Abstract
Objective
This study introduces and evaluates the feasibility, safety, and surgical outcomes of the in-bag power morcellation technique during single-port assisted (SPA) laparoscopic myomectomy in comparison with manual scalpel morcellation.
Methods
This is a retrospective review of a total of 58 patients who underwent SPA laparoscopic myomectomy employing in-bag power morcellation (n=27) or manual scalpel morcellation (n=31), performed between December 2014 and December 2016. Surgical outcomes, including total operation time, estimated blood loss, postoperative hemoglobin changes, postoperative hospital stay, postoperative pain (visual analog scale), perioperative and postoperative complications were evaluated.
Results
The demographics and patient characteristics were similar between both groups. The median patient age was 34 years and median body mass index was 20.84 kg/m2. The median specimen weight was 110 g. The median operating time was 138 minutes. The median estimated blood loss was 50 mL and the median postoperative hemoglobin change was 2.2 g/dL. The median postoperative hospital stay was 2 days and the median postoperative pain scores were 5 after 6 hours, 3 after 24 hours, and 2 after 48 hours. Occult malignancy was not identified in any patients. There were no intraoperative complications such as LapBag ruptures or gross spillage.
Conclusion
In-bag power morcellation for SPA laparoscopic myomectomy is feasible and safe, minimizing the risks of open power morcellation. There were also no statistically significant differences in surgical outcomes.
Keywords: Laparoscopy, Minimally invasive surgical procedures, Myomectomy, Morcellation
Introduction
Minimally invasive laparoscopic surgery continues to be the leading surgical method, offering a shorter recovery time, less postoperative pain, better cosmetic outcomes, and lower complication rates compared to open abdominal surgery [1,2,3]. Unfortunately, some difficulty remains in removing large-sized specimens via single-port assisted (SPA) laparoscopy. A considerable amount of time and effort must be invested for morcellation, which is the fragmentation of a tissue specimen to reduce it to a compact size, enabling extraction through smaller incisions [4].
The prototype for power morcellation was first introduced in 1993 by Rolf Steiner of Switzerland [5]. Electromechanical morcellation is an easy and efficient method for removing tissue from the abdominal cavity compared to hand-manipulated morcellation [6]. However, power morcellation related complications such as injury from morcellator blades to vessels or adjacent visceral organs is a concern [7].
This method also introduces the risk of unintentional dissemination of removed tissue, which could lead to benign myoma seeding or spillage of malignant material into the peritoneal cavity if that tissue is pathologically confirmed to be endometrial cancer or sarcoma [8,9]. A safety communication warning published by the U.S. Food and Drug Administration in April 2014 advised against the use of power morcellation due to the risk of intra-abdominal malignancy dissemination during laparoscopy [10].
The purpose of this study is to introduce and evaluate the feasibility, safety, and surgical outcomes of the in-bag power morcellation technique during SPA laparoscopic myomectomy in comparison with manual scalpel morcellation.
Materials and methods
This study is a retrospective review of a total of 58 patients who underwent SPA laparoscopic myomectomy employing in-bag power morcellation (n=27) or manual scalpel morcellation (n=31), performed between December 2014 and December 2016 at Severance Hospital, Yonsei University College of Medicine, in Seoul, Korea. All surgeries were performed by a single gynecologic surgeon specializing in minimally invasive gynecologic surgical techniques. We received written consent from all patients prior to surgery. Inclusion criteria for this study limited subjects to women undergoing laparoscopic surgical treatment for a benign disease of the uterus such as myoma, adenomyosis, and/or adenomyoma. Exclusion criteria included patients with known or suspected malignancies. Pathologic confirmation was done using tissue extracted during surgery. Patients were categorized into 2 groups according to whether they received specimen extraction using in-bag power morcellation or manual morcellation using a scalpel.
Demographic and physical characteristics such as age, coital history, parity, body mass index (BMI), previous surgical history, and surgical indication were investigated. Parity included both vaginal and cesarean section delivery. Preoperative evaluation included cervical cytology and imaging evaluation such as ultrasonography, magnetic resonance imaging, or abdominal and pelvic computed tomography scans. Myoma size and location were ascertained by imaging. Surgical outcomes such as estimated blood loss during surgery (mL), serum hemoglobin (Hb) differences (the change between pre-surgical Hb and postoperative day 1 Hb), total operation time (minutes), postoperative hospital stay (days), and the dry weight of the extracted specimen (g) were also investigated. Total operation time was calculated as the time from initial incision to final closure. Estimated blood loss during surgery was approximated as the total suctioned volume. Hospital discharge was determined according to whether patients were afebrile for 24 hours, could tolerate a soft diet, could ambulate without assistance, and were able to urinate independently after urinary catheter removal. Postoperative pain was appraised according to the visual analog scale. Patients were asked to rate postoperative pain 6, 24, and 48 hours following surgery.
1. Surgical techniques
All SPA laparoscopic surgeries were performed according to a technique previously described by our group [11]. The SPA system entails a single multichannel port at the umbilicus. In-bag power morcellation was performed by morcellating the removed uterine tissue inside an insufflated endoscopic bag within the abdominal cavity (Supplementary Video 1).
With this single-port surgery technique, an Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA) was inserted into the abdomen through a 2 cm trans-umbilical incision site. A 7½ left-handed surgical glove was affixed to the wound retractor. Incisions were made in the glove fingertips. A 12-mm trocar was inserted into the thumb, a 5-mm trocar into the pinky, and a 5-mm mini trocar into the middle finger. A 45-cm rigid, 30 degrees 5-mm endoscope was used. Instruments used during surgery included a monopolar L-hook, atraumatic graspers, scissors, biopsy forceps with a slightly-bent shaft, a suction-irrigation system, laparoscopic needle holders, and energy devices such as Enseal (Ethicon, Somerville, NJ, USA) and Thunderbeat (Olympus Medical Systems, Tokyo, Japan) [11].
Standard procedure was used for myomectomy. A monopolar hook was used to make a vertical incision in the prominent part of the myoma. Dissection of the cleavage plane between the myoma and surrounding tissue was then completed. Enucleation and removal were achieved by fixing and implementing traction on the myoma. Thunderbeat was used for dissection in several cases. The myomectomy site was repaired in 2 layers with an intracorporeal continuous suture and tie.
For in-bag power morcellation, a 30 cm2 laparoscopic specimen retrieval bag, XXL or 3XL LapBag (Sejong Medical Co., Seoul, Korea), was used to remove the myoma without spillage. After inserting the LapBag into the abdominal cavity, it was opened intra-abdominally and the myoma specimen was placed into the LapBag and pulled out midway through the wound retractor by drawing on the thread of the bag. The surgical glove was then detached from the Alexis wound retractor. The wound retractor and surgical glove were reattached together by folding 3 or 4 times with the LapBag inserted in between (Fig. 1, Supplementary Video 2). After completely attaching the LapBag to the wound retractor and surgical glove, CO2 gas was pumped into the bag. The 12-mm trocar was separated from the surgical glove, and the power morcellator (Chungang Medical Co., Seoul, Korea) was inserted into the thumb of the surgical glove. The entire myoma was morcellated while contained within the insufflated bag (Fig. 2, Supplementary Video 3). After morcellation was complete, the surgeon examined the bag for tears and inspected the pelvis for visible spillage of fluid or uterine tissue. In patients with small myomas that can be easily removed through the umbilical incision, manual morcellation technique was usually selected. But in patients with relatively large myomas (>5 cm), power morcellation was predominantly selected except when the power morcellator was not available.
Fig. 1.
Simulation of 3XL LapBag insufflated with CO2 gas attached to single-port wound retractor.
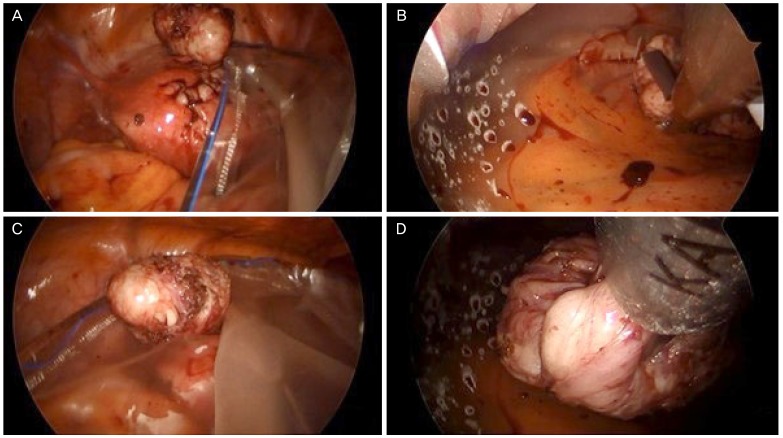
Fig. 2.
Intraoperative laparoscopic view of myoma power morcellation while contained within insufflated LapBag. (A) 3XL LapBag is opened intra-abdominally. (B) Myoma is inserted into the LapBag. (C) The myoma is grabbed with morcellator instrument. (D) The myoma is power morcellated within the insufflated LapBag.
2. Statistical analysis
The demographic and physical characteristics of all patients were obtained retrospectively. Surgical outcome results were obtained pre- and post-operatively. All statistical analyses were performed using SPSS ver. 23 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to summarize the results of the patients' characteristics and operation outcomes. All data was analyzed using the Student's t-test or Pearson's χ2 test and reported as a value of number (%) or a median (range).
Results
The in-bag morcellation technique for specimen extraction was successfully performed in all 27 cases. The demographic and physical characteristics of the patients are shown in Table 1. A known huge myoma (n=12, 44.4%) was the leading indicator for surgery. Other indications included hypermenorrhea (n=5, 18.5%), an increase in myoma size (n=5, 18.5%), and pelvic pain (n=5, 18.5%). Four (14.8%) and 9 (29.0%) women had received previous abdominal surgeries in the in-bag morcellation group and the manual scalpel morcellation group, respectively. The median patient age was 34 years (range, 26–54), and the median BMI was 20.84 kg/m2 (range, 18.26–28.89) for the in-bag morcellation group. For the manual morcellation group, the median patient age was 37 years (range, 26–59) and the median BMI was 21.93 kg/m2 (range, 19.07–29.41). There were no significant differences in age, parity, coital history, or BMI (Table 1) between the 2 groups.
Table 1. Demographics and physical characteristics.
| Characteristics | In-bag power morcellation | Manual scalpel morcellation | P-value | |
|---|---|---|---|---|
| Age (yr) | 34 (26–54) | 37 (26–59) | 0.372a) | |
| BMI (kg/m2) | 20.84 (18.26–28.89) | 21.93 (19.07–29.41) | 0.067a) | |
| Parity | 9.0 (33.3) | 10.7 (35.5) | 0.864b) | |
| Previous abdominal surgery history | 4 (14.8) | 9 (29.0) | 0.195b) | |
| Indication for surgery | 0.635b) | |||
| Known huge myoma | 12 (44.4) | 12 (38.7) | ||
| Hypermenorrhea | 5 (18.5) | 7 (22.6) | ||
| Myoma size increase | 5 (18.5) | 9 (29.0) | ||
| Pelvic pain | 5 (18.5) | 3 (9.7) | ||
Values are presented as median (range) or number (%).
BMI, body mass index.
a)Student's t-test; b)Pearson's χ2 test.
The surgical outcomes of the patients are shown in Table 2. The sizes of the largest uterine tissue removed differed from 4 to 10 cm vs. 3 to 9 cm, and the median specimen weight was 110 g (range, 40–413) vs. 88 g (range, 9–258). The median operating time was 138 minutes (range, 60–308) vs. 129 minutes (range, 51–270). The average time taken to prepare a device for in-bag power morcellation was approximately 5 to 10 minutes. No surgical procedures were converted from laparoscopy to laparotomy. Estimated blood loss was 50 mL (range, minimal–200) vs. 30 mL (range, minimal–180), and the median postoperative Hb change was 2.2 g/dL (range, 0.5–3.8) vs. 1.7 g/dL (range, 0–3.3). Severe adhesions requiring adhesiolysis during surgery were seen in 7 women (25.9%) in the in-bag morcellation group and 9 women (29.0%) in the manual morcellation group. The mean postoperative hospital stay was 2 days (range, 0–5) vs. 2 days (range, 1–4), and the median postoperative pain scores were 5 (range, 2–7) after 6 hours, 3 (range, 1–5) after 24 hours, and 2 (range, 1–5) after 48 hours vs. 5 (range, 1–10) after 6 hours, 3 (range, 2–7) after 24 hours, and 2 (range, 0–5) after 48 hours. There were no significant differences in surgical outcomes such as total dry specimen weight, total operating time, estimated blood loss, Hb difference, postoperative hospital stays, or postoperative pain scores (Table 2).
Table 2. Surgical outcomes.
| Outcomes | In-bag power morcellation | Manual scalpel morcellation | P-value | |
|---|---|---|---|---|
| Operation time (min) | 138 (60–308) | 129 (51–270) | 0.553a) | |
| Estimated blood loss (mL) | 50 (0–200) | 30 (0–180) | 0.059a) | |
| Hb change (g/dL) | 2.2 (0.5–3.8) | 1.7 (0–3.3) | 0.098a) | |
| Postoperative hospital stays (day) | 2 (0–5) | 2 (1–4) | 0.395a) | |
| Pain score (VAS) | ||||
| 6 hr after operation | 5 (2–7) | 5 (1–10) | 0.908a) | |
| 24 hr after operation | 3 (1–5) | 3 (2–7) | 0.347a) | |
| 48 hr after operation | 2 (1–5) | 2 (0–5) | 0.590a) | |
| Specimen dry weight (g) | 110 (40–413) | 88 (9–258) | 0.061a) | |
| Surgical complication | 0 | 0 | ||
| Pelvic adhesion requiring adhesiolysis | 7 (25.9) | 9 (29.0) | 0.792b) | |
| Pathology | 0.383b) | |||
| Leiomyoma | 23 (85.2) | 27 (87.1) | ||
| Leiomyoma with degeneration | 1 (3.7) | 3 (9.7) | ||
| Lipoleiomyoma | 1 (3.7) | 1 (3.2) | ||
| Adenomyoma | 2 (7.4) | 0 (0) | ||
Values are presented as median (range) or number (%).
Hb, hemoglobin; VAS, visual analog scale.
a)Student's t-test; b)Pearson's χ2 test.
Pathologic confirmation following the surgical removal of tissue showed that all patients had benign diseases of the uterus (Table 2). Occult malignancy was not identified in any patients. There were no intraoperative complications such as LapBag ruptures or gross spillage upon visual inspection following surgery. There was also no evidence of tissue dissemination outside of the bag.
Discussion
A major concern with power morcellation is the dissemination of removed tissue into the surrounding area [12]. The dispersal of benign pathology such as leiomyomas can result in recurrences [13]. Even more alarming is the risk of malignancy dispersal, as with endometrial cancer, which can result in a decrease in the overall survival rate [14]. Several methods of specimen removal have been reported to reduce this risk such as vaginal culdotomy or colpotomy extraction, hysteroscopic removal of submucosal myomas, and laparotomy [15]. Of particular interest is contained power morcellation, which allows the surgeon to utilize an electromechanical morcellator while eliminating the associated risks [16]. Several gynecological oncologists have delineated methods of in-bag morcellation that provide safe and feasible outcomes [17,18,19,20]. Our study describes an in-bag morcellation technique that is easily applicable for SPA laparoscopic myomectomy at our institution.
The demographics and patient characteristics of the subjects considered were similar between the in-bag power morcellation group and the manual scalpel morcellation group. Furthermore, there were no statistically significant differences in surgical outcomes between the 2 groups. A history of previous abdominal surgeries can lead to pelvic adhesions that consequently result in a more complicated and lengthy surgery. Patients with pelvic adhesions significant enough to require adhesiolysis during surgery were similar in number for both groups.
The surgical outcomes were also similar between the in-bag power morcellation group and the manual scalpel morcellation group. Although we had anticipated the surgery duration to be shorter with power morcellation, operation time was approximately 2 hours for both groups. This could be explained by the fact that total operation time included the time needed to assemble the apparatus needed for in-bag morcellation. Further prospective studies should include a calculation of exact morcellation time, excluding the time needed for preparation. Also, the patients undergoing each method were not randomized. Surgeon bias as to which patient should receive power morcellation and which patient should receive scalpel morcellation can be expected. Larger myomas, which may take longer to morcellate, are likely to have been chosen for in-bag power morcellation, while smaller myomas underwent manual scalpel morcellation. Although not statistically significant, this difference is reflected in the higher specimen dry weight found for in-bag morcellation cases (110 g) compared to manual scalpel morcellation cases (88 g). Similarities in estimated blood loss, Hb change, postoperative hospital stay, and pain scores demonstrated the non-inferiority of in-bag power morcellation. There were no surgical complications, such as wound complications, fistulas, adjacent organ injuries, or recurrences, for either group. Our in-bag power morcellation method had not been actively utilized until recently, so long-term follow-up of patients was not possible. Complications such as recurrences may be discovered if a long-term follow-up is done.
The strength of our study was the fact that all data retrieved was from a single medical facility and all surgical procedures were performed by a single, experienced gynecologic surgeon with the same protocol. This reduced variations in technique. Inter-observer bias was also prevented. A limitation of this study was its small population pool and homogenous patient demographics. Additional randomized trials involving a larger population should be carried out to fully corroborate the data found in this study and evaluate the potential benefits of this surgical technique. All results were coalesced retrospectively, allowing the possibility of selection bias. We were not able to determine if any microspillage occurred during the surgery because we did not test the LapBag for microperforations. Only visual examinations for gross spillage were done. Further analysis utilizing dyes postoperatively to identify any microperforations could be conducted to provide a more exhaustive database.
A special report was released by the American Congress of Obstetricians and Gynecologists stating that power morcellation should be permitted for women who would benefit from it, but appropriate patient selection and informed consent are necessary [21]. A statement from the American Association of Gynecologic Laparoscopists also asserted that converting all surgical procedures to open surgeries instead of using power morcellation would result in higher mortality rates from surgery [22]. Undoubtedly, power morcellation has its benefits, and appropriate use should be considered suitable as long as patients are properly informed of the risks. The U.S. Food and Drug Administration even released a statement allowing a tissue containment system to be marketed [23].
In conclusion, in-bag power morcellation for SPA laparoscopic myomectomy is feasible and safe, minimizing the risks of open power morcellation.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
Supplementary materials
Supplementary video associated with this article can be found online at https://doi.org/10.5468/ogs.2018.61.2.267.
Myoma power morcellation in 3XL LapBag.
Attaching 3XL LapBag.
Laparoscopic intra-abominal view of In-bag power morcellation.
References
- 1.Bhave Chittawar P, Franik S, Pouwer AW, Farquhar C. Minimally invasive surgical techniques versus open myomectomy for uterine fibroids. Cochrane Database Syst Rev. 2014:CD004638. doi: 10.1002/14651858.CD004638.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009:CD003677. doi: 10.1002/14651858.CD003677.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Wright KN, Jonsdottir GM, Jorgensen S, Shah N, Einarsson JI. Costs and outcomes of abdominal, vaginal, laparoscopic and robotic hysterectomies. JSLS. 2012;16:519–524. doi: 10.4293/108680812X13462882736736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parker WH. Indications for morcellation in gynecologic surgery. Curr Opin Obstet Gynecol. 2018;30:75–80. doi: 10.1097/GCO.0000000000000427. [DOI] [PubMed] [Google Scholar]
- 5.Steiner RA, Wight E, Tadir Y, Haller U. Electrical cutting device for laparoscopic removal of tissue from the abdominal cavity. Obstet Gynecol. 1993;81:471–474. [PubMed] [Google Scholar]
- 6.Carter JE, McCarus SD. Laparoscopic myomectomy. Time and cost analysis of power vs. manual morcellation. J Reprod Med. 1997;42:383–388. [PubMed] [Google Scholar]
- 7.Milad MP, Milad EA. Laparoscopic morcellator-related complications. J Minim Invasive Gynecol. 2014;21:486–491. doi: 10.1016/j.jmig.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Kho KA, Nezhat CH. Evaluating the risks of electric uterine morcellation. JAMA. 2014;311:905–906. doi: 10.1001/jama.2014.1093. [DOI] [PubMed] [Google Scholar]
- 9.Graebe K, Garcia-Soto A, Aziz M, Valarezo V, Heller PB, Tchabo N, et al. Incidental power morcellation of malignancy: a retrospective cohort study. Gynecol Oncol. 2015;136:274–277. doi: 10.1016/j.ygyno.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 10.US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication [Internet] Silver Spring (MD): US Food and Drug Administration; 2014. [cited 2017 Mar 27]. Available from: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. [Google Scholar]
- 11.Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010;203:26.e1–26.e6. doi: 10.1016/j.ajog.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 12.Kho KA, Anderson TL, Nezhat CH. Intracorporeal electromechanical tissue morcellation: a critical review and recommendations for clinical practice. Obstet Gynecol. 2014;124:787–793. doi: 10.1097/AOG.0000000000000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leren V, Langebrekke A, Qvigstad E. Parasitic leiomyomas after laparoscopic surgery with morcellation. Acta Obstet Gynecol Scand. 2012;91:1233–1236. doi: 10.1111/j.1600-0412.2012.01453.x. [DOI] [PubMed] [Google Scholar]
- 14.Anupama R, Ahmad SZ, Kuriakose S, Vijaykumar DK, Pavithran K, Seethalekshmy NV. Disseminated peritoneal leiomyosarcomas after laparoscopic “myomectomy” and morcellation. J Minim Invasive Gynecol. 2011;18:386–389. doi: 10.1016/j.jmig.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 15.AAGL Advancing Minimally Invasive Gynecology Worldwide. AAGL practice report: morcellation during uterine tissue extraction. J Minim Invasive Gynecol. 2014;21:517–530. doi: 10.1016/j.jmig.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Nezhat F, Apostol R, Greene AD, Pilkinton ML. To morcellate or not to morcellate: a cross-sectional survey of gynecologic surgeons. JSLS. 2017;21:e2016.00092. doi: 10.4293/JSLS.2016.00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen SL, Einarsson JI, Wang KC, Brown D, Boruta D, Scheib SA, et al. Contained power morcellation within an insufflated isolation bag. Obstet Gynecol. 2014;124:491–497. doi: 10.1097/AOG.0000000000000421. [DOI] [PubMed] [Google Scholar]
- 18.Serur E, Zambrano N, Brown K, Clemetson E, Lakhi N. Extracorporeal manual morcellation of very large uteri within an enclosed endoscopic bag: our 5-year experience. J Minim Invasive Gynecol. 2016;23:903–908. doi: 10.1016/j.jmig.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 19.Srouji SS, Kaser DJ, Gargiulo AR. Techniques for contained morcellation in gynecologic surgery. Fertil Steril. 2015;103:e34. doi: 10.1016/j.fertnstert.2015.01.022. [DOI] [PubMed] [Google Scholar]
- 20.Vargas MV, Cohen SL, Fuchs-Weizman N, Wang KC, Manoucheri E, Vitonis AF, et al. Open power morcellation versus contained power morcellation within an insufflated isolation bag: comparison of perioperative outcomes. J Minim Invasive Gynecol. 2015;22:433–438. doi: 10.1016/j.jmig.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 21.American College of Obstetricians and Gynecologists. Executive summary. Power morcellation and occult malignancy in gynecologic surgery: a special report. Silver Spring (MD): US Food and Drug Administration; 2014. [Google Scholar]
- 22.American Association of Gynecologic Laparoscopists. AAGL statement to the FDA on power morcellation. Cypress (CA): American Association of Gynecologic Laparoscopists; 2014. [Google Scholar]
- 23.US Food and Drug Administration. FDA allows marketing of first-of-kind tissue containment system for use with certain laparoscopic power morcellators in select patients. Silver Spring (MD): US Food and Drug Administration; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Myoma power morcellation in 3XL LapBag.
Attaching 3XL LapBag.
Laparoscopic intra-abominal view of In-bag power morcellation.