Abstract
Background:
Periostin acts as a necessary protein for tissue integrity and maturity and has a key role as a modulator of periodontal ligament hemostasis. It has been shown that periostin acts as a supportive protein. The aim of this study was to compare the concentration of periostin in the saliva of patients with chronic periodontitis and healthy controls.
Materials and Methods:
In this case–control, cross-sectional study, a total of 45 individuals (25 patients with chronic periodontitis and 20 healthy controls) were evaluated. Whole saliva samples were collected, and periostin levels were evaluated by standard enzyme-linked immunosorbent assay. The results were analyzed by SPSS and Mann–Whitney analysis.
Results:
The results of this study showed that the level of periostin in saliva in patients with periodontitis was significantly lower than healthy controls (P < 0.05). Periostin was detectable in all samples.
Conclusion:
The results show that there is a significant relationship between the level of periostin in saliva and chronic periodontitis. Periostin may be considered as an inflammatory marker in periodontal disease. However, further studies are needed to confirm this finding.
Key words: Chronic periodontitis, periostin, saliva
INTRODUCTION
Periodontitis is an infectious condition caused by periodontal pathogens, which affect the composition and integrity of periodontal structure and cause destruction of cells and connective tissue matrix, clinical attachment loss (CAL), alveolar bone resorption, periodontal pocket formation, and gingival inflammation.[1,2]
Saliva can also reveal the systemic health as well as the oral health to some extent. Whole saliva may also show the presence of periodontal disease, and evidence indicates that the level of some cytokines increases in the saliva of patients with periodontitis. Assessment of the composition of saliva may provide valuable information about biochemical markers for assessment of periodontal diseases.[3]
Periostin is a hemophilic, secretory protein from the fasciclin I family.[4] It is expressed in collagen-rich tissues and fibrous connective tissues such as the heart valves, tendons, cornea, and periodontal ligament (PDL).[5] Periostin serves as a necessary protein for the integrity, development, and maturity of the tissue, and it is believed to play a key role in balancing and regulating homeostasis of the PDL.[6] Expression of periostin is induced by the tumor growth factor (TGF)-β and bone morphogenetic protein-2. It reinforces the cross-linking of collagen and improves the mechanical properties of the connective tissue.[4,5,6,7,8] Furthermore, it has been shown that expression of periostin increases during wound healing.[9]
Some studies have reported a significant association between the severity of periodontal disease and the level of periostin.[9,10,11] However, another study found no significant difference in the level of periostin in periodontitis patients and healthy controls.[5] Considering the existing controversy regarding the correlation of periostin and periodontal disease and gap of information on the level of periostin in the saliva, this study aimed to determine and compare the concentration of periostin in the saliva of patients with chronic periodontitis and healthy controls.
MATERIALS AND METHODS
This case–control, cross-sectional study was performed from December 2016 to August 2017 at the Periodontology Department of Shahid Beheshti University of Medical Sciences. In this study, 45 individuals (15 males and 30 females, aged 25–50 years) including 25 patients with chronic periodontitis and 20 periodontally healthy controls were enrolled. The sample size formula that we used was as follows:
n = (Zα/2 + Zβ) 2 × 2 × σ2/d2
(n = sample size = 17)
Zα = 1.96
Zβ = 0.84
d = difference between two groups = 112
All individuals gave the written informed consent. Institutional ethics review committee approval was obtained. The exclusion criteria of the study include (1) cigarette smoking or tobacco use and alcoholism; (2) systemic diseases such as diabetes mellitus, hypertension, and rheumatoid arthritis; (3) pregnancy; (4) systemic bacterial, viral, or fungal infection; (5) history of antibiotic therapy or use of anti-inflammatory medications during the past 6 months; (6) periodontal therapy during the past 2 years; and (7) patients with aggressive periodontitis.
Periodontal patients were selected according to the criteria set by the American Academy of Periodontology in 1999[12] and had a minimum of two teeth with probing pocket depth (PPD) ≥5 mm, CAL ≥4 mm, and positive bleeding on probing in involved areas. Healthy controls had gingival index <1 mm, PPD <3 mm, and no CAL.
Sampling
Volunteers were enrolled after signing informed consent forms and subjected to intraoral and periodontal examinations. They were requested to refrain from eating and drinking for at least 2 h before saliva collection. Oral cavity was also evaluated to ensure the absence of debris. Using the spitting method,[13] unstimulated saliva was collected between 11:00 am and 13:00 pm for 5 min (one spit per minute). The saliva was collected in sterile tubes and immediately frozen at −70°C until the experiment. After thawing, ELISA kit (RD191016100; BioVendor Laboratory Medicine, Brno, Czech Republic) was used to determine the concentration of periostin. All procedures were carried in accordance with the manufacturer's instructions. Absorbance of wells was measured by ELISA reader (BioTeK Instruments Inc., Winooski, VT, USA) at wavelength of 450 nm. The concentration of periostin was estimated using the assay standard criteria. All laboratory analyses were performed in the Dental Biomaterials Department of Shahid Beheshti University of Medical Sciences.
Data analysis
Statistical analyses were performed using SPSS software-version 21 (SPSS Inc., Chicago, IL, USA). The salivary level of periostin was compared between the two groups using the Mann–Whitney test and t-test. P < 0.05 was considered statistically significant. Data were presented as mean ± standard deviation.
RESULTS
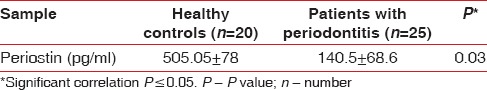
Salivary levels of periostin in the two groups are shown in Table 1. The mean salivary level of periostin was significantly different in patients with periodontitis and healthy controls (P < 0.05). The mean level of periostin was significantly lower in the saliva of patients with periodontitis compared to healthy controls (P = 0.03). Periostin was detectable in all of the samples.
Table 1.
Salivary levels of periostin (mean±standard deviation)
DISCUSSION
Periostin serves as a necessary protein for the integrity and maturation of tissues. It is believed that periostin plays a key role in regulating the PDL homeostasis.[14] This study compared the concentration of periostin in the saliva of patients with periodontitis and healthy controls. Considering the high level of periostin in collagen-rich connective tissue,[5] it is estimated that increased gingival inflammation and periodontal destruction may be responsible for reduction in the salivary level of periostin. Periostin plays an important role in tissue integrity and development of teeth.[15,16,17] It serves as a supporting protein for the periodontium.[18] In a study by Balli et al.,[11] level of periostin in the serum and gingival crevicular fluid of patients with periodontitis was significantly lower than that in healthy controls; their results were in agreement with ours, and it may be concluded that periostin plays a role in periodontal health. Furthermore, as a cellular matrix protein, periostin is extensively expressed in the PDL and periosteum.[4] Level of periostin in fetal periosteum has reported to be very high in bone formation stage.[19] High levels of periostin are also detected in periosteum and PDL in case of fracture, mechanical load application, tooth movement, and tooth eruption.[17,20,21]
TGF-β1 stimulates the release of periostin from the human gingival fibroblasts, while this process is inhibited by tumor necrosis factor-alpha (TNF-α).[22] Interleukins (ILs) 13 and 14 cause significant upregulation of periostin in human gingival and PDL fibroblasts. These two cytokines are detected in periodontal defects.[23] However, lipopolysaccharide of Porphyromonas gingivalis has no significant effect on the level of periostin. Furthermore, periostin has a stimulatory effect on the level of IL6, IL8, and monocyte chemotactic protein 1.[18] An animal study revealed the role of periostin in experimentally induced periodontitis and periodontitis-induced bone destruction. It has been showed that level of periostin decreased over time in the presence of inflammation. A correlation was noted between alveolar bone loss and level of periostin.[14] In periodontitis patients, level of periostin decreases due to two reasons. The first reason is bacteria. Bacterial competition can cause a reduction in level of periostin produced by PDL fibroblasts. The second reason is that reduction in number of PDL fibroblasts can cause a reduction in the level of periostin. Reduction in the level of periostin compromises PDL stability and increases the risk of subsequent damage and inflammatory process due to reduction in biomechanical and structural potential of PDL.[16,17]
In the current study, level of periostin was lower in the saliva of periodontitis patients. Periostin may be used as an inflammatory marker for detection of periodontal disease. Further studies are required to assess the efficacy of this biomarker for early detection of periodontal disease and prevention of its progression. First limitation of this study was that we did not have information about the level of periostin after treatment of periodontitis. Such information would be useful for understanding the role of periostin in periodontal regeneration. Second, the sample size was limited due to the inclusion and exclusion criteria, which makes it difficult to interpret the data; however, the potential confounding factors are minimized. Furthermore, there is no definitive conclusion due to the existing limitations. Finally, for considering periostin as biomarkers of inflammation in periodontitis, further studies are needed with more sample size in different populations.
CONCLUSION
The results show that there is a significant relationship between the level of periostin in saliva and chronic periodontitis. Furthermore, periostin levels in saliva may be considered as a promising diagnostic potential in periodontal disease; however, further studies are needed to confirm this finding.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This study was supported by a grant from School of Dentistry, Shahid Beheshti University of Medical Sciences.
REFERENCES
- 1.Benatti BB, Silvério KG, Casati MZ, Sallum EA, Nociti FH., Jr Physiological features of periodontal regeneration and approaches for periodontal tissue engineering utilizing periodontal ligament cells. J Biosci Bioeng. 2007;103:1–6. doi: 10.1263/jbb.103.1. [DOI] [PubMed] [Google Scholar]
- 2.Giannobile WV. Host-response therapeutics for periodontal diseases. J Periodontol. 2008;79:1592–600. doi: 10.1902/jop.2008.080174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller CS, King CP, Jr, Langub MS, Kryscio RJ, Thomas MC. Salivary biomarkers of existing periodontal disease: A cross-sectional study. J Am Dent Assoc. 2006;137:322–9. doi: 10.14219/jada.archive.2006.0181. [DOI] [PubMed] [Google Scholar]
- 4.Horiuchi K, Amizuka N, Takeshita S, Takamatsu H, Katsuura M, Ozawa H, et al. Identification and characterization of a novel protein, periostin, with restricted expression to periosteum and periodontal ligament and increased expression by transforming growth factor beta. J Bone Miner Res. 1999;14:1239–49. doi: 10.1359/jbmr.1999.14.7.1239. [DOI] [PubMed] [Google Scholar]
- 5.Norris RA, Damon B, Mironov V, Kasyanov V, Ramamurthi A, Moreno-Rodriguez R, et al. Periostin regulates collagen fibrillogenesis and the biomechanical properties of connective tissues. J Cell Biochem. 2007;101:695–711. doi: 10.1002/jcb.21224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Padial-Molina M, Volk SL, Rodriguez JC, Marchesan JT, Galindo-Moreno P, Rios HF, et al. Tumor necrosis factor-α and porphyromonas gingivalis lipopolysaccharides decrease periostin in human periodontal ligament fibroblasts. J Periodontol. 2013;84:694–703. doi: 10.1902/jop.2012.120078. [DOI] [PubMed] [Google Scholar]
- 7.Ji X, Chen D, Xu C, Harris SE, Mundy GR, Yoneda T, et al. Patterns of gene expression associated with BMP-2-induced osteoblast and adipocyte differentiation of mesenchymal progenitor cell 3T3-F442A. J Bone Miner Metab. 2000;18:132–9. doi: 10.1007/s007740050103. [DOI] [PubMed] [Google Scholar]
- 8.Norris RA, Moreno-Rodriguez R, Hoffman S, Markwald RR. The many facets of the matricelluar protein periostin during cardiac development, remodeling, and pathophysiology. J Cell Commun Signal. 2009;3:275–86. doi: 10.1007/s12079-009-0063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Padial-Molina M, Volk SL, Rios HF. Preliminary insight into the periostin leverage during periodontal tissue healing. J Clin Periodontol. 2015;42:764–72. doi: 10.1111/jcpe.12432. [DOI] [PubMed] [Google Scholar]
- 10.Kumaresan D, Balasundaram A, Naik VK, Appukuttan DP. Gingival crevicular fluid periostin levels in chronic periodontitis patients following nonsurgical periodontal treatment with low-level laser therapy. Eur J Dent. 2016;10:546–50. doi: 10.4103/1305-7456.195179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balli U, Keles ZP, Avci B, Guler S, Cetinkaya BO, Keles GC, et al. Assessment of periostin levels in serum and gingival crevicular fluid of patients with periodontal disease. J Periodontal Res. 2015;50:707–13. doi: 10.1111/jre.12254. [DOI] [PubMed] [Google Scholar]
- 12.Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1–6. doi: 10.1902/annals.1999.4.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Navazesh M, Christensen CM. A comparison of whole mouth resting and stimulated salivary measurement procedures. J Dent Res. 1982;61:1158–62. doi: 10.1177/00220345820610100901. [DOI] [PubMed] [Google Scholar]
- 14.Padial-Molina M, Volk SL, Taut AD, Giannobile WV, Rios HF. Periostin is down-regulated during periodontal inflammation. J Dent Res. 2012;91:1078–84. doi: 10.1177/0022034512459655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kruzynska-Frejtag A, Wang J, Maeda M, Rogers R, Krug E, Hoffman S, et al. Periostin is expressed within the developing teeth at the sites of epithelial-mesenchymal interaction. Dev Dyn. 2004;229:857–68. doi: 10.1002/dvdy.10453. [DOI] [PubMed] [Google Scholar]
- 16.Rios H, Koushik SV, Wang H, Wang J, Zhou HM, Lindsley A, et al. Periostin null mice exhibit dwarfism, incisor enamel defects, and an early-onset periodontal disease-like phenotype. Mol Cell Biol. 2005;25:11131–44. doi: 10.1128/MCB.25.24.11131-11144.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rios HF, Ma D, Xie Y, Giannobile WV, Bonewald LF, Conway SJ, et al. Periostin is essential for the integrity and function of the periodontal ligament during occlusal loading in mice. J Periodontol. 2008;79:1480–90. doi: 10.1902/jop.2008.070624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakajima M, Honda T, Miyauchi S, Yamazaki K. Th2 cytokines efficiently stimulate periostin production in gingival fibroblasts but periostin does not induce an inflammatory response in gingival epithelial cells. Arch Oral Biol. 2014;59:93–101. doi: 10.1016/j.archoralbio.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Merle B, Garnero P. The multiple facets of periostin in bone metabolism. Osteoporos Int. 2012;23:1199–212. doi: 10.1007/s00198-011-1892-7. [DOI] [PubMed] [Google Scholar]
- 20.Hakuno D, Kimura N, Yoshioka M, Mukai M, Kimura T, Okada Y, et al. Periostin advances atherosclerotic and rheumatic cardiac valve degeneration by inducing angiogenesis and MMP production in humans and rodents. J Clin Invest. 2010;120:2292–306. doi: 10.1172/JCI40973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamilton DW. Functional role of periostin in development and wound repair: Implications for connective tissue disease. J Cell Commun Signal. 2008;2:9–17. doi: 10.1007/s12079-008-0023-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arancibia R, Oyarzún A, Silva D, Tobar N, Martínez J, Smith PC, et al. Tumor necrosis factor-α inhibits transforming growth factor-β-stimulated myofibroblastic differentiation and extracellular matrix production in human gingival fibroblasts. J Periodontol. 2013;84:683–93. doi: 10.1902/jop.2012.120225. [DOI] [PubMed] [Google Scholar]
- 23.Sidhu SS, Yuan S, Innes AL, Kerr S, Woodruff PG, Hou L, et al. Roles of epithelial cell-derived periostin in TGF-beta activation, collagen production, and collagen gel elasticity in asthma. Proc Natl Acad Sci U S A. 2010;107:14170–5. doi: 10.1073/pnas.1009426107. [DOI] [PMC free article] [PubMed] [Google Scholar]


