Abstract
Objective
The duration of untreated psychosis is associated with poor outcomes in multiple domains in the early course of nonaffective psychotic disorders, although relatively little is known about determinants of this critical period, particularly health services–level determinants. This study examined three hypothesized predictors of duration of untreated psychosis (lack of insurance, financial problems, and broader barriers) among urban, socioeconomically disadvantaged African Americans, while controlling for the effects of three patient-level predictors (mode of onset of psychosis, living with family versus alone or with others before hospitalization, and living above versus below the federally defined poverty level).
Methods
Analyses included data from 42 patient–family member dyads from a larger sample of 109 patients with a first episode of nonaffective psychosis. The duration of untreated psychosis and all other variables were measured in a rigorous, standardized fashion in a study designed specifically to examine determinants of treatment delay. Survival analyses and Cox regression assessed the effects of the independent predictors on time from onset of psychosis to hospital admission for initial evaluation and treatment.
Results
The median duration of untreated psychosis was 24.5 weeks. When the analyses controlled for the three patient-level covariates, patients without health insurance, with financial problems, or with barriers to seeking help had a significantly longer duration of untreated psychosis.
Conclusions
Health services–related factors, such as lack of insurance, are predictive of longer treatment delay. Efforts to eliminate uninsurance and underinsurance, as well as minimize barriers to treatment, would be beneficial for improving the prognosis of young patients with emerging nonaffective psychotic disorders. (Psychiatric Services 60:1489–1494, 2009)
Failure to make prompt initial treatment contact has been noted as a pervasive aspect of unmet need for mental health care in the United States (1). Regarding psychotic disorders, the duration of untreated psychosis represents the interval of time from the onset of positive psychotic symptoms to the initiation of adequate treatment (2–4). This treatment delay has been shown, through numerous studies summarized in two independent meta-analyses (5,6), to be associated with poorer outcomes in the early course of psychosis. Although the adverse correlates of duration of untreated psychosis are relatively clearly established and some evidence indicates that this treatment delay is modifiable through broad community-level informational campaigns and dedicated early-detection teams (7,8), less is known about the causes or determinants of treatment delay, particularly in especially vulnerable populations.
Few health services–related predictors of the delay in treatment for psychosis have been substantiated in the literature, although some factors pertaining to access to care have been explored. A review of studies from multiple countries found that duration of untreated psychosis is inversely correlated with the gross domestic product, presumably because of differences in access to adequate health care (9). In that study a strong relationship was observed between duration of untreated psychosis and purchasing power parity in lower- and middle-income countries, which suggests that the cost of care is a major determining factor. In a sample of 525 patients with affective and nonaffective psychoses hospitalized in psychiatric facilities in Suffolk County, New York, between September 1989 and December 1995, having private insurance was associated with a greater likelihood of being admitted to a hospital for psychosis within three months of onset (10). In that study, having private insurance and, to a lesser extent, having public health insurance increased the likelihood that a patient had received outpatient care before the first hospitalization. Although some patient- and family-level predictors of treatment delay have been studied, little research has identified these or other health services–level determinants, despite the fact that they clearly play a role in expediting or delaying care seeking. Regarding established patient- and illness-level predictors of duration of untreated psychosis, previous research suggests that the mode of onset of psychosis, which indicates how quickly psychotic symptoms develop, is a replicated determinant of this critical variable (11–14).
This report presents data on the effects of three health services–level variables: whether or not a patient with a first episode of nonaffective psychosis had insurance, the presence of financial problems as reported by the patient’s family member, and the family member’s endorsement of several barriers to seeking help beyond financial problems. This analysis focuses on health services–level predictors among urban, socioeconomically disadvantaged African Americans. Work in this area is crucial because of the widely recognized persistence of race-based disparities in mental health domains that adversely affect African Americans (15,16).
Methods
Setting and sample
Hospitalized patients with first-episode nonaffective psychosis were recruited from three inpatient psychiatric units providing services for patients with no insurance or with only public-sector insurance (for example, Medicaid). The population served by these units is predominantly African American, low-income, and socially disadvantaged. Between July 2004 and June 2008, a total of 281 patients were screened for study participation, and 192 were found to be eligible on the basis of the following inclusion criteria: aged 18–40 years, able to speak and read English, absence of known mental retardation, a Mini-Mental State Examination (17,18) score ≥23 (indicating generally intact orientation and basic cognitive functioning), absence of medical conditions that could compromise ability to participate, no prior antipsychotic treatment lasting for more than three months, no previous hospitalization for psychosis more than three months before the index hospitalization, and able to provide written informed consent. Eighty-three patients did not participate because of refusal (N=52, 63%) or discharge from the hospital before an assessment could be conducted (N=31, 37%). Those who did not participate did not differ from the 109 participants with regard to age, gender, or race or ethnicity.
Of the 109 participants in the overarching study, 44 (40%) referred to the study a family member who had been actively involved in initiating care. These family members provided detailed data on a number of family-and health services–related variables. Two Caucasian informants were excluded to enhance homogeneity of the sample, so the analyses presented here included data from 42 African-American patient–family member dyads. When compared on 26 sociodemographic and clinical variables, patients with a participating family member were significantly different from those without a participating family member only in terms of having a longer length of hospital stay and an earlier age at onset of psychosis.
Procedures and materials
Clinical research assessments with patients typically lasted about four hours and were conducted once patients were adequately stabilized to allow for informed consent and evaluation (for example, in the overarching study, 87 of the 109 patients (80%) were assessed between the third and the tenth hospital day). The research assessment with family members lasted approximately two hours and was conducted during the patient’s hospitalization or, rarely, within several days of discharge. The study was approved by all relevant institutional review boards and research oversight committees. All patients and family members gave written informed consent before their participation.
As reported previously (14,19) duration of untreated psychosis was defined as the number of weeks from the onset of positive psychotic symptoms until first hospital admission and was measured in a systematic way by using selected items from the semistructured Course of Onset and Relapse Schedule/Topography of Psychotic Episode (CORS/TOPE) interview (20), as well as the Symptom Onset in Schizophrenia (SOS) inventory (21). Onset of positive symptoms was operationalized as the date on which hallucinations or delusions met the threshold for a Positive and Negative Syndrome Scale (22) score of ≥3, and systematic methods were used to resolve difficulties in obtaining exact dates for the onset of psychotic symptoms. Cross-referencing with milestones and memorable events was used to enhance the accuracy of dating. Consensus-based best estimates of duration of untreated psychosis were derived using all available information, including a thorough chart review, discussions with treating clinicians, an in-depth patient interview, and a detailed interview with family members (also based on selected CORS/TOPE items and the SOS inventory).
Mode of onset of psychosis was categorized, again based on all available information, using five subtypes put forth by the World Health Organization’s International Pilot Study of Schizophrenia (23): sudden, precipitous, subacute, gradual, and insidious. For the analysis presented here, mode of onset of psychosis was trichotomized as acute, subacute, or chronic. Along with mode of onset, we also included data on two other patient-level covariates—who the patient lived with before hospitalization and living above or below the federal poverty level. The latter was determined on the basis of the patient’s report of annual household income and the number of people living in the household, using published federal guidelines for the year in which the patient was assessed. These three variables were used as covariates because they are patient-level variables discovered to be significant predictors of duration of untreated psychosis in the larger study (Compton MT, Gordon TL, Goulding SM, et al., unpublished manuscript, 2009).
Data on the three hypothesized health services–level predictors were collected as part of a detailed structured interview with the family members. The first variable of interest, whether or not the patient had insurance or Medicaid, was queried directly using closed-ended items. The second variable, the presence of financial problems, was assessed by asking, “In your opinion, was seeking help for your family member difficult to do because of financial problems?” Regarding the third hypothesized predictor, more general barriers to accessing health care, the family member’s report of several barriers to seeking help in addition to financial problems was assessed by the aforementioned question and five others that asked about transportation problems, not knowing where to go, having difficulty getting time off work, resistance from the patient, and insurance problems. Responses of the family members were trichotomized on the basis of the endorsement of zero or one, two or three, or four to six barriers.
Data analyses
Survival analyses were employed to examine the hypothesized health services–level predictors of duration of untreated psychosis. All analyses controlled for the effects of the one relatively well-established patient-level predictor of this variable, mode of onset of psychosis (13,14), as well as the two other patient-level factors (Compton MT, Gordon TL, Goulding SM, et al., unpublished manuscript, 2009). For survival analyses, onset of psychosis was the entry point and hospital admission was the end point. Survivor functions representing survival rate as a function of time (Kaplan-Meier survival curves) were constructed to represent the cumulative probability of hospitalization over time in different groups. Log-rank tests assessed whether the probability of first hospitalization over time differed between defined groups, and Cox regression (which predicts survival time from covariates) quantified associations in terms of hazard ratios. As such, hazard ratios of <1 indicated a longer duration of untreated psychosis on average, and hazard ratios of >1 indicated a shorter duration of untreated psychosis (a hazard ratio of 1 would indicate no difference in survival time between groups). Following the convention of most researchers, the median (in addition to mean) duration of untreated psychosis was reported in this study, because of the highly positively skewed distribution of this duration measure. A recent systematic review and meta-analysis concluded that the mean duration of untreated psychosis is unsuitable for benchmarking services, as it is too heavily influenced by a small proportion of patients with remarkably long treatment delays (24).
Results
The mean±SD age of the 42 patients in the subsample was 22.1±4.1 years, and the mean educational attainment was 11.0±2.1 years. Most (N=31, 74%) were men, nearly all (N=40, 95%) were single or never married, and most lived with family members (N=33, 79%) and were unemployed (N=26, 62%) during the month before hospitalization. Structured Clinical Interview for DSM-IV Axis I Disorders (25) diagnoses were as follows: schizophreniform disorder (N=9, 21%), schizophrenia (N=27, 64%), schizoaffective disorder (N=3, 7%), brief psychotic disorder (N=1, 2%), and psychotic disorder not otherwise specified (N=2, 5%).
Regarding family members, the mean age was 46.3±10.1 years, and the mean educational attainment was 12.8±2.5 years. Most (N=31, 74%) were mothers, with the remainder being fathers (N=3, 7%), sisters (N= 3, 7%), or close second-degree relatives (N=5, 12%) who were actively involved in initiating care for patients. The majority of informants (N=31, 74%) were currently or previously married, and just over half (N=25, 60%) were unemployed during the month before the patient’s hospitalization.
In the subsample of 42 patients, the median duration of untreated psychosis was 24.5 weeks (mean=87.1±150.3 weeks, range=0–839.0 weeks). For the overall sample of 109 patients, the median duration of untreated psychosis was 22.3 weeks (mean=67.5±126.1 weeks, range=0–839.3 weeks). The duration of untreated psychosis did not differ between the subsample and the overall, larger sample. For the three hypothesized health services–level predictors, 33 family members (79%) reported that the patient did not have health insurance; 24 family members (57%) endorsed financial problems as a barrier to seeking help for the patient; and 13 family members (31%) endorsed zero or one barrier to seeking help, 14 family members (33%) endorsed two or three barriers, and 15 family members (36%) endorsed four to six barriers. Of note, although not having health insurance was significantly related to financial problems endorsed as a barrier to seeking help (χ2=4.32, df=1, Fisher’s exact p=.05), this relationship was not absolute. For example, 11 patients (26%) did not have health insurance but did not endorse financial problems as a barrier. On the other hand, not having health insurance was not significantly related to the number of endorsed barriers to seeking help, indicating that these two variables are in fact independent.
The median duration of untreated psychosis for participants without insurance was 42.5 weeks (mean= 107.1±167.5), compared with 22.5 weeks (mean=27.3±14.8) for those with insurance. Patients without health insurance had a significantly longer duration of untreated psychosis (χ2=3.92, df=1, p=.05, hazard ratio=.34) when the analysis controlled for the three covariates. This indicates that at any given point in time, patients with insurance were, on average, about three times as likely (1/.34=2.94) to be hospitalized as those without insurance. The duration of untreated psychosis survival distribution function pertaining to patients who did not have insurance versus those who had public insurance is shown in Figure 1.
Figure 1.
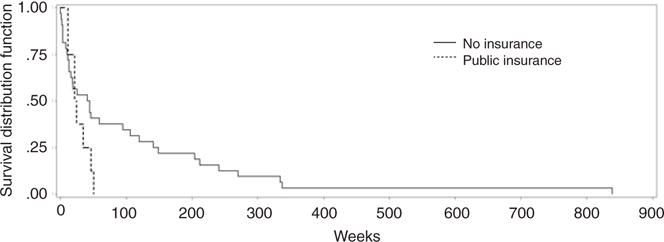
Survival curves for duration of untreated psychosis, stratified by insurance status
The median duration of untreated psychosis for participants whose family members endorsed financial problems was 59.0 weeks (mean=139.9±186.3), compared with 18.0 weeks (mean=25.1±34.9) for those without financial problems. The presence of financial problems as reported by family members was predictive of the duration of untreated psychosis (χ2=10.17, df=1, p=.001, hazard ratio=.24) when the analysis controlled for the three covariates. Thus, on average, patients without financial problems were about four times as likely as those with financial problems to be hospitalized at any given point in time. The survival distribution function is shown in Figure 2.
Figure 2.
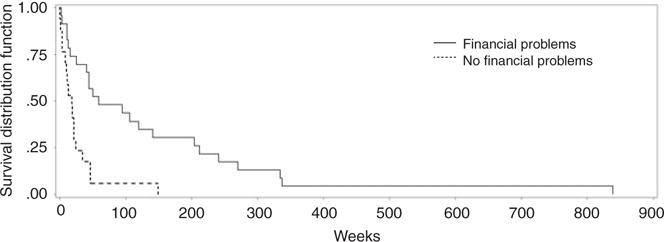
Survival curves for duration of untreated psychosis, stratified by financial problems
The presence of four to six barriers (χ2=9.40, df=1, p=.002, hazard ratio=.18) was predictive of treatment delay (compared with endorsing none or only one barrier) when the analysis controlled for the three covariates, meaning that, on average, patients with none or only one barrier were about 5.5 times as likely as those with four to six barriers to be hospitalized at any given point in time. The survival distribution function for duration of untreated psychosis pertaining to patients with four to six barriers versus two or three barriers versus zero or one barrier is shown in Figure 3.
Figure 3.
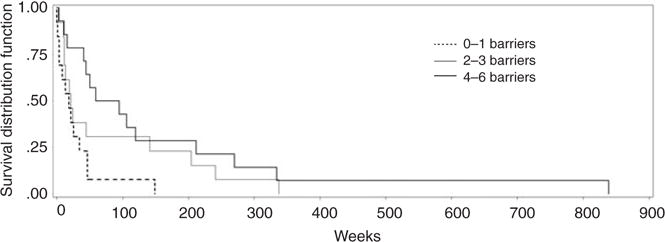
Survival curves for duration of untreated psychosis, stratified by barriers to seeking help beyond financial problems
Discussion
The findings presented here suggest that an accumulation of barriers (patient’s lack of insurance, the presence of financial problems, and a higher number of endorsed barriers to seeking help, all based on the family member’s report) impedes patients and their families from seeking treatment for emerging nonaffective psychotic disorders. These variables are predictive of a longer treatment delay, which in turn may contribute to poorer clinical outcomes and greater family burden. These results support a previous report that lack of insurance predicts a longer duration of untreated psychosis (10), and they are consistent with literature showing that uninsured adults are less likely than those with insurance to obtain care for substance abuse and mental illnesses (26).
Some U.S. studies of the duration of untreated psychosis report a longer period of treatment delay than estimates from European studies. One possible explanation is that prolonged delay may be due to differences in health services delivery across countries. The number of adults who do not have health insurance in the United States increased by six million from 2000 to 2004, and young adults (19–34 years of age) accounted for half of this increase (27). Poverty is another key consideration—two-thirds of the growth in the uninsured was among Americans whose income is 200% below the federal poverty level (27). The association that we found between lack of insurance and a longer duration of untreated psychosis is consistent with data indicating that when analyses controlled for socioeconomic factors, patients who had lost their insurance were more likely to delay seeking care within the four months after visiting an emergency department than people whose health insurance status did not change (28), as well as with data showing that compared with persons with insurance the uninsured were less likely to receive medical care and more likely to report not receiving care even when they thought it was needed (29). Psychotic disorders typically emerge during late adolescence and early adulthood, when individuals are particularly vulnerable to not having insurance, because they are often no longer eligible through their parents’ insurance or publicly funded children’s insurance. Furthermore, psychotic disorders usually become manifest before those affected have been able to obtain stable, full-time employment with health benefits or a sufficient income to purchase health insurance.
Another major, potentially modifiable barrier for family members who are responsible for initiating care is not knowing where to go for help. One research group has demonstrated that the median community-level duration of untreated psychosis can be reduced through an early-detection program that includes educational campaigns for the general population; targeted information campaigns directed at general practitioners, social workers, and high school health care personnel; and a telephone hotline that links potential patients to a specialized early-detection team (7,8). This intervention reduced treatment delay, presumably by removing barriers to treatment and lowering the threshold for initiating treatment.
Research on predictors of treatment delay is of critical importance to secondary prevention efforts for schizophrenia or efforts to reduce the negative long-term consequences of an emerging illness. Meta-analyses have found that a longer duration of untreated psychosis predicts poorer response to treatment when it is initiated (6), as well as poorer outcomes evidenced by greater symptom severity and poorer overall and social functioning at six and 12 months (5). Health services–level determinants of treatment delay are of particular policy interest because these may be more easily addressed than illness-related determinants, some of which are not modifiable (for example, mode of onset of psychosis). The findings presented here suggest that urban, socioeconomically disadvantaged African Americans could benefit from health services–level interventions to reduce barriers to treatment seeking, such as not knowing where to go for help and not being able to pay for medical care. Increased knowledge of predictors within specific communities could lead to targeted community educational and outreach efforts, as well as public policies, tailored to directly address the specific barriers to mental health care access.
Several methodological limitations must be acknowledged when interpreting the findings presented here. For example, because of the unique sociodemographic characteristics of the sample, caution is warranted in generalizing these findings to dissimilar populations. However, these results are particularly relevant in terms of mental health treatment seeking in African-American families with an adolescent or young adult with an emerging psychotic disorder. As highlighted in Mental Health: Culture, Race, and Ethnicity, racial and ethnic minority groups have less access to health care than do non-Hispanic whites (30). Also, when minority populations do receive treatment, the care is more likely to be poor in quality. Lack of appropriate insurance coverage (31), fragmented care (32), and issues pertaining to cultural differences (33) all contribute to the mental health disparities between African Americans and non-Hispanic whites.
Another limitation is that a selected group of only three key variables were examined in an effort to limit the number of hypothesis tests performed. Future studies should address how other health services–level variables affect treatment delay. Despite these limitations, to the authors’ knowledge, this is the only study that quantitatively addresses health services–level predictors of the duration of untreated psychosis by using direct measurements obtained from family members actively involved in initiating care and the only study to do so in an African-American sample.
Conclusions
This study gives evidence of health services–level factors as determinants of treatment delay among urban, socioeconomically disadvantaged African-American patients with a first episode of nonaffective psychosis. Specifically, family member’s endorsement of the patient’s lack of insurance, the presence of financial problems, and a higher number of endorsed barriers to seeking help (for example, transportation problems, not knowing where to go for help, and having difficulty getting time off from work) were associated with a longer duration of untreated psychosis when analyses adjusted for the effects of the three patient-level covariates. Efforts to eliminate uninsurance and underinsurance, educate the public about treatment options, and minimize barriers to prompt access to health care would be beneficial in multiple domains and are of utmost importance as health care professionals seek to improve quality of care and long-term outcomes for this vulnerable population.
Acknowledgments
This work was supported by grant K23 MH067589 from the National Institute of Mental Health.
Footnotes
Disclosures: The authors report no competing interests.
Contributor Information
Michael T. Compton, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Grady Memorial Hospital, Box 26238, 80 Jesse Hill Jr. Dr., Atlanta, GA 30303
Claire E. Ramsay, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Grady Memorial Hospital, Box 26238, 80 Jesse Hill Jr. Dr., Atlanta, GA 30303
Ruth S. Shim, Department of Psychiatry and Behavioral Sciences, Morehouse School of Medicine, Atlanta
Sandra M. Goulding, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Grady Memorial Hospital, Box 26238, 80 Jesse Hill Jr. Dr., Atlanta, GA 30303
Tynessa L. Gordon, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Grady Memorial Hospital, Box 26238, 80 Jesse Hill Jr. Dr., Atlanta, GA 30303
Paul S. Weiss, Department of Biostatistics, Rollins School of Public Health, Emory University, Atlanta
Benjamin G. Druss, Department of Health Policy and Management, Rollins School of Public Health, Emory University, Atlanta
References
- 1.Wang PS, Berglund P, Olfson M, et al. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- 2.Norman RMG, Malla AK. Duration of untreated psychosis: a critical examination of the concept and its importance. Psychological Medicine. 2001;31:381–400. doi: 10.1017/s0033291701003488. [DOI] [PubMed] [Google Scholar]
- 3.Compton MT, Carter T, Bergner E, et al. Defining, operationalizing, and measuring the duration of untreated psychosis: advances, limitations, and future directions. Early Intervention in Psychiatry. 2007;1:236–250. [Google Scholar]
- 4.Compton MT, Goulding SM, Broussard B, et al. Treatment delay in the early course of schizophrenia and the duration of untreated psychosis. Psychiatric Annals. 2008;38:504–511. [Google Scholar]
- 5.Marshal M, Lewis S, Lockwood A, et al. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Archives of General Psychiatry. 2005;62:975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 6.Perkins DO, Gu H, Boteva K, et al. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. American Journal of Psychiatry. 2005;162:1785–1804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- 7.Melle I, Haahr U, Friis S, et al. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Archives of General Psychiatry. 2004;61:143–150. doi: 10.1001/archpsyc.61.2.143. [DOI] [PubMed] [Google Scholar]
- 8.Joa I, Johannessen JO, Auestad B, et al. The key to reducing duration of untreated first psychosis: information campaigns. Schizophrenia Bulletin. 2008;34:466–472. doi: 10.1093/schbul/sbm095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Large M, Farooq S, Nielssen O, et al. Relationship between gross domestic product and duration of untreated psychosis in low- and middle-income countries. British Journal of Psychiatry. 2008;193:272–278. doi: 10.1192/bjp.bp.107.041863. [DOI] [PubMed] [Google Scholar]
- 10.Rabinowitz J, Bromet EJ, Lavelle J, et al. Relationship between type of insurance and care during the early course of psychosis. American Journal of Psychiatry. 1998;155:1392–1397. doi: 10.1176/ajp.155.10.1392. [DOI] [PubMed] [Google Scholar]
- 11.Kalla O, Aaltonen J, Wahlstrom J, et al. Duration of untreated psychosis and its correlates in first-episode psychosis in Finland and Spain. Acta Psychiatrica Scandinavica. 2002;106:262–275. doi: 10.1034/j.1600-0447.2002.02302.x. [DOI] [PubMed] [Google Scholar]
- 12.Chen EYH, Dunn ELW, Miao MYK, et al. The impact of family experience on the duration of untreated psychosis (DUP) in Hong Kong. Social Psychiatry and Psychiatric Epidemiology. 2005;40:350–356. doi: 10.1007/s00127-005-0908-z. [DOI] [PubMed] [Google Scholar]
- 13.Morgan C, Abdul-Al R, Lappin JM, et al. Clinical and social determinants of duration of untreated psychosis in the ÆSOP first-episode psychosis study. British Journal of Psychiatry. 2006;189:446–452. doi: 10.1192/bjp.bp.106.021303. [DOI] [PubMed] [Google Scholar]
- 14.Compton MT, Chien VH, Leiner AS, et al. Mode of onset of psychosis and family involvement in help-seeking as determinants of duration of untreated psychosis. Social Psychiatry and Psychiatric Epidemiology. 2008;43:975–982. doi: 10.1007/s00127-008-0397-y. [DOI] [PubMed] [Google Scholar]
- 15.Hines-Martin V, Malone M, Kim S, et al. Barriers to mental health care access in an African American population. Issues in Mental Health Nursing. 2003;24:237–256. doi: 10.1080/01612840305281. [DOI] [PubMed] [Google Scholar]
- 16.Das AK, Olfson M, McCurtis HL. Depression in African Americans: breaking barriers to detection and treatment. Journal of Family Practice. 2006;55:30–39. [PubMed] [Google Scholar]
- 17.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 18.Cockrell JR, Folstein MF. Mini-Mental State Examination (MMSE) Psychopharmacology Bulletin. 1988;24:689–692. [PubMed] [Google Scholar]
- 19.Compton MT, Esterberg ML, Druss BG, et al. A descriptive study of pathways to care among hospitalized urban African American first-episode schizophrenia-spectrum patients. Social Psychiatry and Psychiatric Epidemiology. 2006;41:566–573. doi: 10.1007/s00127-006-0065-z. [DOI] [PubMed] [Google Scholar]
- 20.Norman RMG, Malla AK. Course of Onset and Relapse Schedule: Interview and Coding Instruction Guide. London, Ontario, Canada: Prevention and Early Intervention for Psychosis Program; 2002. [Google Scholar]
- 21.Perkins DO, Leserman J, Jarskog LF, et al. Characterizing and dating the onset of symptoms in psychotic illness: the Symptom Onset in Schizophrenia (SOS) inventory. Schizophrenia Research. 2000;44:1–10. doi: 10.1016/s0920-9964(99)00161-9. [DOI] [PubMed] [Google Scholar]
- 22.Kay SR, Fizbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 23.Jablensky A, Sartorius N, Ernberg G, et al. Chapter 2: Sociodemographic, clinical and diagnostic description of the study population. Psychological Medicine. 1992;20:18–42. [Google Scholar]
- 24.Large M, Nielssen O, Slade T, et al. Measurement and reporting of the duration of untreated psychosis. Early Intervention in Psychiatry. 2008;2:201–211. doi: 10.1111/j.1751-7893.2008.00080.x. [DOI] [PubMed] [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders. New York: New York State Psychiatric Institute, Biometrics Research Department; 1998. [Google Scholar]
- 26.Wells KB, Sherbourne CD, Sturm R, et al. Alcohol, drug abuse, and mental health care for uninsured and insured adults. Health Services Research. 2002;37:1055–1066. doi: 10.1034/j.1600-0560.2002.65.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holohan J, Cook A. Changes in economic conditions and health insurance coverage, 2000–2004 Health Affairs. Suppl Web Exclusives. 2005:w498–w508. doi: 10.1377/hlthaff.w5.498. [DOI] [PubMed] [Google Scholar]
- 28.Burstin HR, Swartz K, O’Neil AC, et al. The effect of change of health insurance on access to care. Inquiry. 1998–1999;35:389–397. [PubMed] [Google Scholar]
- 29.Baker DW, Shapiro MF, Schur CL. Health insurance and access to care for symptomatic conditions. Archives of Internal Medicine. 2000;160:1269–1274. doi: 10.1001/archinte.160.9.1269. [DOI] [PubMed] [Google Scholar]
- 30.Mental Health. Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Washington, DC: Department of Health and Human Services, US Public Health Service; 2001. [PubMed] [Google Scholar]
- 31.Snowden LR, Thomas K. Medicaid and African American outpatient mental health treatment. Mental Health Services Research. 2000;2:115–120. doi: 10.1023/a:1010161222515. [DOI] [PubMed] [Google Scholar]
- 32.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 33.Swartz MS, Wagner HR, Swanson JW, et al. Administrative update: utilization of services. Community Mental Health Journal. 1998;34:133–144. doi: 10.1023/a:1018736917761. [DOI] [PubMed] [Google Scholar]


