Introduction
Fungus balls or fungal bezoars in the urinary bladder are extremely rare diseases, of which less than 20 previous cases have been described in the literature since the first case was reported in 1961.1 The most common predisposing factor for this opportunistic infection is diabetes mellitus.2 We herein report a case of bladder candidiasis initially misdiagnosed as bladder cancer based on its MRI findings.
Case report
A 75-year-old man was admitted to our department with chief complaints of gross hematuria and incontinence that had been deteriorating for several days. His medical history included untreated type II diabetes mellitus diagnosed eight years earlier. A routine urinalysis showed a significantly high red blood cell count (>100 per high-power field; HPF) and white blood cell count (5–9 per HPF). Ultrasonography revealed obvious residual urine and coagulation in the urinary bladder but no presence of benign prostatic hyperplasia. Thus, a diagnosis of neurogenic bladder with bacterial cystitis was made. He had a urethral catheter inserted and was prescribed oral antibiotics. Three days later, he visited us again due to urinary retention. Laboratory studies were performed: white blood cells 17200/μL, blood urea nitrogen 92.3 mg/dL, creatinine 6.45 mg/dL, C-reactive protein 17.08 mg/dL, glucose 460 mg/dL, and Hb-A1c 14.4%. Under the diagnosis of post-renal acute kidney injury and a urinary tract infection (UTI), he was hospitalized to receive bladder perfusion therapy, intravascular antibiotics (Cefmetazole 1 g q12 h), and strict blood glucose control.
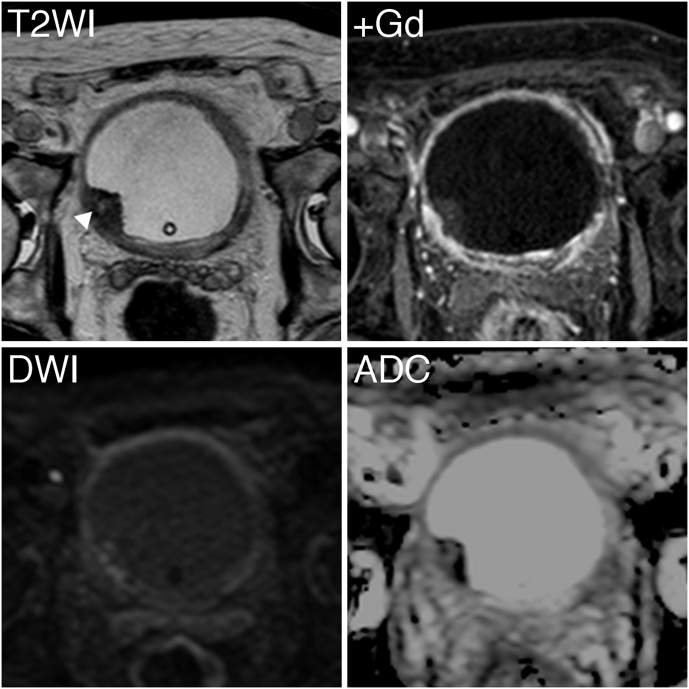
Magnetic resonance imaging (MRI) identified a 20-mm mass on the right lateral wall of the bladder showing hypointensity on T2-weighted imaging, enhancement after gadolinium administration, diffusion restriction, and a low value on apparent diffusion coefficient (ADC) mapping (Fig. 1). Computed tomography showed bilateral hydronephrosis and a thickening wall of the bladder with no evidence of distant metastasis. Cystoscopy revealed an immobile polypoid mass covered with white fur resembling necrotic debris in the same location. Based on these findings, a diagnosis of bladder cancer (cT1N0M0) was made. Subsequently, he underwent transurethral resection (TUR) of the lesion. A pathological examination revealed candidiasis and regenerative urothelium with atypia, showing no CK20 expression except for umbrella cells and weak p53 expression predominantly in a basal distribution, which suggested this lesion was not neoplastic (Fig. 2).3
Fig. 1.
Magnetic resonance imaging findings of the pre-therapeutic urinary bladder lesion are shown. The lesion showed hypointensity for the most part despite a small portion with hyperintensity indicating necrotic portion (arrowed) on T2WI, T2-weighted imaging; enhancement on +Gd, Gadolinium-enhanced imaging; restriction on DWI, diffusion-weighted imaging; a low value on ADC, apparent diffusion coefficient mapping.
Fig. 2.
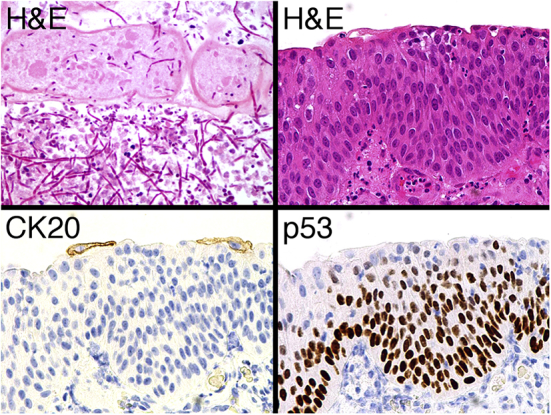
Microscopic photographs of the resected tissues are shown. Hyphae of Candida albicans were observed among degenerated epithelial cells (upper left panel; H&E, hematoxylin and eosin stain). Nuclei of the background urinary bladder epithelial cells were enlarged and irregular; however, structural atypia did not reach the degree seen in cancer cells (upper right panel). Moreover, CK20-positivity was limited in the cytoplasm of umbrella cells (lower left panel) and p53-positivity was weak in the nuclei of basal cells (lower right panel).
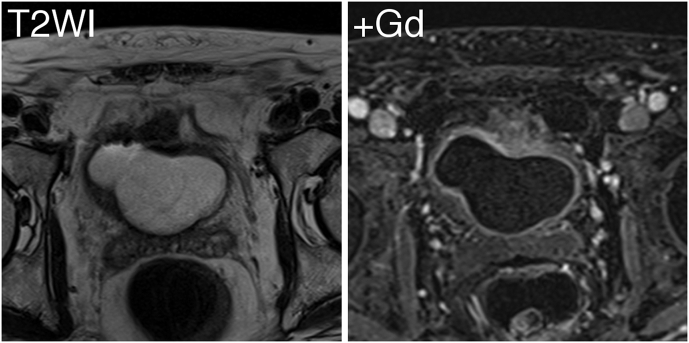
He received systemic antifungal therapy (fluconazole 100 mg once daily) for 2 weeks since Candida albicans (C. albicans) was isolated from urine. He was discharged with a urinary catheter inserted. Nevertheless, he suffered from a fever and urinary retention 2 weeks later. Urinary culture proved the presence of a bacterial infection by several species although a urine fungal culture was negative. The symptoms were relieved within a week by intravenous Cefmetazole. Follow-up MRI taken at 5 months after TUR only showed bladder wall thickness without enhancement, suggesting there was no recurrence of a fungus ball but chronic cystitis (Fig. 3). A urine fungal culture was still negative at the time. He will require a careful follow-up for this refractory disease henceforth.
Fig. 3.
Magnetic resonance imaging findings of the post-therapeutic urinary bladder lesion are shown. There was no mass lesion observed in the bladder on T2WI, T2-weighted imaging; nor was there significant enhancement of the thickening wall of the bladder on +Gd, Gadolinium-enhanced imaging.
Discussion
Fungus balls, also referred to as fungal bezoars, rarely occur in the urinary tract. C. albicans being most commonly (50%–70%) associated with fungus balls formation, other Candida species, Aspergillus, Penicillium, and Mucorales fungus balls have also been reported.2 This opportunistic infection is observed particularly frequently in patients with diabetes mellitus not only because they are immunodeficient but also because a high urinary sugar affords an excellent medium for the growth of fungus in the urinary tract.1 More importantly, urinary tract drainage devices, such as indwelling urethral catheters, were present at the time of or within 30 days prior to funguria in 83.2% of patients.4 Our patient also had untreated type II diabetes mellitus as well as an indwelling urethral catheter due to neurogenic bladder.
In the present case, the lesion was initially misdiagnosed as bladder cancer based on its MRI findings of significant enhancement by dynamic study and restricted diffusion (Fig. 1). Experience with MRI in diagnosing bladder fungal infection is very limited; to our knowledge, this is the first case for which various sequences of MRI were conducted for a fungus ball in the urinary tract. The further characterization of MRI findings on fungal UTI is desired in order to assess the diagnostic power of this sophisticated device, as the differential diagnosis of fungus balls and neoplasms is sometimes challenging and can significantly influence the clinical outcomes.
For symptomatic Candida cystitis, fluconazole is the treatment of a choice because the drug is concentrated in urine and remains a highly active antifungal agent against most species of Candida, especially C. albicans.5 The location of fungus balls in the urinary tract and the presence of indwelling devices will determine the optimum approach to therapy, including intravenous or intravesical antifungal reagents, bladder irrigation, surgical mass removal, and cystostomy. In our case, the combination of bladder irrigation, TUR, and intravenous fluconazole was successful in suppressing fungal growth with negative urine cultures for C. albicans at 7 weeks and 5 months after TUR, although our patient had bacterial cystitis at those times. Treatments for not only fungal infection but also underlying conditions, such as diabetes mellitus and neurogenic bladder, are required in order to avoid the recurrence of this disease.
Given that the number of patients with risk factors (e.g. indwelling urethral catheters, diabetes mellitus, immunosuppressive therapy, malignancy, etc.) is increasing,5 the incidence of fungal UTI is also likely to increase in the future. Therefore, fungus balls should be considered in the differential diagnosis of a bladder mass, particularly in high-risk patients.
Conflicts of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Chisholm E.R., Hutch J.A. Fungus ball (Candida albicans) formation in the bladder. J Urol. 1961;86:559–562. doi: 10.1016/S0022-5347(17)65220-0. [DOI] [PubMed] [Google Scholar]
- 2.Irby P.B., Stoller M.L., McAninch J.W. Fungal bezoars of the upper urinary tract. J Urol. 1990;143(3):447–451. doi: 10.1016/s0022-5347(17)39987-1. [DOI] [PubMed] [Google Scholar]
- 3.Mallofré C., Castillo M., Morente V., Solé M. Immunohistochemical expression of CK20, p53, and Ki-67 as objective markers of urothelial dysplasia. Mod Pathol. 2003;16(3):187–191. doi: 10.1097/01.MP.0000056628.38714.5D. [DOI] [PubMed] [Google Scholar]
- 4.Kauffman C.A., Vazquez J.A., Sobel J.D. Prospective multicenter surveillance study of funguria in hospitalized patients. The national institute for allergy and infectious diseases (NIAID) mycoses study group. Clin Infect Dis. 2000;30(1):14–18. doi: 10.1086/313583. [DOI] [PubMed] [Google Scholar]
- 5.Fisher J.F. Candida urinary tract infections–epidemiology, pathogenesis, diagnosis, and treatment: executive summary. Clin Infect Dis. 2011;52(Suppl 6):S429–S432. doi: 10.1093/cid/cir108. [DOI] [PubMed] [Google Scholar]