Abstract
Objective
Reviewing indications and characteristics of obstetric patients admitted to the intensive care unit (ICU) of a tertiary care center, comparing those patients by time period and place of delivery, and to verify clinical utility of acute physiology and chronic health evaluation (APACHE) II score in ICU-admitted women.
Methods
Retrospective analyses were carried out for parturients admitted to the ICU of our institution from 1994 to 2015. Clinical characteristics were compared between time period (period 1: 1994–2004; period 2: 2005–2015) and place of delivery (our institution and local hospitals). Receiver operating characteristic (ROC) curve analysis was used to evaluate the usefulness of APACHE II score to predict maternal mortality.
Results
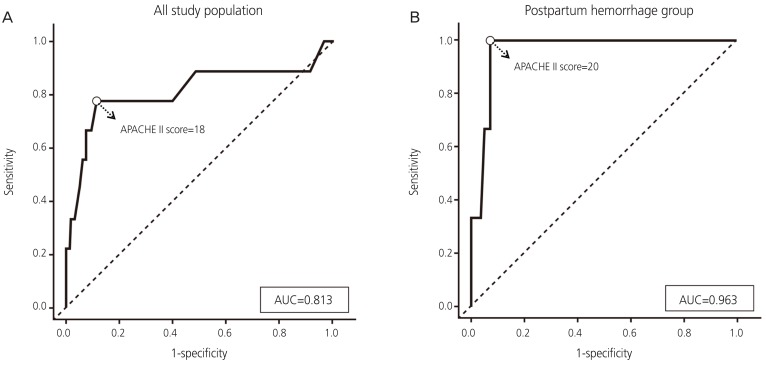
During 22-year period, 176 women required ICU admission, showing the incidence of 2.2 per 1,000 deliveries. The most common reason for ICU admission was postpartum hemorrhage (56.3%), followed by hypertensive disorders (19.3%), sepsis (3.4%), and pulmonary and amniotic fluid embolism (2.3%). Period 2 showed older maternal age (32.7±4.8 vs. 30.8±4.4 years, P=0.006, higher embolization rate (26.4% vs.1.2%, P<0.001), and lower hysterectomy rate (30.8% vs. 49.4%, P=0.012). Cases from local hospitals showed significantly higher proportion of postpartum hemorrhage (84.5% vs. 42.2%, P<0.001). Overall maternal death occurred in 5.1% (9/176) including 6 direct maternal deaths. The APACHE II score showed area under the ROC curve of 0.813 (confidence interval [CI], 0.607–1.000) for prediction of maternal mortality.
Conclusion
The incidence of obstetric ICU admission was 2.2 per 1,000 deliveries and the most common reason was postpartum hemorrhage followed by hypertensive disorders. APACHE II score could be used to predict mortality in obstetric ICU admission.
Keywords: Intensive care units, Maternal death, Postpartum hemorrhage, Amniotic fluid embolism, Acute physiology and chronic health evaluation (APACHE)
Introduction
High-risk pregnancy increases with increased maternal age, pregnancies resulting from assisted reproductive technology, and pregnancies complicated by chronic medical conditions [1,2]. To lower the risk, admission of obstetric patient to intensive care unit (ICU) is expanding. Admission rate to ICU may be considered as an objective indicator of pronounced maternal morbidity [3,4,5]. The percentage of pregnant or puerperal women who require ICU admission was reported as 0.7%–13.5% in previous studies with large variation among different countries and institutions [6], while ICU admission of parturients in developed countries was reported as less than 2% although it reach up to higher than 10% in developing countries [7,8,9,10]. Since the majority of studies on ICU-admitted parturients were conducted in the Western countries, we lack understanding of Eastern Asian subjects including those from our country.
Maternal mortality ratio (MMR) or maternal mortality rate are important indicators of obstetric care. National survey on maternal mortality in Korea started in 1995 [2,11] and MMR of Korea has been steadily decreased from 20 per 100,000 live births in 1995 to 8.4 in 2008 which came down close to the average of Organization for Economic Cooperation and Development countries [11]. However, there was some increase in following years up to 17.2 of MMR in 2012 and remained in range of 10–11 in the recent 4 years [1,12]. Therefore, any kind of efforts in medical or social aspect to further decrease maternal mortality is continuously needed.
We consider that identifying indication and characteristics of obstetric patients admitted to the ICU can be a vital mean to decrease MMR. Here, we investigated all pregnant or puerperal women admitted to the ICU of a tertiary care center over 22-year period and compared the clinical characteristics based on time period and place of delivery. We also tried to evaluate clinical utility of acute physiology and chronic health evaluation (APACHE) score, which has been frequently used to assess ICU patients [13], in relation to maternal mortality in obstetric patients admitted to the ICU. These data will provide a better understanding of clinical profile of this unique ICU population and help us to determine the utility of the ICU admission criterion as an indicator of severe maternal morbidity.
Materials and methods
A retrospective observational study was conducted on pregnant or puerperal patients admitted to the ICU in our institution, a tertiary referral hospital located in Seoul, Korea. The subject population included patients who were pregnant at any gestational age or postpartum within 6 weeks, admitted to the ICU of our institution after delivery either in our institution or in local hospitals. The study period was about 22 years from September 1994 to October 2015. The study population was divided into 2 groups each by two criteria; by time period (period 1: 1994–2004; period 2: 2005–2015) and by place of delivery (our institution and local hospitals). Time period was divided arbitrarily into 11 equal years.
All data were collected by reviewing of individual medical records. Research data included patient demographics, parity, gestational age at delivery, number of fetus, mode of delivery, place of delivery, APACHE II score at ICU admission, time taken from delivery to ICU admission, duration of hospital stay, duration stay at ICU, primary cause of ICU admission, hysterectomy, embolization, and mortality. The APACHE II score is calculated by adding points of acute physiology score (body temperature, mean arterial pressure, heart rate, respiratory rate, oxygenation, arterial pH, serum sodium, serum potassium, serum creatinine, hematocrit, white blood cell count, and Glasgow Coma Score), age score and chronic health score. The total number of points ranges from 0 to 70; increasing points correlate with subsequent risk of mortality [13]. APACHE II score of study population was retrieved from the ICU records. The primary cause of ICU admission was grouped either obstetric or non-obstetric. Obstetric causes included postpartum hemorrhage, hypertensive disorders, sepsis and embolism, and non-obstetric causes were sorted by organ system as sorted in previous studies [14,15,16,17]. World Health Organization criteria was used to classify direct and indirect maternal death [18]. Clinical characteristics and indication of ICU admission were compared by time period and place of delivery.
Statistical analysis was done by SPSS statistics version 18.0 (IBM Corp., Chicago, IL, USA). P-values were calculated using the χ2 test, Fisher's exact test, t-test, and Mann-Whitney U test according to the type of data to compare clinical characteristics between 2 groups. Spearman correlation analysis was performed to find out the relation between the time taken from delivery to ICU admission and APACHE II score. Differences were considered statistically significant if P<0.05. Receiver operating characteristic (ROC) curve was generated and cut-off value was determined to evaluate the usefulness of APACHE II score to predict mortality for obstetric patients admitted to the ICU. This study was approved by Institutional Review Board of Samsung Medical Center as a retrospective study using medical records (2017-03-125).
Results
Among 176 women who admitted to the ICU during the study period, 118 (67.0%) women delivered in our institution and 58 (33.0%) women delivered in local hospitals. The total delivery of 53,689 took place in our institution during the study period, and the incidence of ICU admission among parturients was estimated as 2.2 per 1,000 deliveries. The most common obstetric reason for admitting to the ICU was postpartum hemorrhage (56.3%), followed by hypertensive disorders (19.3%), sepsis (3.4%), and pulmonary and amniotic fluid embolism (2.3%). Non-obstetric causes (18.8%) consisted of acute fatty liver, postpartum cardiomyopathy, pulmonary hypertension, pulmonary edema, pneumonia, and renal failure. The most common non-obstetric cause of ICU admission for obstetric patient was respiratory failure including pulmonary edema and pneumonia. The primary cause of ICU admission for obstetric patients showed no difference between time periods (Table 1) but, of note, embolism showed increasing trend in period 2 (P=0.069).
Table 1. Primary cause of intensive care unit admission of obstetric patients: comparison by period.
| Primary diagnosis | Total (1994–2015) (n=176) | Period 1 (1994–2004) (n=85) | Period 2 (2005–2015) (n=91) | P-value | ||
|---|---|---|---|---|---|---|
| Obstetric | 143 (81.2) | 69 (81.2) | 74 (81.3) | 0.566 | ||
| Postpartum hemorrhage | 99 (56.3) | 48 (56.5) | 51 (56.0) | 0.538 | ||
| Uterine atony | 65 (36.9) | 26 (30.6) | 39 (42.9) | |||
| Laceration | 4 (2.3) | 1 (1.2) | 3 (3.3) | |||
| Placental (previa, accreta, abruption) | 20 (11.4) | 14 (16.5) | 6 (6.6) | |||
| Others | 1 (0.6) | 1 (1.2) | 0 (0.0) | |||
| Mixed (PPH+hypertensive disease) | 8(4.5) | 5 (5.9) | 3 (3.3) | |||
| Hypertensive disorders | 34 (19.3) | 19 (22.4) | 15 (16.5) | 0.213 | ||
| Preeclampsia | 19 (1.08) | 11 (12.9) | 8 (8.8) | |||
| Eclampsia | 7 (4.0) | 3 (3.5) | 4 (4.4) | |||
| HELLP | 8 (4.5) | 5 (5.9) | 3 (3.3) | |||
| Sepsis | 6 (3.4) | 2 (2.4) | 4 (4.4) | 0.374 | ||
| Septic abortion | 5 (2.8) | 2 (2.4) | 3 (3.3) | |||
| Puerperal sepsis | 1 (0.6) | 0 (0.0) | 1 (0.6) | |||
| Embolism | 4 (2.3) | 0 (0.0) | 4 (4.4) | 0.069 | ||
| Pulmonary thromboembolism | 2 (1.2) | 0 (0.0) | 2 (2.2) | |||
| Amniotic fluid embolism | 2 (1.2) | 0 (0.0) | 2 (2.2) | |||
| Non-obstetric | 33 (18.8) | 16 (18.8) | 17 (18.7) | 0.566 | ||
| Gastrointestinal, hepatobiliary | 6 (3.4) | 5 (5.9) | 1 (1.1) | |||
| Cardiovascular | 10 (5.7) | 4 (4.7) | 6 (6.6) | |||
| Pulmonary | 14 (8.0) | 5 (5.9) | 9 (9.9) | |||
| Renal | 1 (0.6) | 0 (0.0) | 1 (1.1) | |||
| Others | 2 (1.2) | 2 (2.4) | 0 (0.0) | |||
Value expressed as number (percentage).
PPH, postpartum hemorrhage; HELLP, hemolysis, elevated liver enzymes, and low platelets.
Table 2 summarizes the baseline characteristics of the study population and comparison by the study period. Among the total study population, mean maternal age was 31.8 years, median stay at ICU was 3 (1–25) days and median hospital stay was 11 (1–63) days. Median APACHE II score was 10 (0–32) at ICU admission. Hysterectomy was performed in 70 patients (39.8%), and uterine artery embolization was performed in 25 patients (14.2%) of study population. Of note, higher mean maternal age (32.7 vs. 30.8 years; P=0.006), higher embolization rate (26.4% vs. 1.2%; P<0.001), and lower hysterectomy rate (30.8% vs. 49.4%; P=0.012) were observed in period 2. However, other variables including parity, gestational age at delivery, number of fetus, mode of delivery and place of delivery showed no significant difference between 2-time periods. There was also no significant difference in maternal death rate and APACHE II score at ICU admission between 2-time periods (Table 2).
Table 2. Baseline characteristics of 176 obstetric patients admitted to the intensive care unit (ICU): comparison by period.
| Variable | Total (1994–2015) (n=176) | Period 1 (1994–2004) (n=85) | Period 2 (2005–2015) (n=91) | P-value | |
|---|---|---|---|---|---|
| Age (yr) | 31.8±4.7 | 30.8±4.4 | 32.7±4.8 | 0.006 | |
| ≥35 years of age | 44 (25.0) | 12 (14.1) | 32 (35.2) | 0.001 | |
| Nulliparity | 101 (57.4) | 54 (63.5) | 47 (51.6) | 0.273 | |
| GA at delivery (wk) | 36.1 (10.0–41.3) | 35.3 (10.0–40.0) | 36.6 (11.1–41.3) | 0.404 | |
| Singleton pregnancy | 154 (87.5) | 76 (89.4) | 78 (86.7) | 0.576 | |
| Mode of delivery | 0.993 | ||||
| Vaginal delivery | 39 (22.2) | 19 (22.4) | 20 (22.0) | ||
| Cesarean section | 129 (73.3) | 62 (72.9) | 67 (73.6) | ||
| Abortion | 8 (4.5) | 4 (4.7) | 4 (4.4) | ||
| Place of delivery | 0.198 | ||||
| Our institution | 118 (67.0) | 61 (71.8) | 57 (62.6) | ||
| Local hospitals | 58 (33.0) | 24 (28.3) | 34 (37.4) | ||
| APACHE II score | |||||
| All patients | 10 (0–32) | 8 (1–25) | 10 (0–32) | 0.110 | |
| Postpartum hemorrhage | 7 (0–30) | 5 (1–25) | 10 (0–30) | 0.011 | |
| APACHE II score ≥18* | |||||
| All patients | 25 (15.0) | 8 (10.3) | 17 (19.1) | 0.110 | |
| Postpartum hemorrhage | 11 (12.5) | 3 (7.7) | 8 (16.3) | 0.224 | |
| Hospital stay (day) | 11 (1–63) | 11 (4–63) | 10 (1–62) | 0.161 | |
| ICU stay (day) | 3 (1–25) | 3 (2–25) | 3 (1–23) | 0.753 | |
| Hysterectomy | 70 (39.8) | 42 (49.4) | 28 (30.8) | 0.012 | |
| Embolization | 25 (14.2) | 1 (1.2) | 24 (26.4) | <0.001 | |
| Mortality | 9 (5.1) | 2 (2.4) | 7 (7.7) | 0.102 | |
Value expressed as mean±standard deviation, median (range), or number (percentage).
GA, gestational age, APACHE, acute physiology and chronic health evaluation.
*Cut-off value of 18 points of APACHE score was calculated from the following receiver-operator characteristic curve analysis in Fig. 1A.
The primary cause of obstetric ICU admission had significant difference between groups sorted by place of delivery (Table 3). Although postpartum hemorrhage was the most common cause of ICU admission regardless of place of delivery, patients who delivered in local hospitals showed significantly higher proportion of postpartum hemorrhage compared to patients who delivered in our institution (84.5% vs. 42.2%; P<0.001). Meanwhile, patients who delivered in our institution was associated with higher proportion of hypertensive disorders (28.8% vs. 0.0%; P<0.001) and non-obstetric causes (25.4% vs. 5.2%; P=0.001) compared to patients from local hospitals. There were 4 cases of pulmonary and amniotic fluid embolism during the study period, all of them delivered in local hospitals.
Table 3. Primary cause of intensive care unit admission of obstetric patients: comparison by place of delivery.
| Primary diagnosis | Total (n=176) | Our institution (n=118) | Local hospitals (n=58) | P-value | ||
|---|---|---|---|---|---|---|
| Obstetric | 143 (81.2) | 88 (74.6) | 55 (94.8) | 0.001 | ||
| Postpartum hemorrhage | 99 (56.3) | 50 (42.2) | 49 (84.5) | <0.001 | ||
| Uterine atony | 65 (36.9) | 27 (22.9) | 38 (65.5) | |||
| Laceration | 4 (2.3) | 1 (0.8) | 3 (5.2) | |||
| Placental (previa, accreta, abruption) | 20 (11.4) | 14 (11.9) | 6 (10.3) | |||
| Others | 1 (0.6) | 0 (0.0) | 1 (1.7) | |||
| Mixed (PPH+hypertensive disease) | 8 (4.5) | 7 (5.9) | 1 (1.7) | |||
| Hypertensive disorders | 34 (19.3) | 34 (28.8) | 0 (0.0) | <0.001 | ||
| Preeclampsia | 19 (1.08) | 19 (16.1) | 0 (0.0) | |||
| Eclampsia | 7 (4.0) | 7 (5.9) | 0 (0.0) | |||
| HELLP | 8 (4.5) | 8 (6.8) | 0 (0.0) | |||
| Sepsis | 6 (3.4) | 4 (3.4) | 2 (3.4) | 0.645 | ||
| Septic abortion | 5 (2.8) | 3 (2.5) | 2 (3.4) | |||
| Puerperal sepsis | 1 (0.6) | 1 (0.8) | 0 (0.0) | |||
| Embolism | 4 (2.3) | 0 (0.0) | 4 (6.9) | 0.011 | ||
| Pulmonary thromboembolism | 2 (1.2) | 0 (0.0) | 2 (3.5) | |||
| Amniotic fluid embolism | 2 (1.2) | 0 (0.0) | 2 (3.5) | |||
| Non-obstetric | 33 (18.8) | 30 (25.4) | 3 (5.2) | 0.001 | ||
| Gastrointestinal, hepatobiliary | 6 (3.4) | 4 (3.4) | 2 (3.4) | |||
| Cardiovascular | 10 (5.7) | 9 (7.6) | 1 (1.7) | |||
| Pulmonary | 14 (8.0) | 14 (11.9) | 0 (0.0) | |||
| Renal | 1 (0.6) | 1 (0.8) | 0 (0.0) | |||
| Others | 2 (1.1) | 2 (2.4) | 0 (0.0) | |||
Value expressed as number (percentage).
PPH, postpartum hemorrhage; HELLP, hemolysis, elevated liver enzymes, and low platelet.
Table 4 summarizes the baseline characteristics of the study population and comparison by the place of delivery. Patients who delivered in our institution showed higher rate of nulliparity (71.2% vs. 29.3%; P<0.001). There was a significant difference in mode of delivery, indicating higher proportion of cesarean section in patients who delivered in our institution. The median gestational age at delivery of patients delivered in our institution was significantly earlier compared to the gestational age of patients who delivered in local hospitals. APACHE II score at ICU admission, and ICU admission showed no difference by place of delivery. However, proportion of patients whose APACHE II score was more than or equal to 18 points tended to be higher in patients who delivered in local hospitals compared to patients who delivered in our institution. (11.5% vs. 22.2%; P=0.069) Especially in subgroup analysis with postpartum hemorrhage group, proportion of patients whose APACHE II score was more than or equal to 18 points, was significantly higher in patients who delivered in local hospitals compared to patients who delivered in our institution (4.7% vs. 20.0%; P=0.030). As shown in Table 4, both hysterectomy and embolization rate were higher in patients who delivered in local hospitals compared to those delivered in our institution. Maternal death rate showed no significant differences by place of delivery.
Table 4. Baseline characteristics of 176 obstetric patients admitted to the intensive care unit (ICU): comparison by place of delivery.
| Variable | Total (n=176) | Our institution (n=118) | Local hospitals (n=58) | P-value | |
|---|---|---|---|---|---|
| Age (yr) | 31.8±4.7 | 31.7±4.7 | 31.9±4.7 | 0.796 | |
| ≥35 years of age | 44 (25.0) | 31 (26.3) | 13 (22.4) | 0.359 | |
| Nulliparity | 101 (57.4) | 84 (71.2) | 17 (29.3) | <0.001 | |
| GA at delivery (wk) | 36.1 (10.0–41.3) | 34.1 (10.0–41.2) | 39.0 (16.0–41.3) | <0.001 | |
| Singleton pregnancy | 154 (87.5) | 98 (83.1) | 56 (96.6) | 0.003 | |
| Mode of delivery | 0.001 | ||||
| Vaginal delivery | 39 (22.2) | 17 (14.4) | 22 (37.9) | ||
| Cesarean section | 129 (73.3) | 97 (82.2) | 32 (55.2) | ||
| Abortion | 8 (4.5) | 4 (3.4) | 4 (6.9) | ||
| Period | 0.130 | ||||
| Period 1 (1994–2004) | 85 (48.3) | 61 (51.7) | 24 (41.4) | ||
| Period 2 (2005–2015) | 91 (51.7) | 57 (48.3) | 34 (58.6) | ||
| APACHE II score | |||||
| All patients | 10 (0–32) | 10 (0–29) | 8.5 (0–32) | 0.846 | |
| Postpartum hemorrhage | 7 (0–30) | 8 (1–29) | 7 (0–30) | 0.851 | |
| APACHE II score ≥18* | |||||
| All patients | 25 (15.0) | 13 (11.5) | 12 (22.2) | 0.069 | |
| Postpartum hemorrhage | 11 (12.5) | 2 (4.7) | 9 (20.0) | 0.030 | |
| Hospital stay (day) | 11 (1–63) | 11 (4–63) | 9.5 (1–35) | 0.008 | |
| ICU stay (day) | 3 (1–25) | 3 (2–25) | 3 (1–13) | 0.344 | |
| Hysterectomy | 70 (39.8) | 34 (28.8) | 36 (62.1) | <0.001 | |
| Embolization | 25 (14.2) | 12 (10.2) | 13 (22.4) | 0.027 | |
| Mortality | 9 (5.1) | 4 (3.4) | 5 (8.6) | 0.133 | |
Value expressed as mean±standard deviation, median (range), or number (percentage).
GA, gestational age; APACHE, acute physiology and chronic health evaluation.
*Cut-off value of 18 points of APACHE score was calculated from the following receiver-operator characteristic curve analysis in Fig. 1A.
Next, we performed ROC curve analysis of APACHE II to determine the cutoff value to predict maternal mortality in ICU-admitted women. Overall, the APACHE II score showed area under the ROC curve (AUC) of 0.813 (confidence interval [CI], 0.607–1.000) for prediction of maternal mortality (Fig. 1A). And the cut-off value of APACHE II score more than or equal to 18 points showed 77.8% of sensitivity, 88.6% of specificity, 28.0% of positive predictive value (PPV), and 98.6% of negative predictive value (NPV), respectively. Since postpartum hemorrhage was the most common reason for ICU admission of obstetric patients, we did subgroup analysis to assess predictive value of APACHE II score in this population. As shown in Fig. 1B, AUC for prediction of mortality among patients admitted to the ICU due to postpartum hemorrhage was 0.963 (CI, 0.000–1.000). And with the cut-off value of 20 of the APACHE II score, sensitivity, specificity, PPV, and NPV to predict maternal mortality was 100%, 90.6%, 33.3%, and 100%, respectively.
Fig. 1.
Receiver-operator characteristic curve analysis of acute physiology and chronic health evaluation (APACHE) II score to predict mortality in obstetric patients admitted to the intensive care unit. (A) All obstetric patients. The round circle indicates (B) patients with postpartum hemorrhage.
AUC, area under the receiver operating characteristic curve.
The median time taken from delivery to ICU admission was 4.83 (0.37–48) hours among study population except 8 patients for whom that time took more than 48 hours. The reasons for delayed ICU admission were delayed postpartum hemorrhage, delayed complication of preeclampsia such as intracranial hemorrhage or hypertensive encephalopathy, progression of postoperative sepsis or septic abortion and postpartum pulmonary edema. The correlation between the time taken from delivery to ICU admission and APACHE II score was not statistically significant (correlation coefficient=−0.075, P=0.356) among the total study population, but it showed negative correlation in subgroup analysis with postpartum hemorrhage group (correlation coefficient=−0.226, P=0.038).
Overall, maternal death occurred 5.1% among ICU-admitted patients, which included 6 cases of direct maternal death and 3 cases of indirect maternal death. There was one case of direct maternal death occurred in case of patient delivered in our institution. Detailed clinical information including primary cause of ICU admission, underlying diseases, and intervention are summarized in Table 5. There were 3 cases of disseminated intravascular coagulation due to postpartum hemorrhage, 2 cases of amniotic fluid embolism, 1 case of hemolysis, elevated liver enzymes, and low platelets syndrome with intracranial hemorrhage, 1 case of pulmonary thromboembolism, 1 case of postpartum cardiomyopathy, and 1 case of post-adrenalectomy bleeding due to pheochromocytoma.
Table 5. Detailed clinical information of mortality cases.
| No. | Date of admission (yr, mon) | Age (yr) | GA at delivery (wk) | Mode of delivery | Place of delivery | Classification of maternal death | Primary cause of ICU admission | Underlying disease | Interventions | Postpartum time of death (day) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2000.10. | 29 | 20.0 | Abortion | Local hospital | Direct | Postpartum hemorrhage, pulmonary edema | Hysterectomy, mechanical ventilation | 6 | |
| 2 | 2004.06. | 28 | 39.1 | Cesarean section | Our institution | Indirect | Non-obstetric (others)a) | Pheochromocytoma | Mechanical ventilation | 2 |
| 3 | 2007.03. | 30 | 40.5 | Vaginal delivery | Local hospital | Direct | Postpartum hemorrhage, DIC | Hysterectomy, mechanical ventilation | 7 | |
| 4 | 2008.11. | 31 | 40.6 | Vaginal delivery | Local hospital | Direct | Amniotic fluid embolism, DIC | Mechanical ventilation | 1 | |
| 5 | 2011.06. | 30 | 39.5 | Cesarean section | Our institution | Direct | Preeclampsia, HELLP, intracranial hemorrhage | Craniectomy, coma therapy | 10 | |
| 6 | 2011.07. | 37 | N/A | Cesarean section | Local hospital | Direct | Postpartum hemorrhage, DIC | Hysterectomy, ECMO | 1 | |
| 7 | 2012.08. | 20 | 23.6 | Vaginal delivery | Our institution | Indirect | Postpartum aggravation of dilated cardiomyopathy | Dilated cardiomyopathy | Not done | 79 |
| 8 | 2013.07. | 38 | 32.4 | Cesarean section | Our institution | Indirect | Pulmonary thromboembolism, infective endocarditis | Ovarian cancer, deep vein thrombosis | Not done | 28 |
| 9 | 2015.09. | 35 | 36.6 | Vaginal delivery | Local hospital | Direct | Amniotic fluid embolism, DIC | Hysterectomy, ECMO | 1 |
GA, gestational age; ICU, intensive care unit; DIC, disseminated intravascular coagulation; N/A, not available; ECMO, extra-corporeal membrane oxygenation; HELLP, hemolysis, elevated liver enzymes, and low platelets.
a)Post-adrenalectomy bleeding due to pheochromocytoma.
Discussion
Pregnancy causes physiological and anatomical changes and those changes proceed uneventfully in most of pregnant women. However, these changes play important roles in maternal morbidity and mortality even in women with no prior risk factor, and who may require further intensive care. This suggests that the risk of serious maternal morbidity and mortality is applicable to all pregnancies, and not only limited to those with high-risk pregnancy [19].
Our study showed that obstetric admission rate to the ICU represented 0.22%, equating to 1 ICU admission for every 455 deliveries. The figure is comparable with previous published studies, where the frequencies ranged from 0.17% to 0.73% [20,21,22,23,24,25,26] similar to the median incidence of ICU admission of studies reporting 0.27% of obstetric ICU admission rate in systematic review [6].
In our study, the most common cause of admission to the ICU of pregnant or puerperal women was postpartum hemorrhage which accounted for 56.3% of all admissions, followed by hypertensive disorders of 19.3%. This result is different from previous studies performed in western countries, in which hypertensive disorder showed the highest rate as 62.0%, 59.0%, 67.9%, or 54.2% for the cause of ICU admission [14,15,17,27]. The relatively high incidence of postpartum hemorrhage in our study may be due to referral bias, because our hospital acts as a tertiary referral center with diverse quality of antenatal care. This interpretation is supported by the fact that percentage of postpartum hemorrhage was significantly higher among patients transferred from local hospitals compared to patients delivered in our institution (84.5% vs. 42.2%). In the other hand, relatively low percentage of hypertensive disorders among primary cause of obstetric ICU admission in our study could be due to the racial difference in the incidence of hypertensive disorder. In fact, it was known that East Asian women showed relatively low incidence of preeclampsia compared to African American or Hispanic women in previous studies [28,29].
Recently, increased maternal age at childbearing period is observed in most countries [30]. A Korean study demonstrated that mean maternal age at delivery has increased from 29.49 to 31.63 years in 2002 to 2012 and the proportion of pregnant women with maternal age over 35 years has also increased from 6.7% to 18.7% in 2000 to 2012 [31]. Recent statistics in 2015 which renewed the record shows that mean maternal age was 32.2 years old and the proportion of women with maternal age over 35 was about 24% in Korea [32]. High maternal age in period 2 of our data can be understood in the same direction with the recent national survey. The prevalence of high-risk pregnancy is increasing continuously with increase in maternal age [1]. According to the data from Health Insurance Review and Assessment Service, high-risk pregnancy accounted for only 7% in maternal age of 25–30 years, but increased to 24% in maternal of 35–40 years and 40% in maternal age over 40 years [1,33]. Lee et al. [12] also reported that old maternal age group had shown higher MMR compared to younger maternal age group consistently from 1995 to 2010 in Korea, as MMR in 2010 was 14.7 in total population but as high as 28.2 in maternal age of 35–39 years and 86.1 in maternal age over 40 years.
APACHE II score is the most frequently used scoring system to assess disease severity in ICU-admitted patients based on physiologic measurements, age and chronic health condition [13]. APACHE II scoring system showed high accuracy in prediction of the ICU outcome for critically ill obstetric patients in previous study [34]. In our study, ROC curve analysis of APACHE II score showed high predictability of maternal death. APACHE II score more than or equal to 18 points showed with high sensitivity (77.8%) and specificity (88.6%) in prediction of maternal death. This cut-off value would be clinically useful to predict the mortality risk of critically ill obstetric patients especially with high NPV (98.6%). In patients admitted to the ICU due to postpartum hemorrhage, predictability of maternal death with APACHE II score was even higher than in all study population, so it would help to counsel patients and their family about the risk of mortality especially in case of postpartum hemorrhage.
Our data showed that hysterectomy rate has decreased and uterine artery embolization rate has increased in period 2 compared to period 1. This is supported by the fact that uterine artery embolization is considered as a proper management with reasonable success rate, minimal safety complications and shorter hospital staying in previous studies [35,36,37]. Success rate of uterine artery embolization was reported as 89% in retrospective studies with 53 patients in 1999–2007 and 88% in 117 patients in 2006–2013, respectively [35,36].
Our observed mortality rate of 5.1% for maternal ICU admission is closer to the median of 3.4% (ranged 0%–18.4%) in developed countries and much lower than the median of 14.0% (ranged 0%–40%) in developing countries [6]. In our study, postpartum bleeding is the most common cause of maternal ICU admission (56.3%, 99 cases) and accounted for 3 out of 9 mortality cases. In contrast, while pulmonary or amniotic embolism consist only a small proportion of total ICU-admitted patients (2.3%, 4 cases), they also accounted for 3 out of 9 mortality cases. This finding obviously reflects notoriously poor outcome of obstetric embolism, pulmonary and amniotic fluid embolism as previously indicated [38,39,40]. Our observation is in line with a Korean study which already showed that obstetric embolism accounted for 24.4% (88 cases) and postpartum hemorrhage accounted for 18.3% (66 cases) among 239 direct maternal deaths occurred from 2009 to 2014 [11,12].
It is noteworthy that all cases of pulmonary and amniotic fluid embolism among ICU-admitted patients were occurred in period 2, although statistical analysis failed to reach significant difference between time period groups in current study (P=0.069). However, considering the significant increase in maternal age in this period 2, it is probably due to beta error. Therefore, pulmonary and amniotic fluid embolism could be expected to increase continuously due to increase in maternal age and high-risk pregnancy. The most frequent organ dysfunction associated with non-obstetric cause of ICU admission among parturients was respiratory failure, potentially as a common outcome for critically ill patients who have suffered from cardiovascular collapse or aggressive fluid resuscitation. This information can then provide support for targeted systems-based improvements at an institutional, local, and further nationwide level [41].
Our study is limited by a possibility of biased population since our study included patients from only a single tertiary referral center located in Seoul. Therefore, comparison and extrapolation should be carried out with caution. And ideally, multicenter study or national data about ICU-admitted patients among parturients should be carried out as a future study.
Our study does have a point, however. This is the very first study conducted in Korea that analyzed ICU admissions of pregnant or puerperal women in a tertiary care center. Our data shows different trends for the causes of obstetric ICU admission with postpartum hemorrhage as the most common cause, whereas previous studies performed in Western countries showed relatively higher proportion of hypertensive disorders. Therefore, our result provides insights into severe maternal morbidity that requires intensive care, at least limited within but can be expanded beyond Korea. Considering that postpartum hemorrhage was the leading cause of ICU admission of parturients regardless of place of delivery, we argue that every tertiary hospital need to develop a predetermined flow with multidisciplinary team approach involving obstetricians, anesthesiologists, critical care division and nursing to provide organized management for these patients, especially coping with massive postpartum hemorrhage.
In summary, our study provided important information about ICU admission of obstetric patients over 22 years of study period in a single tertiary hospital in Korea. We hope that our data would primarily help counsel patients about complications and prognosis of high-risk pregnancy. Furthermore, it can provide support to establish a medical care system on maternal morbidity and mortality either hospital-based or nation-based. A large, prospective, nationwide multicenter study would further assist us to have a better understanding of ICU admissions of obstetric patients.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
This work was presented at 102th Annual Congress of Korean Society of Obstetrics and Gynecology as oral presentation in Seoul, September 24th, 2016.
References
- 1.Kim HY, Moon CS. Integrated care center for high risk pregnancy and neonate: an analysis of process and problems in obstetrics. Korean J Perinatol. 2014;25:140–152. [Google Scholar]
- 2.Seo K, Park MI, Kim SY, Park JS, Han YJ. Changes of maternal mortality ratio and the causes of death in Korea during 1995–2000. Korean J Obstet Gynecol. 2004;47:2345–2350. [Google Scholar]
- 3.Collop NA, Sahn SA. Critical illness in pregnancy. An analysis of 20 patients admitted to a medical intensive care unit. Chest. 1993;103:1548–1552. doi: 10.1378/chest.103.5.1548. [DOI] [PubMed] [Google Scholar]
- 4.Bouvier-Colle MH, Varnoux N, Salanave B, Ancel PY, Bréart G. Case-control study of risk factors for obstetric patients’ admission to intensive care units. Eur J Obstet Gynecol Reprod Biol. 1997;74:173–177. doi: 10.1016/s0301-2115(97)00116-4. [DOI] [PubMed] [Google Scholar]
- 5.Gilbert TT, Smulian JC, Martin AA, Ananth CV, Scorza W, Scardella AT, et al. Obstetric admissions to the intensive care unit: outcomes and severity of illness. Obstet Gynecol. 2003;102:897–903. doi: 10.1016/s0029-7844(03)00767-1. [DOI] [PubMed] [Google Scholar]
- 6.Pollock W, Rose L, Dennis CL. Pregnant and postpartum admissions to the intensive care unit: a systematic review. Intensive Care Med. 2010;36:1465–1474. doi: 10.1007/s00134-010-1951-0. [DOI] [PubMed] [Google Scholar]
- 7.Karnad DR, Guntupalli KK. Critical illness and pregnancy: review of a global problem. Crit Care Clin. 2004;20:555–576. vii. doi: 10.1016/j.ccc.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Gatt S. Pregnancy, delivery and the intensive care unit: need, outcome and management. Curr Opin Anaesthesiol. 2003;16:263–267. doi: 10.1097/00001503-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Soubra SH, Guntupalli KK. Critical illness in pregnancy: an overview. Crit Care Med. 2005;33:S248–S255. doi: 10.1097/01.ccm.0000183159.31378.6a. [DOI] [PubMed] [Google Scholar]
- 10.Munnur U, Karnad DR, Bandi VD, Lapsia V, Suresh MS, Ramshesh P, et al. Critically ill obstetric patients in an American and an Indian public hospital: comparison of case-mix, organ dysfunction, intensive care requirements, and outcomes. Intensive Care Med. 2005;31:1087–1094. doi: 10.1007/s00134-005-2710-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park HS, Kwon H. Analysis of the causes and trends of maternal mortality in Korea: 2009–2014. Korean J Perinatol. 2016;27:110–117. [Google Scholar]
- 12.Lee YJ, Kim SH, Seol HJ, Chung SH, Choi YS, Lee KS, et al. Changes in statistics of maternal death in Korea (1995–2010) Korean J Perinatol. 2012;23:179–187. [Google Scholar]
- 13.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 14.Rios FG, Risso-Vázquez A, Alvarez J, Vinzio M, Falbo P, Rondinelli N, et al. Clinical characteristics and outcomes of obstetric patients admitted to the intensive care unit. Int J Gynaecol Obstet. 2012;119:136–140. doi: 10.1016/j.ijgo.2012.05.039. [DOI] [PubMed] [Google Scholar]
- 15.Togal T, Yucel N, Gedik E, Gulhas N, Toprak HI, Ersoy MO. Obstetric admissions to the intensive care unit in a tertiary referral hospital. J Crit Care. 2010;25:628–633. doi: 10.1016/j.jcrc.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 16.Vasquez DN, Estenssoro E, Canales HS, Reina R, Saenz MG, Das Neves AV, et al. Clinical characteristics and outcomes of obstetric patients requiring ICU admission. Chest. 2007;131:718–724. doi: 10.1378/chest.06-2388. [DOI] [PubMed] [Google Scholar]
- 17.Keizer JL, Zwart JJ, Meerman RH, Harinck BI, Feuth HD, van Roosmalen J. Obstetric intensive care admissions: a 12-year review in a tertiary care centre. Eur J Obstet Gynecol Reprod Biol. 2006;128:152–156. doi: 10.1016/j.ejogrb.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. The WHO application of ICD-10 to deaths during pregnancy, childbirth and the puerperium: IDC MM. Geneva: World Health Organization; 2012. [Google Scholar]
- 19.Lataifeh I, Amarin Z, Zayed F, Al-Mehaisen L, Alchalabi H, Khader Y. Indications and outcome for obstetric patients’ admission to intensive care unit: a 7-year review. J Obstet Gynaecol. 2010;30:378–382. doi: 10.3109/01443611003646298. [DOI] [PubMed] [Google Scholar]
- 20.Hazelgrove JF, Price C, Pappachan VJ, Smith GB. Multicenter study of obstetric admissions to 14 intensive care units in southern England. Crit Care Med. 2001;29:770–775. doi: 10.1097/00003246-200104000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Mahutte NG, Murphy-Kaulbeck L, Le Q, Solomon J, Benjamin A, Boyd ME. Obstetric admissions to the intensive care unit. Obstet Gynecol. 1999;94:263–266. doi: 10.1016/s0029-7844(99)00274-4. [DOI] [PubMed] [Google Scholar]
- 22.Loverro G, Pansini V, Greco P, Vimercati A, Parisi AM, Selvaggi L. Indications and outcome for intensive care unit admission during puerperium. Arch Gynecol Obstet. 2001;265:195–198. doi: 10.1007/s004040000160. [DOI] [PubMed] [Google Scholar]
- 23.Quah TC, Chiu JW, Tan KH, Yeo SW, Tan HM. Obstetric admissions to the intensive therapy unit of a tertiary care institution. Ann Acad Med Singapore. 2001;30:250–253. [PubMed] [Google Scholar]
- 24.Panchal S, Arria AM, Harris AP. Intensive care utilization during hospital admission for delivery: prevalence, risk factors, and outcomes in a statewide population. Anesthesiology. 2000;92:1537–1544. doi: 10.1097/00000542-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Kilpatrick SJ, Matthay MA. Obstetric patients requiring critical care. A five-year review. Chest. 1992;101:1407–1412. doi: 10.1378/chest.101.5.1407. [DOI] [PubMed] [Google Scholar]
- 26.Mirghani HM, Hamed M, Ezimokhai M, Weerasinghe DS. Pregnancy-related admissions to the intensive care unit. Int J Obstet Anesth. 2004;13:82–85. doi: 10.1016/j.ijoa.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 27.Bandeira AR, Rezende CA, Reis ZS, Barbosa AR, Peret FJ, Cabral AC. Epidemiologic profile, survival, and maternal prognosis factors among women at an obstetric intensive care unit. Int J Gynaecol Obstet. 2014;124:63–66. doi: 10.1016/j.ijgo.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 28.Gong J, Savitz DA, Stein CR, Engel SM. Maternal ethnicity and pre-eclampsia in New York City, 1995–2003. Paediatr Perinat Epidemiol. 2012;26:45–52. doi: 10.1111/j.1365-3016.2011.01222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tanaka M, Jaamaa G, Kaiser M, Hills E, Soim A, Zhu M, et al. Racial disparity in hypertensive disorders of pregnancy in New York State: a 10-year longitudinal population-based study. Am J Public Health. 2007;97:163–170. doi: 10.2105/AJPH.2005.068577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Organisation for Economic Co-operation and Development. OECD family database. Paris: Organisation for Economic Co-operation and Development; 2016. [Google Scholar]
- 31.Statistics Korea. Census statics survey: current state according maternal aging. Daejeon: Statistics Korea; 2012. [Google Scholar]
- 32.Statistics Korea. Census statics survey. Daejeon: Statistics Korea; 2015. [Google Scholar]
- 33.Health Insurance Review and Assessment Service (KO) National health medical survey. Seoul: Health Insurance Review and Assessment Service; 2012. [Google Scholar]
- 34.El-Solh AA, Grant BJ. A comparison of severity of illness scoring systems for critically ill obstetric patients. Chest. 1996;110:1299–1304. doi: 10.1378/chest.110.5.1299. [DOI] [PubMed] [Google Scholar]
- 35.Yoon JY, Ryoo UN, Noh SK, Song SE, Seo ES, Lee SH, et al. Emergent hysterectomy and angiographic embolization for the management of obstetrical hemorrhage: 8-year experiences. Korean J Obstet Gynecol. 2009;52:180–187. [Google Scholar]
- 36.Cheong JY, Kong TW, Son JH, Won JH, Yang JI, Kim HS. Outcome of pelvic arterial embolization for postpartum hemorrhage: a retrospective review of 117 cases. Obstet Gynecol Sci. 2014;57:17–27. doi: 10.5468/ogs.2014.57.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Byun JM, Kim YN, Jeong DH, Seo YJ, Jeong EJ, Kang JY, et al. Prognosis and indication of emergency hysterectomy following postpartum hemorrhage. Korean J Obstet Gynecol. 2012;55:901–906. [Google Scholar]
- 38.Gist RS, Stafford IP, Leibowitz AB, Beilin Y. Amniotic fluid embolism. Anesth Analg. 2009;108:1599–1602. doi: 10.1213/ane.0b013e31819e43a4. [DOI] [PubMed] [Google Scholar]
- 39.Fitzpatrick KE, Tuffnell D, Kurinczuk JJ, Knight M. Incidence, risk factors, management and outcomes of amniotic-fluid embolism: a population-based cohort and nested case-control study. BJOG. 2016;123:100–109. doi: 10.1111/1471-0528.13300. [DOI] [PubMed] [Google Scholar]
- 40.Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123:337–348. doi: 10.1097/AOG.0000000000000107. [DOI] [PubMed] [Google Scholar]
- 41.Wanderer JP, Leffert LR, Mhyre JM, Kuklina EV, Callaghan WM, Bateman BT. Epidemiology of obstetric-related ICU admissions in Maryland: 1999–2008*. Crit Care Med. 2013;41:1844–1852. doi: 10.1097/CCM.0b013e31828a3e24. [DOI] [PMC free article] [PubMed] [Google Scholar]