Abstract
Purpose
The purpose of the study was to qualitatively and quantitatively assess bone regeneration potential of tentpole technique using beta tricalcium phosphate bone graft in vertically deficient alveolar ridges.
Materials and Method
This prospective study comprised of 20 patients with vertically deficient alveolar ridges, wherein thirty one implants were placed. Tenting of the soft tissue matrix was done using titanium screws and beta tricalcium phosphate synthetic bone graft was filled in the vertical defect. Clinical and radiographic assessment was done at 1, 3 and 6 months. Preoperative biochemical analysis of Osteopontin and RANKL was done and then reassesed at 3 months postoperative. Bone core collected at 6 postoperative months, while removal of screw, was analysed histologically.
Results
A significant gain in bone height of 2.87 ± 0.79 mm was seen at 6 months postoperative. All implants osseointegrated. Loosening of screw was seen in two patients.There was no postoperative wound dehiscence. Histologic analysis revealed new bone formation .There was no significant change in the levels of RANKL and Osteopontin at 3 months postoperative.
Conclusion
This is a safe and effective technique for bone regeneration in vertically deficient alveolar ridges and has minimal complications. The regenerated bone has new and viable bone content and supports implant material. More studies with long term follow up are needed to assess the stability of bone after long term loading.
Keywords: Tent pole, Dental implants, Alveolar bone height
1. Introduction
The alveolar bone is maintained by the presence of teeth that it retains. Loss of teeth results in alteration in alveolar bone both in buccolingual and apicocoronal dimensions.
Ridge augmentation is required for successful retention of prosthesis. Techniques like distraction osteogenesis,1 autogenous onlay block or particulate grafts,2, 3 titanium mesh or combination4 have been used for ridge augmentation. Reconstruction of a vertical defect is challenging as contraction of the overlying soft tissue matrix causes resorption and migration of the graft, resulting in net loss of bone. Soft tissue matrix, if expanded, surgically maintains the space .This decreases pressure of the overlying soft tissue onto the graft and hence prevents its resorption.5, 6
Autogenous grafts are considered the gold standard, although postoperative complications like donor site morbidity, altered sensation, and unpredictable resorption of autogenous graft have been reported.7, 8 Alloplasts, like beta tricalcium phosphate (β TCP), Hydroxyapatite (HA), bioactive glass etc are synthetic bone substitutes, which offer the advantage of unlimited supply and avoidance of a second surgical site. Among these, β TCP has been found as a potent bone graft substitute, with sufficient strength, for alveolar ridge augmentation.9
The purpose of this study was to qualitatively and quantitatively assess bone regeneration potential of tentpole technique using beta tricalcium phosphate bone graft in vertically deficient alveolar ridges.
2. Materials and method
This is a prospective study. The study comprised of 20 patients, within age limit of 18-60 years,with clinically resorbed ridges. Patients were evaluated on the basis of clinical and radiographic examination. Patiens were enrolled in the study after obtaining informed consent. Ethical approval was taken from institutional ethical committee.
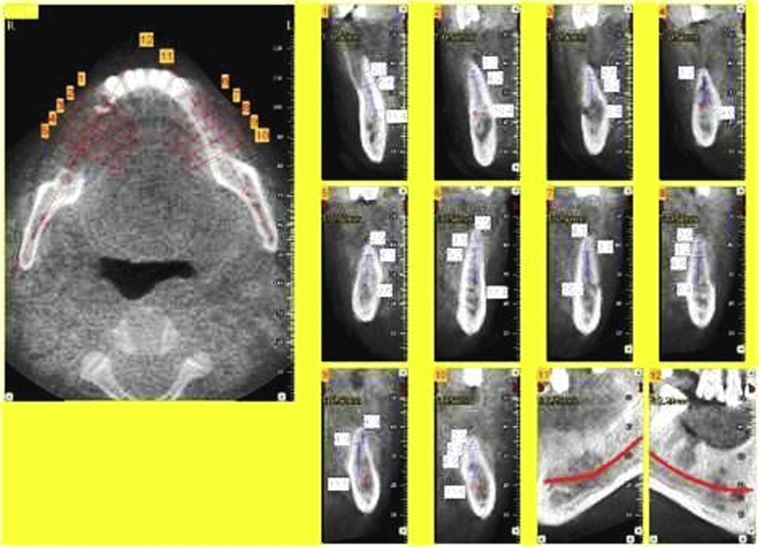
Patients having any debilitating disease, systemic autoimmune disease, disturbed coagulation ability, allergic reaction to metals; medications, smokers were excluded from the study. Preoperative clinical and radiographic (intraoral periapical radiograph, orthopantomogram, dentascan) evaluation were done to record bone loss. The bone height was measured using Dentascan. (Fig. 1)
Fig. 1.
Dentascan showing measurement of bone height.
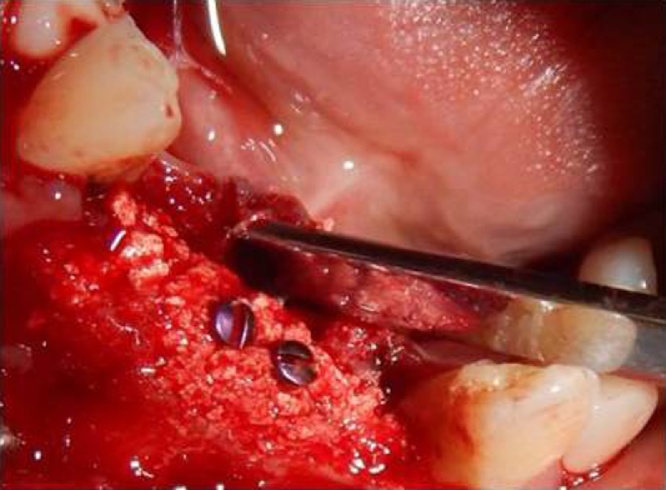
The procedure was performed under local anaesthesia. Standard part preparation and surgical draping was done to ensure sterile field. Crestal incision along with releasing incisions was placed and mucoperiosteal flap was elevated to expose the defect. 1.5 mm diameter titanium screws of various lengths were placed strategically as tenting screws to create the potential threshold of vertical bone gain. 2 ml of autologous blood was drawn;mixed with β TCP synthetic bone graft (chronOS, Synthes) and placed around the tenting screws to cover up to the screw head. Primary closure was done with 3-0 black silk using mattress suture. Standard post operative instructions and chlorhexidine mouth rinses were advised. (Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6)
Fig. 2.
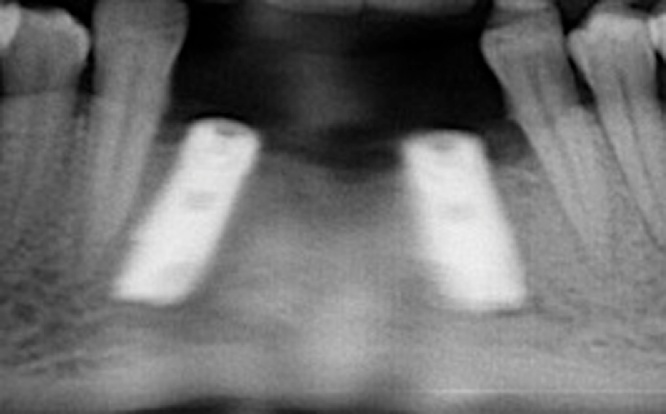
Preoperative Radiograph.
Fig. 3.
Tenting Screws.
Fig. 4.
Bone graft with screws.
Fig. 5.
Postoperative 6 month with implant.
Fig. 6.
With final prosthesis in place.
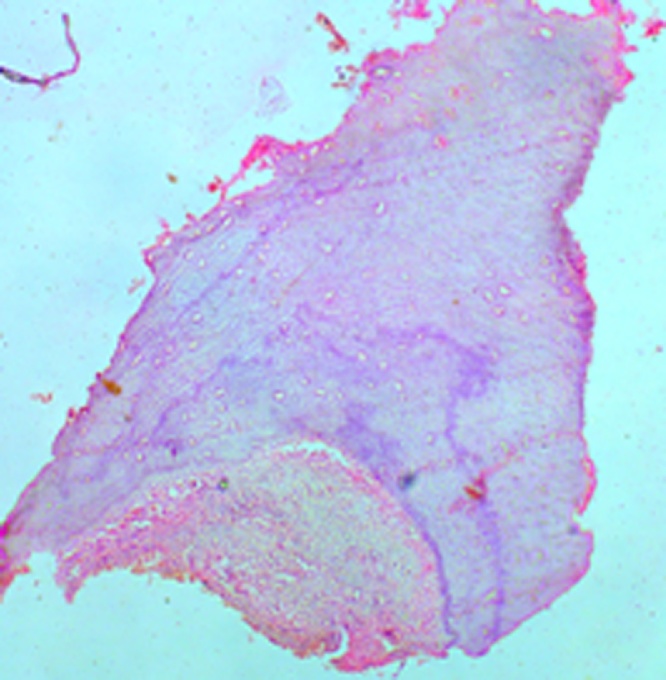
Postoperative clinical and radiographic assessment included recording of pain, discharge, or loosening of screws. Assessment of pain was done based on VAS scale. Erythema, discharge and loosening were assessed as present or absent. Assessment was done at 1,3 and 6 months postoperatively. Preoperative and postoperative clinical and radiographic assessment was done at the time of implant placement. Follow up OPG was done after implant placement and functional rehabilitation. Biochemical analysis of Osteopontin and RANKL by ELISA method was done preoperative and at 3 months postoperative. Histologic analysis of bone core collected while removal of screw was done at 6 months post-operative. (Fig. 7). Images were analyzed using microscopes from Leica at 10 x and 40x. Image J software (Java based image processing program developed at National Institute of Health) was used for quantitative estimation of new bone.
Fig. 7.
Histologic analysis showing new bone (10×).
Statistical Analysis was done. The mean change from preoperative to subsequent follow-up was assessed by Wilcoxon rank sum test. 95% confidence interval (CI) of mean was calculated. The p-value<0.05 was considered significant. All the analysis was carried out on SPSS 16.0 version (Chicago, Inc., USA).
3. Results
A total of 20 patients were included in the study with maximum being in the age range of 25-50 years and females(55%) > males(45%). (Table 1)
Table 1.
prospective study with maximum being in the age range of 25–50 years and females(55%) > males(45%).
| patient | Age (years) | sex | Implant site | Height gain at 6 month follow up (mm) |
|---|---|---|---|---|
| 1 | 45 | F | 31,41 | 3 |
| 2 | 33 | M | 46,47 | 3.5 |
| 3 | 23 | F | 23 | 2.5 |
| 4 | 30 | F | 31,41 | 2 |
| 5 | 28 | F | 22 | 2.5 |
| 6 | 24 | M | 16 | 3 |
| 7 | 16 | F | 11,21,23,24 | 3 |
| 8 | 30 | F | 36 | 2.5 |
| 9 | 18 | M | 31,41 | – |
| 10 | 52 | F | 34,36 | 2 |
| 11 | 32 | F | 46,47 | 2.5 |
| 12 | 36 | M | 46 | 2 |
| 13 | 19 | F | 31,41 | 2.5 |
| 14 | 36 | M | 36 | 2 |
| 15 | 52 | F | 44,46 | – |
| 16. | 26 | F | 13 | 2.5 |
| 17 | 32 | M | 21 | 3 |
| 18 | 53 | M | 35,37 | 2.5 |
| 19 | 24 | M | 22,23 | 3 |
| 20 | 25 | M | 31,32,41 | 2.5 |
A significant decrease in pain score was seen from 24 hours post op to 1 month post op (p = 0.0001). The pain score was 3.65 ± 0.74 (95%CI = 3.30-4.00) at 24 hours. The pain decreased 0.20 ± 0.41 (95%CI = 0.20 ± 0.41) at 1 month. The pain became nil at 3 and 6 months. The erythema score was 0.30 ± 0.47 (95%CI = 0.08-0.52) at 24 hours and became nil at 1, 3 and 6 months.
There was no postoperative wound infection. Loosening of screw was seen in two patients. There was no postoperative erythema or discharge.
There was significant gain in bone height (p = 0.0001) from preop to 6 months post op, mean 2.87 ± 0.79 (95%CI = 2.50–3.24) at 6 months post operative. (Table 2)
Table 2.
Gain in bone height from pre-op to subsequent time periods.
 |
Of the 31 implants placed, all implants osseointegrated. There was no significant change in levels of RANKL and Osteopontin from preoperative to 3 months postoperative (p > 0.05).
Bone cores collected at the time of screw removal were sent for histologic examination using haematoxylin eosin stain, and revealed new bone formation. Quantitative measurement of new bone was done with the help of Image J software which revealed 80% new vital bone content.
4. Discussion
Alveolar ridge augmentation is necessary for maintaining proper interarch dimensions and esthetics. Various grafts available for alveolar ridge reconstruction include autografts, allografts, xenografts, and alloplasts. We used βTCP bone graft, a biocompatible alloplast which has osteoconductive action.
β TCP has been shown to be efficacious in maintaining ridge dimensions after extraction. Regeneration of bone clinically and radiographically by βTCP has shown to have enough density to support implant material.10 Histologic evidence of new bone formation with β TCP has also been reported9.
The most common limitation in reconstruction of the defect is the resorption of bone graft due to the contraction of the overlying soft tissue volume. In our study, maintenance of the soft tissue volume was done by strategic placement of titanium screws as “tent poles”.
A mean gain in bone height of 10.2 mm using tentpole technique using implants as “tent pole” with iliac crest graft was successfully obtained by Marx,5 but short term paresthesia was seen in their study. When an autogenous block bone graft was compared with particulate autogenous block bone graft covered by a nonresorbable expanded polytetrafluoroethylene (ePTFE) membrane for vertical bone augmentation, block grafts were found to outperform the particulate grafts in terms of bone-to-implant contact and bone fill values.11 However autogenous grafts are associated with donor site morbidity, increased surgical time (increasing rates of infection), general anaesthesia and lengthier hospital stays.12
Korpi et al13 achieved mean alveolar ridge augmentation of 6.3 mm with autogenous bone graft from posterior iliac crest and transcutaneous approach. Mental nerve paresthesia was seen immediately after in two of their patients. Another study showed a mean gain of 9.7 mm when tenting of the periosteum matrix was done using 1.5 mm titanium screws with particulate human mineralised allograft but wound dehiscence was seen in two cases.10 The feasibility of screw tentpole technique combined with guided bone regeneration was evaluated in a complicated tridemensional alveolar ridge defect caused by maxillary tumor surgery where regenerated bone was achieved 10 months later, leading to a successful maxillary prosthesis.14
Wang evaluated porous β- TCP combined with autologous osteoblasts to augment edentulous alveolar ridge in a canine model, and demonstrated the potential of porous β-TCP as a substrate for autogenous osteoblasts in bone tissue engineering for alveolar ridge augmentation.15
In this study also, we used titanium screws as “tent pole” which prevented contraction of the soft tissue around the β TCP graft material used in our study. We performed the surgical procedure under local anaesthesia thereby avoiding the risks of general anaesthesia. Surgical principles like tension free closure and use of releasing incisions were followed.16 We observed a mean gain of 2.87+/−0.79 in bone height at 6months. No paresthesia was reported in our study. None of our patients showed any sign of postoperative infection or wound dehiscence. There was no postoperative erythema or discharge. All incisions healed properly. Loosening of screw was seen in two cases in this study. Histologic examination of the bone core collected during removal of screw, revealed formation of new vital bone and quantitative estimation revealed new vital bone content to be about 80%.
No significant change was observed statistically in the values of Osteopontin and RANKL at baseline and at 3 postoperative months. This may be attributed to the fact that intravenous blood sample was taken for estimation of RANKL and Osteopontin. Local tissue samples might have been more representative of real measures.
5. Conclusion
We conclude that it is a safe and effective procedure for bone regeneration in vertically deficient alveolar ridges and presents minimal complications. However, our study relates the experience of one hospital only. More studies with long term follow up are needed to evaluate the stability of vertically grafted bone after long term loading and for definite conclusion.
Conflict of Interest
None.
Contributor Information
Dipti Daga, Email: diptidaga10@gmail.com.
Divya Mehrotra, Email: divyamehrotra@hotmail.com.
References
- 1.Rachmiel A., Srouji S., Peled M. Alveolar ridge augmentation by distraction osteogenesis. Int J Oral Maxillofac Surg. 2001;30(6):510–517. doi: 10.1054/ijom.2001.0134. [DOI] [PubMed] [Google Scholar]
- 2.Keller E.E., Tolman D.E., Eckert S. Surgical-prosthodontic reconstruction of advanced maxillary bone compromise with autogenous onlay block bone grafts and osseointegrated endosseous implants: a 12-year study of 32 consecutive patients. Int J Oral Maxillofac Implants. 1999;14(2):197–209. [PubMed] [Google Scholar]
- 3.Buser D., Dula K., Hess D., Hirt H.P., Belser U.C. Localized ridge augmentation with autografts and barrier membranes. Periodontol. 2000;1999(19):151–163. doi: 10.1111/j.1600-0757.1999.tb00153.x. Review. [DOI] [PubMed] [Google Scholar]
- 4.Boyne P.J., Cole M.D., Stringer D., Shafqat J.P. A technique for osseous restoration of deficient edentulous maxillary ridges. J Oral Maxillofac Surg. 1985;43(2):87–91. doi: 10.1016/0278-2391(85)90054-0. [DOI] [PubMed] [Google Scholar]
- 5.Marx R.E., Shellenberger T., Wimsatt J., Correa P. Severely resorbed mandible: predictable reconstruction with soft tissue matrix expansion (tent pole) grafts. J Oral Maxillofac Surg. 2002;60(8):878–888. doi: 10.1053/joms.2002.33856. [DOI] [PubMed] [Google Scholar]
- 6.Daga D., Mehrotra D., Mohammad S., Singh G., Natu S.M. Tentpole technique for bone regeneration in vertically deficient alveolar ridges: A review. J Oral Biol Craniofac Res. 2015;5(2):92–97. doi: 10.1016/j.jobcr.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.(a) Clavero J., Lundgren S. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res. 2003;5(3):154–160. doi: 10.1111/j.1708-8208.2003.tb00197.x. [DOI] [PubMed] [Google Scholar]; (b) Joshi A. An investigation of post-operative morbidity following chin graft surgery. Br Dent J. 2004;196(4):215–218. doi: 10.1038/sj.bdj.4810987. 28. [DOI] [PubMed] [Google Scholar]
- 8.Yamauchi K., Takahashi T., Funaki K., Hamada Y., Yamashita Y. Histological and histomorphometrical comparative study of β-tricalcium phosphate block grafts and periosteal expansion osteogenesis for alveolar bone augmentation. Int J Oral Maxillofac Surg. 2010;39(10):1000–1006. doi: 10.1016/j.ijom.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Horowitz R.A., Mazor Z., Miller R.J., Krauser J., Prasad H.S., Rohrer M.D. Clinical evaluation alveolar ridge preservation with a beta-tricalcium phosphate socket graft. Compend Contin Educ Dent. 2009;30(9):588–590. 592, 594 passim; quiz 604, 606. [PubMed] [Google Scholar]
- 10.Le B., Rohrer M.D., Prasad H.S. Screw tent-pole grafting technique for reconstruction of large vertical alveolar ridge defects using human mineralized Allograft for implant site preparation. J Oral Maxillofac Surg. 2010;68(2):428–435. doi: 10.1016/j.joms.2009.04.059. [DOI] [PubMed] [Google Scholar]
- 11.Rocchietta I., Simion M., Hoffmann M., Trisciuoglio D., Benigni M., Dahlin C. Vertical Bone Augmentation with an Autogenous Block or Particles in Combination with Guided Bone Regeneration: A Clinical and Histological Preliminary Study in Humans. Clin Implant Dent Relat Res. 2016;18(1):19–29. doi: 10.1111/cid.12267. [DOI] [PubMed] [Google Scholar]
- 12.Patel N., Kim B., Zaid W., Spagnoli D. Tissue Engineering for Vertical Ridge Reconstruction. Oral Maxillofac Surg Cl North Am. 2017;29(1):27–49. doi: 10.1016/j.coms.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Korpi J.T., Kainulainen V.T., Sándor G.K., Oikarinen K.S. Long-term follow-up of severely resorbed mandibles reconstructed using tent pole technique without Platelet-rich plasma. J Oral Maxillofac Surg. 2012;70(11):2543–2548. doi: 10.1016/j.joms.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 14.Xiao T., Zhao Y., Luo E., Hu J. Tent-Pole for Reconstruction of Large Alveolar Defects: A Case Report. J Oral Maxillofac Surg. 2016;74(1):55–67. doi: 10.1016/j.joms.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Wang S., Zhang Z., Zhao J., Zhang X., Jiang X. Vertical alveolar ridge augmentation with β-tricalcium phosphate and autologous osteoblasts in canine mandible. Biomater. 2009;30(13):2489–2498. doi: 10.1016/j.biomaterials.2008.12.067. [DOI] [PubMed] [Google Scholar]
- 16.Wang H.L., Boyapati L. PASS principles for predictable bone regeneration. Implant Dent. 2006;15(1):8–17. doi: 10.1097/01.id.0000204762.39826.0f. [DOI] [PubMed] [Google Scholar]