Patients with cystic fibrosis endure “chronic focal infections” with a variety of microorganisms. One microorganism, Pseudomonas aeruginosa, adapts to the host and develops resistance to a wide range of antimicrobials. Interestingly, as the infection progresses, multiple isogenic strains of P. aeruginosa emerge and coexist within the airways of these patients. Despite a common parental origin, the multiple strains of P. aeruginosa develop vastly different susceptibility patterns to actively used antimicrobial agents—a phenomenon we define as “heterogeneous MICs.” By sequencing pairs of P. aeruginosa isolates displaying heterogeneous MICs, we observed widespread isogenic gene lesions in drug transporters, DNA mismatch repair mechanisms, and many other structural or cellular functions. Coupled with the heterogeneous MICs, these genetic lesions demonstrated a symbiotic response to host selection and suggested evolution of a multicellular syntrophic bacterial lifestyle. Current laboratory standard interpretive criteria do not address the emergence of heterogeneous growth and susceptibilities in vitro with treatment implications.
KEYWORDS: Pseudomonas aeruginosa, cystic fibrosis, heterogeneous, heteroresistance, isogenic, syntrophic
ABSTRACT
Clinical isolates of Pseudomonas aeruginosa from patients with cystic fibrosis (CF) are known to differ from those associated with non-CF hosts by colony morphology, drug susceptibility patterns, and genomic hypermutability. Pseudomonas aeruginosa isolates from CF patients have long been recognized for their overall reduced rate of antimicrobial susceptibility, but their intraclonal MIC heterogeneity has long been overlooked. Using two distinct cohorts of clinical strains (n = 224 from 56 CF patients, n = 130 from 68 non-CF patients) isolated in 2013, we demonstrated profound Etest MIC heterogeneity in CF P. aeruginosa isolates in comparison to non-CF P. aeruginosa isolates. On the basis of whole-genome sequencing of 19 CF P. aeruginosa isolates from 9 patients with heterogeneous MICs, the core genome phylogenetic tree confirmed the within-patient CF P. aeruginosa clonal lineage along with considerable coding sequence variability. No extrachromosomal DNA elements or previously characterized antibiotic resistance mutations could account for the wide divergence in antimicrobial MICs between P. aeruginosa coisolates, though many heterogeneous mutations in efflux and porin genes and their regulators were present. A unique OprD sequence was conserved among the majority of isolates of CF P. aeruginosa analyzed, suggesting a pseudomonal response to selective pressure that is common to the isolates. Genomic sequence data also suggested that CF pseudomonal hypermutability was not entirely due to mutations in mutL, mutS, and uvr. We conclude that the net effect of hundreds of adaptive mutations, both shared between clonally related isolate pairs and unshared, accounts for their highly heterogeneous MIC variances. We hypothesize that this heterogeneity is indicative of the pseudomonal syntrophic-like lifestyle under conditions of being “locked” inside a host focal airway environment for prolonged periods.
IMPORTANCE Patients with cystic fibrosis endure “chronic focal infections” with a variety of microorganisms. One microorganism, Pseudomonas aeruginosa, adapts to the host and develops resistance to a wide range of antimicrobials. Interestingly, as the infection progresses, multiple isogenic strains of P. aeruginosa emerge and coexist within the airways of these patients. Despite a common parental origin, the multiple strains of P. aeruginosa develop vastly different susceptibility patterns to actively used antimicrobial agents—a phenomenon we define as “heterogeneous MICs.” By sequencing pairs of P. aeruginosa isolates displaying heterogeneous MICs, we observed widespread isogenic gene lesions in drug transporters, DNA mismatch repair machinery, and many other structural or cellular functions. Coupled with the heterogeneous MICs, these genetic lesions demonstrated a symbiotic response to host selection and suggested evolution of a multicellular syntrophic bacterial lifestyle. Current laboratory standard interpretive criteria do not address the emergence of heterogeneous growth and susceptibilities in vitro with treatment implications.
INTRODUCTION
In the airway environment of patients with cystic fibrosis (CF), Pseudomonas aeruginosa and other common bacterial cohabitants undergo host airway niche adaption and virulence attenuation (1, 2). When the organism first enters the CF airway, it is under enormous host selective pressure. This pressure leads to a number of well-described phenotypic and genotypic adaptive features such as an overall slow growth rate, diverse colony variants, heterogeneous antimicrobial susceptibility patterns, adoption of a biofilm or multicellular lifestyle, and the emergence of hypermutators, which result from nonsynonymous changes or loss of function mutations in mutS, mutL, and/or uvr (3–6).
Hospital antibiograms are routinely constructed by clinical microbiology laboratories annually (7). The format of hospital antibiograms is standardized by reporting “percent susceptible” using interpretive criteria recommended by professional advisory organizations such as the Clinical and Laboratory Standards Institute (CLSI) (8). Additionally, for clinical laboratories constructing institutional antibiograms, CLSI recommends inclusion of only the first isolate of a given species per patient per reporting period irrespective of body site, antibiotic susceptibility, or other phenotypic characteristics (8). This selection has unintended implications with respect to our understanding of a subset of clinical cultures. For example, unlike the pseudomonal isolates from non-CF patients, pseudomonal colony variants from CF patients producing highly variable and constantly changing susceptibilities are frequently encountered but not accounted for (9–11). Thus, the biological characteristics associated with this subset of organisms have been overlooked.
In the case of CF P. aeruginosa infection, research attention has been paid not only to high-level antimicrobial resistance but also to the phenomena of antimicrobial hypersusceptibilities, heteroresistance, and heterogeneous susceptibilities between isogenic coisolates (9, 12–15). For example, high-level resistance to beta-lactams, including carbapenems, in CF P. aeruginosa has long been linked to acquisition of corresponding hydrolytic enzymes, inactivation or alteration of the drug transporter porin D, and many adaptive mutations in regulatory determinants such as mexR, nalC, and nalD. Mutations in these regulatory elements were previously demonstrated to contribute to the hyperexpression of mexAB-oprM, encoding a prominent drug-proton antiporter or a resistance-nodulation-cell division (RND)-type multidrug efflux pump (16–18). However, our understanding of the mechanism(s) associated with a paradoxical CF P. aeruginosa multiagent hypersusceptibility phenomenon in vitro remains limited (9, 13). In our previous study, we reported that P. aeruginosa isolates with heterogeneous sulfamethoxazole-trimethoprim (SMX-TMP) MICs from the same CF patient were isogenic by pulsed-field gel electrophoresis (PFGE) (9). Moreover, we found mixed mexAB-oprM alleles among clonally coexisting P. aeruginosa isogenic isolates that were associated with heterogeneous SMX-TMP MICs (19–21). As previously proposed (9, 14, 22), the CF airway-specific bacterial colony variants may have assumed an interdependent multicellular mode of replication and resistance. Once a founder clone diverges to show diverse colony morphotypes, auxotrophism, and adaptive lasR inactivation within a P. aeruginosa lineage, therapy based on in vitro susceptibilities is a poor predictor of clinical outcome and the organism is nearly impossible to eradicate (15, 23–28).
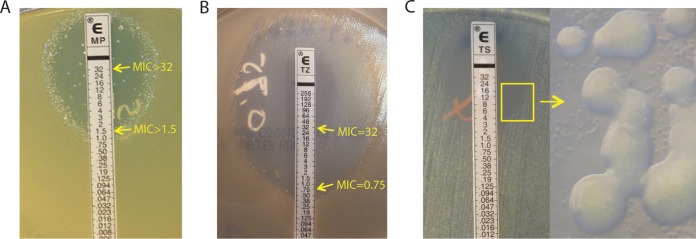
Heteroresistance is generally described as a state represented by subpopulations of bacteria that exhibit a heterogeneous range of susceptibilities to a particular antibiotic in an otherwise clonal population (Fig. 1A and B) (14). The underlying concept of “subpopulations of bacteria” suggested differences within a bacterial clonal population that could not be further separated in vitro by selective subculture passages. In this study, we chose to use the term “heterogeneous MICs” to describe highly variable (>4-fold difference) in vitro MIC values generated by 2 or more P. aeruginosa isolates from the same culture with respect to at least one drug tested in common.
FIG 1 .
P. aeruginosa “strain-specific” heteroresistance. (A) Inner colonies growing above the MIC level where the predominant growth was inhibited at a meropenem concentration of 1.5 μg/ml. E MP, meropenem Etest. (B) Two subpopulations of the same P. aeruginosa isolate showing two distinct ceftazidime MICs, 0.75 and 32 μg/ml. E TZ, ceftazidime Etest. (C) Heterogeneous growth of two subpopulations (big and small) of P. aeruginosa as seen under a microscope with total magnification of ×30. E TS, sulfamethoxazole-trimethoprime Etest.
This investigation aimed to describe the heterogeneous in vitro MIC patterns found in CF P. aeruginosa isolates by inclusion of all colony variants from all cultures within the 7-month study period. Both within- and between-patient P. aeruginosa antimicrobial MIC variances were computed for comparisons between two cohorts of P. aeruginosa isolates (non-CF and CF). The mechanism of pseudomonal heterogeneous MICs and the proposed pseudomonal isogenic syntrophic growth and resistance were further explored by whole-genome sequencing of selected patient-specific P. aeruginosa isolate pairs.
RESULTS
Specimen characteristics of the two cohorts of P. aeruginosa isolates.
A total of 354 clinical P. aeruginosa isolates were included in this analysis: 224 CF P. aeruginosa isolates from 100 cultures obtained from 56 patients and 130 non-CF P. aeruginosa isolates from 99 cultures obtained from 68 patients (Table 1). The CF P. aeruginosa isolates were generally from sputum samples, throat swabs, and bronchoalveolar lavage fluid specimens. The non-CF P. aeruginosa isolates came from a variety of specimen types (tracheal aspirates [n = 41], bronchoalveolar lavage fluid [n = 3], urine [n = 24], wound [n = 8], ear canal [n = 7], blood [n = 5], cerebral spinal fluid [n = 3], sinus [n = 1], and stool [hematology-oncology patients] [n = 7]).
TABLE 1 .
Culture and isolate characteristics classified by CF and non-CF cohorts
|
P. aeruginosa cohort category |
No. of patients |
No. of cultures |
No. of isolates |
Avg no. (range) of isolates per culture |
No. (%) of cultures with ≥2 isolates |
No. (%) of cultures that had isolates with discordant susceptibilitiesa |
Avg no. (range) of agents involved in discordant susceptibilities per culturea |
|---|---|---|---|---|---|---|---|
| CF | 56 | 100 | 224 | 2.24 (1–5) | 64 (64.00) | 41/64 (64.06) | 1.73 (0–10 in 64 cultures) |
| Non-CF | 68 | 99 | 130 | 1.31 (1–3) | 28 (28.28) | 6/28 (21.43) | 0.39 (0–3 in 28 cultures) |
The data for discordant susceptibilities include only those representing changes in MIC interpretations between “S” and “R.” Data corresponding to changes in MIC interpretations between “I” and “S” or between “I” and “R” are not included.
Examples of heteroresistance and their frequencies in each cohort.
In contrast to the stable wild-type P. aeruginosa homogeneous growth, which is sustained through in vitro passages, heterogeneous growth and resistance patterns are frequently found and considered to be “mixed” in clinical laboratories (Fig. 1). Heterogeneous growth properties of CF P. aeruginosa can often be determined by the naked eye but sometimes can be recognized only under a microscope (Fig. 1C). In the most extreme example, this property of P. aeruginosa is defined as heteroresistance, as further subculturing of the isolate results in the same heterogeneous growth and resistance patterns.
The first example of heteroresistance can be common to both CF and non-CF P. aeruginosa isolates where “inner colonies” were growing above the meropenem MIC level of 1.5 μg/ml, the level at which the predominant population of the clone was inhibited (Fig. 1A). The second example of two subpopulations with an antimicrobial MIC at either 0.75 μg/ml or 32 μg/ml, respectively, was also found in CF P. aeruginosa isolates (Fig. 1B). In this study, for isolates generating MIC patterns similar to those shown in Fig. 1A and B, MICs of >32 μg/ml for meropenem (Fig. 1A) and 32 μg/ml for ceftazidime (Fig. 1B) were recorded, respectively, and their heteroresistance patterns were noted as part of the susceptibility record. During the study period, patterns of heteroresistance to at least one antimicrobial agent tested were found in 16 (7%) CF P. aeruginosa isolates and 4 (3%) non-CF P. aeruginosa isolates in our clinical microbiology laboratory. As the extreme heteroresistance phenotype is less frequent than that of the extensively heterogeneous MICs seen with CF P. aeruginosa isolates, we undertook a systematic analysis of differences in the levels of inter- and intrapatient P. aeruginosa antimicrobial MIC heterogeneity between two cohorts of CF and non-CF P. aeruginosa isolates.
CF P. aeruginosa isolates show higher numbers of colony variants by culture and more-pronounced between-patient and within-patient MIC heterogeneity.
In order to examine between-patient, within-patient, and within-culture phenotypic heterogeneity of P. aeruginosa isolates, we specifically included multiple isolates from the same patient (whether from the CF or non-CF cohort). The term “coisolates” was used to describe ≥2 colony variant P. aeruginosa isolates from the same culture. The average number of P. aeruginosa coisolates per culture in the CF cohort was twice as high as in the non-CF cohort (Table 1). Overall, 64% of cultures from the CF cohort had ≥2 P. aeruginosa isolates compared to only 28% of cultures from the non-CF cohort (Table 1). Examining antibiotic susceptibilities, a higher proportion of coisolates from the CF cohort had discordant susceptibilities with respect to at least one antimicrobial agent than among those from the non-CF cohort (64% versus 21%). Further, the average number of agents with discordant susceptibilities was also higher among the P. aeruginosa coisolates from the CF cohort than among those from the non-CF cohort (1.73 versus 0.39) (Table 1).
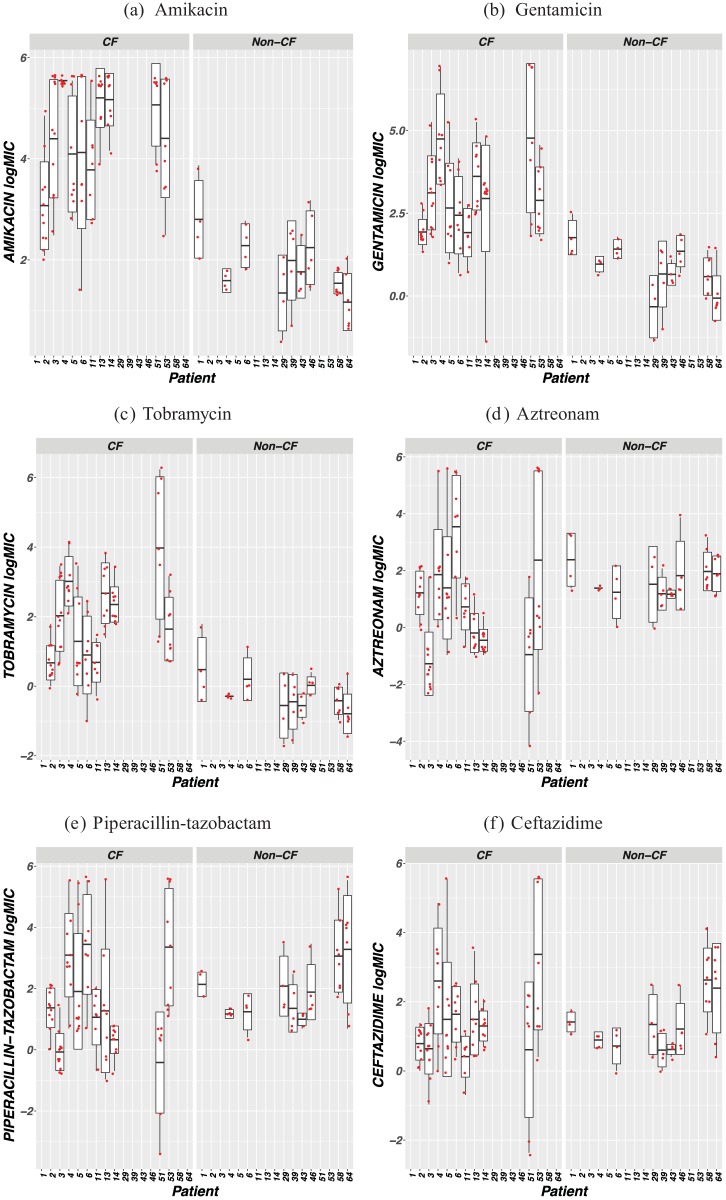
In order to collect exact MIC values, the wide-range Etest method was chosen for this study and logarithmic MIC values (logMICs) were calculated to allow quantitative comparisons between antimicrobial concentration ranges that would be otherwise difficult to accurately compare in the linear range (e.g., 0.002 to 32 µg/ml for meropenem versus 0.064 to 1,024 µg/ml for tobramycin). Comparisons of within-patient antimicrobial susceptibilities between cohorts are shown in Fig. 2 for patients who contributed more than four isolates within the study period. The within-patient logMIC heterogeneities appeared more pronounced in the CF cohort than in the non-CF cohort against all examined agents except for imipenem, meropenem, and ciprofloxacin (CIP) (Fig. 2).
FIG 2 .
Antimicrobial logMIC distributions for P. aeruginosa isolates from selected patients in both CF and non-CF cohorts who contributed >4 isolates within the study period. The dots indicate the logMICs from patient-specific isolates, the vertical lines represent the range of logMICs, the box represents the lower (25%) quartile and upper (75%) quartile, and the horizontal line represents the median.
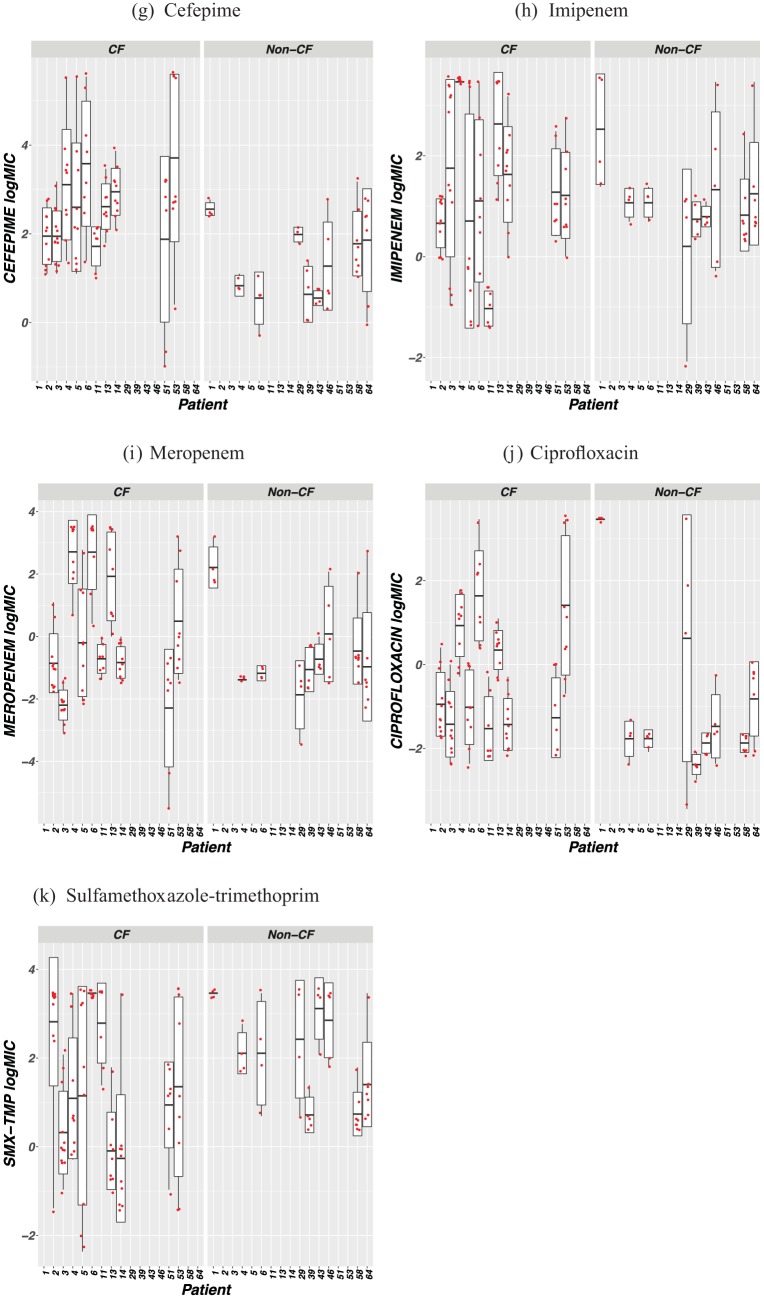
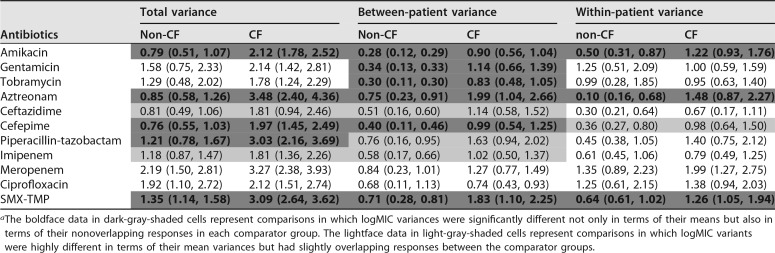
Comparing total levels of variance of antimicrobial logMICs between P. aeruginosa isolates from the CF cohort and those from the non-CF cohort, significantly more heterogeneity was observed for amikacin, aztreonam, cefepime, piperacillin-tazobactam, and SMX-TMP in the isolates from the CF cohort (Table 2). The same comparisons also suggested a trend toward heterogeneity in the CF cohort for ceftazidime and imipenem, but the difference was not statistically significant.
TABLE 2 .
Within- and between-patient variances as well as total variances in logMICs for P. aeruginosa isolates associated with cultures from the two cohorts of patients, namely, the CF patients and non-CF patientsa
The boldface data in dark-gray-shaded cells represent comparisons in which logMIC variances were significantly different not only in terms of their means but also in terms of their nonoverlapping responses in each comparator group. The lightface data in light-gray-shaded cells represent comparisons in which logMIC variants were highly different in terms of their mean variances but had slightly overlapping responses between the comparator groups.
Comparing between-patient variances of antimicrobial logMICs between P. aeruginosa isolates from the CF cohort and those from the non-CF cohort, significantly more heterogeneity was observed for amikacin, gentamicin, tobramycin, aztreonam, cefepime, and SMX-TMP in the isolates from the CF cohort (Table 2). The same comparisons also suggested a trend toward heterogeneity in the CF cohort for ceftazidime, piperacillin-tazobactam, and imipenem, but the difference was not statistically significant.
Comparing within-patient variances of antimicrobial logMICs between P. aeruginosa isolates from the CF cohort and those from the non-CF cohort, significantly more heterogeneity was observed for amikacin, aztreonam, and SMX-TMP in isolates from the CF cohort (Table 2). The same comparisons also suggested a trend toward heterogeneity in the CF cohort for cefepime, but the difference was not statistically significant.
Whole-genome sequencing of 9 sets of CF P. aeruginosa isolates revealed a within-patient clonal lineage in the setting of heterogeneous MICs in vitro.
To examine the molecular basis and clonal relatedness of P. aeruginosa isolates producing heterogeneous MICs, 19 CF P. aeruginosa isolates belonging to 9 patients (8 pairs of P. aeruginosa isolates from 8 patients and 1 set of 3 P. aeruginosa isolates from 1 patient) were selected for whole-genome sequencing. P. aeruginosa isolates were named based on the study patient number using a capital “P” followed by an isolate designation of A, B, or C (Table 3). All patient isolates selected for genome sequencing were either from the same cultures (patients 4, 6, 9, 19, 34, 51, and 53) or from different cultures from the same patient within the 7-month study period (patients 5 and 28) (Table 3). Genomes of both PAO1 and UCBPP-PA14 (PA14) were included as wild-type P. aeruginosa references, as both strains originated from non-CF sources (29, 30). Two genomes corresponding to CF P. aeruginosa strains *356 and *381 belonging to clonal type DK40 and representing isolates collected from two different patients whose data were reported in an earlier European study (10) and which clustered closer to PA14 than other isolates were also included for analysis (Fig. 3). In order to assist the annotation of variants selected in the CF host, sequence variants against the PAO1 reference genome that were also found in PA14 were treated as “neutral” changes for study strains, with the assumption that they would not result in major MIC discrepancies or in other CF P. aeruginosa phenotypic characteristics (Table 4 and 5; see also Table S1 to S4 in the supplemental material).
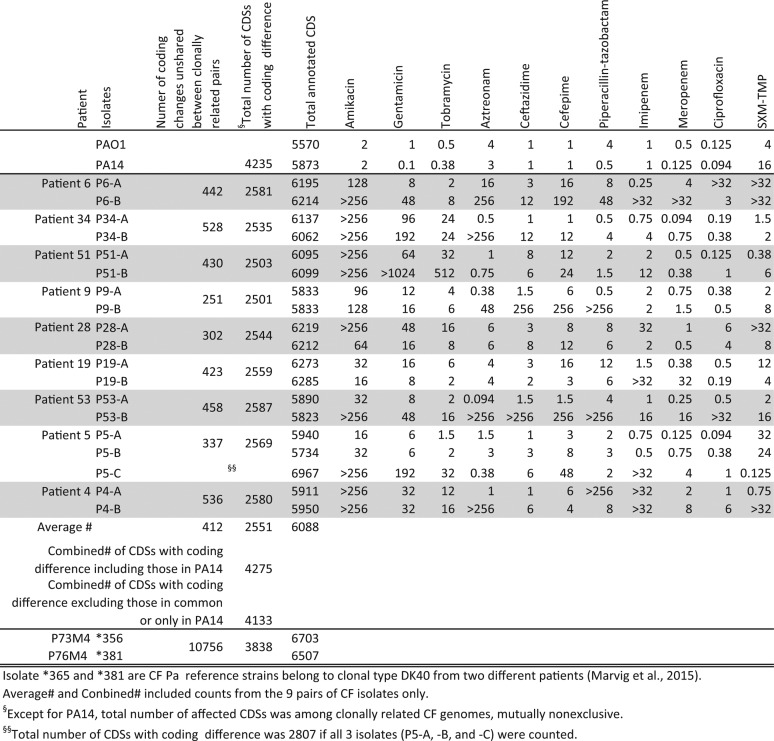
TABLE 3 .
Summary of in vitro antimicrobial MICs and overall genomic polymorphisms of the 19 CF P. aeruginosa isolates and control strains that were subjected to whole-genome sequencing and comparison
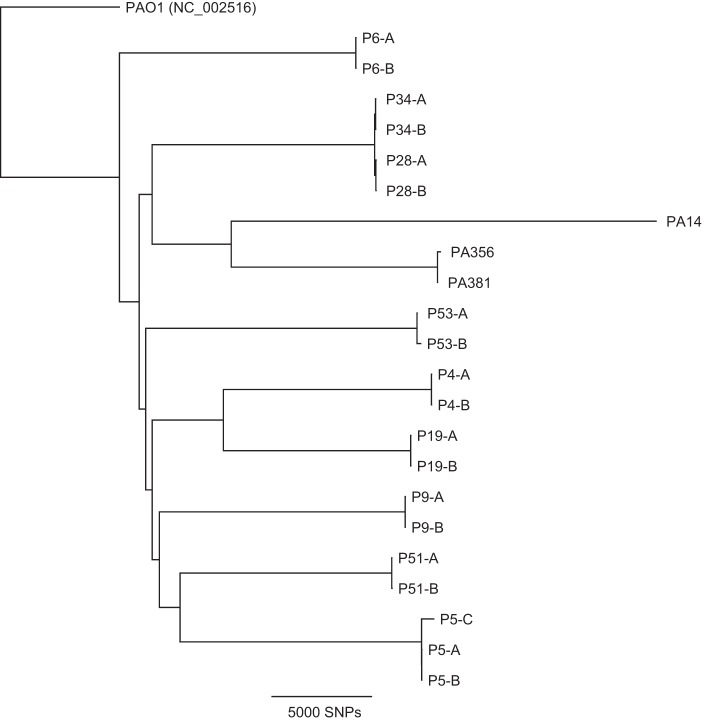
FIG 3 .
Core genome tree data confirming close intrahost relatedness of the 19 CF P. aeruginosa isolates. A core genome single nucleotide polymorphism (SNP) tree was created based on read mapping to the PAO1 reference genome. Additional P. aeruginosa reference genomes PA14 (wild type, non-CF), PA356 (CF), and PA381 (CF) are included in the tree. Each patient is represented by a designation consisting of a capital “P” followed by a number, and different isolates from the same patient are labeled with the letters A, B, and C.
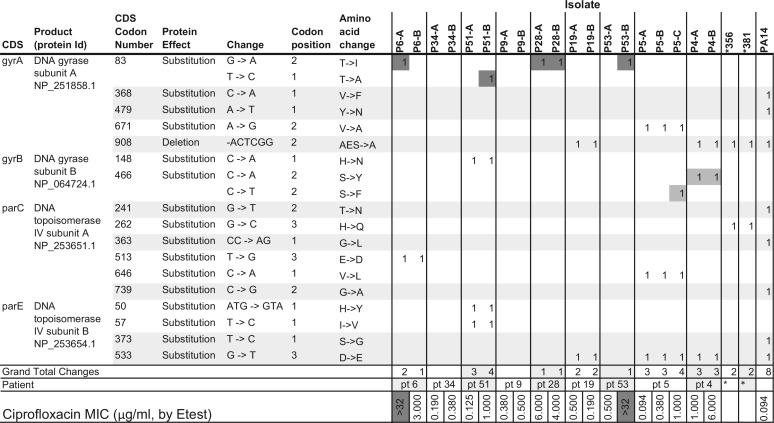
TABLE 4 .
Polymorphic QRDR mutations detected in the 19 CF P. aeruginosa isolates with heterogeneous ciprofloxacin MICs, with the reference genomes of *356, *381, and PA14 included in the comparisona
The well-known QRDR mutations and lesser-known mutations are represented in darker-gray and lighter-gray cells, respectively, while data in the lightest-gray rows represent polymorphisms that are shared with PA14. Id, identifier; pt, patient.
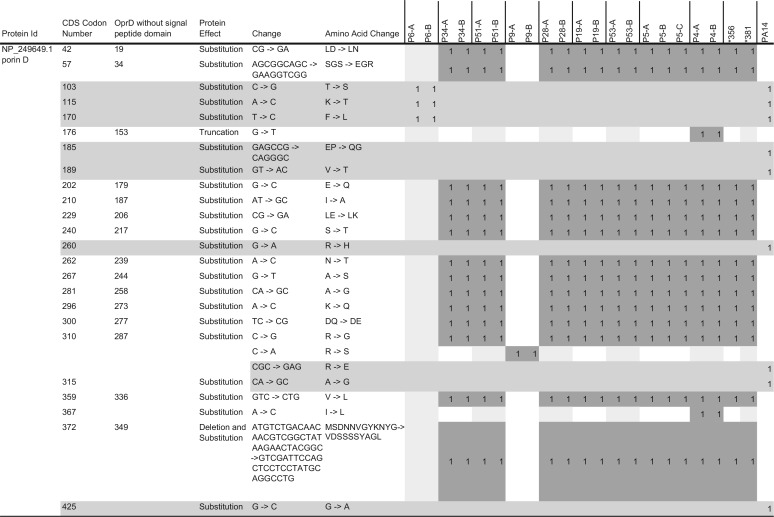
TABLE 5 .
A unique pattern of polymorphic oprD genes identified in CF P. aeruginosa isolatesa
The dark-shaded cells represent the mutations that are not shared with PA14. The light-gray-shaded rows represent the polymorphic changes that are shared with PA14 or present in PA14 only.
Polymorphic changes detected in gene determinants of RND and porin. Note that the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S1, XLSX file, 0.04 MB (41.1KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Summary of CDS polymorphic changes in chromosomal antibiotic resistance genes ampC, ampD, ampD, ampG, dacB, blaOXA-50, aph(3′)-IIb, and cat. Note that the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S2, XLSX file, 0.02 MB (16.2KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Polymorphic changes in genes governing DNA mismatch repair, nucleic acid synthesis, DNA or RNA modification and integrity, and DNA recombination functions in P. aeruginosa isolates. Note that the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S3, XLSX file, 0.02 MB (25.6KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Annotated CDSs with significant mutations, such as deletions, insertions, or frameshift or nonsense/stop codon truncations, among CF P. aeruginosa isolates. Note that those CDSs encoding hypothetical proteins and polymorphic changes that resulted in amino acid nonsynonymous substitutions were not included; the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S4, XLSX file, 0.1 MB (116.1KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Table 3 summarizes the in vitro MICs of the isolates as well as the nonsynonymous coding changes affecting the number of coding sequences (CDSs) among 9 sets of CF P. aeruginosa isolates in reference to the CDSs of PAO1. Intragenic or noncoding sequence mutations were not included in this study. Notably, all 9 of our sets of P. aeruginosa genomes were significantly more closely related to their corresponding coisolate(s) than to other P. aeruginosa isolates, suggesting that each of them derived from a clonal lineage within the same patient (Fig. 3). The clonal relatedness of isolates appeared to be patient specific regardless of whether they were from the same culture or from temporally different cultures within the 7-month study period (Fig. 3) (Table 4 and 5; see also Table S1 to S4) (a similarly organized whole-genome table is not shown). However, the number of unshared CDS polymorphic changes between the members of coisolate pairs ranged from 302 (P28-A and P28-B) to 536 (P4-A and P4-B), suggesting isogenic differences (Table 3). DK40 isolates of the same clonal type (*356 and *381) from different CF patients showed a significantly higher number (n = 10,756) of unshared CDS polymorphic changes between the two. When a value of 5,570 CDSs in PAO1 was used as the reference denominator (excluding all silent or synonymous substitutions and all differences in total CDSs), 2,501 to 2,587 (<50%) nonidentical CDSs were found in the 9 sets of CF P. aeruginosa-related lineage pairs (Table 3) (Fig. 3). In contrast, there were 3,838 (69%) nonidentical CDSs in CF P. aeruginosa pair *365 and *381 and 4,235 (76%) nonidentical CDSs in all PA14 isolates compared to those of PAO1, which further confirmed that CF P. aeruginosa strains *365 and *381 were more closely related to PA14 (Table 3) (Fig. 3). In an analysis in which all nonidentical CDSs were combined from all 9 sets of CF P. aeruginosa genomes, a combined total of 4,133 (74%, excluding the ones that were shared with those in PA14) CDSs were found to be different from those in PAO1.
In order to explain heterogeneous MICs between paired isolates, we first examined known antibiotic resistance genes also present in the genomes of PAO1 and PA14. The chromosomal antibiotic resistance genes ampC, ampD, ampD, ampG, dacB, blaOXA-50, aph(3′)-IIb, and cat were compared. There were significant numbers of coding polymorphisms that were specifically shared between clonally related P. aeruginosa pairs except for a single unshared point mutation associated with a Y132C substitution in ampD of isolate P53-B only and two point mutations with substitutions in cat of isolate P5-C only. None of the intra- or interclonal polymorphisms could explain their tested heterogeneous beta-lactam MIC patterns (Table 3; see also Table S2). On the basis of genome coverage, only a 390-kb region of P6-A showed a 3-fold increase in coverage relative to the background genome. This fragment aligned to a 350-kb region of PAO1 chromosome and to 40 kb of the FluMu prophage present in P. aeruginosa strain ATCC 27853 (GenBank accession no. CP015117.1), suggesting that the coverage variation was likely due to phage sequence. No other areas of significant coverage variation were observed in the rest of the sequenced isolates.
Multiple unpaired coding polymorphisms in known quinolone resistance-determining regions (QRDR) were found in clonal pairs.
Highly heterogeneous CIP MICs were observed in coisolate pair P6-A and P6-B from CF patient 6 and coisolate pair P53-A and P53-B from CF patient 53 (Table 4). The classic mutations in the QRDR in gyrA codon 83 (T83I and T83A) were detected in both P6-A and P53-B and in an additional 3 isolates (P51-B, P28-A, and P28-B). However, the 3 additional isolates, P51-B, P28-A, and P28-B, did not produce an ultrahigh MIC of >32 μg/ml (Table 4). The lesser-known QRDR mutations in gyrB (S466F and S466Y) were also identified in strains P5-C, P4-A, and P4-B, although they showed variable CIP MICs at 1, 1, and 6 μg/ml, respectively, spanning clinical breakpoints of ≤1 μg/ml susceptible (“S”), 2 μg/ml intermediate (“I”), and ≥4 μg/ml resistant (“R”) (Table 4) (31). In fact, none of the amino acid substitutions (absent in PA14) detected in these four genes (gyrA, gyrB, parC, and parE) was able to entirely account for either the ultrahigh or ultralow CIP MICs among the 19 isolates measured in vitro (Table 4).
A unique pattern of porin D mutation was found in 15 of the 19 genomes sequenced.
Gene determinants associated with outer membrane porin proteins and efflux pumps and their regulators were highly polymorphic among all isolates (Table 5; see also Table S1 and S2). However, polymorphic mutations in this group of porin and efflux pumps did not indicate the presence of any previously known mechanisms of resistance. For example, despite the highly heterogeneous MICs seen in vitro among the 19 isolates, the well-known porin D determinant oprD (a total of 443 amino acid residues in PAO1 with a signal peptide of 23 amino acids at the N terminus) was similarly altered among 15 of the 19 isolates (P34-A, P34-B, P51-A, P51-B, P28-A, P28-B, P19-A, P19-B, P53-A, P53-B, P5-A, P5-B, P5-C, P4-A, and P4-B), with strikingly identical patterns even at the nucleotide level (Table 5). Moreover, the same OprD pattern was also shared by two clonally distant reference CF P. aeruginosa strains, *356 and *381 (Table 5). All isolates contained identical nonsynonymous substitutions affecting 16 positions, including a well-known outer membrane surface loop 7 variant with a pattern of MSDNNVGYKNYG to VDSSSSYAGL (Table 5) (18).
In addition, an OprD truncation was found in pair P4-A and P4-B due to a stop codon at residue 176 showing nonuniform MIC levels of carbapenems or other agents (Table 3 and 5; see also Table S1). Significantly different OprD coding patterns were associated with two coisolate pairs—P6-A and P6-B shared 3 amino acid substitutions identical to those in PA14, and P9-A and P9-B shared a unique R310S substitution, regardless of the detected intraclonal heterogeneous MICs of both imipenem and meropenem and of other 9 agents tested (Table 3 and 5).
P6-A and P6-B showed ultrahigh SMX-TMP MICs of >32 μg/ml that could be correlated to possible mexAB-oprM overexpression resulting from frameshift deletions in negative regulator gene nalD at codon 85 (−TGCGCTCGCTCTAC) and at codon 133 (−TG), respectively (32). However, their heterogeneous antimicrobial MICs for all beta-lactam agents (aztreonam, ceftazidime, cefepime, piperacillin-tazobactam, imipenem, and meropenem) could not be simply delineated by the presence of their presumably intact oprD gene without considering many additional mutations in other relevant genes and regulators (Table 5; see also Table S1 to S4). In fact, multiple polymorphic mutations in efflux genes (e.g., mexAB-oprM, mexCD-oprJ, mexEF-oprN, mexXY-oprA, and mexJK) and multiple regulators (e.g., mexR, mexZ, nalC, and nalD) were detected in all 19 isolates that were both shared and not shared between intra- and interclonal isolates (Table S1).
Polymorphic mutations in CDSs associated with P. aeruginosa hypermutability and other cellular functions.
Mutations that resulted in high numbers of polymorphic mutations were common not only in isolates containing lesions in DNA mismatch repair genes (mutL and mutS) but also in those containing lesions in many other determinants. The affected CDSs, including genes involved in nucleotide synthesis (mutM and mutY), DNA repair or DNA/RNA folding, and recombination functions (recB, recC, recD, recF, recG, recJ, recN, recO, rdgC, rarA, recX, recR, uvrA, uvrB, uvrC, and uvrD), were detected in our CF P. aeruginosa isolates and in CF P. aeruginosa isolates *356 and *381 (Table S3). A 13-bp deletion in mutS (Table S3) was found only in P53-B, but this isolate did not have an increased number of significant mutations in CDSs compared to its coisolate P53-A or compared to the rest of 17 P. aeruginosa strains (Table 3).
A number of other bacterial cellular functions and known P. aeruginosa pathogenicity factors also demonstrated coding variants that were found only in the 19 CF P. aeruginosa isolate sequences and not in PAO1 and PA14 (Table 4 to 5; see also Table S1 to S4) (Fig. 3). The affected CDSs included those in genes related to metabolic functions, ABC transporter proteins, electron transport chain functions for ATP synthesis, iron acquisition, two-component sensors and regulators, the RND proteins and membrane porin proteins, transcription regulators, type III secretion systems, DNA repair, RNA polymerization, and structures of flagella and fimbriae, as well as biosynthesis of alginate, pyoverdine, sugar, lipids, nucleotides, amino acids, and vitamins.
DISCUSSION
Our study demonstrated that antimicrobial MIC heterogeneity is more characteristic of CF P. aeruginosa than of non-CF P. aeruginosa. We found that both the average number of P. aeruginosa coisolates per culture and the average number of agents with discordant susceptibilities between coisolates were higher in the CF cohort than in the non-CF cohort. CF cohort P. aeruginosa isolates presented antimicrobial MICs that were more heterogeneous than those seen with non-CF isolates, in the overall analyses as well as in the within-patient and between-patient analyses.
The characteristic phenomenon of the CF P. aeruginosa heterogeneous antimicrobial MIC distribution in clonally related isolates is strongly supported by the genomic evidence of a high degree of core genome relatedness as well as unshared coding changes—an average of 412 coding changes—between patient-specific P. aeruginosa pairs (Table 3 to 5) (Fig. 2 and 3). We believe that their heterogeneous MICs are the net results of the combined impact of their diverse structural and functional mutations in response to CF host selection. Functional genomic features specific to CF P. aeruginosa may not be immediately apparent based on the proportion of CDSs that deviated from those of either PAO1 or PA14, but the unique patterns in specific gene determinants common among CF P. aeruginosa isolates may be more informative (Table 3 to 5; see also Table S1 to S4). For example, the mutations that were shared or not shared between the same clonal lineages affecting the known QRDRs had no clear association with CIP MICs (Table 4). In contrast, the unique amino acid substitution patterns, including “loop 7” in OprD, in the majority of CF P. aeruginosa isolates could not be mistaken for random events (Table 5) (18). The heterogeneous CF P. aeruginosa antimicrobial MICs, especially among clonal pairs, may just be one aspect of the overall adaptive evolution to the host airways (Fig. 1 to 3) (Table 1 to 5; see also Table S1 to S4).
Despite coming from different patients and different lineages, the CF P. aeruginosa genomes studied here had similar mutational patterns affecting the same genes (e.g., oprD, mexAB, mutL, and mutS), suggesting a common selective pressure (Table 3 to 5; see also Table S3 and S4) (Fig. 3). The unshared changes detected between CF P. aeruginosa clonal pairs that occurred in response to host selective pressure are indicative of a transition to a potentially multicellular lifestyle with functional syntrophic associates that are heterogeneous and obligate for growth and resistance (Table 3) (Fig. 1) (3). The plethora of coding polymorphisms (Table 3 to 5; see also Table S1 to S4) detected in CF P. aeruginosa isolates is not only responsible for their heterogeneous MIC patterns, but also for a series of adaptive evolutionary process indicative of niche specialization (Fig. 1) (3, 9). The mutations described here will require further characterization in vitro and in vivo to test these hypotheses.
The overall lack of horizontal gene transfer in CF P. aeruginosa is shown by the absence of evidence of areas of sequences with increased coverage (except for P6-A), consistent with the lack of plasmids or other accessory genes that usually drive the emergence of bacterial “superbugs” in free-living bacteria (33, 34). The 19 representative CF P. aeruginosa strains all contained a chromosomal ampC gene, which, upon induction, is associated with the ability to hydrolyze cephalosporins but not carbapenems, and blaOXA-50, encoding a constitutively expressed oxacillinase (35). The aph(3′)-IIb gene is known to confer resistance to kanamycin and neomycin but not to amikacin, gentamicin, or tobramycin (36). In fact, none of the chromosomal resistance gene determinants [ampC, blaOXA-50, and aph(3′)-IIb] or putative regulator mutations in ampR, ampD, ampG, or dacB can be used to explain the phenomenon of highly heterogeneous MICs seen with CF P. aeruginosa pairs for any single beta-lactam agent tested (Table 3 to 5; see also Table S3). Similar to the 47 P. aeruginosa isolates reported by Lee et al. that produced CIP MIC levels of 2 to 64 µg/ml with only the gyrA T83I as the “first step” mutation(s) (31), the 19 CF P. aeruginosa isolates containing either the well-defined QRDR mutations or novel amino acid substitutions did not show a consistent correlation with their wide range of CIP MICs (Table 4). Quinolone resistance in P. aeruginosa has been well characterized as involving porin and efflux mechanisms as well (37, 38). The highly distinct OprD mutational patterns that were conserved within the majority of unrelated CF P. aeruginosa isolates (Table 5), along with those associated with the highly polymorphic RND family of efflux proteins and regulators, showed no correlation to previously reported drug transporter or efflux pump activities uniformly affecting P. aeruginosa susceptibilities with respect to SMX-TMP, aztreonam, carbapenems, or other classes of antimicrobials (16, 17, 21, 39, 40).
There is ample evidence of the existence of relaxed DNA mismatch repair systems due to mutations in both mutL and mutS in CF P. aeruginosa isolates contributing to “hypermutability” and thus to altered virulence and susceptibilities (9, 13, 29, 41, 42). A previously reported laboratory P. aeruginosa strain containing an 11-bp deletion in mutS was found to show increases in the rate of base pair mutations of 267× and in the rate of indels of 230× in comparison to a wild-type founder P. aeruginosa strain under culture conditions (43). On the basis of the variants seen in the 19 CF P. aeruginosa isolates, we believe that the hypermutable state of CF P. aeruginosa strains cannot be solely attributed to diverse mutations in mutL and/or mutS, as a mutS deleterious frameshift mutation in an isolate from P53-B did not show increased total numbers of mutations or CDSs affected in comparison to the other 18 isolates (Table 3; see also Table S1 to S4). Our additional findings of mutations in determinants responsible for nucleotide synthesis, DNA/RNA modification, and recombination enzymes further support the long-standing observation of the “genome decay” phenomenon as part of the bacterial symbiotic response to host selective pressure (Table S4) (3, 10, 44).
The current state of clinical laboratory susceptibility reporting has strictly followed the conventions of the three categories of interpretations for in vitro antimicrobial activities (“S,” “I,” and “R”). These interpretations have played and will continue to play a significant role in providing clinical reference values and guiding treatment decisions. These categories are accurate for rapidly growing bacterial strains that are phenotypically homogeneous, likely due to their brief encounters with the host organisms in settings of “acute” infections. Although content is limited with respect to heteroresistance, CLSI has also developed technical instructions such as “examine carefully with transmitted light for >1 colony or light film of growth” regarding recording zones of inhibition around oxacillin/cefoxitin against staphylococcus and streptococcus (7). These instructions have begun to address susceptibility characteristics that are beyond the clear-cut “S,” “I,” and “R” categories. However, heterogeneous susceptibilities generated from colony variants of the same culture have not received elevated recognition. Before we can embark on a proper laboratory report with treatment implications, we propose the use of broad-range microdilutions for susceptibility testing of bacterial isolates exhibiting slow and heterogeneous growth patterns in vitro. We also propose the use of a proper form of laboratory documentation in the presence of heterogeneous MICs.
This study was limited by the overall small number of isolates used for statistical analysis and the lack of information regarding the duration of P. aeruginosa infection in the members of either cohort. Neither patient underlying diseases nor patient treatment history was included in this analysis. The non-CF cohort of P. aeruginosa isolates may have included patients whose pseudomonal infections were similar to those of patients with CF or those of patients who have had prolonged infections affecting other organ or tissue systems. Such mixed inclusion would bias results toward the null instead of exacerbating the effects seen here. Future studies separating P. aeruginosa isolates collected from hosts with newly acquired infections and isolates collected from hosts with chronic infections (both CF and non-CF) would improve data clarity. Bacterial whole-genome longitudinal analysis of isolates will be able to recapitulate the process by which continuous host-selected genome decay leads to the rise of a “host tissue-definitive” P. aeruginosa multicellular specialist and to confirm the lack of repeat wild-type P. aeruginosa infections thereafter.
The term “heteroresistance” may represent just one specific segment on the continuum of heterogeneous MICs. The finding of disparate intraclonal antimicrobial MICs in vitro may be explained by bacterial functional divergence with increased interdependence of growth and resistance during niche specialization (Fig. 1 and 2) (14). With the advances in treatment of congenital or acquired defects and many other complex diseases, there is a growing patient population receiving frequent and long-term antibiotic therapy that may be at increased risk of developing chronic focal infections (14). The acknowledgment and understanding of laboratory findings of bacterial discordant susceptibilities and/or heteroresistance in the setting of chronic focal infections can open opportunities for the use of alternative therapeutic evaluations and approaches (3).
MATERIALS AND METHODS
Bacterial isolates from cultures included for antimicrobial MIC analysis.
This study included all clinically obtained P. aeruginosa isolates identified in the Clinical Microbiology Laboratory at Seattle Children’s Hospital (SCH) over a 7-month period (June 2013 to December 2013) and was approved by the SCH Institutional Review Board. All P. aeruginosa isolates were identified by matrix-assisted laser desorption ionization–time of flight (MALDI-TOF) analysis (Bruker Daltonics Inc.). Culture methods for isolates from CF patients were distinct from those used with non-CF isolates as previously described (9, 45). Colony variants of all bacterial isolates were separated from mixed cultures using single-colony subcultures based on size, pigment, texture, hemolysis patterns, mucoidy, etc. Potential susceptibilities associated with a nonhomogeneous appearance were reexamined after maximal purification of colony variants for repeat susceptibility testing. Where Etest patterns similar to those shown in Fig. 1A and B were reproducible, “heteroresistance” was noted; otherwise, separate susceptibility data are reported for isolates showing homogeneous growth and susceptibilities.
Antibiotic susceptibility testing and MIC determination.
Antibiotic susceptibility was determined by the Etest (BioMérieux) MIC method. All isolates were tested for susceptibility to amikacin, gentamicin, tobramycin, aztreonam, ceftazidime, cefepime, imipenem, meropenem, piperacillin-tazobactam, CIP, and SMX-TMP. Each single isolate from mixed cultures was maximally purified by the use of single-colony subcultures based on colony size, hemolysis, pigment, texture, mucoidy, etc. Etest susceptibility testing was set up as previously described (9). In general, the Etest plates were incubated at 35°C in ambient air for 18 to 24 h. Prolonged incubation was frequently required for some CF P. aeruginosa isolates due to slow growth (requiring up to 36 to 48 h) for MIC determination. Antimicrobial susceptibility data were interpreted using CLSI M100-S23 MIC breakpoint criteria (46).
Statistical analyses of variability in antimicrobial MICs.
We first assigned detection limits corresponding to those MIC data points for which the highest or the lowest detection limits were reached (e.g., an MIC value of >256 was entered as a value of 256). We then applied logarithmic transformation to all the MIC readings (logMICs) to make the data less skewed for analysis. All subsequent analyses were based on logMICs.
Since multiple isolates from the same patients were collected and tested in the same period, we applied repeated analysis of variance (ANOVA) to decompose the data corresponding to the total variance in logMICs into the categories of variance within patients (among isolates from the same patient) and variance between patients. The repeated ANOVA was conducted separately for CF and non-CF patients. In order to statistically compare the differences in the levels of logMIC variability between the CF and non-CF patients, we derived 95% bootstrap confidence intervals for the within- and between-patient variations, as well as for the total variations. We decided a priori that two variance estimates were significantly different if their corresponding confidence intervals did not overlap. All statistical analyses were performed using Stata version 12 (Stata Corp., College Station, TX).
Bacterial whole-genome sequencing.
A subset of P. aeruginosa isolate pairs was selected for whole-genome sequencing based on their heterogeneous or discordant in vitro antimicrobial MICs for at least 1 of the 11 agents tested (Table 4). All 19 CF P. aeruginosa isolates were verified both by naked eye and by microscopic appearance on Mueller Hinton (MH) and M9 minimal media to produce relatively homogeneous growth in vitro. Isolates showing nonhomogeneous growth patterns (Fig. 1) were not included in the sequencing investigation. The control genomes of strains PAO1 (NC_002516.2) and UCBPP-PA14 (PA14; NC_008463.1) and two previously sequenced genomes of clonally related CF P. aeruginosa reference strains *356 and *381 (SRA accession ERS402683 and ERS402710, respectively) from a European study were included for this analysis (10). PAO1 and PA14 are used to represent the two highly dissimilar P. aeruginosa genomes for analysis as non-CF P. aeruginosa references or “wild-type” susceptibility controls (9, 13, 47). All sequence polymorphisms associated with our CF P. aeruginosa strains (i.e., strains *356 and *381) as well as with PA14 were generated in reference to the PAO1 genome (10). In this study, polymorphisms found in PA14 in reference to PAO1 were assumed to have minimal functional impact on structural or biological functions, including in vitro susceptibilities, if both were treated as non-CF “wild-type” strains (Table 4 and 5; see also Table S1 to S4).
DNA was extracted from P. aeruginosa isolates and diluted to 1 ng/μl for sequencing library generation with third-volume Nextera XT and 14 cycles of PCR amplification (48, 49). Sequencing reads were adapter and quality trimmed using cutadapt, de novo assembled using SPAdes v3.9, and annotated using prokka (50, 51). Reads were mapped to the PAO1 reference genome (NC_002516.2), and variant call files were generated using Geneious v9.1 and cutoff values of at least 7× coverage and 70% allele frequency. Core genome trees were generated based on single nucleotide variants that excluded indels as described previously (52).
Accession number(s).
Bacterial assemblies were deposited in NCBI GenBank under BioProject PRJNA369567.
ACKNOWLEDGMENTS
We thank Anne Marie Buccat and Jenny R. Stapp for their years of contributions to Cystic Fibrosis Microbiology Reference Laboratory operation and quality maintenance of clinical and research data. We thank the Seattle Children’s Microbiology team for their high-quality performance and quality documentation of susceptibility testing and quality control results. We are also grateful for the Project Hope scholarship that supported S. Yuan during her Microbiology and Infectious Diseases training at Seattle Children’s Hospital.
X. Qin and A. L. Greninger designed and performed the research. X. Qin, A. L. Greninger, C. Zhou, A. Adler, A. Addetia, S. Yuan, and D. M. Zerr analyzed and discussed the data. X. Qin, C. Zhou, D. M. Zerr, A. Addetia, and A. L. Greninger wrote the paper.
REFERENCES
- 1.Hentzer M, Wu H, Andersen JB, Riedel K, Rasmussen TB, Bagge N, Kumar N, Schembri MA, Song Z, Kristoffersen P, Manefield M, Costerton JW, Molin S, Eberl L, Steinberg P, Kjelleberg S, Høiby N, Givskov M. 2003. Attenuation of Pseudomonas aeruginosa virulence by quorum sensing inhibitors. EMBO J 22:3803–3815. doi: 10.1093/emboj/cdg366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mena A, Maciá MD, Borrell N, Moya B, de Francisco T, Pérez JL, Oliver A. 2007. Inactivation of the mismatch repair system in Pseudomonas aeruginosa attenuates virulence but favors persistence of oropharyngeal colonization in cystic fibrosis mice. J Bacteriol 189:3665–3668. doi: 10.1128/JB.00120-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qin X. 2016. Chronic pulmonary pseudomonal infection in patients with cystic fibrosis: a model for early phase symbiotic evolution. Crit Rev Microbiol 42:144–157. doi: 10.3109/1040841X.2014.907235. [DOI] [PubMed] [Google Scholar]
- 4.Oliver A, Baquero F, Blázquez J. 2002. The mismatch repair system (mutS, mutL and uvrD genes) in Pseudomonas aeruginosa: molecular characterization of naturally occurring mutants. Mol Microbiol 43:1641–1650. doi: 10.1046/j.1365-2958.2002.02855.x. [DOI] [PubMed] [Google Scholar]
- 5.Ciofu O, Riis B, Pressler T, Poulsen HE, Høiby N. 2005. Occurrence of hypermutable Pseudomonas aeruginosa in cystic fibrosis patients is associated with the oxidative stress caused by chronic lung inflammation. Antimicrob Agents Chemother 49:2276–2282. doi: 10.1128/AAC.49.6.2276-2282.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oliver A, Cantón R, Campo P, Baquero F, Blázquez J. 2000. High frequency of hypermutable Pseudomonas aeruginosa in cystic fibrosis lung infection. Science 288:1251–1254. doi: 10.1126/science.288.5469.1251. [DOI] [PubMed] [Google Scholar]
- 7.CLSI 2017. Performance standards for antimicrobial susceptibility testing, M100. Clinical and Laboratory Standards Institute, Wayne, PA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CLSI 2009. Analysis and presentation of cumulative antimicrobial susceptibility test data, M39-A3. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 9.Qin X, Zerr DM, McNutt MA, Berry JE, Burns JL, Kapur RP. 2012. Pseudomonas aeruginosa syntrophy in chronically colonized airways of cystic fibrosis patients. Antimicrob Agents Chemother 56:5971–5981. doi: 10.1128/AAC.01371-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marvig RL, Sommer LM, Molin S, Johansen HK. 2015. Convergent evolution and adaptation of Pseudomonas aeruginosa within patients with cystic fibrosis. Nat Genet 47:57–64. doi: 10.1038/ng.3148. [DOI] [PubMed] [Google Scholar]
- 11.Clark ST, Diaz Caballero J, Cheang M, Coburn B, Wang PW, Donaldson SL, Zhang Y, Liu M, Keshavjee S, Yau YC, Waters VJ, Elizabeth Tullis D, Guttman DS, Hwang DM. 2015. Phenotypic diversity within a Pseudomonas aeruginosa population infecting an adult with cystic fibrosis. Sci Rep 5:10932. doi: 10.1038/srep10932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.López-Causapé C, Rojo-Molinero E, Macià MD, Oliver A. 2015. The problems of antibiotic resistance in cystic fibrosis and solutions. Expert Rev Respir Med 9:73–88. doi: 10.1586/17476348.2015.995640. [DOI] [PubMed] [Google Scholar]
- 13.Wolter DJ, Black JA, Lister PD, Hanson ND. 2009. Multiple genotypic changes in hypersusceptible strains of Pseudomonas aeruginosa isolated from cystic fibrosis patients do not always correlate with the phenotype. J Antimicrob Chemother 64:294–300. doi: 10.1093/jac/dkp185. [DOI] [PubMed] [Google Scholar]
- 14.El-Halfawy OM, Valvano MA. 2015. Antimicrobial heteroresistance: an emerging field in need of clarity. Clin Microbiol Rev 28:191–207. doi: 10.1128/CMR.00058-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahida K, Kwon DH. 2010. Co-existence of multidrug-resistant and -susceptible strains of Pseudomonas aeruginosa from a single clinical isolate. Curr Microbiol 61:19–24. doi: 10.1007/s00284-009-9570-0. [DOI] [PubMed] [Google Scholar]
- 16.Braz VS, Furlan JP, Fernandes AF, Stehling EG. 2016. Mutations in NalC induce MexAB-OprM overexpression resulting in high level of aztreonam resistance in environmental isolates of Pseudomonas aeruginosa. FEMS Microbiol Lett 363:fnw166. doi: 10.1093/femsle/fnw166. [DOI] [PubMed] [Google Scholar]
- 17.Pan YP, Xu YH, Wang ZX, Fang YP, Shen JL. 2016. Overexpression of MexAB-OprM efflux pump in carbapenem-resistant Pseudomonas aeruginosa. Arch Microbiol 198:565–571. doi: 10.1007/s00203-016-1215-7. [DOI] [PubMed] [Google Scholar]
- 18.Pirnay JP, De Vos D, Mossialos D, Vanderkelen A, Cornelis P, Zizi M. 2002. Analysis of the Pseudomonas aeruginosa oprD gene from clinical and environmental isolates. Environ Microbiol 4:872–882. doi: 10.1046/j.1462-2920.2002.00281.x. [DOI] [PubMed] [Google Scholar]
- 19.Wilke MS, Heller M, Creagh AL, Haynes CA, McIntosh LP, Poole K, Strynadka NC. 2008. The crystal structure of MexR from Pseudomonas aeruginosa in complex with its antirepressor ArmR. Proc Natl Acad Sci U S A 105:14832–14837. doi: 10.1073/pnas.0805489105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daigle DM, Cao L, Fraud S, Wilke MS, Pacey A, Klinoski R, Strynadka NC, Dean CR, Poole K. 2007. Protein modulator of multidrug efflux gene expression in Pseudomonas aeruginosa. J Bacteriol 189:5441–5451. doi: 10.1128/JB.00543-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Köhler T, Kok M, Michea-Hamzehpour M, Plesiat P, Gotoh N, Nishino T, Curty LK, Pechere JC. 1996. Multidrug efflux in intrinsic resistance to trimethoprim and sulfamethoxazole in Pseudomonas aeruginosa. Antimicrob Agents Chemother 40:2288–2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Falagas ME, Makris GC, Dimopoulos G, Matthaiou DK. 2008. Heteroresistance: a concern of increasing clinical significance? Clin Microbiol Infect 14:101–104. doi: 10.1111/j.1469-0691.2007.01912.x. [DOI] [PubMed] [Google Scholar]
- 23.Evans TJ. 2015. Small colony variants of Pseudomonas aeruginosa in chronic bacterial infection of the lung in cystic fibrosis. Future Microbiol 10:231–239. doi: 10.2217/fmb.14.107. [DOI] [PubMed] [Google Scholar]
- 24.Smith AL, Fiel SB, Mayer-Hamblett N, Ramsey B, Burns JL. 2003. Susceptibility testing of Pseudomonas aeruginosa isolates and clinical response to parenteral antibiotic administration: lack of association in cystic fibrosis. Chest 123:1495–1502. doi: 10.1378/chest.123.5.1495. [DOI] [PubMed] [Google Scholar]
- 25.Pollack M (ed). 2000. Pseudomonas aeruginosa. Churchill Livingstone, New York, NY. [Google Scholar]
- 26.Gillham MI, Sundaram S, Laughton CR, Haworth CS, Bilton D, Foweraker JE. 2009. Variable antibiotic susceptibility in populations of Pseudomonas aeruginosa infecting patients with bronchiectasis. J Antimicrob Chemother 63:728–732. doi: 10.1093/jac/dkp007. [DOI] [PubMed] [Google Scholar]
- 27.D’Argenio DA, Wu M, Hoffman LR, Kulasekara HD, Déziel E, Smith EE, Nguyen H, Ernst RK, Larson Freeman TJ, Spencer DH, Brittnacher M, Hayden HS, Selgrade S, Klausen M, Goodlett DR, Burns JL, Ramsey BW, Miller SI. 2007. Growth phenotypes of Pseudomonas aeruginosa lasR mutants adapted to the airways of cystic fibrosis patients. Mol Microbiol 64:512–533. doi: 10.1111/j.1365-2958.2007.05678.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agarwal G, Kapil A, Kabra SK, Das BK, Dwivedi SN. 2005. Characterization of Pseudomonas aeruginosa isolated from chronically infected children with cystic fibrosis in India. BMC Microbiol 5:43. doi: 10.1186/1471-2180-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee DG, Urbach JM, Wu G, Liberati NT, Feinbaum RL, Miyata S, Diggins LT, He J, Saucier M, Déziel E, Friedman L, Li L, Grills G, Montgomery K, Kucherlapati R, Rahme LG, Ausubel FM. 2006. Genomic analysis reveals that Pseudomonas aeruginosa virulence is combinatorial. Genome Biol 7:R90. doi: 10.1186/gb-2006-7-10-r90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klockgether J, Munder A, Neugebauer J, Davenport CF, Stanke F, Larbig KD, Heeb S, Schöck U, Pohl TM, Wiehlmann L, Tümmler B. 2010. Genome diversity of Pseudomonas aeruginosa PAO1 laboratory strains. J Bacteriol 192:1113–1121. doi: 10.1128/JB.01515-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee JK, Lee YS, Park YK, Kim BS. 2005. Alterations in the GyrA and GyrB subunits of topoisomerase II and the ParC and ParE subunits of topoisomerase IV in ciprofloxacin-resistant clinical isolates of Pseudomonas aeruginosa. Int J Antimicrob Agents 25:290–295. doi: 10.1016/j.ijantimicag.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 32.Evans K, Passador L, Srikumar R, Tsang E, Nezezon J, Poole K. 1998. Influence of the MexAB-OprM multidrug efflux system on quorum sensing in Pseudomonas aeruginosa. J Bacteriol 180:5443–5447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xiong J, Alexander DC, Ma JH, Déraspe M, Low DE, Jamieson FB, Roy PH. 2013. Complete sequence of pOZ176, a 500-kilobase IncP-2 plasmid encoding IMP-9-mediated carbapenem resistance, from outbreak isolate Pseudomonas aeruginosa 96. Antimicrob Agents Chemother 57:3775–3782. doi: 10.1128/AAC.00423-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shen K, Sayeed S, Antalis P, Gladitz J, Ahmed A, Dice B, Janto B, Dopico R, Keefe R, Hayes J, Johnson S, Yu S, Ehrlich N, Jocz J, Kropp L, Wong R, Wadowsky RM, Slifkin M, Preston RA, Erdos G, Post JC, Ehrlich GD, Hu FZ. 2006. Extensive genomic plasticity in Pseudomonas aeruginosa revealed by identification and distribution studies of novel genes among clinical isolates. Infect Immun 74:5272–5283. doi: 10.1128/IAI.00546-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Girlich D, Naas T, Nordmann P. 2004. Biochemical characterization of the naturally occurring oxacillinase OXA-50 of Pseudomonas aeruginosa. Antimicrob Agents Chemother 48:2043–2048. doi: 10.1128/AAC.48.6.2043-2048.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zeng L, Jin S. 2003. aph(3′)-IIb, a gene encoding an aminoglycoside-modifying enzyme, is under the positive control of surrogate regulator HpaA. Antimicrob Agents Chemother 47:3867–3876. doi: 10.1128/AAC.47.12.3867-3876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Llanes C, Köhler T, Patry I, Dehecq B, van Delden C, Plésiat P. 2011. Role of the MexEF-OprN efflux system in low-level resistance of Pseudomonas aeruginosa to ciprofloxacin. Antimicrob Agents Chemother 55:5676–5684. doi: 10.1128/AAC.00101-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jacoby GA. 2005. Mechanisms of resistance to quinolones. Clin Infect Dis 41(Suppl 2):S120–S126. doi: 10.1086/428052. [DOI] [PubMed] [Google Scholar]
- 39.Ocampo-Sosa AA, Cabot G, Rodríguez C, Roman E, Tubau F, Macia MD, Moya B, Zamorano L, Suárez C, Peña C, Domínguez MA, Moncalián G, Oliver A, Martínez-Martínez L; Spanish Network for Research in Infectious Disease . 2012. Alterations of OprD in carbapenem-intermediate and -susceptible strains of Pseudomonas aeruginosa isolated from patients with bacteremia in a Spanish multicenter study. Antimicrob Agents Chemother 56:1703–1713. doi: 10.1128/AAC.05451-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li XZ, Plésiat P, Nikaido H. 2015. The challenge of efflux-mediated antibiotic resistance in Gram-negative bacteria. Clin Microbiol Rev 28:337–418. doi: 10.1128/CMR.00117-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.López-Causapé C, Rojo-Molinero E, Mulet X, Cabot G, Moyà B, Figuerola J, Togores B, Pérez JL, Oliver A. 2013. Clonal dissemination, emergence of mutator lineages and antibiotic resistance evolution in Pseudomonas aeruginosa cystic fibrosis chronic lung infection. PLoS One 8:e71001. doi: 10.1371/journal.pone.0071001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Montanari S, Oliver A, Salerno P, Mena A, Bertoni G, Tümmler B, Cariani L, Conese M, Döring G, Bragonzi A. 2007. Biological cost of hypermutation in Pseudomonas aeruginosa strains from patients with cystic fibrosis. Microbiology 153:1445–1454. doi: 10.1099/mic.0.2006/003400-0. [DOI] [PubMed] [Google Scholar]
- 43.Dettman JR, Sztepanacz JL, Kassen R. 2016. The properties of spontaneous mutations in the opportunistic pathogen Pseudomonas aeruginosa. BMC Genomics 17:27. doi: 10.1186/s12864-015-2244-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Degnan PH, Yu Y, Sisneros N, Wing RA, Moran NA. 2009. Hamiltonella defensa, genome evolution of protective bacterial endosymbiont from pathogenic ancestors. Proc Natl Acad Sci U S A 106:9063–9068. doi: 10.1073/pnas.0900194106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burns JL, Emerson J, Stapp JR, Yim DL, Krzewinski J, Louden L, Ramsey BW, Clausen CR. 1998. Microbiology of sputum from patients at cystic fibrosis centers in the United States. Clin Infect Dis 27:158–163. doi: 10.1086/514631. [DOI] [PubMed] [Google Scholar]
- 46.CLSI 2009–2014. Performance standards for antimicrobial susceptibility testing, M100-MS19. Clinical and Laboratory Standards Institute, Wayne, PA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kos VN, Déraspe M, McLaughlin RE, Whiteaker JD, Roy PH, Alm RA, Corbeil J, Gardner H. 2015. The resistome of Pseudomonas aeruginosa in relationship to phenotypic susceptibility. Antimicrob Agents Chemother 59:427–436. doi: 10.1128/AAC.03954-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Greninger AL, Langelier C, Cunningham G, Keh C, Melgar M, Chiu CY, Miller S. 2015. Two rapidly growing mycobacterial species isolated from a brain abscess: first whole-genome sequences of Mycobacterium immunogenum and Mycobacterium llatzerense. J Clin Microbiol 53:2374–2377. doi: 10.1128/JCM.00402-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Herman EK, Greninger AL, Visvesvara GS, Marciano-Cabral F, Dacks JB, Chiu CY. 2013. The mitochondrial genome and a 60-kb nuclear DNA segment from Naegleria fowleri, the causative agent of primary amoebic meningoencephalitis. J Eukaryot Microbiol 60:179–191. doi: 10.1111/jeu.12022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, Lesin VM, Nikolenko SI, Pham S, Prjibelski AD, Pyshkin AV, Sirotkin AV, Vyahhi N, Tesler G, Alekseyev MA, Pevzner PA. 2012. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol 19:455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seemann T. 2014. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30:2068–2069. doi: 10.1093/bioinformatics/btu153. [DOI] [PubMed] [Google Scholar]
- 52.Kozyreva VK, Truong CL, Greninger AL, Crandall J, Mukhopadhyay R, Chaturvedi V. 2017. Validation and implementation of clinical laboratory improvements act-compliant whole-genome sequencing in the public health microbiology laboratory. J Clin Microbiol 55:2502–2520. doi: 10.1128/JCM.00361-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Polymorphic changes detected in gene determinants of RND and porin. Note that the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S1, XLSX file, 0.04 MB (41.1KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Summary of CDS polymorphic changes in chromosomal antibiotic resistance genes ampC, ampD, ampD, ampG, dacB, blaOXA-50, aph(3′)-IIb, and cat. Note that the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S2, XLSX file, 0.02 MB (16.2KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Polymorphic changes in genes governing DNA mismatch repair, nucleic acid synthesis, DNA or RNA modification and integrity, and DNA recombination functions in P. aeruginosa isolates. Note that the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S3, XLSX file, 0.02 MB (25.6KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Annotated CDSs with significant mutations, such as deletions, insertions, or frameshift or nonsense/stop codon truncations, among CF P. aeruginosa isolates. Note that those CDSs encoding hypothetical proteins and polymorphic changes that resulted in amino acid nonsynonymous substitutions were not included; the gray-shaded rows represent the mutations that were shared with PA14 or present in PA14 only. Download TABLE S4, XLSX file, 0.1 MB (116.1KB, xlsx) .
Copyright © 2018 Qin et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.