted imaging.
Table 2.
Cohen’s kappa coefficient for interobserver agreement of positivity for sacroiliitis for both image sets and intersequence agreement of positivity for sacroiliitis for both observers
| κ | |
|---|---|
| STIR & T2FS | 0.978 |
| T1CE | 0.956 |
| Observer 1 | 0.891 |
| Observer 2 | 0.870 |
STIR, short tau inversion recovery; T1CE, contrast-enhanced fat-saturated T1 weighted imaging; T2FS, fat-saturated T2 weighted imaging.
Analysis of additional active inflammatory findings of spondyloarthropathy including synovitis, enthesitis and capsulitis is as follows: Intersequence agreements of synovitis and enthesitis were moderate at both right and left SI joints (0.330 < κ < 0.569) (Table 3). Intersequence agreements of capsulitis were substantial at both SI joints (0.612 < κ < 0.796) (Table 3). Interobserver agreements for synovitis, enthesitis and capsulitis were substantial or almost perfect (0.733 < κ < 0.950) (Table 3). Cohen’s kappa coefficients for the intersequence agreement of capsulitis were relatively high compared with those of synovitis and enthesitis.
Table 3.
Cohen’s kappa coefficient for interobserver agreement and intersequence agreement of additional active inflammatory findings
| Interobserver agreement | Intersequence agreement | ||||
| STIR & T2FS | T1CE | Observer 1 | Observer 2 | ||
| Synovitis | Right SIJ | 0.783 | 0.867 | 0.498 | 0.569 |
| Left SIJ | 0.832 | 0.780 | 0.498 | 0.476 | |
| Capsulitis | Right SIJ | 0.950 | 0.742 | 0.612 | 0.796 |
| Left SIJ | 0.897 | 0.793 | 0.614 | 0.731 | |
| Enthesitis | Right SIJ | 0.733 | 0.822 | 0.330 | 0.461 |
| Left SIJ | 0.822 | 0.785 | 0.371 | 0.374 | |
SIJ, sacroiliac joint; STIR, short tau inversion recovery; T1CE, contrast-enhanced fat-saturated T1 weighted imaging; T2FS, fat-saturated T2 weighted imaging.
DISCUSSION
This study was conducted to evaluate the role of contrast agent administration on MRI for the evaluation of sacroiliitis. In the advanced stage of spondyloarthropathy, especially in ankylosing spondylitis, typical bilateral and symmetric structural abnormalities of SIJs can be detected on plain radiograph. MRI serves an important role in diagnosis of spondyloarthropathy by facilitating early detection of small or unilateral abnormalities of SIJs regarding spondyloarthropathy. Indeed, the latest classification criteria for axial spondyloarthropathy proposed by ASAS in 2009 suggest MRI as one of the two major arms for diagnosis.
Several studies have emphasized the lack of utility of contrast agents in evaluating sacroiliitis. However, most of these studies have used only the coronal plane in their evaluation.8,9,20–23In some of these studies, an axial scan was also taken for contrast enhanced T1weighted image, but in both cases, a concrete method for interpretation of osteitis using both coronal and axial images were not described.20,22 This approach (or any approach that employs only coronal or only axial images) is vulnerable to partial volume artefacts. We therefore used both coronal and axial images in the present study.
Additionally, we used coronal STIR with axial T2FS imaging in this study. Fat-saturated images are good at visualizing small anatomic details, but possibly accompany inhomogeneity of the image, which is exacerbated in cases using surface coil. In contrast, STIR imaging is insensitive to magnetic field inhomogeneity but has low signal-to-noise ratio.24 We expected that the two sequences could complement each other, and therefore used them both for interpretation.
The Cohen’s kappa coefficients calculated in this study suggest two ideas. Both observers showed almost perfect intersequence agreement on the positivity of sacroiliitis on MRI (κ = 0.870 and 0.891). Additionally, interobserver agreement on the positivity of sacroiliitis was also almost perfect for both image sets (κ = 0.978 and 0.956). These results suggest that the positivity of sacroiliitis on coronal STIR with axial T2FS is reproducible and comparable with the results of contrast-enhanced study in evaluating spondyloarthropathy on MRI. Furthermore, ICC showed good or excellent intersequence and interobserver agreements in all quadrants. These results suggest quantification of the degree of bone marrow edema and osteitis are relatively well-correlated. Furthermore, evaluation of bone marrow edema and osteitis could be performed regardless of experience. These results suggest that usage of contrast media could be omitted for the diagnosis of spondyloarthropathy on MRI.
In contrast to previous studies, this study used both coronal STIR and axial T2FS, and found results in better agreement.8,9,20–22This suggests that use of axial T2FS with coronal STIR could be more reliable than using coronal STIR alone. However, there are many remaining obstacles for the additional active inflammatory findings assessed in this study. All additional active inflammatory findings showed poor Cohen’s kappa coefficients for intersequence agreement but were relatively good for interobserver agreement. We interpreted synovitis as increased signal in the synovial joint that seemed not to be caused from synovial joint fluid or blood vessels on coronal STIR and axial T2FS images. This definition is rather objective, so reliable differentiation between true inflammation and normal joint fluid is tricky in many cases.9 Additionally, blood vessels are seen as signal void on T2FS or STIR and seen inconstantly on T1CE which is possibly misinterpreted as inflammation. There are normal blood vessels surrounding the SI joint.12 Furthermore, there is discrepancy in signal intensity of cartilage between T2 weighted image and T1CE; cartilage shows delayed enhancement after several hours of contrast injection, so usually a low signal intensity on T1CE is seen whereas, cartilage shows high signal intensity on T2 weighted image.25,26 These factors may contribute to the poor intersequence agreement for the active inflammatory findings assessed in this study.
Cohen’s kappa coefficients for the intersequence agreement of capsulitis were relatively higher compared with those of synovitis and enthesitis. The capsular portion of the SIJ has blood vessels, but no joint fluid or cartilage. These factors may be attributed to the relatively good intersequence agreement.
We defined synovitis, enthesitis and capsulitis as additional active inflammatory findings. These findings do not heavily affect establishing a diagnosis of spondyloarthropathy on MRI but could be used for response grading after treatment. After appropriate treatment, overall inflammatory processes in the SI joint subside, including additional active inflammatory findings. In this study, agreements of additional active inflammatory findings between sequences were not good, suggesting that T1CE and coronal STIR with axial T2FS cannot replace each other. Rather, each study may have a distinct role in evaluating response to treatment. Some studies have reported that contrast enhancement is more sensitive for synovitis compared with the T2FS or STIR images.8,20,21
Besides the retrospective nature of our study, there are several limitations in this study. First, due to complex diagnostic criteria of spondyloarthropathy, with MRI finding itself serving a major role for establishing diagnosis of spondyloarthropathy and absence of a single reference standard for confirming diagnosis (such as histologic evaluation), we could not evaluate diagnostic performance. This study was specifically designed to evaluate whether STIR with T2FS without contrast study could replace c & a T1CE. We therefore analysed positivity for sacroiliitis and agreement of grading for bone marrow edema and osteitis. Second, additional active inflammatory findings of spondyloarthropathy such as synovitis, capsulitis and enthesitis were not quantitatively analysed. Only presence was evaluated not using grading scale. Further studies will be needed to address these limitations.
In conclusion, STIR with T2FS is sufficient to diagnosing spondyloarthropathy, and contrast enhancement is not necessary. T1CE images may have a role in evaluating additional active inflammatory findings such as synovitis, enthesitis and capsulitis.
Contributor Information
Siyoun Sung, Email: asterism35@naver.com.
Hyun Su Kim, Email: calmuri@naver.com.
Jong Won Kwon, Email: jwjwkwon@gmail.com.
REFERENCES
- 1.Braun J, Sieper J, Bollow M. Imaging of sacroiliitis. Clin Rheumatol 2000; 19: 51–7. [DOI] [PubMed] [Google Scholar]
- 2.Dougados M. Diagnosis and monitoring of spondyloarthropathy. Compr Ther 1998; 24590–5. [PubMed] [Google Scholar]
- 3.Zhang P, Yu KH, Guo RM, Ran J, Liu Y, Morelli J, et al. Comparing the diagnostic utility of sacroiliac spectral CT and MRI in axial spondyloarthritis. Br J Radiol 2016; 89: 20150196https://doi.org/10.1259/bjr.20150196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vendhan K, Bray TJ, Atkinson D, Punwani S, Fisher C, Sen D, et al. A diffusion-based quantification technique for assessment of sacroiliitis in adolescents with enthesitis-related arthritis. Br J Radiol 2016; 89: 20150775https://doi.org/10.1259/bjr.20150775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudwaleit M, Jurik AG, Hermann KG, Landewé R, van der Heijde D, Baraliakos X, et al. Defining active sacroiliitis on magnetic resonance imaging (MRI) for classification of axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI group. Ann Rheum Dis 2009; 68: 1520–7.https://doi.org/10.1136/ard.2009.110767 [DOI] [PubMed] [Google Scholar]
- 6.van Tubergen A, Weber U. Diagnosis and classification in spondyloarthritis: identifying a chameleon. Nat Rev Rheumatol 2012; 8: 253–61.https://doi.org/10.1038/nrrheum.2012.33 [DOI] [PubMed] [Google Scholar]
- 7.Algin O, Gokalp G, Baran B, Ocakoglu G, Yazici Z. Evaluation of sacroiliitis: contrast-enhanced MRI with subtraction technique. Skeletal Radiol 2009; 38: 983–8.https://doi.org/10.1007/s00256-009-0723-9 [DOI] [PubMed] [Google Scholar]
- 8.van Onna M, van Tubergen A, van der Heijde D, Jurik AG, Landewé R. Gadolinium contrast-enhanced MRI sequence does not have an incremental value in the assessment of sacroiliitis in patients with early inflammatory back pain by using MRI in combination with pelvic radiographs: a 2-year follow-up study. Clin Exp Rheumatol 2014; 32: 225–30. [PubMed] [Google Scholar]
- 9.Althoff CE, Feist E, Burova E, Eshed I, Bollow M, Hamm B, et al. Magnetic resonance imaging of active sacroiliitis: do we really need gadolinium? Eur J Radiol 2009; 71: 232–6.https://doi.org/10.1016/j.ejrad.2009.04.034 [DOI] [PubMed] [Google Scholar]
- 10.Puhakka KB, Melsen F, Jurik AG, Boel LW, Vesterby A, Egund N. MR imaging of the normal sacroiliac joint with correlation to histology. Skeletal Radiol 2004; 33: 15–28.https://doi.org/10.1007/s00256-003-0691-4 [DOI] [PubMed] [Google Scholar]
- 11.Puhakka KB, Jurik AG, Egund N, Schiottz-Christensen B, Stengaard-Pedersen K, van Overeem Hansen G, et al. Imaging of sacroiliitis in early seronegative spondylarthropathy. Assessment of abnormalities by MR in comparison with radiography and CT. Acta Radiol 2003; 44: 218–29.https://doi.org/10.1034/j.1600-0455.2003.00034.x [DOI] [PubMed] [Google Scholar]
- 12.Navallas M, Ares J, Beltrán B, Lisbona MP, Maymó J, Solano A. Sacroiliitis associated with axial spondyloarthropathy: new concepts and latest trends. Radiographics 2013; 33: 933–56.https://doi.org/10.1148/rg.334125025 [DOI] [PubMed] [Google Scholar]
- 13.Özgen A. Comparison of fat-saturated T2-weighted and contrast-enhanced fat-saturated T1-weighted sequences in MR imaging of sacroiliac joints in diagnosing active sacroiliitis. Eur J Radiol 2015; 84: 2593–6.https://doi.org/10.1016/j.ejrad.2015.08.021 [DOI] [PubMed] [Google Scholar]
- 14.Sieper J, van der Heijde D, Landewé R, Brandt J, Burgos-Vagas R, Collantes-Estevez E, et al. New criteria for inflammatory back pain in patients with chronic back pain: a real patient exercise by experts from the assessment of SpondyloArthritis international society (ASAS).. Ann Rheum Dis 2009; 68: 784–8.https://doi.org/10.1136/ard.2008.101501 [DOI] [PubMed] [Google Scholar]
- 15.Hermann KG, Braun J, Fischer T, Reisshauer H, Bollow M. Magnetic resonance tomography of sacroiliitis: anatomy, histological pathology, MR-morphology, and grading. Radiologe 2004; 44: 217–28. [DOI] [PubMed] [Google Scholar]
- 16.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005; 37: 360–3. [PubMed] [Google Scholar]
- 17.Müller R, Büttner P. A critical discussion of intraclass correlation coefficients. Stat Med 1994; 13: 2465–76.https://doi.org/10.1002/sim.4780132310 [DOI] [PubMed] [Google Scholar]
- 18.Vargha P. A critical discussion of intraclass correlation coefficients. Stat Med 1997; 16: 821–3. [DOI] [PubMed] [Google Scholar]
- 19.Koo TK, Li MY, My L. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016; 15: 155–63.https://doi.org/10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maksymowicz H, Kowalewski K, Lubkowska K, Zołud W, Sąsiadek M. Diagnostic value of gadolinium-enhanced MR imaging of active sacroiliitis in seronegative spondyloarthropathy. Pol J Radiol 2010; 75: 58–65. [PMC free article] [PubMed] [Google Scholar]
- 21.de Hooge M, van den Berg R, Navarro-Compán V, van Gaalen F, van der Heijde D, Huizinga T, et al. Magnetic resonance imaging of the sacroiliac joints in the early detection of spondyloarthritis: no added value of gadolinium compared with short tau inversion recovery sequence. Rheumatology 2013; 52: 1220–4.https://doi.org/10.1093/rheumatology/ket012 [DOI] [PubMed] [Google Scholar]
- 22.Boy FN, Kayhan A, Karakas HM, Unlu-Ozkan F, Silte D, Aktas I. The role of multi-parametric MR imaging in the detection of early inflammatory sacroiliitis according to ASAS criteria. Eur J Radiol 2014; 83: 989–96.https://doi.org/10.1016/j.ejrad.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 23.Weiss PF, Xiao R, Biko DM, Johnson AM, Chauvin NA. Detection of inflammatory sacroiliitis in children with magnetic resonance imaging: is gadolinium contrast enhancement necessary? Arthritis Rheumatol 2015; 67: 2250–6.https://doi.org/10.1002/art.39159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Delfaut EM, Beltran J, Johnson G, Rousseau J, Marchandise X, Cotten A. Fat suppression in MR imaging: techniques and pitfalls. Radiographics 1999; 19: 373–82.https://doi.org/10.1148/radiographics.19.2.g99mr03373 [DOI] [PubMed] [Google Scholar]
- 25.Mayerhoefer ME, Mamisch TC, Riegler G, Welsch GH, Dobrocky T, Weber M, et al. Gadolinium diethylenetriaminepentaacetate enhancement kinetics in the menisci of asymptomatic subjects: a first step towards a dedicated dGEMRIC (delayed gadolinium-enhanced MRI of cartilage)-like protocol for biochemical imaging of the menisci. NMR Biomed 2011; 24: 1210–5.https://doi.org/10.1002/nbm.1676 [DOI] [PubMed] [Google Scholar]
- 26.Recht MP, Goodwin DW, Winalski CS, White LM. MRI of articular cartilage: revisiting current status and future directions. AJR Am J Roentgenol 2005; 185: 899–914.https://doi.org/10.2214/AJR.05.0099 [DOI] [PubMed] [Google Scholar]