Summary
Children who were overweight or obese, particularly with asthma, had higher odds of intensive care admission or mechanical ventilation. There was no association between elevated BMI and severe outcomes in adults, however, underweight adults had longer hospital stay..
Keywords: pneumonia, CAP, BMI, obesity, outcomes.
Abstract
Background.
The effect of body mass index (BMI) on community-acquired pneumonia (CAP) severity is unclear.
Methods.
We investigated the relationship between BMI and CAP outcomes (hospital length of stay [LOS], intensive care unit [ICU] admission, and invasive mechanical ventilation) in hospitalized CAP patients from the Centers for Disease Control and Prevention Etiology of Pneumonia in the Community (EPIC) study, adjusting for age, demographics, underlying conditions, and smoking status (adults only).
Results.
Compared with normal-weight children, odds of ICU admission were higher in children who were overweight (adjusted odds ratio [aOR], 1.7; 95% confidence interval [CI], 1.1–2.8) or obese (aOR, 2.1; 95% CI, 1.4–3.2), and odds of mechanical ventilation were higher in children with obesity (aOR, 2.7; 95% CI, 1.3–5.6). When stratified by asthma (presence/absence), these findings remained significant only in children with asthma. Compared with normal-weight adults, odds of LOS >3 days were higher in adults who were underweight (aOR, 1.6; 95% CI, 1.1–2.4), and odds of mechanical ventilation were lowest in adults who were overweight (aOR, 0.5; 95% CI, .3–.9).
Conclusions.
Children who were overweight or obese, particularly those with asthma, had higher odds of ICU admission or mechanical ventilation. In contrast, adults who were underweight had longer LOS. These results underscore the complex relationship between BMI and CAP outcomes.
In the United States, 17% of children 2–19 years and 36% of adults ≥20 years old were obese, while 4% of children and 2% of adults were underweight based on data from 2009–2010 [1]. Obesity in adults has been identified as a risk factor for hospitalization due to seasonal influenza [2] and during the 2009 influenza pandemic, obesity emerged as a risk factor for intensive care unit (ICU) admission [3] and death [3–5]. Obesity in adults has also been suggested as a risk factor for invasive pneumococcal disease [6] and community-acquired pneumonia (CAP) [7–9], but not all studies support this association [10–13]. In addition, the effect of obesity on clinical outcomes due to CAP in adults is unclear, with several studies suggesting either no impact or even a protective effect [12, 14–18]. Adults who are underweight may also be at increased risk for respiratory infections, including CAP [8, 10–13, 19], and its severe outcomes, including death [12, 14, 17, 20]. Some studies that examined the effect of body mass index (BMI) on respiratory infections in children suggest that being underweight may be a risk factor for hospitalization due to influenza A(H1N1)pdm09 virus infection [6] or CAP [21].
Understanding the association between BMI and CAP severity could help guide public health policy and practice as rates of obesity remain high [1] and pneumonia is a leading cause of morbidity and mortality in the United States [22, 23]. Using the Centers for Disease Control and Prevention (CDC) Etiology of Pneumonia in the Community (EPIC) study data, we examined the association between BMI and outcomes, including hospital length of stay (LOS), ICU admission, and invasive mechanical ventilation.
METHODS
From 1 January 2010 to 30 June 2012, children (<18 years) and adults (≥18 years) hospitalized with CAP were enrolled in the EPIC study at 3 pediatric hospitals (Memphis and Nashville, Tennessee and Salt Lake City, Utah; hereafter randomly designated as cities A–C) and 5 adult hospitals (Chicago, Illinois and Nashville, Tennessee; hereafter randomly designated as cities D–E) [24, 25]. Patients were enrolled if they had clinical and radiographically confirmed pneumonia and were excluded if recently hospitalized, severely immunocompromised, a child residing in an extended care facility, or an adult residing in a nursing home unable to function independently [24, 25]. Informed consent was obtained and the study protocol was approved by institutional review boards at each institution and CDC.
Using standardized methods, demographic and clinical information was collected through patient interview and medical chart abstraction [24, 25]. Admission Pneumonia Severity Index (PSI) [26] and CURB-65 [27] scores were calculated for adults. Blood and respiratory specimens were collected from children and adults, and urine specimens from adults only. Diagnostic testing for bacterial and viral pathogens included bacterial culture, real-time polymerase chain reaction (PCR), serology, and urine antigen (Supplementary Materials) [24, 25].
For this analysis, we included patients ≥2 years of age with available height and weight abstracted from medical charts; pregnant women and children aged <2 years were excluded as pre-pregnancy weight was not collected for pregnant women and BMI is not calculated for children <2 years [28]. For children (2–17 years), age- and sex-specific z scores for BMI were calculated based on the 2000 CDC growth charts with BMI categories of underweight (<5th percentile), normal weight (5th–84th percentile), overweight (85th–94th percentile), and obesity (≥95th percentile) [28]; children with extreme or biologically implausible values [29] were excluded. For adults (≥18 years), BMI was calculated as weight in kilograms divided by square height in meters. BMI categories included underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obesity (30.0–39.9 kg/m2), and extreme obesity (≥40 kg/m2) [30]; all adults with available BMI were included (BMI range, 12–78). LOS was dichotomized based on the median of 3 days.
For children and adults, demographics, clinical characteristics, and pathogen detections were compared across different BMI categories using χ2 or Fisher exact test for categorical variables and the Kruskal-Wallis test for continuous variables. All comparisons were 2-sided; P < .05 was considered significant. Logistic regression models were used to examine the relationship between BMI and outcomes including LOS >3 days, ICU admission, and invasive mechanical ventilation (hereafter referred to as mechanical ventilation) with normal weight as the referent. Factors determined a priori and biologically plausible factors significant in bivariate analyses were included as potential confounders; factors with a prevalence of <5% were excluded. All models were assessed for goodness of fit and collinearity.
Age and underlying conditions for children and adults and PSI score for adults were considered potential effect modifiers a priori and placed into the adult and pediatric models as interaction terms with BMI. The final pediatric and adult models were adjusted for age (continuous variable), sex, race/ethnicity, enrollment city, and history of asthma, heart disease, or neurological conditions. Adult models were also adjusted for chronic obstructive pulmonary disease (COPD), diabetes, immunosuppression, cancer (excluding dermatological malignancies), and current smoking status. Based on the statistical significance of the interaction terms and our a priori considerations, all final pediatric models were stratified by age (2–4 years and 5–17 years) and presence or absence of asthma, and all final adult models were stratified by age (18–49 years, 50–64 years, and ≥65 years) and PSI score class (low, 1–3 vs moderate/high, 4–5). In a separate analysis, all pediatric and adult models were also adjusted for presence or absence of bacterial, atypical bacterial, or viral etiologies. Analyses were performed in SAS software version 9.3 (SAS Institute, Cary, North Carolina).
RESULTS
Children
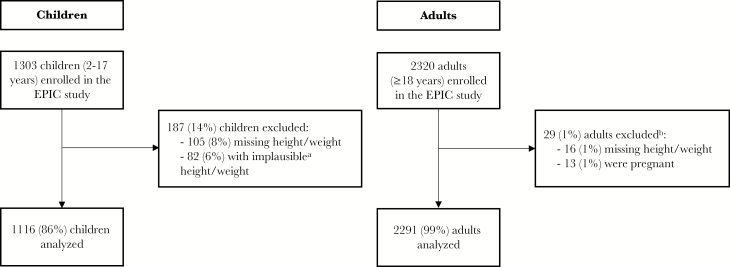
Among 1303 children (2–17 years) who met the final study criteria, 105 (8%) had missing height or weight and were excluded. An additional 82 (6%) had implausible height and weight and were also excluded (Figure 1). Of 1116 children with available BMI, 176 (16%) were underweight, 657 (59%) normal weight, 126 (11%) overweight, and 157 (14%) obese.
Figure 1.
Children and adults enrolled in the Etiology of Pneumonia in the Community (EPIC) study who were included in the analysis of the relationship between body mass index (BMI) and community-acquired pneumonia outcomes. aExtreme or biologically implausible values were assessed based on Centers for Disease Control and Prevention growth charts [29] for children; of 82 children with implausible height/weight information, 35 (43%) would have been categorized as underweight, 15 (18%) as normal weight, 4 (5%) as overweight, and 28 (34%) as obese. bAll BMI values were included (range, 12–78).
BMI increased with increasing age; 66% of children who were underweight were 2–4 years of age, and 71% of children with obesity were ≥5 years of age (Table 1). Race and ethnicity were similar among children who were normal weight, overweight, or obese. However, compared with other BMI groups, there were more black children (42%) and fewer Hispanic children (6%) in the underweight group. Although a similar proportion of children with obesity was enrolled in each city (31%–35%), nearly half (49%) of children who were underweight were from city A. Asthma/reactive airway disease was the most common underlying condition across all BMI categories (41%) including among children who were overweight (48%) and obese (46%).
Table 1.
Proportion of Select Characteristics in Children Hospitalized With Community-Acquired Pneumonia by Body Mass Index Category (n = 1116)
| Characteristics | All | Underweight | Normal | Overweight | Obesity | P Valuea |
|---|---|---|---|---|---|---|
| (N = 1116) | (n = 176) | (n = 657) | (n = 126) | (n = 157) | ||
| Age group, % | <.01 | |||||
| 2–4 y | 45 | 66 | 48 | 24 | 29 | |
| 5–11 y | 40 | 25 | 39 | 52 | 54 | |
| 12–17 y | 15 | 9 | 14 | 25 | 17 | |
| Female sex, % | 47 | 48 | 49 | 41 | 44 | .36 |
| Race/Ethnicity, % | <.01 | |||||
| Non-Hispanic white | 45 | 44 | 47 | 47 | 41 | |
| Non-Hispanic black | 33 | 42 | 32 | 28 | 30 | |
| Hispanic | 15 | 6 | 16 | 20 | 18 | |
| Other | 7 | 8 | 5 | 6 | 11 | |
| Enrollment city, % | <.01 | |||||
| A | 37 | 49 | 35 | 36 | 31 | |
| B | 26 | 23 | 23 | 34 | 34 | |
| C | 37 | 27 | 42 | 30 | 35 | |
| Insurance, % | .06 | |||||
| None | 2 | 2 | 2 | 4 | 2 | |
| Public | 53 | 63 | 50 | 51 | 54 | |
| Private | 45 | 35 | 48 | 45 | 44 | |
| Clinical presentation, % | ||||||
| Onset to admission, d, median (IQR) | 3 (1–6) | 3 (1–6) | 4 (1–7) | 3 (1–7) | 3 (1–5) | .52 |
| Wheezing | 38 | 37 | 35 | 40 | 48 | .02 |
| Tachypneab | 51 | 49 | 50 | 51 | 54 | .88 |
| Tachycardiac | 56 | 66 | 52 | 49 | 65 | <.01 |
| Hypoxiad | 37 | 32 | 37 | 37 | 46 | .07 |
| Radiographic characteristics, % | ||||||
| Consolidation | 63 | 66 | 61 | 60 | 68 | .27 |
| Infiltrate | 46 | 48 | 47 | 44 | 41 | .56 |
| Pleural effusion | 19 | 16 | 18 | 17 | 22 | .56 |
| Underlying conditions, % | 55 | 53 | 51 | 67 | 64 | <.01 |
| Asthma | 41 | 40 | 39 | 48 | 46 | .15 |
| Heart disease | 7 | 8 | 6 | 6 | 11 | .14 |
| Immunosuppression/ HIV | 3 | 1 | 3 | 6 | 2 | .06 |
| Cancer | 1 | 0 | 1 | 2 | 1 | .12 |
| Neurological disease | 11 | 14 | 9 | 17 | 10 | .02 |
Abbreviations: HIV, human immunodeficiency virus; IQR, interquartile range.
aUnivariate comparisons with P values by χ2 (count ≥5 in each cell) or Fisher exact test.
bTachypnea (breaths/min): respiratory rate >40 (1–5 y) or >25 (>5 y).
cTachycardia (beats/min): heart rate >151 (2 y), >137 (3–4 y), >133 (5–7 y), >130 (8–11 y), >119 (12–16 y),>100 (>16 y).
dHypoxia: oxygen saturation <92% or on oxygen at presentation.
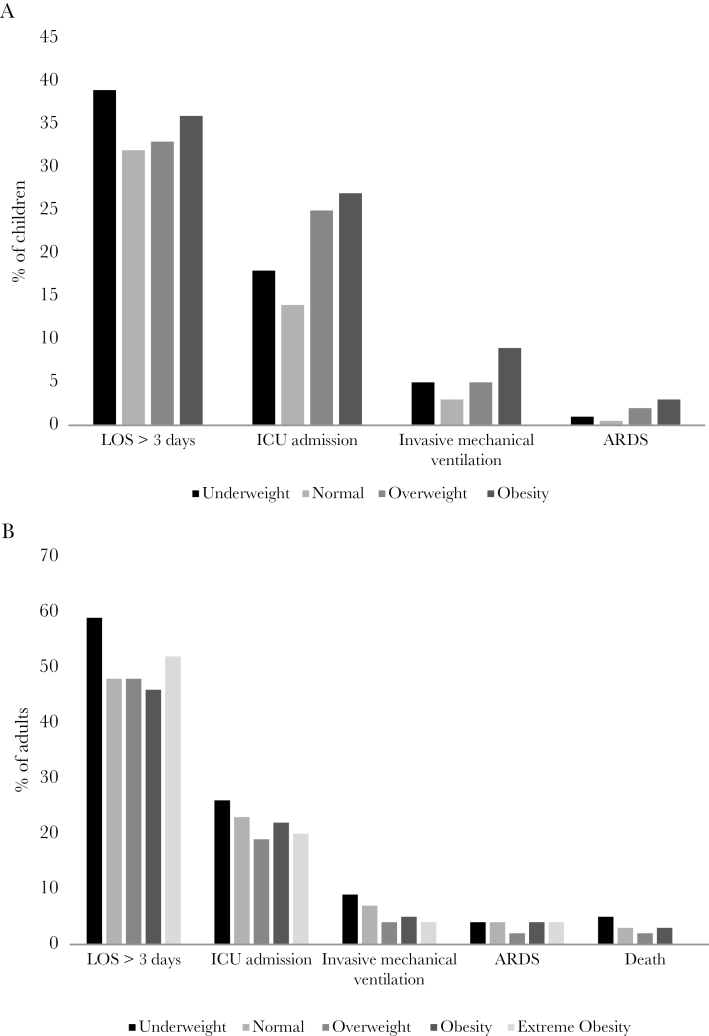
In unadjusted analyses, LOS >3 days was similar across different BMI categories (Figure 2A). Compared with children of normal weight, ICU admission was more common among children who were overweight (14% vs 25%; odds ratio [OR], 1.93; 95% confidence interval [CI], 1.22–3.06) or obese (14% vs 27%; OR, 2.16; 95% CI, 1.43–3.27), and children with obesity had higher prevalence of mechanical ventilation (3% vs 9%; OR, 2.97; 95% CI, 1.47–5.97). Eleven (<1%) children developed acute respiratory distress syndrome (ARDS): 4 (3%) of the children with obesity compared with 3 (<1%) children of normal weight (OR, 5.70; 95% CI, 1.26–25.73). Two children died; both had normal weight.
Figure 2.
Clinical outcomes by body mass index category among children (A) and adults (B) hospitalized with community-acquired pneumonia. Abbreviations: ARDS, acute respiratory distress syndrome; ICU, intensive care unit; LOS, length of stay.
After adjusting for demographics and underlying conditions, there was no significant difference in odds of LOS >3 days between the different BMI categories (Table 2). However, odds of ICU admission were higher in children who were overweight (adjusted OR [aOR], 1.70; 95% CI, 1.05–2.75) or obese (aOR, 2.09; 95% CI, 1.36–3.22) and odds of mechanical ventilation were higher in children with obesity (aOR, 2.70; 95% CI, 1.31–5.57).
Table 2.
Odds Ratios and Confidence Intervals for Hospital Length of Stay, Intensive Care Unit Admission, and Invasive Mechanical Ventilation by Body Mass Index Category Among Children Hospitalized With Community-Acquired Pneumonia Adjusted for Demographics, Select Chronic Conditions, and Etiologya
| Outcome | BMI Category | Adjustedb | Adjusted for Etiologyc | ||||
|---|---|---|---|---|---|---|---|
| % With Outcome | OR (95% CI) | P Value | % With Outcome | OR (95% CI) | P Value | ||
| Hospital length of stay >3 d | n = 1115 | n = 1065 | |||||
| Underweight | 39 | 1.35 (.95–1.93) | .10 | 40 | 1.41 (.98–2.05) | .06 | |
| Normal | 32 | Ref | 32 | Ref | |||
| Overweight | 33 | 0.92 (.60–1.40) | .70 | 33 | 0.88 (.56–1.37) | .56 | |
| Obesity | 36 | 1.18 (.81–1.71) | .40 | 36 | 1.15 (.78–1.72) | .48 | |
| With asthma | n = 460 | n = 443 | |||||
| Underweight | 45 | 2.48 (1.41–4.37) | .002 | 46 | 2.48 (1.39–4.40) | .002 | |
| Normal | 27 | Ref | 27 | Ref | |||
| Overweight | 30 | 1.19 (.63–2.28) | .59 | 29 | 1.10 (.56–2.16) | .78 | |
| Obesity | 39 | 2.07 (1.16–3.69) | .01 | 39 | 2.13 (1.15–3.93) | .02 | |
| Without asthma | n = 655 | n = 622 | |||||
| Underweight | 35 | 0.95 (.59–1.53) | .83 | 36 | 0.99 (.60–1.63) | .97 | |
| Normal | 36 | Ref | 35 | Ref | |||
| Overweight | 35 | 0.77 (.43–1.38) | .38 | 35 | 0.74 (.40–1.38) | .35 | |
| Obesity | 34 | 0.76 (.46–1.28) | .31 | 33 | 0.72 (.41–1.26) | .25 | |
| Intensive care unit admission | n = 1116 | n = 1065 | |||||
| Underweight | 18 | 1.32 (.84–2.10) | .23 | 19 | 1.40 (.88–2.24) | .16 | |
| Normal | 14 | Ref | 14 | Ref | |||
| Overweight | 25 | 1.70 (1.05–2.75) | .03 | 24 | 1.68 (1.01–2.80) | .05 | |
| Obesity | 27 | 2.09 (1.36–3.22) | <.001 | 27 | 2.20 (1.41–3.50) | <.001 | |
| With asthma | n = 461 | n = 443 | |||||
| Underweight | 24 | 1.50 (.77–2.93) | .23 | 24 | 1.50 (.76–2.96) | .24 | |
| Normal | 17 | Ref | 17 | Ref | |||
| Overweight | 25 | 1.49 (.73–3.02) | .27 | 24 | 1.44 (.69–3.03) | .33 | |
| Obesity | 31 | 2.48 (1.32–4.68) | .005 | 32 | 2.95 (1.50–5.78) | .002 | |
| Without asthma | n = 655 | n = 622 | |||||
| Underweight | 14 | 1.15 (.60–2.20) | .68 | 15 | 1.29 (.66–2.52) | .46 | |
| Normal | 13 | Ref | 12 | Ref | |||
| Overweight | 25 | 1.79 (.91–3.52) | .09 | 24 | 1.81 (.88–3.75) | .11 | |
| Obesity | 24 | 1.72 (.93–3.18) | .08 | 22 | 1.63 (.84–3.14) | .15 | |
| Invasive mechanical ventilation | n = 1116 | n = 1065 | |||||
| Underweight | 5 | 1.45 (.64–3.31) | .37 | 5 | 1.59 (.68–3.74) | .28 | |
| Normal | 3 | Ref | 3 | Ref | |||
| Overweight | 5 | 1.14 (.43–3.01) | .79 | 4 | 0.82 (.27–2.49) | .72 | |
| Obesity | 9 | 2.70 (1.31–5.57) | .007 | 9 | 3.08 (1.43–6.67) | .004 | |
| With asthma | n = 461 | n = 443 | |||||
| Underweight | 4 | 1.09 (.25–4.87) | .91 | 4 | 1.18 (.24–5.90) | .84 | |
| Normal | 3 | Ref | 3 | Ref | |||
| Overweight | 3 | 0.70 (.13–3.81) | .68 | 3 | 0.38 (.06–2.49) | .31 | |
| Obesity | 10 | 5.01 (1.49–16.84) | .009 | 11 | 8.87 (2.17–36.29) | .002 | |
| Without asthma | n = 655 | n = 622 | |||||
| Underweight | 6 | 1.63 (.59–4.52) | .35 | 6 | 2.04 (.70–5.94) | .19 | |
| Normal | 4 | Ref | 3 | Ref | |||
| Overweight | 6 | 1.55 (.46–5.16) | .48 | 5 | 1.10 (.26–4.67) | .90 | |
| Obesity | 8 | 2.32 (.88–6.13) | .09 | 7 | 2.39 (.82–7.02) | .11 | |
Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio.
aAll comparisons were with the normal weight category.
bAdjusted pediatric regression models were controlled for age, sex, race/ethnicity, enrollment city, history of asthma, heart disease, and neurological conditions. Adjusted models stratified by age category were controlled for age, sex, race/ethnicity, enrollment city, history of asthma, heart disease, and neurological conditions. Adjusted models stratified by presence or absence of asthma were controlled for age, sex, race/ethnicity, enrollment city, heart disease, and neurological conditions.
cAdjusted models with etiology were adjusted for all the factors mentioned above as well as for the presence or absence of bacterial, atypical bacterial (Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Legionella species), or viral etiology.
Models stratified by age (2–4 years and 5–17 years) yielded similar results (Supplementary Table 1).
When stratified by presence or absence of asthma, among children with asthma, odds of LOS >3 days was higher in children who were underweight (aOR, 2.48; 95% CI, 1.41–4.37) or obese (aOR, 2.07; 95% CI, 1.16–3.69); and odds of ICU admission (aOR, 2.48; 95% CI, 1.32–4.68) and mechanical ventilation (aOR, 5.01; 95% CI, 1.49–16.84) were significantly higher for children with obesity (Table 2). No significant association was observed between BMI and severe outcomes in children without asthma.
Adults
Among 2320 adults who met the final study criteria, 13 (1%) were pregnant, and 16 (1%) had missing height or weight (Figure 1) and were excluded. Of 2291 adults with available BMI, 110 (5%) were underweight, 713 (31%) normal weight, 631 (28%) overweight, 606 (26%) obese, and 231 (10%) extremely obese.
Obesity was more common in adults <65 years of age; 67% with obesity and 81% with extreme obesity were adults aged <65 years (Table 3). Female sex (72%) and black race (56%) were more common in adults with extreme obesity. Asthma (41%) and diabetes (44%) were most common among adults with extreme obesity, whereas COPD (37%) and immunosuppression (26%) were most common among adults who were underweight. PSI and CURB-65 were lowest (indicating a lower risk for 30-day mortality) among adults with extreme obesity (PSI median, 2; CURB-65 median, 0).
Table 3.
Proportion of Select Characteristics in Adults Hospitalized With Community-Acquired Pneumonia by Body Mass Index Category (n = 2291)
| Characteristics | All | Underweight | Normal | Overweight | Obesity | Extreme Obesity | P Valuea |
|---|---|---|---|---|---|---|---|
| (n = 2291) | (n = 110) | (n = 713) | (n = 631) | (n = 606) | (n = 231) | ||
| Age group, % | <.01 | ||||||
| 18–49 y | 30 | 25 | 28 | 29 | 30 | 38 | |
| 50–64 y | 34 | 27 | 32 | 31 | 37 | 43 | |
| ≥65 y | 36 | 48 | 40 | 40 | 33 | 19 | |
| Female sex, % | 51 | 59 | 47 | 44 | 54 | 72 | <.01 |
| Race/Ethnicity, % | <.01 | ||||||
| Non-Hispanic white | 47 | 56 | 52 | 49 | 43 | 30 | |
| Non-Hispanic black | 39 | 34 | 35 | 33 | 42 | 56 | |
| Hispanic | 10 | 6 | 8 | 13 | 11 | 11 | |
| Other | 4 | 4 | 5 | 4 | 3 | 3 | |
| Enrollment city, % | .06 | ||||||
| City D | 66 | 54 | 67 | 68 | 67 | 65 | |
| City E | 34 | 46 | 33 | 32 | 33 | 35 | |
| Insurance, % | .44 | ||||||
| None | 15 | 15 | 16 | 15 | 15 | 16 | |
| Public | 48 | 57 | 50 | 47 | 45 | 49 | |
| Private | 35 | 28 | 33 | 36 | 39 | 35 | |
| Unknown | 1 | 0 | 1 | 2 | 1 | 1 | |
| Clinical presentation, % | |||||||
| Onset to admission, d, median (IQR) | 4 (2–7) | 4 (2–7) | 4 (1–9) | 4 (2–7) | 4 (2–7) | 4 (2–7) | .7 |
| Altered mental status | 7 | 16 | 8 | 8 | 6 | 3 | <.01 |
| Wheezing | 28 | 25 | 24 | 26 | 30 | 46 | <.01 |
| Tachypneab | 15 (n = 2285) |
12 (n = 110) |
15 (n = 711) |
12 (n = 629) |
14 (n = 606) |
23 (n = 229) |
<.01 |
| Tachycardiac | 48 (n = 2276) |
50 (n = 109) |
50 (n = 706) |
46 (n = 628) |
48 (n = 606) |
48 (n = 227) |
.71 |
| Hypotensiond | 20 (n = 2284) |
24 (n = 110) |
23 (n = 711) |
20 (n = 627) |
19 (n = 606) |
14 (n = 230) |
.02 |
| Hypoxiae | 26 (n = 2275) |
28 (n = 110) |
26 (n = 707) | 23 (n = 627) |
26 (n = 602) | 30 (n = 220) | .32 |
| Radiographic characteristics, % | |||||||
| Consolidation | 62 | 73 | 64 | 63 | 60 | 54 | <.01 |
| Infiltrate | 40 | 33 | 40 | 40 | 39 | 45 | .2 |
| Pleural effusion | 31 | 36 | 34 | 31 | 28 | 22 | <.01 |
| Chronic conditions, % | 79 | 78 | 76 | 77 | 81 | 84 | .04 |
| Asthma | 26 | 24 | 21 | 24 | 28 | 41 | <.01 |
| COPD | 23 | 37 | 24 | 20 | 21 | 26 | <.01 |
| Heart disease | 35 | 25 | 34 | 35 | 39 | 37 | .03 |
| Diabetes | 26 | 9 | 18 | 24 | 34 | 44 | <.01 |
| Immunosuppression/ HIV | 19 | 26 | 20 | 20 | 16 | 18 | .04 |
| Cancer | 18 | 21 | 22 | 18 | 16 | 10 | <.01 |
| Neurological disease | 11 | 13 | 13 | 12 | 8 | 9 | .04 |
| Current smoker, % | 26 | 34 | 31 | 23 | 23 | 23 | <.01 |
| PSI class, median (IQR) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 2 (2–3) | <.01 |
| PSI class, % | <.01 | ||||||
| 1–3 (low) | 65 | 54 | 59 | 64 | 67 | 83 | |
| 4 (moderate) | 26 | 35 | 28 | 27 | 26 | 16 | |
| 5 (high) | 9 | 11 | 13 | 9 | 7 | 2 | |
| CURB-65, median (IQR) | 1 (0–2) | 1 (0–2) | 1 (0–2) | 1 (0–2) | 1 (0–2) | 0 (0–1) | <.01 |
| CURB-65 class, % | <.01 | ||||||
| Low (0–1 points) | 69 | 54 | 67 | 68 | 71 | 80 | |
| Moderate (2 points) | 19 | 30 | 19 | 20 | 18 | 17 | |
| High (5 points) | 11 | 16 | 14 | 12 | 11 | 4 | |
Abbreviations: COPD, chronic obstructive pulmonary disease; HIV, human immunodeficiency virus; IQR, interquartile range; PSI, Pneumonia Severity Score.
aUnivariate comparisons with P values by χ2 (count ≥ 5 in each cell) or Fisher exact test.
bTachypnea: respiratory rate >25 breaths/min.
cTachycardia: heart rate >100 beats/min.
dHypotension: systolic blood pressure <90 mm/Hg and diastolic blood pressure <60 mm Hg.
eHypoxia: oxygen saturation <92 or on oxygen at presentation.
In unadjusted analyses, compared with adults of normal weight, LOS >3 days was more common in adults who were underweight (48% vs 59%; OR, 1.57; 95% CI, 1.04–2.36) (Figure 2B); there were no other statistically significant differences. The proportion of adults admitted to ICU ranged from 19% in overweight to 26% in underweight adults. Mechanical ventilation ranged from 4% among adults who were either overweight or extremely obese to 9% among adults who were underweight. Seventy-three (3%) adults developed ARDS, including adults who were overweight (2%) and adults in each other category (4%). In-hospital death occurred in 5% of adults who were underweight, ranging between 2% and 3% in adults who were of normal weight, overweight, or obese; no deaths occurred among adults with extreme obesity.
In adjusted analyses, the odds of LOS >3 days were higher in adults who were underweight (aOR 1.59; 95% CI, 1.05–2.42) compared with normal weight (Table 4). BMI was not significantly associated with ICU admission, but odds of mechanical ventilation were lower among adults who were overweight (aOR, 0.51; 95% CI, .31–.85).
Table 4.
Odds Ratios and Confidence Intervals for Hospital Length of Stay, Intensive Care Unit Admission, and Invasive Mechanical Ventilation by Body Mass Index Category Among Adults Hospitalized With Community-Acquired Pneumonia Adjusted for Demographics, Select Chronic Conditions, and Etiologya
| Outcome | BMI Category | Adjustedb | Adjusted With Etiologyc | ||||
|---|---|---|---|---|---|---|---|
| % With Outcome (n = 2285) | OR (95% CI) | P Value | % With Outcome (n = 2224) | OR (95% CI) | P Value | ||
| Hospital length of stay >3 d | |||||||
| Underweight | 59 | 1.59 (1.05–2.42) | .03 | 59 | 1.65 (1.08–2.53) | .02 | |
| Normal | 48 | ref | 47 | ref | |||
| Overweight | 48 | 0.97 (.78–1.21) | .80 | 48 | 1.00 (.80–1.26) | .97 | |
| Obesity | 46 | 0.96 (.77–1.20) | .73 | 46 | 0.99 (.78–1.25) | .93 | |
| Extreme obesity | 52 | 1.31 (.95–1.80) | .10 | 51 | 1.36 (.98–1.88) | .07 | |
| Intensive care unit admission | |||||||
| Underweight | 26 | 1.29 (.80–2.06) | .29 | 26 | 1.27 (.78–2.06) | .34 | |
| Normal | 23 | ref | 23 | ref | |||
| Overweight | 19 | 0.80 (.61–1.04) | .10 | 19 | 0.80 (.61–1.07) | .13 | |
| Obesity | 22 | 0.96 (.73–1.25) | .74 | 22 | 0.97 (.74–1.29) | .86 | |
| Extreme obesity | 19 | 0.87 (.58–1.29) | .48 | 19 | 0.91 (.60–1.36) | .63 | |
| Invasive mechanical ventilation | |||||||
| Underweight | 9 | 1.43 (.69–2.98) | .34 | 8 | 1.32 (.60–2.91) | .49 | |
| Normal | 7 | ref | 7 | ref | |||
| Overweight | 4 | 0.51 (.31–.85) | .009 | 4 | 0.52 (.31–.88) | .02 | |
| Obesity | 5 | 0.73 (.45–1.18) | .20 | 5 | 0.74 (.45–1.22) | .24 | |
| Extreme obesity | 4 | 0.69 (.33–1.43) | .32 | 4 | 0.78 (.37–1.65) | .52 | |
Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio.
aAll comparisons were with the normal weight category.
bAdjusted adult logistic regression models were controlled for age group, sex, race/ethnicity, enrollment city, history of asthma, heart disease, immunosuppression, cancer (excluding dermatological malignancies), neurological conditions, chronic obstructive pulmonary disease, diabetes, and current smoking status.
cAdjusted models with etiology were adjusted for all the factors mentioned above as well as for the presence or absence of bacterial, atypical bacterial (Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Legionella species), or viral etiology.
While no significant interaction terms were observed between age, or PSI and BMI in the adult models, in age-stratified analysis, the association between being underweight and longer LOS was significant only among adults aged 50–64 years (Supplementary Table 2). Odds of ICU admission were higher in adults 18–49 years who were underweight (aOR, 2.70 95% CI, 1.06–6.86), and lower in adults ≥65 years who were overweight (aOR, 0.58; 95% CI, .38–.87). When stratified by PSI, the association between extreme obesity and longer LOS was significant among adults with low PSI (aOR, 1.67; 95% CI, 1.16–2.41) (Supplementary Table 2).
Etiology
A pathogen was detected in 819 of 1065 (77%) children with specimens collected: viruses in 63% and bacteria in 21% (Supplementary Table 3). Prevalence was similar across all BMI categories for most pathogens. Respiratory syncytial virus (RSV) was detected in 17% of children: 23% in underweight, 12% in overweight, and 12% in children with obesity (P = .03). Parainfluenza virus was detected in 6% of children, more commonly in the underweight (11%) (P = .03).
A pathogen was detected in 845 of 2230 (38%) adults with specimens collected: viruses in 26% and bacteria in 14% (Supplementary Table 4). Prevalence was similar across all BMI categories for most pathogens. Streptococcus pneumoniae was detected in 5% of adults: 7% in underweight and normal adults, and 2% in adults with extreme obesity (P = .04). The addition of etiology (bacterial, atypical, or viral) to pediatric and adult models for LOS, ICU admission, and mechanical ventilation yielded similar results to models without etiology (Tables 2 and 4; Supplementary Tables 1 and 2).
DISCUSSION
Compared with normal-weight children, children who were overweight or obese experienced more severe CAP outcomes, including ICU admission among those who were overweight or obese, and mechanical ventilation among those with obesity. In stratified analyses, the association between elevated BMI and more severe outcomes was only apparent in children with asthma. In contrast, we did not observe an association between elevated BMI and severe outcomes in adults; rather, underweight adults had longer LOS than those with normal weight.
Few epidemiologic studies have examined the impact of BMI on respiratory infections in children. A cross-sectional study of 1129 children in Poland found that children who were overweight were at higher risk for acute upper respiratory tract infections [31]. Another observational study of 1746 children seen in an emergency department in Oklahoma found that children who were underweight with lower respiratory tract infections including pneumonia were more likely to be admitted than children with normal weight [21]. Being underweight was also associated with hospitalization but not mortality during the 2009 H1N1 pandemic [5]. In our study of children hospitalized with CAP, being underweight was not associated with severe outcomes. However, children who were overweight or obese were more likely to be admitted to the ICU and children with obesity were more likely to require mechanical ventilation. With only 2 pediatric deaths, we could not examine the association between BMI and death.
More than 40% of children in our study had asthma, which was most common among children who were overweight (48%) or obese (46%). Among children with asthma, being underweight or obese was associated with longer LOS, and asthma and obesity were associated with ICU admission and mechanical ventilation. No significant associations were found in children without asthma. Several hypotheses exist regarding the association between obesity and asthma. Obesity-related inflammation, chest wall restriction, or other comorbidities may play a role in development of asthma [32]; these same mechanisms may play a role in CAP severity among people with asthma and obesity. Further studies exploring the relationship between obesity, asthma, and CAP severity are warranted.
We found no significant differences in ICU admission by BMI category among adults hospitalized with CAP, but adults who were underweight had longer LOS than those with normal weight. In addition, while only 6% of adults in our study required mechanical ventilation, mechanical ventilation was significantly less common among adults who were overweight. Strict exclusion criteria and difficulties in enrolling older patients, including those who required mechanical ventilation, may have contributed to the low mortality observed in the EPIC study [24, 25] and thus associations between BMI and mortality are difficult to assess. However, our data are consistent with other studies which suggest that while low BMI may impact the course of illness associated with CAP, neither low nor high BMI is associated with severe outcomes among adults hospitalized with CAP. A study using a large administrative dataset reported no significant difference in ICU admission or mechanical ventilation by BMI category [16], but demonstrated that being underweight was associated with an increased risk, and being obese was associated with a decreased risk of 90-day mortality. A prospective Canadian cohort study of 907 adults hospitalized with pneumonia found no association between ICU admission and BMI [15]; however, in-hospital mortality was highest among the adults who were underweight whereas those with obesity were less likely to die [15]. Among 1079 adults hospitalized with CAP in the United Kingdom, no significant difference in immediate requirement for mechanical ventilation or inotropic support by BMI category was seen; however, obesity was associated with a reduced risk of 30-day mortality [18].
Other studies have also found that the risk of mortality in CAP decreased with higher BMI [9, 14, 17], a phenomenon often referred to as the “obesity survival paradox.” In our study, the overall in-hospital mortality ranged from 2% among adults who were overweight to 3% among the normal weight or obese to 5% among the underweight; however, these differences were not statistically significant after controlling for confounders (data not shown). Our overall mortality was lower than that from other studies (9%–18%), which reported a statistically significant association between lower BMI and mortality [14–16, 18]. One potential explanation for why adults who were underweight or extremely obese were not more likely to require ICU admission or mechanical ventilation, and why adults with obesity in other studies had lower mortality, is that these patients may be more likely to be admitted to the hospital even when presenting with milder disease than patients with normal weight. However, since admission PSI and CURB-65 scores were similar in all BMI groups, with the exception of those with extreme obesity whose scores were lower, this explanation may apply only to adults with extreme obesity in our study; it is possible that there is a different threshold for admission in this group.
Studies exploring interactions between BMI and CAP highlight the complexity of the relationship. Both human and animal studies have suggested immune function impairment in individuals who are underweight [33, 34] or obese [35–37]. In people who are underweight, immune function impairment may occur from coexisting chronic conditions, which we adjusted for in this analysis. Among those with obesity, adipose tissue that accumulates around the chest may decrease lung compliance and increase the risk of airway closure and ventilation-perfusion mismatch [38]. However, cytokines, such as leptin, from adipose tissue may have an anti-inflammatory effect. Mouse studies show that leptin deficiency was associated with reduced bacterial clearance and increased mortality [39, 40]; increasing leptin levels improved bacterial clearance and survival [39].
This study has limitations. First, height and weight were collected for the majority (86% of children and 99% of adults) but not all patients. Second, although obtained through medical chart abstraction, some height and weight values may have been self-reported, which may have underestimated the actual BMI, leading to misclassification bias [41, 42]. Third, few patients were represented in certain strata, limiting interpretation of stratified analyses. In addition, the low number of deaths precluded examination of the relationship between BMI and mortality. Last, while adjusted for potential confounders, our results may be subject to bias due to unmeasured factors, and residual confounding cannot be ruled out.
In this large prospective study of children and adults hospitalized with CAP, children who were overweight or obese experienced more severe outcomes than those of normal weight, including ICU admission in the overweight and obese, and mechanical ventilation in obese children. Asthma was an important effect modifier that needs further study. In contrast, while adults who were underweight had longer LOS, neither low nor high BMI was associated with ICU admission or mechanical ventilation. Our findings underscore the complexity of the relationship between BMI and CAP outcomes during hospitalization with CAP. Further studies exploring the mechanisms of BMI-associated modulation of the immune response and the impact on clinical outcomes of patients hospitalized with CAP are warranted.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Notes
Acknowledgments. We thank the patients who graciously consented to participate in this study and all members of the Etiology of Pneumonia in the Community (EPIC) Study Team for their contributions.
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official views of the US Centers for Disease Control and Prevention (CDC).
Financial support. This work was supported by the Influenza Division in the National Center for Immunization and Respiratory Diseases at the CDC through cooperative agreements with each study site and was based on a competitive research funding opportunity.
Potential conflicts of interest. W. H. S. reports grants from bioMérieux, Affinium Pharmaceuticals, Astute Medical, BRAHMS GmbH/Thermo Fisher, Pfizer, Rapid Pathogen Screening, Venaxis, BioAegis Inc, Sphingotec GmbH, and Ferring Pharmaceuticals and personal fees from BioFire Diagnostics, Venaxis, Inc, Abbott Point of Care, and Cempra Pharmaceuticals. E. J. A. reports personal fees from AbbVie, grants and nonfinancial support from MedImmune, and grants from Regeneron and Novavax. R. B. reports grants from bioMérieux, and has served as a scientific advisor for bioMérieux, Thermo Fisher Scientific, and Roche Scientific. C. S. was supported by grants from Merck, the Thrasher Research Fund, and the Primary Children’s Hospital Foundation. A. T. P. reports grants from the National Institute of Allergy and Infectious Diseases/BioFire, royalties as Editor of the Sanford Guide from Antimicrobial Therapy Inc, and personal fees from WebMD, Alios/Johnson, and Johnson Pharmaceuticals. K. M. E. reports serving on a data and safety monitoring board for Novartis for which her institution receives fees. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief 2015; 1–8. [PubMed] [Google Scholar]
- 2. Kwong JC, Campitelli MA, Rosella LC. Obesity and respiratory hospitalizations during influenza seasons in Ontario, Canada: a cohort study. Clin Infect Dis 2011; 53:413–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fezeu L, Julia C, Henegar A et al. Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: a systematic review and meta-analysis. Obes Rev 2011; 12:653–9. [DOI] [PubMed] [Google Scholar]
- 4. Louie JK, Acosta M, Samuel MC et al. A novel risk factor for a novel virus: obesity and 2009 pandemic influenza A (H1N1). Clin Infect Dis 2011; 52:301–12. [DOI] [PubMed] [Google Scholar]
- 5. Morgan OW, Bramley A, Fowlkes A et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PLoS One 2010; 5:e9694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Watt JP, O’Brien KL, Benin AL et al. Risk factors for invasive pneumococcal disease among Navajo adults. Am J Epidemiol 2007; 166:1080–7. [DOI] [PubMed] [Google Scholar]
- 7. Baik I, Curhan GC, Rimm EB, Bendich A, Willett WC, Fawzi WW. A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women. Arch Intern Med 2000; 160:3082–8. [DOI] [PubMed] [Google Scholar]
- 8. Phung DT, Wang Z, Rutherford S, Huang C, Chu C. Body mass index and risk of pneumonia: a systematic review and meta-analysis. Obes Rev 2013; 14:839–57. [DOI] [PubMed] [Google Scholar]
- 9. Nie W, Zhang Y, Jee SH, Jung KJ, Li B, Xiu Q. Obesity survival paradox in pneumonia: a meta-analysis. BMC Med 2014; 12:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Braun ES, Crawford FW, Desai MM et al. Obesity not associated with severity among hospitalized adults with seasonal influenza virus infection. Infection 2015; 43:569–75. [DOI] [PubMed] [Google Scholar]
- 11. Almirall J, Bolíbar I, Serra-Prat M et al. ; Community-Acquired Pneumonia in Catalan Countries (PACAP) Study Group New evidence of risk factors for community-acquired pneumonia: a population-based study. Eur Respir J 2008; 31:1274–84. [DOI] [PubMed] [Google Scholar]
- 12. Inoue Y, Koizumi A, Wada Y et al. Risk and protective factors related to mortality from pneumonia among middle aged and elderly community residents: the JACC Study. J Epidemiol 2007; 17:194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schnoor M, Klante T, Beckmann M et al. ; CAPNETZ Study Group Risk factors for community-acquired pneumonia in German adults: the impact of children in the household. Epidemiol Infect 2007; 135:1389–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Corrales-Medina VF, Valayam J, Serpa JA, Rueda AM, Musher DM. The obesity paradox in community-acquired bacterial pneumonia. Int J Infect Dis 2011; 15:e54–7. [DOI] [PubMed] [Google Scholar]
- 15. Kahlon S, Eurich DT, Padwal RS et al. Obesity and outcomes in patients hospitalized with pneumonia. Clin Microbiol Infect 2013; 19:709–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. King P, Mortensen EM, Bollinger M et al. Impact of obesity on outcomes for patients hospitalised with pneumonia. Eur Respir J 2013; 41:929–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. LaCroix AZ, Lipson S, Miles TP, White L. Prospective study of pneumonia hospitalizations and mortality of U.S. older people: the role of chronic conditions, health behaviors, and nutritional status. Public Health Rep 1989; 104:350–60. [PMC free article] [PubMed] [Google Scholar]
- 18. Singanayagam A, Singanayagam A, Chalmers JD. Obesity is associated with improved survival in community-acquired pneumonia. Eur Respir J 2013; 42:180–7. [DOI] [PubMed] [Google Scholar]
- 19. Kornum JB, Nørgaard M, Dethlefsen C et al. Obesity and risk of subsequent hospitalisation with pneumonia. Eur Respir J 2010; 36:1330–6. [DOI] [PubMed] [Google Scholar]
- 20. Hedlund J, Hansson LO, Ortqvist A. Short- and long-term prognosis for middle-aged and elderly patients hospitalized with community-acquired pneumonia: impact of nutritional and inflammatory factors. Scand J Infect Dis 1995; 27:32–7. [DOI] [PubMed] [Google Scholar]
- 21. Wyrick S, Hester C, Sparkman A et al. What role does body mass index play in hospital admission rates from the pediatric emergency department? Pediatr Emerg Care 2013; 29:974–8. [DOI] [PubMed] [Google Scholar]
- 22. Griffin MR, Zhu Y, Moore MR, Whitney CG, Grijalva CG. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med 2013; 369:155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2010. Natl Vital Stat Rep 2013; 61:1–117. [PubMed] [Google Scholar]
- 24. Jain S, Self WH, Wunderink RG et al. ; CDC EPIC Study Team Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med 2015; 373:415–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jain S, Williams DJ, Arnold SR et al. ; CDC EPIC Study Team Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med 2015; 372:835–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fine MJ, Auble TE, Yealy DM et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:243–50. [DOI] [PubMed] [Google Scholar]
- 27. Lim WS, van der Eerden MM, Laing R et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003; 58:377–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kuczmarski RJ, Ogden CL, Guo SS et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11 2002; 1–190. [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention. A SAS program for the 2000 CDC growth charts (ages 0 to <20 years) 2016. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed 10 February 2017.
- 30. World Health Organization. Physical status: the use and interpretation of anthropometry Report of a WHO expert committee. World Health Organization technical report series; 1995; 854: 1–452. [PubMed] [Google Scholar]
- 31. Jedrychowski W, Maugeri U, Flak E, Mroz E, Bianchi I. Predisposition to acute respiratory infections among overweight preadolescent children: an epidemiologic study in Poland. Public Health 1998; 112:189–95. [DOI] [PubMed] [Google Scholar]
- 32. Lang JE. Obesity, nutrition, and asthma in children. Pediatr Allergy Immunol Pulmonol 2012; 25:64–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Allende LM, Corell A, Manzanares J et al. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology 1998; 94:543–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ritz BW, Gardner EM. Malnutrition and energy restriction differentially affect viral immunity. J Nutr 2006; 136:1141–4. [DOI] [PubMed] [Google Scholar]
- 35. Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis 2006; 6:438–46. [DOI] [PubMed] [Google Scholar]
- 36. Karlsson EA, Beck MA. The burden of obesity on infectious disease. Exp Biol Med 2010; 235:1412–24. [DOI] [PubMed] [Google Scholar]
- 37. Tsatsanis C, Margioris AN, Kontoyiannis DP. Association between H1N1 infection severity and obesity–adiponectin as a potential etiologic factor. J Infect Dis 2010; 202:459–60. [DOI] [PubMed] [Google Scholar]
- 38. Salome CM, King GG, Berend N. Physiology of obesity and effects on lung function. J Appl Physiol (1985) 2010; 108:206–11. [DOI] [PubMed] [Google Scholar]
- 39. Hsu A, Aronoff DM, Phipps J, Goel D, Mancuso P. Leptin improves pulmonary bacterial clearance and survival in ob/ob mice during pneumococcal pneumonia. Clin Exp Immunol 2007; 150:332–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wieland CW, Stegenga ME, Florquin S, Fantuzzi G, van der Poll T. Leptin and host defense against gram-positive and gram-negative pneumonia in mice. Shock 2006; 25:414–9. [DOI] [PubMed] [Google Scholar]
- 41. Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. Arch Pediatr Adolesc Med 2007; 161:1154–61. [DOI] [PubMed] [Google Scholar]
- 42. Clarke P, Sastry N, Duffy D, Ailshire J. Accuracy of self-reported versus measured weight over adolescence and young adulthood: findings from the National Longitudinal Study of Adolescent Health, 1996–2008. Am J Epidemiol 2014; 180:153–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.