Abstract
Background
Availability of the opioid antagonist naloxone for lay administration has grown substantially since first proposed in 1996. Gaps remain, though, in our understanding of how people who inject drugs (PWID) engage with naloxone programmes over time.
Aims
This paper aimed to address three specific evidence gaps: the extent of naloxone supply to PWID; supply-source (community or prisons); and the carriage of naloxone among PWID.
Materials and methods
Analysis of Scotland’s Needle Exchange Surveillance Initiative (NESI) responses in 2011–2012 and 2013–2014 was undertaken with a specific focus on the extent of Scotland’s naloxone supply to PWID; including by source (community or prisons); and on the carriage of naloxone. Differences in responses between the two surveys were measured using Chi-square tests together with 95% confidence intervals for rate-differences over time.
Results
The proportion of NESI participants who reported that they had been prescribed naloxone within the last year increased significantly from 8% (175/2146; 95% CI: 7–9%) in 2011–2012 to 32% (745/2331; 95% CI: 30% to 34%) in 2013–2014. In contrast, the proportion of NESI participants who carried naloxone with them on the day they were interviewed decreased significantly from 16% (27/169; 95% CI: 10% to 22%) in 2011–2012 to 5% (39/741; 95% CI: 4% to 7%) in 2013–2014.
Conclusions
The supply of naloxone to PWID has increased significantly since the introduction of a National Naloxone Programme in Scotland in January 2011. In contrast, naloxone carriage is low and decreased between the two NESI surveys; this area requires further investigation.
Keywords: Opioid, Overdose, Naloxone, Injecting, PWID, Prison
1. Introduction
Mortality rates among people who inject drugs (PWID) are much higher than in the general population (Mathers et al., 2013). Overdose is a major cause of premature death among PWID, opioid users in particular (Darke et al., 2006).
Since first conceptualised by Strang et al. (1996), distribution of the opioid antagonist naloxone for lay administration (henceforth referred to as ‘take-home naloxone’; THN) has developed into one of the main drug-related death (DRD) prevention strategies. In 2014, the World Health Organisation published guidelines recommending expansion of naloxone access to people likely to witness an overdose in their community and it is now supplied for lay administration to opioid users and their family/friends in an increasing number of countries (European Monitoring Centre for Drugs and Drug Addiction, 2015; World Health Organisation, 2014). In the United States alone, over 26,000 peer-administered naloxone reversals are estimated to have been achieved between 1996 and 2014 (Centers for Disease Control and Prevention, 2015). Although increasingly adopted internationally, the evidence base for THN’s effectiveness is still in its infancy; see for example (Walley et al., 2013) and (Coffin and Sullivan, 2013) on the likely effectiveness and cost-effectiveness of THN in reducing DRDs.
DRD rates in Scotland are higher than anywhere else in the UK and amongst the highest in Europe (English et al., 2012) averaging 500 annually, 400 of which are opioid-related (National Records of Scotland, 2014). In 2011, Scotland became the first country in the world to implement a National Naloxone Programme (McAuley et al., 2012; Bird et al., 2014,2015). Take-home naloxone is available to any individual at risk of opioid overdose and is supplied following successful completion of a brief 10–15 min training session incorporating basic life support and naloxone administration. Training and supply of naloxone to individuals in Scotland takes place in a range of community settings (including pharmacy) and across the entire prison estate. The latter group holds particular significance given the elevated risk of DRD in the weeks following liberation from prison (Merrall et al., 2010).
Key gaps exist in understanding how naloxone is experienced by service providers and service users, including how PWIDs engage with naloxone programmes over time. Such knowledge is vital to understanding the uptake of THN by recent injectors and hence its effectiveness at a national level in reaching those most at risk of opioid overdose, PWID in particular. For THN to be effective, it has to be available at the time of the overdose event, whether in a domestic or public setting. Thus, knowledge of naloxone ‘carriage’ provides important insight to how naloxone is managed by individuals day to day and potentially serves as an estimate of the likelihood of naloxone availability during an overdose emergency. Scotland’s National Naloxone Programme affords a unique opportunity to address these and other important questions related to the population level impact of this innovative public health policy.
Using data from approximately 5000 PWID who took part in nation-wide surveys in 2011–2012 and 2013–2014, we address three specific evidence gaps: the extent of Scotland’s naloxone supply to PWID; supply-source (community or prisons); and the carriage of naloxone.
2. Material and methods
2.1. Setting
Scotland has approximately 60,000 problem drug users (Information Services Division Scotland, 2014), at least 20,000 of whom are in receipt of opioid-substitution therapy (OST) (Scottish Prison Service, 2014). Hay et al. (2009) estimated there to be 20,000 PWID in Scotland, Overstall et al. (2014) reported a somewhat lower figure (15,000). Among those entering prison in Scotland, a third test positive for opiates at reception (Scottish Prison Service, 2014).
2.2. Data collection
The Needle Exchange Surveillance Initiative (NESI) is conducted biennially and aims to measure and monitor the prevalence of the Hepatitis C virus (HCV) and injecting risk behaviours among people who inject drugs (PWID) in Scotland (University of the West of Scotland et al., 2015). Within each survey, NESI recruits [on average] a demographically-representative sample of between 2000–3000 PWID from across Scotland, and over 90% report heroin as the drug injected most often within the past 6 months. Approximately half (51%) of potentially eligible clients that were approached agreed to participate, however a true refusal rate is difficult to calculate as individuals may not engage one day but participate the next.
Of those who did agree to participate in NESI, approximately 80% are ‘recent’ injectors (defined as having injected at least once in the previous 6-months) and 20% are ‘ever’ injectors (injected in the past but not in the previous 6-months). Trained interviewers recruit participants from selected agencies and pharmacies across Scotland that primarily provide injecting equipment but may also offer other harm reduction services, such as OST. Questions related to naloxone supply and carriage were first asked in the survey in 2011–2012 to complement the formal implementation of the Scottish National Naloxone Programme in January 2011. We use data from two NESI surveys; one undertaken between April, 2011 and January, 2012 and the other between February 2013 and February 2014. Participation in NESI is voluntary, consented and anonymous. Full details on methods used in NESI are available in detail elsewhere (University of the West of Scotland et al., 2015; Aspinall et al., 2012). Ethical approval for NESI was obtained from the West of Scotland Research Ethics Committee.
2.3. Analysis
Prior to analysis, within-survey duplicate respondents (i.e. individuals who participated more than once in a survey year) were identified and excluded. Although NESI is an anonymous survey, it does collect details on date of birth, gender, initials and locality where recruited, therefore duplicates can be identified for exclusion based on these data.
The outcomes – naloxone supply and carriage – were measured via self report answers to the following questions:
Have you been prescribed THN in the past year?
Where did you obtain your supply of naloxone (community or prison)?
Are you carrying any THN with you today?
Analysis was undertaken to determine changes in naloxone supply and carriage over time, both overall and by sub-group (i.e. gender, age-group, homelessness, injector status, and injecting frequency). Differences in responses between the two data surveys were measured using Chi-square tests together with 95% confidence intervals for rate-differences over time. All analyses were undertaken in IBM SPSS Statistics 21.0.
3. Results
Overall, the proportion of NESI participants who reported that they had been prescribed THN within the last year increased significantly from 8% (175/2146; 95% CI: 7% to 9%) in 2011–2012 to 32% (745/2331; 95% CI: 30% to 34%) in 2013–2014 (Table 1). Significant increases in naloxone supply were evident across all sub-groups analysed, that is: by gender, age-group, homelessness, and by injecting status and frequency. By 2013–2014, per subgroup, the higher proportions of naloxone supply in the past year were among: those aged under 35 years; those who had been recently homeless; and those who inject most frequently.
Table 1.
Take-home naloxone prescriptions and carriage by people who inject drugs (PWID) in Scotland; 2011–12 and 2013-14.
| Needle-Exchange Surveillance Initiative (NESI) | Have you been prescribed take-home naloxone in the past year? | Between eraa% difference, p-Value (95% CI) | Are you carrying any take-home naloxone with you today? | Between eraa% difference, p-Value (95% CI) | ||
|---|---|---|---|---|---|---|
| NESI surveillance era | 2011-12 | 2013-14 | 2011–12 | 2013–14 | ||
| Overall (%) | 175/2146 (8) | 745/2331 (32) | 24, <0.001 (22, 26) | 27/169 (16) | 39/741 (5) | −11, <0.001 (−17, −6) |
| Gender | ||||||
| Male (%) | 125/1554 (8) | 505/1613 (31) | 23, <0.001 (21, 26) | 18/122 (15) | 26/502 (5) | −10, <0.001 (−17, −4) |
| Female (%) | 50/589 (8) | 238/705 (34) | 26, <0.001 (21, 29) | 9/47 (19) | 13/237(5) | −14, <0.001 (−27, −4) |
| Age-group | ||||||
| ≤35 years (%) | 102/1065 (10) | 357/993 (36) | 26, <0.001 (23, 30) | 13/97 (13) | 16/355 (5) | −8, <0.001 (−17, −3) |
| >35 years (%) | 73/1078 (7) | 388/1337 (29) | 22, 0.001 (19, 25) | 14/72 (19) | 23/386 (6) | −13, <0.001 (−24, −6) |
| Homeless in the last 6 months | ||||||
| Yes (%) | 52/460 (11) | 241/580 (42) | 31, <0.001 (25, 35) | 5/49 (10) | 18/241 (7) | −3, <0.03 (−15, 4) |
| No (%) | 75/1003 (7) | 349/1132 (31) | 23, <0.001 (20, 26) | 11/74 (15) | 14/345 (1) | −14, <0.001 (−23, −7) |
| Injecting status | ||||||
| Recent (%) | 153/1797 (9) | 663/1930 (34) | 25, <0.001 (23, 28) | 22/147 (15) | 38/660 (6) | −9, <0.001 (−16, −4) |
| Ever (%) | 22/349 (6) | 82/401 (20) | 14, <0.001 (9, 19) | 5/22 (23) | 1/81 (1) | −21, <0.001 (−42, −8) |
| Frequency of injecting | ||||||
| Daily or more (%) | 84/885 (9) | 352/878 (40) | 31, <0.001 (27, 34) | 12/81 (15) | 25/350 (7) | −8, <0.001 (−17, −1) |
| Less than daily (%) | 91/1261 (7) | 391/1450 (27) | 20, <0.001 (17, 22) | 15/88 (17) | 14/389 (4) | −13, <0.001 (−23, −7) |
Chi-square test of association.
NB: not all sub-group totals add up to overall number due to missing data.
In contrast to supply, the proportion of NESI participants who were carrying naloxone with them on the day they were interviewed decreased significantly from 16% (27/169; 95% CI: 10% to 22%) in 2011–2012 to 5% (39/741; 95% CI: 4% to 7%) in 2013–2014. Significant decreases in naloxone carriage were evident across all sub-groups with the exception of those who had been recently homeless. Carriage was lowest among those who had not injected in the previous 6-months.
The proportion of participants reporting that their last naloxone supply was made via the prison service was stable across the two surveys: 16% (27/168) in 2011–2012 to 19% (138/732) in 2013–2014 (95% CI for difference in %: −4.1% to 8.4%). Additional analysis suggests that, when short prison sentences are taken into account, both community services and prisons were equally efficient at targeting their naloxone supplies to PWID (see supplementary analysis).1
4. Discussion
This study presents insight into the adoption and reach of a National Naloxone Programme among a key target group for the intervention. Results suggest that supply of naloxone to PWID has increased significantly since the introduction of a National Naloxone Programme in Scotland, but that naloxone carriage is low and has decreased from 2011/12 to 2013/14.
NESI samples have previously been shown to be demographically representative of Scotland’s PWID population (Aspinall et al., 2012). Comparability of results over time is strengthened by NESI’s use of similar sampling frameworks which recruit potential respondents from the same services across each survey with few exceptions. Potential weaknesses of this study are in its use of self-report data on supply and carriage which increases potential for socially desirable responses related to THN. However, given that data are collected by independent university researchers, with no relationship to participants or the services from which they recruit PWID, this risk is minimised. Also, previous research has suggested that self-reports from drug users are “sufficiently reliable and valid” to describe their behaviours in relation to drug use and related harms (Darke, 1998). However, the validity of naloxone carriage when attending for harm reduction services or OST as a reliable indicator of overall carriage is as yet untested and limits the applicability of these findings more widely.
The increased proportion of NESI participants who reported having been supplied with naloxone in the past year – from 8% in 2011–2012 to 32% in 2013–2014 – is consistent with national surveillance data in Scotland where the number of kits supplied increased from 3436 (2011/12) to 6465 (2013/14; Information Services Division Scotland, 2015). Assuming NESI is representative of the current Scottish PWID population, then extrapolation from the NESI study results suggests that around 4800 to 6400 of Scotland’s current injectors received naloxone in 2013–2014 if Scotland were to have in the region of 15,000 to 20,000 current injectors. As anticipated by Overstall et al. (2014), the upper estimate is too high because it accounts for almost all the naloxone kits issued in that year, whereas we assume kits will also have been prescribed for Scotland’s OST clients not all of whom will have injected in the past year. Hence, NESI’s respondents confirm that Overstall et al. (2014) would seem to be correct in their analysis that showed 20,000 injectors to be an over-estimate of Scotland’s injectors in 2006. Nonetheless, the vast majority of naloxone kits distributed across Scotland in the 2013–2014 period was issued to recent or ever injectors and the targeting of supply was indeed to highest risk groups as had been intended at the outset of the National Naloxone Programme. If we also consider that, by 2013–2014, the sub-groups reporting the highest prevalence of naloxone supply were those injecting most frequently (daily or more) (40%) and those reporting being recently homeless (42%), then the case that the National Naloxone Programme has successfully targeted the most at-risk and vulnerable individuals in the population becomes even more compelling.
Equally encouraging is our evidence that community services and prisons were equally efficient at targeting their naloxone supplies to PWID. It is important to recognise that beneficiaries of naloxone-on-release are not solely those recently-released from prison and that those recently-released benefit from community-issued naloxone-kits. Surveillance data from the National Naloxone Programme highlights a ratio of 2:1 against the person to whom naloxone-on-release was prescribed being its beneficiary and 6:1 against for those supplied in the community (Bird et al., 2015).
In contrast to the evidence that increasing numbers of PWID have been given naloxone over time, NESI data also suggest that naloxone carriage has declined since the National Naloxone Programme was implemented in 2011. The carriage rates from NESI (5–16%) are markedly lower than the carriage rates assumed by N-ALIVE team (75% naloxone-carriage in 1st 4-weeks but 50% in next 8 weeks) which also informed the 20% to 30% effectiveness targets adopted for the Scottish National Naloxone Programme during the design of its before and after evaluation (Bird et al., 2014). N-ALIVE was the first (and to date only) prison-based randomized controlled trial of naloxone-on-release (Strang et al., 2013). Had the carriage rates in the N-ALIVE Trial been as low as reported in this study then it is likely that the trial would have been stopped on grounds that so low a carriage rate made the main trial infeasible.
There are several potential reasons as to why carriage of naloxone may have decreased amongst NESI participants and for the difference between the NESI results, the N-ALIVE team’s assumptions, and Scotland’s before-after evaluation (Bird et al., 2015). Firstly, carriage was lowest among those who had not injected in the previous 6-months therefore it is possible that self-reported naloxone carriage is associated with current injecting behaviour and perceived risk of experiencing an overdose. Secondly, if there is a negative association between THN availability (observed increase) and naloxone carriage (observed decrease), as the NESI data suggests, it might also be possible that individual THN recipients feel that it is less crucial that they always have their kit on their person, as more kits are now in circulation and another THN recipient might be able to intervene if an overdose occurred and was witnessed (i.e., diffusion of responsibility).
Alternatively, Gaston et al. (2009) reported that those supplied with naloxone were reluctant to carry it on their person for fear of being identified as an injecting drug user. In addition, drug users have reported concerns that carriage of naloxone might expose them as a current injector to their families or to prison authorities (National Treatment Agency for Substance Misuse, 2011). PWIDs may also be reluctant to carry naloxone on their person because of fear of coming in to contact with the police. Despite research highlighting positive police attitudes toward naloxone (Ray et al., 2015), drug users across different countries have historically relayed unwillingness to call the emergency services in the event of overdose for fear of police attendance (Darke et al., 1996; Powis et al., 1999). This ‘guilt-by-association’ perception that opioid users reported prior to the availability of naloxone could also apply to naloxone carriage where PWID may assume that police will interpret a naloxone kit on their person as representing intention to use drugs and invite further investigation.
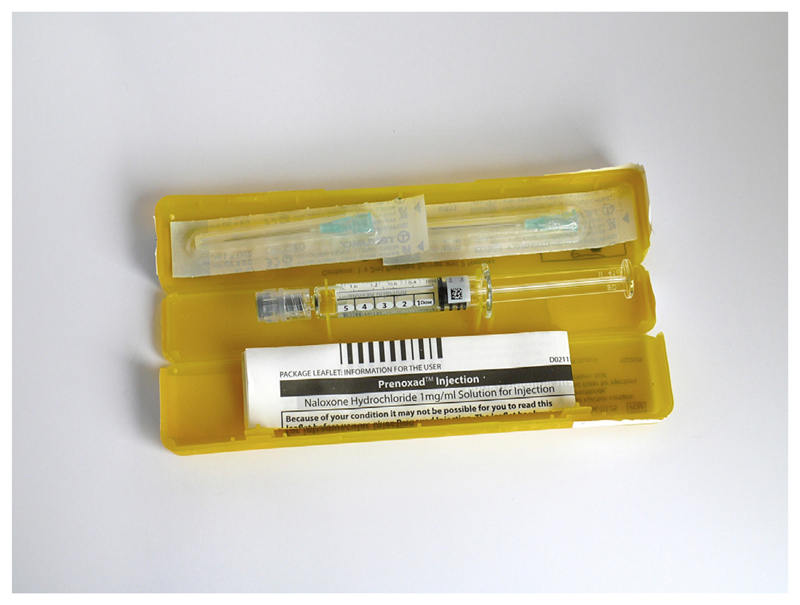
Finally, the naloxone kit supplied to participants in the N-ALIVE study was concealed in a wallet, designed to be discreet and portable. In contrast, the naloxone kit available via Scotland’s National Naloxone Programme is in a clinically labelled yellow box, and far bulkier (Length 160 mm, Depth 30 mm, Width 30 mm), making it less discreet and less portable (Fig. 1). It is plausible that the physical properties of naloxone kits may influence carriage rates among PWIDs. Carriage may also be less of an issue if most injecting [and overdose] takes place in a domestic setting, as is common (Strang et al., 1999).
Fig. 1.
Take-home naloxone kit supplied through the national programme in Scotland.
This study has several implications for future research, in particular a requirement for qualitative research to explore, in-depth, low naloxone carriage rates among PWID. Police attitudes toward naloxone in the UK, where it is not routinely carried by officers, also merit further exploration. In addition, future analysis of NESI data will yield insights into whether increasing levels of naloxone engagement and decreasing carriage rates are maintained over time. Lastly, investigation of carriage rates among PWID in different countries and settings are necessary to validate our initial findings.
The supply of naloxone to PWID has increased significantly since the introduction of a National Naloxone Programme in Scotland. NESI data suggests that the majority of supplies were issued to those at highest risk of opioid overdose as the national programme had intended, and prisons and community services were correspondingly efficient in terms of targeting this group. In contrast, naloxone carriage is low and decreased between the two NESI surveys; this area requires further investigation. Future analysis of NESI data will aim to explore these findings in more detail.
Supplementary Material
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.drugalcdep.2016.02.031.
Acknowledgements
The authors would like to acknowledge the contributions of the following individuals and organisations for their roles in the NESI study: Tony Knox, Elizabeth Allen, Cheryl Rees, Lauren Johnston, Julie Burza, Donald Falconer, Germana Vitrano and Alex Matheson (University of the West of Scotland); and Linda MacDonald and Tony Bimpson (West of Scotland Specialist Virology Centre). Finally, we would like to thank all the respondents and services that participated in the NESI study.
Role of funding source
This work was funded by the Scottish Government. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: 10.1016/j.drugalcdep.2016.02.031.
Conflict of interest
S.M.B. holds G.S.K. shares. S.M.B. is co-principal investigator for MRC-funded N-ALIVE pilot Trial.
A.Mc and S.M.B. serve on Scotland’s National Naloxone Advisory Group, but write in a personal capacity.
Contributors
A.T., S.J.H., D.J.G. and A.M. conceived and designed the survey. A.M. and A.T. implemented the survey. A.Mc. and S.M.B. conceived the statistical analysis. A.Mc and S.M.B. analyzed the data. A.Mc wrote first draft of the manuscript. A.Mc, A.M., S.M.B, S.J.H, D.J.G. and A.T. critically reviewed and approved the final manuscript.
References
- Aspinall E, Hutchinson SJ, Taylor A, Goldberg D. Uptake of paraphernalia from injecting equipment provision services and its association with sharing of paraphernalia among injecting drug users in Scotland. Drug Alcohol Depend. 2012;126:340–346. doi: 10.1016/j.drugalcdep.2012.05.041. [DOI] [PubMed] [Google Scholar]
- Bird S, McAuley A, Perry S, Hunter S. Effectiveness of Scotland’s National Naloxone Programme for reducing opioid-related deaths: a before (2006–10) versus after (2011–13) comparison. Addiction. 2015 doi: 10.1111/add.13265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SM, Parmar MKB, Strang J. Take-home naloxone to prevent fatalities from opiate-overdose: protocol for Scotland’s public health policy evaluation, and a new measure to assess impact. Drugs Educ Prev Policy. 2014;22:66–76. doi: 10.3109/09687637.2014.981509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Opioid Overdose Prevention Programs Providing Naloxone to Laypersons—United States, 2014. [accessed 17.08.15];2015 http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6423a2.htm?s_cid=mm6423a2_w. [PMC free article] [PubMed]
- Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal. Ann Int Med. 2013;158:1–9. doi: 10.7326/0003-4819-158-1-201301010-00003. [DOI] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Darke S, Degenhardt L, Mattick R. Mortality Amongst Illicit Drug Users: Epidemiology Causes And Intervention. University Press; Cambridge: 2006. [Google Scholar]
- Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia II. Responses to overdose. Addiction. 1996;91:413–417. doi: 10.1046/j.1360-0443.1996.91341310.x. [DOI] [PubMed] [Google Scholar]
- English L, Corkery J, Hope V. In: United Kingdom Drug Situation: Annual Report on the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) Stewart C, Edginton M, McVeigh J, Bellis MA, editors. UK Focal Point; 2012. [accessed 4.07.15]. http://www.nta.nhs.uk/uploads/2012.pdf. [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction. Preventing Fatal Overdoses: A Systematic Review of the Effectiveness of Take-Home Naloxone. EMCDDA Papers. Publications Office of the European Union; Luxembourg: 2015. [Google Scholar]
- Gaston RL, Best D, Manning V, Day E. Can we prevent drug related deaths by training opioid users to recognize and manage overdose? Harm Reduct J. 2009;6:1–8. doi: 10.1186/1477-7517-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay G, Gannon M, Casey J, McKeganey N. Estimating the National and Local Prevalence of Problem Drug Misuse in Scotland. University of Glasgow; 2009. [accessed 17th August 2015]. http://www.scotpho.org.uk/downloads/drugs/Prevalence_Report_%202006.pdf. [Google Scholar]
- Information Services Division Scotland. Estimating the National and Local Prevalence of Problem Drug Use in Scotland 2012/13. [accessed 17.08.15];2014 https://isdscotland.scot.nhs.uk/Health-Topics/Drugs-and-Alcohol-Misuse/Publications/2014-10-28/2014-10-28-Drug-Prevalence-Report.pdf?33819216490.
- Information Services Division Scotland. National Naloxone Programme Scotland—Monitoring Report 2014/15. [accessed 27.10.15];2015 http://www.isdscotland.org/Health-Topics/Drugs-and-Alcohol-Misuse/Publications/2015-10-27/2015-10-27-Naloxone-Report.pdf.
- Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull WHO. 2013;91:102–123. doi: 10.2471/BLT.12.108282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley A, Best D, Taylor A, Hunter C, Robertson R. From evidence to policy: the Scottish national naloxone programme. Drugs Educ Prev Policy. 2012;19:309–319. [Google Scholar]
- Merrall ELC, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, et al. Meta analysis of drug-related deaths soon after release from prison. Addiction. 2010;105:1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Records of Scotland. Drug-Related Deaths in Scotland in 2014. [accessed 29.01.16];2014 http://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/deaths/drug-related-deaths-in-scotland/2014.
- National Treatment Agency for Substance Misuse. The NTA Overdose and Naloxone Training Programme for Families and Carers. [accessed 27.10.15];2011 http://www.nta.nhs.uk/uploads/naloxonereport2011.pdf.
- Overstall A, King R, Bird SM, Hay G, Hutchinson SJ. Incomplete contingency tables with censored cells with application to estimating the number of people who inject drugs in Scotland. Stat Med. 2014;33:1564–1579. doi: 10.1002/sim.6047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powis B, Strang J, Griffiths P, Taylor C, Williamson S, Fountain J, et al. Self-reported overdose among injecting drug users in London: extent and nature of the problem. Addiction. 1999;94:471–478. doi: 10.1046/j.1360-0443.1999.9444712.x. [DOI] [PubMed] [Google Scholar]
- Ray B, O’Donnell D, Kahre K. Police officer attitudes towards intranasal naloxone training. Drug Alcohol Depend. 2015;146:107–110. doi: 10.1016/j.drugalcdep.2014.10.026. [DOI] [PubMed] [Google Scholar]
- Scottish Prison Service. Addiction Prevalence Testing for Performance Measurement Purposes 2014–15. [accessed 17.8.15];2014 http://www.scotpho.org.uk/downloads/drugs/SPS-Addiction-Prevalence-Testing-Stats-Final-2014-15.pdf.
- Strang J, Bird SM, Parmar MKB. Take-home emergency naloxone to prevent heroin overdose deaths after prison release: rationale and practicalities for the N-ALIVE randomised trial. J Urban Health. 2013;90:983–996. doi: 10.1007/s11524-013-9803-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, Darke S, Hall W, Farrell M, Ali R. Heroin overdose: the case for take-home naloxone. BMJ. 1996;312:1435–1436. doi: 10.1136/bmj.312.7044.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, Powis B, Best D, Vingoe L, Griffiths P, Taylor C, Welch S, Gossop M. Preventing opiate overdose fatalities with take-home naloxone: pre-launch study of possible impact and acceptability. Addiction. 1999;94:199–204. doi: 10.1046/j.1360-0443.1999.9421993.x. [DOI] [PubMed] [Google Scholar]
- University of the West of Scotland, Health Protection Scotland, Glasgow Caledonian University, the West of Scotland Specialist Virology Centre. The Needle Exchange Surveillance Initiative (NESI): Prevalence Of HCV and Injecting Risk Behaviours Among People Who Inject Drugs (PWID) Attending Injecting Equipment Provision Services (Ieps) in Scotland, 2008/2009–2013/2014. [accessed 11.07.15];2015 http://www.uws.ac.uk/workarea/downloadasset.aspx?id=19327355743.
- Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, Ruiz S, Ozonoff A. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation (WHO) Community Management Of Opioid Overdose. [accessed 4.08.15];2014 http://apps.who.int/iris/bitstream/10665/137462/1/9789241548816_eng.pdf?ua=1&ua=1. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.