Abstract
Objectives
In evaluating the historical context of the first description of Menière’s disease, its association with migraine headaches is compelling. We have outlined the events and observations of Prosper Menière, which led him to establish a link between migraine headaches and his eponymous disease.
Study Design
Prosper Menière’s original French writings were translated by our group and used to recount his observations and thoughts. Miles Atkinson’s English translations were used as a reference. Additional otological texts of the era were also reviewed as it relates to Menière’s disease.
Methods
Prosper Menière wrote a series of four papers one year before his death. In one of these papers, he makes references to migraine headaches on several occasions. These original writings were analyzed, and the physical findings he described were interpreted based on their relation to migraine headaches.
Results
The passages in his published papers provide historical insight into Menière’s observations. His writings describe in detail symptoms of migraine headaches uniquely evident in his patient population. Through his observations, he recognized that in addition to exhibiting symptoms of tinnitus, hearing loss and vertigo his patients also suffered from migraine headaches.
Conclusions
Although his colleagues discounted Menière’s theory concerning migraine headaches, he continued to make deductive inferences and publish his findings, leading to the association of migraine headaches and Menière’s disease. Today, this association continues to be debated, adding to Prosper Menière’s legacy.
Keywords: Historical, Menière, Menière’s disease, migraine, headache, ear, dizziness, vestibular migraine
Introduction
In 1861, Prosper Menière (figure 1) described in a series of four papers a group of symptoms that later became known as Menière’s disease.1, 2,3,4 His observations made him the first to recognize the symptomatic triad, which includes vertigo, tinnitus and sensorineural hearing loss, as a single unifying syndrome sharing a common etiology.5
Figure 1.
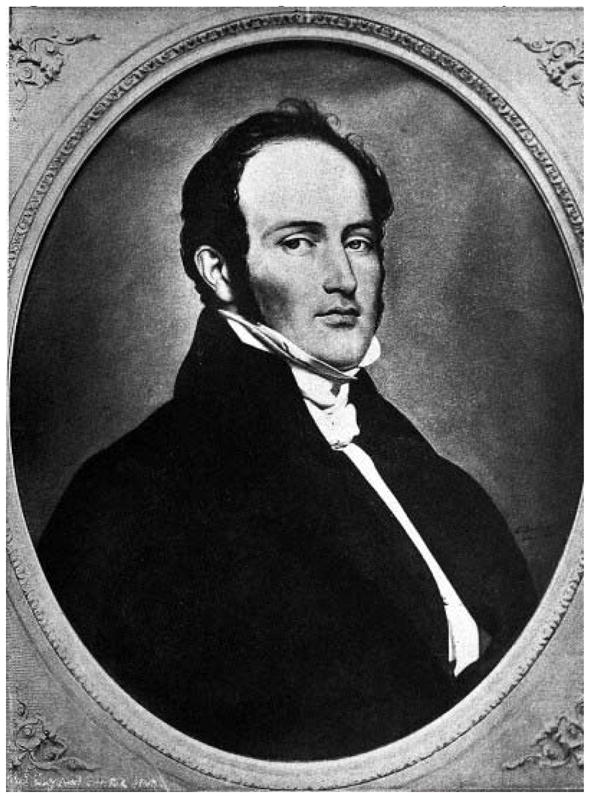
Portrait of Prosper Menière drawn by Bodinier in 1833. 45
According to the current American Academy of Otolaryngology- Head and Neck Surgery (AAO-HNS) criteria, Menière’s disease is diagnosed clinically based on the presence of vertigo, tinnitus and hearing loss.6 However, these criteria do not include a fourth symptom observed and described in Menière’s original writing, migraine headaches. More recently, the significant overlap between migraine headaches and Menière’s disease has prompted consideration of a common etiology between the two – an idea Menière had contemplated.7, 8 This paper examines Menière’s original description of migraine headaches and their relationship to the triad of symptoms in Menière’s disease.
The recognition of migraines and its association with hearing and balance was first identified by Aretaeus of Cappadocia in the second century in Rome.9 It was at this time in which the pathophysiology of migraine headaches was re-explored. Interestingly, in 1856, Aretaeus’ work was translated from Greek to English four years prior to Menière’s publication. Prior to this, German-born physician Emil du Bois-Reymond and Mauritian Charles-Edouard Brown-Séquard were the first to publish theories on the pathophysiology of migraines in 1860 and 1861 respectively. Brown-Séquard publically refuted du Bois-Reymond’s claims that migraines were the result of sympathetic changes on blood vessels, which he suggested could better explain seizures rather than migraines.10 During this era, two schools of thoughts on the etiology of migraines predominated. One group considered the source of migraines to lie within the central nervous system, while the other believed the etiology to be of vascular origin secondary to vasoconstriction or vasodilation.10, 11 At the time of Menière’s publication, these discrepant theories undoubtedly impacted his predictions and writings. Within the context of this debate, Menière contributed by suggesting that one etiology of migraines can lie within the inner ear.
Methods
We examined Miles Atkinson’s English translations of Menière’s original four papers, in addition to our group’s translations of Menière’s original writing (figure 2). Specifically, we analyzed the content and context of Menière’s writing for any description of migraine or headaches in his patients and their relationship to tinnitus, vertigo and hearing loss. In addition, we reviewed pertinent writings of otologistswho were contemporaries of Menière’s as they related to the disease to determine the context in which these new ideas were being propagated.
Figure 2.
Figure 2a: Original cover to Gazette Medicale published in 1861.46 This edition contains the original writings of Prosper Menière’s work, which includes the first mention of migraine headaches as it relates to Menière’s disease.
Figure 2b: Original French writing as published in Gazette Medicale in 1861of Prosper Menière’s famous article entitled Pathologie Auriculaire.4, 46 The first two pages of his article are included with the direct reference to migraine headaches demarcated on the second page.
Results
Prosper Menière’s first description of migraine headaches is focused on their association with the triad of tinnitus, vertigo, and hearing loss.
Excerpt one: “I do not hesitate to regard these migraines as dependent upon a lesion of the inner ear; they are accompanied by noises, by vertigo, by gradual diminution of hearing…”12
Later in his writing, Menière describes a patient experiencing what seems to be a migraine-related visual aura.
Excerpt two: “The faces of [the patient’s] parents seemed to him covered by a greyish veil.”12
Menière continues to elaborate on the presence of migraine headaches in his patients by proposing a relationship between migraine headaches, tinnitus, vertigo, and hearing loss.
Excerpt three: “If it is incontestable that individuals who are a prey to vertigo with syncope and vomiting have at the same time head noises and rapidly become deaf, it is not less certain that cerebral states, called migraine, give place in the end to similar attacks, and the deafness which arises in these circumstances would seem to us inevitably to be related to a disease of the same nature.”12
In order to bolster his theory, Menière notes that although migraine headaches are common, their incidence in these patients is unlikely to be a coincidence.
Excerpt four: “Persons affected with chronic migraine are so numerous in the world, it is easy to assume oneself of their state of hearing, that it should soon be possible to be conceived of the truth of the fact that we have established as a result a mass of perfectly conclusive observations.”12
Furthermore, Menière concedes that not all migraine headaches are necessarily associated with hearing loss or deficits of the inner ear.
Excerpt five: “It is, of course, understood that we do not regard every case of hemicranias as dependent upon a disorder of the inner ear; one knows only too well how often the same symptoms can arise from different causes; but we believe that it can be asserted that many so-called migraines are only the index of a morbid process leading infallibly to deafness.”12
In addition to auras, Menière describes a drop attack seen in a patient with migraine headaches comorbid with Menière’s disease.
Excerpt six: “Suddenly she felt… ‘a rush of blood’ to the left ear. She was seized at the same time with an attack of syncope but without nausea”12
Menière also specifically describes the details of the vertigo as described by the patient.
Excerpt seven: “...the patient was carried to his bed completely helpless. Consciousness returned…everything in the room seemed to be turning, the patient said that he was seasick, he clung to his bed as if fearing that he would be thrown out..”12
Menière also continues to describe the ear fullness commonly experienced by the patient.
Excerpt eight: “…there was in the left occipito-mastoid region a feeling of weight, of pressure…” 12
Menière also describes the unique nature of hearing loss experienced by the patient.
Excerpt nine: “…but it was soon noticed that his hearing was diminishing, particularly on the left…”12
Moreover, Menière’s writings elucidate his effort to explain the etiology of migraine and associated symptoms by comparing symptoms of patients after sustaining physical trauma.
Excerpt ten: “Perforations of the drum, produced by an external cause, …do not give rise to the attacks of which we have just been speaking.”12
Lastly, Menière invites his peers to examine these migraine-suffering patients for themselves.
Excerpt eleven: “if such an assertion should seem [too] astonishing…we would beg our colleagues to direct their research along the lines which we have indicated.”12
Discussion
In his writings, Menière noted that migraine headaches were repeatedly present in his patients with vertigo, tinnitus and hearing loss. In excerpt 1, Menière proposes a common etiology between migraine headaches and the symptomatic triad of Menière’s disease. Menière’s observations allowed him to deduce that migraine headaches were a unique symptom present in parallel with, but not consequential to, the triad of symptoms of Menière’s disease.
Furthermore, Menière’s descriptions support his clinical judgment of his patients suffering specifically from migraine headaches. In excerpt 2, Menière describes a patient that could possibly be experiencing a visual aura, a symptom classically associated with migraine headaches.13 Those with migraine aura can suffer from a color perception aberration.14 It has been observed that migraine sufferers with aura have difficulty distinguishing red and blue colors.15 Alternatively, the description is also consistent with a patient suffering from a scotoma, another symptom commonly experienced during migraine headaches.16 The inability to perceive faces due to a scotoma could be interpreted as having a “greyish veil” in the visual field. Although impossible to determine with certainty from what the patient was suffering, migraine headache with aura is a likely diagnosis. Moreover in excerpt 6, Menière discusses a patient suffering from syncope, or “drop attacks.” Drop attacks, or “crisis of Tumarkin,” was originally thought to be an independent inner ear condition separate from Menière’s disease.17 However, based on our observations and those of Menière himself, in addition to the known link between migraine and drop attacks, this likely represents a migraine related problem.18 Interestingly, the link between migraine headaches and syncope is also well established, bolstering Menière’s clinical diagnosis of migraine headaches in his patients.19,20
The constellation of tinnitus, vertigo and hearing loss is repeatedly present in Menière’s writings describing his namesake disease. However, migraine headaches are not currently part of the diagnostic criteria for Menière’s disease. Menière reasoned that although migraine headaches experienced by patients in isolation are not linked to the group of inner ear symptoms, when present in conjunction with tinnitus, vertigo and hearing loss, he argues that a common etiology linking the symptoms exists [excerpt 3]. Furthermore, in excerpt 4, Menière questions whether the presence of migraine headaches in his patients was inconsequential, or indicative of a clinically significant pattern in his patients. Menière suggests that the consistent presentation of migraine headaches in his patients makes them unlikely to be comorbidities. Rather, he suggests they are a distinctive component of the syndrome later coined Menière’s disease with all symptoms sharing a common etiology. Excerpt 5 further supports Menière’s proposition that migraine headaches share a common etiology with tinnitus, vertigo and hearing loss when present in patients. Menière concedes however, that not all cases of isolated migraine headaches are necessarily linked to inner ear pathology.
Menière’s description of vertigo in excerpt 7 is significant since various pathologies can cause vertigo. Notably, distinguishing between vestibular migraine and Menière’s has been difficult to this day. With present-day knowledge, it is possible that Menière may have incorrectly diagnosed his patients who might actually have been suffering from vestibular migraines. This however is unlikely. As illustrated in excerpt 7, Menière’s description of vertigo is one of true spinning vertigo in which the patient describes the room spinning, which is a known feature of Menière’s vertigo.21 This is in contrast to dizziness experienced in vestibular migraine, which is often described as dysequilibrium.22 Despite not having the modern audiometry to document symptoms of hearing loss, Menière continued to detect and describe hearing loss according to empirical documentation of patient accounts and describe symptoms unique to the classic presentation of Menière’s disease. This is designated by both excerpts 8 and 9 which depict unilateral fullness and hearing loss, symptoms that are more common in Menière’s disease, especially in the early stages of the disease.23 These detailed descriptions of symptoms described by Menière, are highly consistent with the view that he was indeed documenting Menière’s disease and not vestibular migraines.
Menière not only identified symptoms of Menière’s disease but also sought to understand the pathophysiological mechanisms responsible for these manifestations. Drawing from his clinical experience in treating patients with otologic trauma, Menière noted that trauma to the inner ear that presumably results in a perilymphatic fistula could mimic the symptoms experienced by his patients [excerpt 10]. Menière’s writings suggested that he ruled out physical trauma as the cause of his patients’ symptoms and proposed that intrinsic changes of the inner ear were the primary cause. This was an innovative proposition, and Menière acknowledged that it would seem implausible to most. In excerpt 11, Menière advocates that if his colleagues meet his observations with skepticism, they are welcome to observe his patients for themselves.
Menière’s colleagues took note of his work, which led to discussion amongst his contemporaries. In a paper published by Armand Trousseau following Menière’s presentation, he mentions Menière’s work, and does mention headache and migraines but not as it relates to vertigo.24 Additionally, Menière’s response letter to Trousseau, includes no mention of headaches.12 Later in 1874, Trousseau mentions Menière’s observations, and includes headaches as one of many symptoms, but does not elaborate or state that it is indeed migraine headache. 25
After Menière’s death in 1864, otologists Anton von Tröltsch, Adam Politzer, and Hermann Schwartze published the first volume of their journal entitled Archiv für Ohrenheilkunde.- a new journal dedicated to otology. In this journal, there are multiple articles authored by von Tröltsch, Schwartze and Arnold Pagenstecher referencing headaches in relation to recurrent vertigo in various contexts. 26–29
Furthermore, Menière’s influence on his colleagues is further strengthened by Adam Poltizer’s visits, as documented in biographies of both Poltizer and Menière.30,31 It is unknown what was discussed between them since the details are not documented nor presented in Menière’s journals.32 Nevertheless, five years after Menière’s death, Poltizer published a description of Menière’s disease, but does not make any reference to headache in his description of vertigo.33 In that same year, August Lucae, references Poltizer when describing a patient suffering from the classic symptoms of Menière’s disease – in this description he includes headaches as a symptom of the disease.34
Additionally, Liveing, who observed the connection between migraines and vertigo two years later in 1863–1865, published his findings in 1873.35 Despite this, the relationship between Menière’s and headache failed to receive further study until a century later first by Atkinson in 1962 and later Hincliffe in 1967.36, 37
The prevalence of migraine symptoms in conjunction with vertigo at the time of Menière’s findings is unclear, since a definitive connection between these entities is only recently being elucidated. Despite this, the publication of these findings in multiple journals and by various authors, the prevalence can be inferred. It is evident that headaches in the context of vertigo and hearing loss were not a rare occurrence.
Menière’s original proposal that migraine headaches are related to tinnitus, vertigo and hearing loss is not unanimously accepted. Migraine headache is not included in the diagnostic criteria for Menière’s disease.6, 38 At present, efforts to understand the pathophysiologic mechanisms underlying this association with headaches are on going. The existing mechanism of Menière’s disease is described as a change in both mechanical and chemical factors within the cochlea.39 However, the pathophysiological link between migraine headaches and Menière’s is less clear. It is suggested that activation of the trigeminal sensory neurons causes changes in vascular permeability of the cochlea, resulting in the symptoms of Menière’s disease.40 Others have characterized various pharmacological and physical maneuvers to treat the vertigo associated with Menière’s, but no therapy has been proven efficacious.41
Currently, Menière’s disease is diagnosed clinically according to the AAO-HNS criteria.6 The symptoms of vestibular migraine are diagnosed independently according to the International Headache Society.42 Despite this distinction, much overlap exists between these two diseases. Notably, vestibular migraines has been shown to present without any headache symptoms in 30% of cases.43 Interestingly, one study found that 51% of patients suffering from Menière’s also suffered from migraine headaches.44 In another, 45% of patients with Menière’s disease suffered at lease one migraine symptom.7
Menière spent his entire medical career attempting to join the French Imperial Academy of Medicine. Despite his prominence as a physician, he was rejected twice because he did not have enough votes. Menière was only given one opportunity to present his work, but very few academy members attended the presentation due to inclement weather.12 The presentation left the members unimpressed. In response, the committee members did not discuss his presentation, but rather, created a committee to revisit the subject - it is unknown if this committee ever met.12 Menière’s article received attention one week later when Trousseau, an academy member, referenced Menière’s work and brought the discussion to the forefront.24 Despite a lack of uniform consensus, Menière’s work has prompted the discussion of the link between migraine headaches and Menière’s disease, providing the impetus for investigating the relevant underlying pathophysiologic mechanisms of this association.
Footnotes
Authors have not received funding from any organization.
References
- 1.Menière P. Pathologie Auriculaire[in French] Gaz Med De Paris. 1861;16:88–89. [Google Scholar]
- 2.Menière P. Correspondance Medicale [in French] Gaz Med De Paris. 1861;16:239–240. [Google Scholar]
- 3.Menière P. Observations de maladies de L’oreille interne caracterisee par des symptomes de congestion apoplectiforme [in French] Gaz Med De Paris. 1861;16:379–380. [Google Scholar]
- 4.Menière P. Pathologie Auriculaire [in French] Gaz Med De Paris. 1861;16:597–601. [Google Scholar]
- 5.Mancini F, Catalani M, Carru M, Monti B. History of Menière’s disease and its clinical presentation. Otolaryngol Clin North Am. 2002;35(3):565–80. doi: 10.1016/s0030-6665(02)00017-8. [DOI] [PubMed] [Google Scholar]
- 6.Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Menière’s disease. American Academy of Otolaryngology-Head and Neck Foundation, Inc. Otolaryngol Head Neck Surg. 1995;113(3):181–5. doi: 10.1016/S0194-5998(95)70102-8. [DOI] [PubMed] [Google Scholar]
- 7.Radtke A, Lempert T, Gresty MA, Brookes GB, Bronstein AM, Neuhauser H. Migraine and Ménière’s disease: is there a link? Neurology. 2002;59(11):1700–4. doi: 10.1212/01.wnl.0000036903.22461.39. [DOI] [PubMed] [Google Scholar]
- 8.Rassekh CH, Harker LA. The prevalence of migraine in Menière’s disease. Laryngoscope. 1992;102(2):135–8. doi: 10.1288/00005537-199202000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Adams Francis., editor. The extant works of Aretaeus: the Cappadocian. Vol. 27. Sydenham Society; 1856. pp. 294–296. [Google Scholar]
- 10.Brown-Séquard CE. Remarques sur le travail précédent. J Phys Homme Animaux. 1861;4:137–9. [Google Scholar]
- 11.Dubois Reymond E. Zur Kenntniss der Hemikrania. Arch Anat Physiol Wissensch Med. 1860:461–468. [Google Scholar]
- 12.Menière P, Atkinson M. Méniére’s original papers: reprinted with an English translation together with commentaries and biographical sketch. Stockholm: ActaOto-laryngologica; 1961. [Google Scholar]
- 13.Rasmussen BK, Olesen J. Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia. 1992;12(4):221–8. doi: 10.1046/j.1468-2982.1992.1204221.x. [DOI] [PubMed] [Google Scholar]
- 14.Cutrer FM, Huerter K. Migraine aura. Neurologist. 2007;13(3):118–25. doi: 10.1097/01.nrl.0000252943.82792.38. [DOI] [PubMed] [Google Scholar]
- 15.De marinis M, Rinalduzzi S, Accornero N. Impairment in color perception in migraine with and without aura. Headache. 2007;47(6):895–904. doi: 10.1111/j.1526-4610.2007.00774.x. [DOI] [PubMed] [Google Scholar]
- 16.Odkvist LM, Bergenius J. Drop attacks in Menière’s disease. ActaOtolaryngol Suppl. 1988;455:82–5. doi: 10.3109/00016488809125064. [DOI] [PubMed] [Google Scholar]
- 17.Black FO, Effron MZ, Burns DS. Diagnosis and management of drop attacks of vestibular origin: Tumarkin’s otolithic crisis. Otolaryngol Head Neck Surg. 1982;90(2):256–62. doi: 10.1177/019459988209000221. [DOI] [PubMed] [Google Scholar]
- 18.Ishiyama G, Ishiyama A, Baloh RW. Drop attacks and vertigo secondary to a non-Menièreotologic cause. Arch Neurology. 2003;60(1):71–5. doi: 10.1001/archneur.60.1.71. [DOI] [PubMed] [Google Scholar]
- 19.Thijs RD, Kruit MC, Van buchem MA, Ferrari MD, Launer LJ, Van dijk JG. Syncope in migraine: the population-based CAMERA study. Neurology. 2006;66(7):1034–7. doi: 10.1212/01.wnl.0000204186.43597.66. [DOI] [PubMed] [Google Scholar]
- 20.Curfman D, Chilungu M, Daroff RB, Alshekhlee A, Chelimsky G, Chelimsky TC. Syncopal migraine. ClinAuton Res. 2012;22(1):17–23. doi: 10.1007/s10286-011-0141-7. [DOI] [PubMed] [Google Scholar]
- 21.Furman JM, Jacob RG. A clinical taxonomy of dizziness and anxiety in the otoneurological setting. Journal of anxiety disorders. 2001;15(1):9–26. doi: 10.1016/s0887-6185(00)00040-2. [DOI] [PubMed] [Google Scholar]
- 22.Stolte B, Holle D, Naegel S, Diener HC, Obermann M. Vestibular migraine. Cephalalgia. 2015;35(3):262–70. doi: 10.1177/0333102414535113. [DOI] [PubMed] [Google Scholar]
- 23.Sajjadi H, Paparella MM. Menière’s disease. Lancet. 2008;372(9636):406–14. doi: 10.1016/S0140-6736(08)61161-7. [DOI] [PubMed] [Google Scholar]
- 24.Trousseau A. De la congestion cérébrale apoplectiforme, dans ses rapports avec épilepsie. Gaz Med Paris. 1861;26:378–394. [Google Scholar]
- 25.Trousseau A. Vertigo ab aure laesa. Gaz des hop. 1874:73–76. [Google Scholar]
- 26.von Tröltsch A. Das Politzer’sche Verfahren zur Wegsammachung der Ohrtrompete. Arch Ohrenheil. 1864;1:28–43. [Google Scholar]
- 27.Schwartze H. Heber die sogenannte “Electro-Oliatrik” Brenncfs. Arch Ohrenheil. 1864;1:44–58. [Google Scholar]
- 28.Schwartze H. Beiträge zur Pathologie und palhol. Anatomie des Obres. Arch Ohrenheil. 1864;1:195–220. [Google Scholar]
- 29.Pagenstecher A. Zur Anbohrung des Warzenfortsatzes. Arch Ohrenheil. 1864;1:360–363. [Google Scholar]
- 30.Mudry A. The role of Adam Politzer (1835–1920) in the history of otology. Am J Otol. 2000;21(5):753–63. [PubMed] [Google Scholar]
- 31.Legent F, Gourevitch D, Verry E, Morgon AH, Michel O. Prosper Menière auriste et érudit 1799–1862. Paris: Flammarion; 1999. [Google Scholar]
- 32.Menière E. Journal du docteur Prosper Menière. Paris: Plon; 1903. [Google Scholar]
- 33.Politzer A. Ueber Laesion des Labyrinthes. Arch Ohrenheil. 1867;2:88–99. [Google Scholar]
- 34.Lucae A. Ohrenkrankheiten. Jahresbericht Über Die Leistungen Und Fortschritte in Der Gesammten Medicin. 1867;2:455–463. [Google Scholar]
- 35.Liveing E, Jelliffe SE. On Megrim, Sick-Headache, and Some Allied Disorders: a Contribution to the Pathology of Nerve-Storms. London: J. and A. Churchill; 1873. pp. 120–145. [Google Scholar]
- 36.Atkinson M. Migraine and Menière’s disease. Arch Otolaryngol. 1962;75:220–5. doi: 10.1001/archotol.1962.00740040228008. [DOI] [PubMed] [Google Scholar]
- 37.Hinchcliffe R. Headache and Menière’s disease. Acta Otolaryngol. 1967;63(4):384–90. doi: 10.3109/00016486709128772. [DOI] [PubMed] [Google Scholar]
- 38.Shepard Neil T. Differentiation of Menière’s Disease and Migraine-Associated Dizziness: A Review. J Am AcadAudiol. 2006;17:69–80. doi: 10.3766/jaaa.17.1.7. [DOI] [PubMed] [Google Scholar]
- 39.Paparella MM, Djalilian HR. Etiology, pathophysiology of symptoms, and pathogenesis of Menière’s disease. Otolaryngol Clin North Am. 2002;35(3):529–45. vi. doi: 10.1016/s0030-6665(02)00019-1. [DOI] [PubMed] [Google Scholar]
- 40.Vass Z, Steyger PS, Hordichok AJ, Trune DR, Jancsó G, Nuttall AL. Capsaicin stimulation of the cochlea and electric stimulation of the trigeminal ganglion mediate vascular permeability in cochlear and vertebro-basilar arteries: a potential cause of inner ear dysfunction in headache. Neuroscience. 2001;103(1):189–201. doi: 10.1016/s0306-4522(00)00521-2. [DOI] [PubMed] [Google Scholar]
- 41.Cesarani A, Alpini D, Monti B, Raponi G. The Treatment of Acute Vertigo. Neurol Sci. 2004;(Suppl 1):S26–30. doi: 10.1007/s10072-004-0213-8. [DOI] [PubMed] [Google Scholar]
- 42.The International Classification of Headache Disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 43.Strupp M, Versino M, Brandt T. Vestibular migraine. Handb Clin Neurol. 2010;97:755–71. doi: 10.1016/S0072-9752(10)97062-0. [DOI] [PubMed] [Google Scholar]
- 44.Ghavami Y, Mahboubi H, Yau AY, Maducdoc M, Djalilian HR. Migraine features in patients with Menière’s disease. Laryngoscope. 2015 doi: 10.1002/lary.25344. [DOI] [PubMed] [Google Scholar]
- 45.Wellcome Library, London. Wellcome Images. 1911. Prosper Menière, from a portrait painted by G. Bodinier Painting By: G. Bodinier Les collections artistiques de la faculte de medecine de Paris Noe Legrand Published. [Google Scholar]
- 46.Guerin J René, Baudouin M, Ranse F Henri. Gazette médicale de Paris v. 32. Paris: 1861. [Google Scholar]