Abstract
Plants & their extracts have immense potential for the management or treatment of the wounds. The pyhto medicines for the wound healing are not only cheap & affordable but are purportedly safe as hypersensitivity reactions are rarely encountered with the use of these agents, these natural agents induce healing & regeneration of the lost tissue by multiple mechanisms Turmeric commonly is called as Haldi in Hindi. C Longa has been reported to possess anti bacterial, anti fungal & anti inflammatory activities. Turmeric is known as traditional herb to Asia & India also called as curcuma longa, with maximum healing properties & other great uses. It is widely used in India & China for traditional Chinese medicine. This act as anti inflammatory agent to treat different kind of diseases & health problems.
Aims & objectives
The aim of this study was to study the therapeutic, healing benefits of turmeric, an herb commonly used in Asia
Material & methods
The study was conducted in department of oral & maxillofacial surgery of Indira Gandhi government dental college jammu.178 patients were selected from the outpatient department of oral & maxillofacial surgery. The diagnosis of dry socket was made clinically. Turmeric dressing with mustard oil was given in group A & in group B ZOE dressing was given.
Results
In this study there was significant reduction in pain, inflammation & discomfort after turmeric and ZOE dressing. Wound healing was seen faster, than dressing with ZOE. There is no side effect of Turmeric. Statistical analysis was done p < 0.05, was found statistically significant
Keywords: Mustard oil, dry socket, Curcumin, Holy powder, Anti-inflammatory
1. Introduction
Wound is defined as the disruption of the cellular & anatomic continuity of a tissue of a tissue1 or as a break in integrity of skin or mucosa & may also be defined as a loss or breaking of cellular & anatomic of functional continuity of living tissue.2 Wound may be produced by physical, chemical, thermal, microbial or immunological insult to the tissues & damage to the skin or mucosa is a good medium for entry & growth of micro organism.
Alveolar osteitis also called dry socket is the most common post extraction complication of teeth, most commonly occurring in 40–45 years of age. Traumatic extraction, aggressive curettage & irrigation, oral microorganisms, remaining fragments of bone & root in extraction wound, dislodgement of blood clot by excessive mouth rinsing & gargles by patient, oral contraceptives & smoking are important etiologic factors responsible for dry socket. There is loss of blood clot from socket. Symptom ranges from mild discomfort to sever pain, radiating to temporal region, TMJ, ear & eye, halitosis, empty socket & Trismis.
There are various modalities used for management of dry socket like use obtund ant & pain reducing dressing such as zinc oxide euginol dressing,anti infective agents, systemic or local,anti fibrinolytic agent & surgical intervention to remove necrotic clot & encourage the formation of blood clot. Treatment include administration of drugs either locally or systemically in attempt to initiate wound repair.3 The topical agents include antibiotic & antiseptic,4 dislodging agent (chemical debridement eg hydrogen peroxide,eusol & collagenase ointment).5 Wound healing promoters eg tretinoin,aloe Vera extract honey comfrey, benzoyl peroxide,dexapanthol, tetrachloridecaxide solution,clostebol acetate & chamomillia
Various substances like tissue extracts,6 vitamins & minerals & No of plant products7 have been reported by various workers to possess pro healing effects. Wound healing herbals accelerates blood clotting,fight infection & accelerates the wound healing also. Plants or chemicals derived from plants need to be identified & formulated for treatment & management of wounds. No of herbal products are being investigated at present & various herbal products have been used in management of wounds over the years, few of them are Aloe Vera, Neem, cedrus, turmeric, jasmine auriculatum.
Turmeric is an amazing natural herbal with healing properties. It has been used as traditional remedy in ayurvedic medicine for thousands of years. it has powerful anti oxidant & anti inflammatory properties.8, 9, 10 Turmeric has many valuable components but the one seems getting attention is curcumin.11 Curcumin is a yellow pigment present in the spice turmeric (curcuma Longa) & has been linked with anti oxidant,anti inflammatory,antiprolifeartive,anti diabetic,anticancer,anti viral,& anti Rheumatic effects.
In India & Asia this native traditional herb is called holy powder because of its anti inflammatory properties to treat different kinds of diseases & health problems, digestive difficulties, treatment of infections & wounds. It is only soluble in fat, so curcumin is best to combine with fats, coconut milk, ghee, butter, oils etc.11 In the present study turmeric powder was mixed with mustard oil to make paste.
2. Methodology
A total of 178 patients of dry socket were selected from outpatient department of Oral & Maxillofacial surgery. Patients with systemic ailments like diabetes, patients on steroid therapy, hypothyroid patients, pregnant & lactating mothers were not included in the study. The informed consent was taken from the patient. Diagnosis of dry socket was made clinically. Wound was checked for necrotic bone, fetid odour, pain swelling, and pus discharge. Patients were divided in two groups
GROUP A was treated with a dressing of turmeric & mustard oil.
GROUP B was treated with zinc oxide euginol dressing.
Dried Rhizome of C longa (Haldi) collected from local market was crushed into powder using a mechanical blender. The fine powder was obtained after sieving using 150 Mm sieve. This powder was stored & fresh dressing using sterile gauge & mustard oil was prepared. This dressing was done on alternate days till symptoms subsided. After irrigation with saline socket was packed with dressing. (Fig. 1, Fig 2, Fig. 3) This study was under taken to evaluate the effect of turmeric dressing in management of dry socket wound
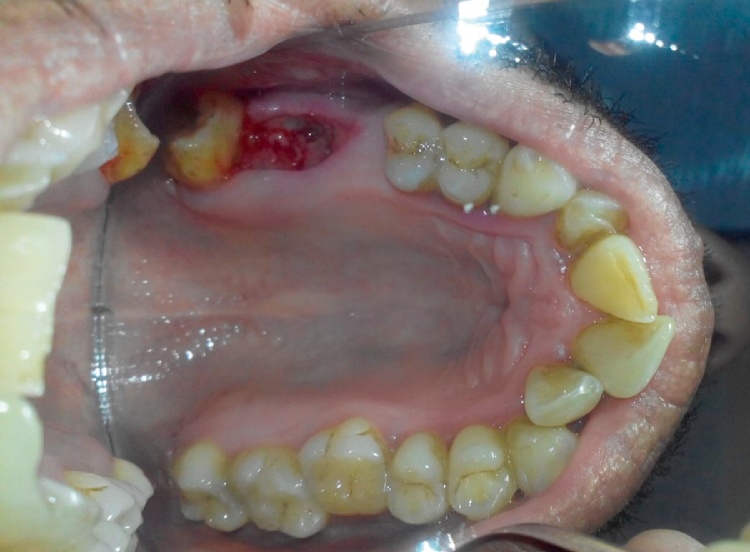
Fig. 1.
Dry socket wound.
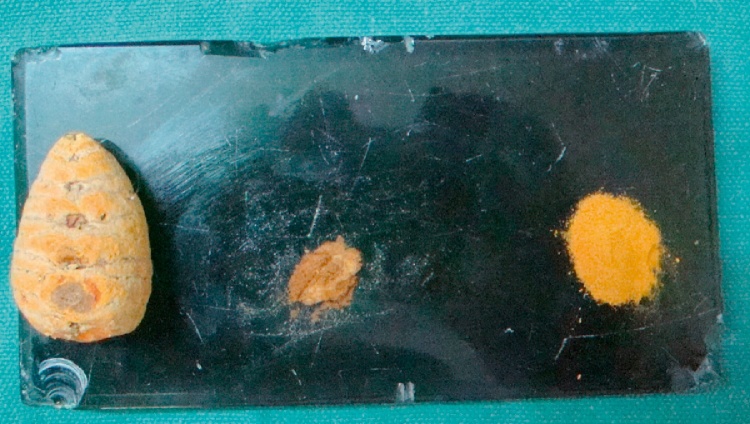
Fig 2.
Dressing prepared.
Fig. 3.
Dressing in socket.
3. Results
In group A all the symptoms like pain, swelling, necrotic socket,halitosis,started subsiding from 2 nd day as shown in Table 1 & bar graph. Whereas in group B in majority of the patients symptoms started subsiding on 4 th dressing onwards
Table 1.
Number of patients revealed subsided symptoms in different days of dressing.
| Group | Day of dressing |
Total | |||||
|---|---|---|---|---|---|---|---|
| 2nd | 3rd | 4th | 5th | 6th | 7th | ||
| Group A | 55 | 25 | 10 | 0 | 0 | 0 | 90 |
| group B | 0 | 0 | 40 | 37 | 0 | 11 | 88 |
| Total | 55 | 25 | 50 | 37 | 0 | 11 | 178 |
Test of significance between two treatment groups (Chi-square test/goodness of fit test)
H0 (Null hypothesis)
Two treatment groups are independent i.e. No difference between two treatments is seen
H1 (Alternate hypothesis)
Two treatment groups are not independent i.e. significant difference between two treatments is noted
Note: 6 th day figure not considered for calculation as none of the cases was reported. After (χ2 test) p < 0.05, reject H0, statistically significant. (Table 2)
Table 2.
Test calculation (χ2 tests).
| Group | 2nd Day | 3rd Day | 4th Day | 5th Day | 7th Day | Total |
|---|---|---|---|---|---|---|
| Observed Frequency | ||||||
| Group A | 55 | 25 | 10 | 0 | 0 | 90 |
| group B | 0 | 0 | 40 | 37 | 11 | 88 |
| Total | 55 | 25 | 50 | 37 | 11 | 178 |
| Expected frequency | ||||||
| Group A | 27.81 | 12.64 | 25.28 | 18.71 | 5.56 | 90 |
| group B | 27.19 | 12.36 | 24.72 | 18.29 | 5.44 | 88 |
| Total | 55 | 25 | 50 | 37 | 11 | 178 |
| df | 4 | |||||
| p | 1.47E-30 | |||||
| α | 0.05 | |||||
4. Discussion
Dry socket alveolar osteitis is a very common complication after extraction or surgical removal of tooth. Commonly known as “dry socket” this condition remains a common postoperative problem that results in severe pain and repeated practice/hospital visits.12 most studies have shown that the incidence of dry socket is 1–4% of all routine dental extractions. & 5–30% of impacted third molar.13, 14 In the present study dry socket was seen in 7% extractions & 4% after impactions
Onset of Alveolar osteitis (AO) is 1–3 days after tooth extraction & duration usually ranges from 5 to 10 days. Similarly in the present study Patients with the symptoms reported as follows 58 on 5 th day, 24 on 4 th day 22 on 6 th day 13 on 7 th 3 on 9 th day.15
During last century many attempts have been made to find proper way of preventing & management of dry socket & large no of clinical studies have been carried out in these subjects. Medical treatment of wound include administration of drugs either locally or systemically in an attempt to aid wound repair.16 Various herbal products have been used in wound management like, Aloe Vera, Neem, & turmeric. Turmeric, curcuma longa, cedrus deodar, jasminum auriculatum. Honey has been used in management alveolar osteitis.16
C.longa commonly known as turmeric & Haldi in Hindi has been reported to possess antibacterial, anti-fungal activities.17 Turmeric extract rich in curcuminoids a widely known for its anti inflammatory, anti oxidant & anti microbial properties. The mechanism of action of Curcumin may be considered as multicentric since it act as a prostaglandin inhibitor,stabilizer of the liposomal membrane,inhibitor of the activity of leucotrienes & thromboxaneB4 without effecting the synthesis of prostacyclines,stimulator of adrenal steroidogenesis,substance P Depletor in nerve terminals,analgesic & anti oxidant.18, 19
Curcuma longa also contains proteins,fats, (A,B,c) all have important role in wound healing & regeneration.20 The anti-inflammatory property & presence of vit A & protein result in early synthesis of collagen fibers by mimicking fibroblastic activity. Juice of fresh rhizome is commonly applied to recent wounds, bruises & leech bites.21
The anti-inflammatory properties of curcumin were shown to inhibit the 5-lipoxygenase activity in rat peritoneal neutrophils as well as the 12-lipoxygenase and the cyclooxygenase activities in human platelets.22 Curcumin had no significant effect on quercetin-induced nuclear DNA damage, lipid per oxidation and protein degradation and thus has the unique potential of acting as both pro- and antioxidants, depending on the redox state of their biological environment. Extensive in vitro and in vivo testing has shown that turmeric inhibits chemically-induced epidermal ornithine decarboxylase activity, epidermal DNA synthesis, and the promotion of skin tumours in mice.23
Turmeric also reduce arachidonic acid induced rat paw & mouse skin oedema & markedly inhibit epidermal lipoxygenase & cyclooxygenase activity in vitro as reported in few studies.24
Ingestion of turmeric has demonstrated a bacteriostatic or bactericidal effect against organism involved in cholecystitis & has been used to treat biliary infection in humans. Topical application of turmeric paste has shown good results in scabies.25
It has been demonstrated that turmeric helps in treatment of chronic ulcers through the following mechanism 1) microcirculation improvement 2) angiogenesis stimulation 3) granulation tissue formation promotion, 4) re epithelialization acceleration. All of the wounds in their study exhibited the typical pattern of wound healing, with minimal wound contraction noted during the initial lag phase followed by a rapid increase in wound contraction during the proliferative phase day 6 today 25.It has been reported that with topical or oral use of turmeric the size of wound reduced significantly during proliferative phase when compared to wound size treated with saline. This shows that oral intake or topical application of turmeric may enhance wound healing & contraction of wound when compared with daily cleansing with saline & ZOE dressing. Turmeric powder was tested for its healing abilities in acute wounds created by surgical incisions before entering the clinical trials.26
5. Conclusion
The present study was done to use turmeric to promote wound healing. We found that the use of turmeric at the site of an injury by topical application promotes healing of wounds. The results of present study clearly indicated that the turmeric Accelerated wound healing process. & has great potential for wound healing. Therefore the turmeric can be used in different forms for treating different ailments including surgical wounds.
Contributor Information
Parveen Akhter Lone, Email: parveen.lone@yahoo.com.
Syed wakeel Ahmed, Email: syedwakeel12@gmail.com.
Vivek Prasad, Email: Drprasadvivek1991@gmail.com.
Bashir Ahmed, Email: basher@jugga.com.
References
- 1.Bennet R.G. C.V.Mosby; St. Louis: 1988. Fundamentals of Cutaneous Surgery. [778] [Google Scholar]
- 2.Rizvi S.C., Vinay K., Stainly R. 2017. Pathologic Basis of the Disease WB Saunders Company Philade Curcuma Longa Linn. [Google Scholar]
- 3.Savanth S.S., Shah R.A. In: Text Book and Atlas of Dermatology and Cosmetology. 1 st edn. Savant S.S., Shah R.A., Gore D., editors. ASCAD; Mumbai: 1998. pp. 12–17. [Google Scholar]
- 4.Chulani H.L. 1st edn. Radhakrishan Medical and Educational Trust; Mumbai: 1996. The Law of Medical Negligence; pp. 51–83. [Google Scholar]
- 5.Savanth S.S., Mehta N. In: Text Book & Atlas of Dermatosurgery & Cosmetology. 1st edition. Savanth S.S., Shah R.A., Gore D., editors. ASCAD; Mumbai: 1996. pp. 50–61. [Google Scholar]
- 6.Rao S.G., Udupa A.L., Udupa S.L., Rao P.G.M., Rao Ganesh., Kulkarni D.R. Calendula and Hypericum: two homeopathic drugs promoting wound healing in rat. Fitoterapia. 1991;LXII(6):508–510. [Google Scholar]
- 7.Dahanukar S.A., Kulkarni R.A., Rege N.N. Pharmacology of medicinal plants and natural products. Indian J Pharmacol. 2000;32:S81–S118. [Google Scholar]
- 8.Menon V.P., Sudheer A.R. Antioxidant & anti inflammatory properties of curcumin. Adv Exp Med Biol. 2007;595:105–125. doi: 10.1007/978-0-387-46401-5_3. [Article] [DOI] [PubMed] [Google Scholar]
- 9.Jagetia G., Aggarwal C.B.B. Spicing up of the immune system by curcumin. J Clin Immunol. 2007;27(1):19–35. doi: 10.1007/s10875-006-9066-7. [DOI] [PubMed] [Google Scholar]
- 10.White B. D. Z. clinical inquiry,does turmeric relieve inflammatory condition? J Fam pract. 2011;60(3):155–156. [11 Pari] [PubMed] [Google Scholar]
- 11.Tewas D., Eckel J. Role of curcumin in health & diseases. Arch physiol Biochem. 2008;114(2):127–149. doi: 10.1080/13813450802033958. [DOI] [PubMed] [Google Scholar]
- 12.Rood J.P., Danford M. Metronidazole in the treatment of Dry Socket. Int J Oral Surg. 1981;10:345–347. doi: 10.1016/s0300-9785(81)80032-4. [DOI] [PubMed] [Google Scholar]
- 13.Rud J. Removal of impacted lower third molar with acute pericoronitis and acute nectrotizing gingivitis. Br J Oral Surg. 1970;7:153–159. doi: 10.1016/s0007-117x(69)80015-6. [DOI] [PubMed] [Google Scholar]
- 14.Blum I.R. Contemporary views of dry socket (AO): a clinical appraisal of standardization, aetiopathogenesis and management: a clinical review. Int J Oral Maxillofac Surg. 2002;31:309–317. doi: 10.1054/ijom.2002.0263. [DOI] [PubMed] [Google Scholar]
- 15.Trieger N., Schlagel G.D. Preventing dry socket: a simple procedure that works. J Am Dent Assoc. 1991;122:67–68. doi: 10.14219/jada.archive.1991.0067. [DOI] [PubMed] [Google Scholar]
- 16.Sanchis J.M., Penarrocha M. Tetracycline compound placement to prevent dry socket: a postoperative study of 200 impacted mandibular third molars. J Oral Maxillofac Surg. 2004;62:587–591. doi: 10.1016/j.joms.2003.08.035. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt J.M., Greenspoon J.S. Aloe vera dermal wound gel is associated with a delay in wound healing. Obstet Gynecol. 1991;78:115–117. [PubMed] [Google Scholar]
- 18.Chopra R.N., Nayar S.L., Chopra I.C. Vol. 1. CSIR; New Delhi: 1986. (Glossary of Indian Medicinal Plants). [Google Scholar]
- 19.Jorge Alonso. Vol. 1. Corpus; Barcelona: 2004. pp. 395–403. (Tratado De Fitofármacos Y Nutracéuticos). [633.8 ALO] [Google Scholar]
- 20.Srimal R.C. Turmeric: a brief review of medicinal properties. Fitoterapia. 1997;68(6):83–94. [ref.2503] [Google Scholar]
- 21.Rao S.G.V., Selvaraj J., Senthil R., Radhakrishnan R.N., Murali Manokar B. Efficacy of some indigenous medicines in wound healing in rats. Indian J Anim Sci. 2003;73:652–653. [Google Scholar]
- 22.Kumar A.S., Singh H.P., Parkash Prem, Singh S.P. Efficacy of some indigenous drugs in tissue repair in buffaloes. Indian Vet J. 1993;70:42–44. [Google Scholar]
- 23.Ammon H.P.T. Mechanism of antiinflammatory actions of curcumine and boswellic acids. J Ethopharmacol. 1993;38:113–119. doi: 10.1016/0378-8741(93)90005-p. [DOI] [PubMed] [Google Scholar]
- 24.Huang M.T. Inhibitory effect of curcumin, chlorogenic acid, caffeic acid, and ferulic acid on tumor promotion in mouse skin by 12-O-tetradecanoylphorbol-13-acetate. Cancer Res. 1988;48:5941–5946. [PubMed] [Google Scholar]
- 25.Conney A.H. Inhibitory effect of curcumin and some related dietary compounds on tumor promotion and arachidonic acid metabolism in mouse skin. Adv Enzyme Regul. 1991;31:385–396. doi: 10.1016/0065-2571(91)90025-h. [DOI] [PubMed] [Google Scholar]
- 26.Ramprasad C. Observation on the Pharmacology of Curcuma Longa, Linn. Ind. J. Phys. and Pharm. A. 1957;1:136–143. [Google Scholar]