Abstract
The use of magnification to perform various procedures in medical and dental field, particularly endodontics has long been recognized. Unfortunately, its application in periodontics is not widely popularized. The objective of this article is to emphasize the application of microsurgical principles in various periodontal surgical procedures and to reinforce the incorporation of microscope into periodontal practice. The most recent periodontal journals were reviewed and a search of databases such as PubMed or Medline and Google Scholar was conducted for relevant material from published literature up to 2017. Medical Subject Headings words looked for were “periodontal microsurgery” and “minimally invasive periodontal surgery.” The available literature, specifically to periodontal surgical procedures was analyzed and compiled. The analysis indicates that incorporation of magnification in periodontal practice is associated with improved visual acuity, ergonomic benefits, decreased patient morbidity, rapid healing, and enhanced patient acceptance.
Key words: Ergonomics, magnification, minimally invasive, periodontal microsurgery, surgical microscope
INTRODUCTION
Dental sciences have gone through a plethora of changes both in concepts and techniques in the last few decades. Although the use of loupes and surgical operating microscope to achieve magnification to perform various procedures in different disciplines of medical and surgical field is widely acclaimed, its incorporation in dentistry, particularly periodontics needs to be addressed at a broader level. This article provides a review of applications of periodontal microsurgery for the procedures ranging from mucogingival surgeries to the regenerative procedures and implant dentistry. A brief overview of microsurgical principles, ergonomics, and instruments is also discussed.
MATERIALS AND METHODS
A thorough literature search of PubMed or Medline and Google Scholar was conducted for relevant material from studies up to 2017. Medical Subject Headings words searched were “periodontal microsurgery” and “minimally invasive periodontal surgery.” Systematic and narrative reviews, relevant case reports/case series, clinical and comparative studies pertaining specifically to periodontal surgical procedures and published in English were included. All articles were selected with no inclusion or exclusion criteria.
History
Daniel defined microsurgery in broad terms as surgery performed under magnification by the microscope.[1] Serafin described microsurgery as a methodology – modification and refinement of existing surgical techniques using magnification to improve visualization, with applications to all specialties.[2]
Apotheker and Jako first introduced commercial operating microscope to dentistry in 1981.[3] Microsurgery was introduced to the field of periodontics in 1992.[4] A continuing education course was subsequently conferred by Shanelec and Tibbetts on periodontal microsurgery at the annual meeting of the American Academy of Periodontology held in 1993.[5]
Microsurgical triad
Operating microscope renders three unambiguous benefits of illumination, magnification, and increased precision in delivery of surgical skills, collectively known as microsurgical triad [Figure 1].[6] Illumination achieved through fiberoptic technology has improved the methods of focusing light on specific areas and is a standard feature of surgical operating microscopes.
Figure 1.
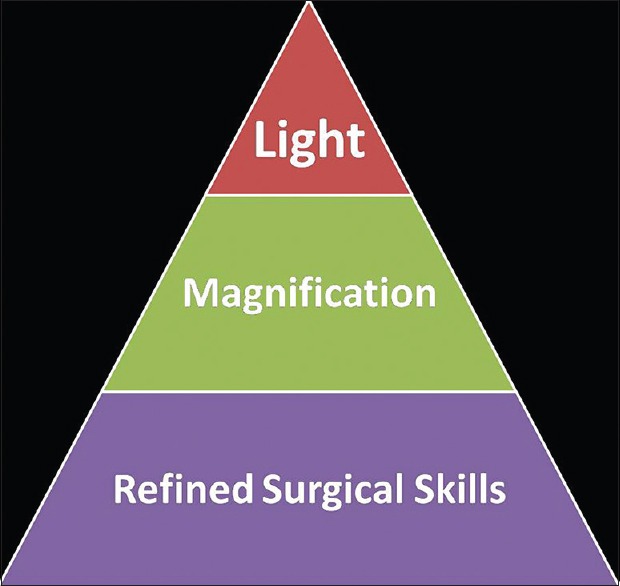
Microsurgical triad
Magnification, the second component of the microsurgical triad, can be achieved through the use of the loupes and the operating microscope. Both types of optical magnification have their own advantages and limitations.[7] Loupes can be simple, compound, or prism in design. These are available in the form of eyeglasses or attached to a headset.
Compound and prism designs produce superior magnification and are commonly used in dentistry today.[8] Caplan published an excellent review article that describes comparison of different types of loupes.[9] In a well-established periodontal microsurgical practice, 70%–80% of the typical periodontal microsurgeries can be done at a magnification of ×10–×20 with the surgical operating microscope. The remaining procedures can be performed with loupes under ×6–×8 using enhanced motor skills acquired during microsurgery training sessions with a surgical microscope.[10] Under magnification of ×20, the preciseness of hand movement approaches 10 μm and visual resolution approaches 1 μm.[11] Proprioceptive guidance is therefore of little value under the microscope.[12]
Increased precision in delivery of surgical skills, the third component of microsurgical triad, is the synergistic result of illumination and magnification.
Ergonomics in microsurgery
Operating surgeon must have a relaxed state of mind, good body comfort and posture, a well-supported hand, and a stable instrument-holding position.[7] To accomplish precise controlled movements of fingers, the ulnar surface of the forearm and wrist should be supported by resting on a flat surface, angled in a dorsiflexion position at approximately 20° to reduce muscle tremor originating from both the unintentional and intentional actions of the body.[13,14] The operating surgeon must be seated upright (back straight and head erect) with both feet flat on floor so that thighs are parallel to the floor. All movements should be efficient enough to produce purposeful, deliberate motions.
The most commonly advocated precision grip for microsurgical procedures is the pen grip or internal precision grip [Figure 2], which provides a greater stability in comparison to any other hand grip due to the tripod formed by the fingers, while the middle finger holds the instrument.[13,15] It is best to start with the pen grip until basic manipulations are mastered and more freehand positions can be initiated.[7]
Figure 2.
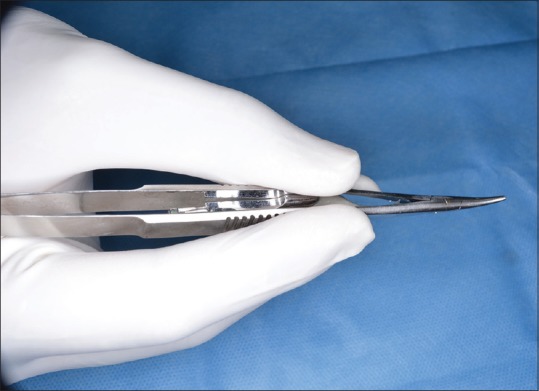
Precision grip
Ergonomic benefits in the form of diminished shoulder, neck, and back problems, improved vision, and reduced eye fatigue have been reported from the findings of qualitative research at Vancouver Community College in British Columbia.[16,17] Therefore, beneficial ergonomic aspect of magnification may be the most influential factors in its adoption by the dental profession at large scale.
Microsurgical instruments
Smaller instruments can be used with more precision due to improved visual acuity. To aid in proper handling and for a high-precision movement, microsurgical instruments should be slightly top heavy, circular in cross-section, and approximately 18 cm in length.[18] Shorter instruments with a rectangular cross-sectional design do not allow precise manipulation and are not ideal for microsurgery.[7] Microsurgical instruments usually have a color-coated surface to avoid an unfavorable metallic flare due to the light of the microscope. Weight of microsurgical instruments should not be more than 15–20 g to avoid fatigue of hand and arm muscles.[18] Needle holders should have an appropriate working lock which does not surpass a locking force of 50 g (0.5 N) as low locking forces diminish the precision and high locking forces engender tremors [Figure 3].[18]
Figure 3.
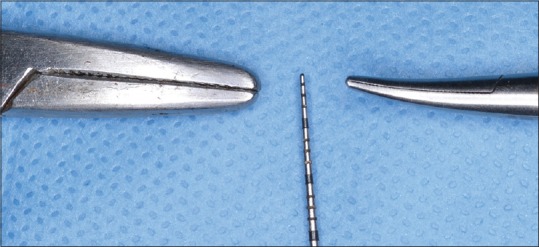
Relative size of microsurgical and conventional needle holder
Different manufacturers provide sets of periodontal microsurgical instruments made of steel or titanium. Titanium made microsurgical instruments are stronger, lighter, and nonmagnetized in comparison to stainless steel instruments but are expensive and get readily distorted, if not properly cared. Care should be taken during sterilization procedures and transportation so as not to allow instrument's tips to touch each other.[18]
A basic set of microsurgical instruments comprises a microscalpel holder, needle holder, microscissors, microforceps, and elevators. Different types of blades used in ophthalmic surgery can also be used for periodontal microsurgery [Figure 4].
Figure 4.

Periodontal microsurgical knives
The advantage of these knives is their small size and extreme sharpness.[6] This enables clean, non-ragged incisions to achieve wound healing by primary intention. Needle holders, elevators, mirrors are downsized from those used for conventional periodontal surgery. Small tissue pieces can be removed more efficiently with micro-Vannas scissors.[19] Slippage of the suture thread while tying a knot can be avoided using forceps with flat surfaced tips or needle holders with a surface roughened through the finely coated diamond grain.[20]
To minimize the tissue trauma, the sharpest needles, spatula needle (6.6 mm long with curvature of 140°) with microtips, or reverse cutting needles with precision tips are preferred.[20,21] For microsurgical periodontal procedures, 3/8” circular needle usually provide favorable results. As far as the length of the needle is concerned, 13–15-mm long needles are considered adequate for papillary sutures in posterior areas, 10–12-mm needle lengths in the anterior region, and 5–8 mm long needles are suitable for approximating vertical incisions.[18] Most periodontal microsurgical suturing is done with sutures ranging in size from 6-0 to 9-0 [Figure 5]. Among the different suture materials available, monofilament nonabsorbable sutures are more preferable but should be removed at the earliest biologically acceptable time.[22] Interestingly, suture materials like Vicryl® Plus (Ethicon®, Norderstedt, Germany) coated with a bacteriostatic substance like triclosan seem to be a looming alternative to further minimize the microbial passage along the sutures.[23,24]
Figure 5.
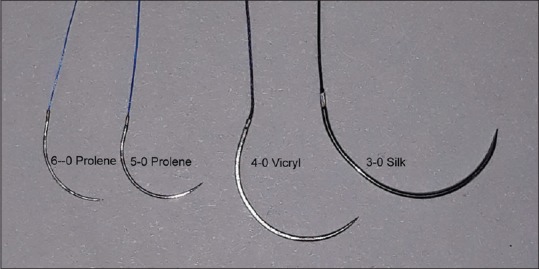
Relative size of different sutures
The combined use of small-sized needles and sutures under magnification permits wound closure with sufficient tension and least possible dead space.
Microsurgical suturing
Suturing techniques in microsurgery differ from conventional surgery. In microsurgical procedures, the needle should penetrate perpendicular to the tissues and exit at equal distances. Suture bite size should be approximately 1.5 times the tissue thickness to achieve proper wound approximation.[25]
Knot tying using the microscope is done using instrument ties, with a microsurgical needle holder in the dominant hand and a microsurgical tissue pickup in the nondominant hand.[7] Integrity of a knot is best achieved with square knots and the preferred knot combination is a surgeon's knot followed by a square knot. Adding excess ties to a knot increases its bulk rather than an increase in its strength or integrity.[19]
Recently, a novel suturing technique based on both the vertical and horizontal mattress sutures supported at the temporarily splinted interdental contact points has been described to ensure a proper soft-tissue harmonization along with atraumatic displacement in minimally invasive periodontal plastic procedures and management of soft tissues around implants.[26]
Clinical applications
Periodontal microsurgery is the descendant of conventional periodontal surgery in an attempt to reduce the surgical trauma and opens the horizons for better patient care.
-
Root surface debridement: The importance of root debridement is recognized universally as an essential component of periodontal therapy.[27,28,29,30] Several authors have emphasized that thoroughness of root surface debridement is more crucial for the improved outcome of periodontal treatment rather than the choice of grafting modality [Figure 6].[31,32] It has been reported that root instrumentation is effective when done under illumination[33] along with an improved early healing index and less postoperative pain[34]
Furthermore, root preparation can be done with microultrasonic instruments. The smaller size (about 0.2–0.6 mm in diameter) and variable power settings (25,000 to more than 40,000 cycles per second) of these instruments allows subgingival treatment in deep pockets with less chances of overinstrumentation of the root surface.[35] Moreover, these instruments have active working sides on all surfaces; deliver ultrasonically activated lavage in the working area and can be used with minimal water spray In conclusion, magnification improves the root surface debridement by enhancing clinician's ability to differentiate the calculus from tooth surface and biofilm to the microscopic level, which reveals morphological contours of both supragingival and subgingival tooth surfaces and accurately procreates working end angles during instrumentation[36]
-
Periodontal regeneration: In the last decades, a modification in the existing surgical procedures and their clinical effectiveness for periodontal regeneration of intrabony defects has been extensively studied.[37,38,39,40,41] Several authors have proposed the use of microsurgical approach for the treatment of isolated[42,43,44,45,46,47,48,49,50] or multiple[51,52] intrabony defects. The advantages of microsurgical approach in regenerative therapy relate to improved illumination and magnification of the surgical field that permits proper access to and debridement of the intrabony defect with an increased accuracy and minimal trauma.[45,46] Furthermore, the competency to achieve and maintain a primary wound closure minimizes bacterial contamination, and thereby provides more favorable conditions for periodontal regeneration[44,49,50,53]
Minimal marginal tissue recession and thus improved esthetics[44,49,50,52,54,55] and a very limited intra- and postoperative morbidity, thereby high patient acceptance and satisfaction,[45,46,49,52,55,56] are the other advantages of microsurgical approach for the treatment of intrabony defects. Nevertheless, it should be noted that probing depth reduction and clinical attachment level gain for the regenerative procedures performed with microsurgical approach has been found similar to those achieved with conventional surgical approach.[57,58,59] A recent meta-analysis found no significant differences in treatment of intrabony defects treated with minimally invasive periodontal surgery (MIPS) plus biomaterials and MIPS alone for the observed parameters (probing depth, clinical attachment level, marginal recession, and radiographic bone fill), pointing out that costs and benefits should be considered substantially while deciding a regenerative therapeutic modality[60]
Isolated interproximal defects that are usually limited to interproximal site are considered ideal for bone grafting with MIPS. Generalized horizontal bone loss and multiple interconnected intrabony defects are a contraindication for MIPS and are best managed with more conventional surgical approaches.[57] In MIPS, head-mounted operating microscope (Varioscope®) with appropriate lightening is preferable rather than a surgical microscope as it allows the visualization of the defect more easily from different angles for proper debridement of the periodontal defect and the root surfaces[57]
Apart from MIPS, minimally invasive nonsurgical therapy has shown significant clinical (probing depth, clinical attachment level) and radiographic improvements for the treatment of periodontal intrabony defects[61]
Recently, a new microsurgical approach for periodontal regeneration named “Entire Papilla Preservation Technique” (EPP) has been described in literature. In this technique, an interdental tunnel is made through the defect associated papilla by giving a beveled vertical releasing incision in the buccal gingiva of the adjacent interdental space.[62] After granulation tissue removal and root surface debridement, regenerative materials such as bone grafts and enamel matrix derivative are applied. Primary advantage of EPP technique is enhanced wound stability and limited premature exposure of regenerative biomaterials
Mucogingival surgery: To achieve an excellent result in terms of both esthetics and function, it is fundamental to perform extremely fine and accurate incisions, meticulous suturing to promote stabilization and immobilization of the graft [Figure 7],[63] and precise closure of wound margins. Therefore, the use of surgical microscope in mucogingival therapy might be helpful for those sites where esthetics demand complete and perfect coverage. Periodontal microsurgery performed by a trained and skilled surgeon offers an improved outcome of the root coverage procedures[64,65,66,67,68,69] and interdental papilla augmentation.[70] Compared to the conventional macrosurgical approach for the treatment of gingival recession, microsurgical approach has been shown to offer the distinct advantage of increased vascularization of the grafts,[65] relatively better percentages of root coverage,[65,71,72,73] a significant increase in width and thickness of keratinized tissue,[66] an improved esthetic outcome,[64,74] and decreased patient morbidity[67,75]
Implant therapy: Surgical microscope can be a valuable tool in implant dentistry. Different stages of implant treatment ranging from implant placement to implant recovery and peri-implantitis management may be accomplished with more precision under magnification.[76,77] One of the novel applications of microsurgery is in the sinus lift procedure with a success rate of 97%.[78,79] The surgical microscope can aid indirect visualization of the sinus membrane and minimizes the risk of perforations. Incorporation of microsurgical techniques for an improvement of altered sensation due to implants encroaching on the inferior alveolar nerve even without unscrewing them has also been reported[80]
Crown lengthening: Although the comparative studies of crown lengthening[81] and ridge augmentation[82,83] with microsurgical methods are limited, it seems logical to substantiate the fact that magnification is beneficial in such procedures.
Figure 6.
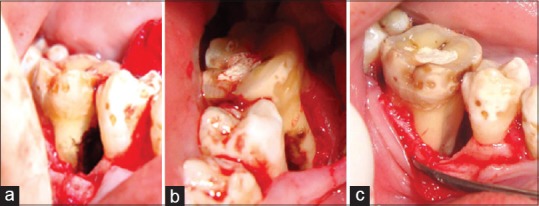
Root surface debridement. (a) Buccal and (b) lingual view showing calculus along the root surface of the bony defect and (c) after root preparation
Figure 7.
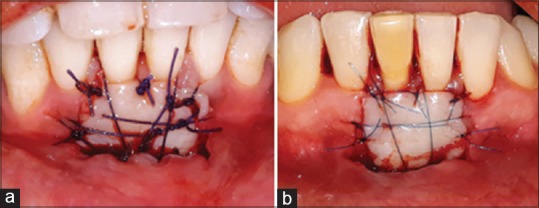
Free gingival graft sutured with (a) 4-0 and (b) 6-0 suture
Despite the several benefits of microsurgical principles and techniques, limited adoption of microsurgery in periodontal surgical practice may owe to its inherent disadvantages. These may include restricted areas of vision, loss of depth of field and visual reference point, steep learning curve, and a relatively higher initial cost of microsurgical setup.
Recent advances in microsurgery include three-dimensional on-screen microsurgery system (allows three-dimensional view of the working surgical field on a video monitor obviating the need of direct physical visualization),[84] HDTV single camera 3D system (involves attachment of a high-definition display with microscope),[85] and mechanical optical rotating assembly interface (allows the clinician to work at different seating positions).[86]
CONCLUSION
Perusal of the data from the reviewed literature justifies that periodontal microsurgery seems to show promising clinical results along with an increased clinician as well as patient acceptance. As the benefits of magnification in periodontal surgical procedures are realized, its incorporation in periodontal practice at global level will become a treatment standard in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Daniel RK. Microsurgery: Through the looking glass. N Engl J Med. 1979;300:1251–7. doi: 10.1056/NEJM197905313002205. [DOI] [PubMed] [Google Scholar]
- 2.Serafin D. Microsurgery: Past, present, and future. Plast Reconstr Surg. 1980;66:781–5. [PubMed] [Google Scholar]
- 3.Apotheker H, Jako GJ. A microscope for use in dentistry. J Microsurg. 1981;3:7–10. doi: 10.1002/micr.1920030104. [DOI] [PubMed] [Google Scholar]
- 4.Shanelec DA, Tibbetts LS. Periodontal Microsurgery, Continuing Education Course, 78th American Academy of Periodontology Annual Meeting; Orlando, FL. 1992. Nov 19, [Google Scholar]
- 5.Shanelec DA, Tibbetts LS. The Status of Periodontal Microsurgery, Continuing Education Course, 79th American Academy of Periodontology Annual Meeting; Chicago. 1993. [Google Scholar]
- 6.Belcher JM. A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent. 2001;21:191–6. [PubMed] [Google Scholar]
- 7.Tibbetts LS, Shanelec D. Principles and practice of periodontal microsurgery. Int J Microdent. 2009;1:13–24. [Google Scholar]
- 8.Shanelec DA. Optical principles of loupes. J Calif Dent Assoc. 1992;20:25–32. [PubMed] [Google Scholar]
- 9.Caplan SA. Magnification in dentistry. J Esthet Dent. 1990;2:17–21. doi: 10.1111/j.1708-8240.1990.tb00598.x. [DOI] [PubMed] [Google Scholar]
- 10.Shanelec DA, Tibbetts LS. A perspective on the future of periodontal microsurgery. Periodontol 2000. 1996;11:58–64. doi: 10.1111/j.1600-0757.1996.tb00183.x. [DOI] [PubMed] [Google Scholar]
- 11.Harwell RC, Ferguson RL. Physiologic tremor and microsurgery. Microsurgery. 1983;4:187–92. doi: 10.1002/micr.1920040310. [DOI] [PubMed] [Google Scholar]
- 12.Gibbs CB. The continuous regulation of skilled response by kinaesthetic feed back. Br J Med Psychol. 1954;45:24–39. doi: 10.1111/j.2044-8295.1954.tb01223.x. [DOI] [PubMed] [Google Scholar]
- 13.Barraquer JI. The history of the microscope in ocular surgery. J Microsurg. 1980;1:288–99. doi: 10.1002/micr.1920010407. [DOI] [PubMed] [Google Scholar]
- 14.Acland R. Practice Manual for Microvascular Surgery. 2nd ed. St Louis: Mosby; 1989. [Google Scholar]
- 15.Bunke H, Chater N, Szabo Z. The Manual of Microvascular Surgery. San Francisco: Ralph K Daves Medical Centre; 1975. [Google Scholar]
- 16.Sunell S, Maschak L. Positioning for clinical dental hygiene care. Preventing back, neck and shoulder pain. Probe. 1996;30:216–9. [PubMed] [Google Scholar]
- 17.Sunell S, Rucker LM. Ergonomic risk factors associated with clinical dental hygiene practice. Probe. 2003;37:159–66. [Google Scholar]
- 18.Burkhardt R, Lang NP. Periodontal plastic microsurgery. In: Lindhe J, Lang NP, Karring T, editors. Clinical Periodontology and Implant Dentistry. 5th ed. Oxford, USA: Blackwell Munksgaard; 2008. pp. 1029–44. [Google Scholar]
- 19.Belcher JM. Periodontal microsurgery. In: Dibart S, Karima M, editors. Practical Periodontal Plastic Surgery. Oxford, USA: Blackwell Munksgaard; 2006. pp. 15–22. [Google Scholar]
- 20.Abidin MR, Dunlapp JA, Towler MA, Becker DG, Thacker JG, McGregor W, et al. Metallurgically bonded needle holder jaws. A technique to enhance needle holding security without sutural damage. Am Surg. 1990;56:643–7. [PubMed] [Google Scholar]
- 21.Thacker JG, Rodeheaver GT, Towler MA, Edlich RF. Surgical needle sharpness. Am J Surg. 1989;157:334–9. doi: 10.1016/0002-9610(89)90565-5. [DOI] [PubMed] [Google Scholar]
- 22.Gutmann JL, Harrison JW. Surgical Endodontics. Boston: Blackwell Scientific; 1991. pp. 278–99. [Google Scholar]
- 23.Rothenburger S, Spangler D, Bhende S, Burkley D. In vitro antimicrobial evaluation of coated VICRYL* plus antibacterial suture (Coated Polyglactin 910 with Triclosan) using zone of inhibition assays. Surg Infect (Larchmt) 2002;3(Suppl 1):S79–87. doi: 10.1089/sur.2002.3.s1-79. [DOI] [PubMed] [Google Scholar]
- 24.Storch M, Perry LC, Davidson JM, Ward JJ. A 28-day study of the effect of coated VICRYL* plus antibacterial suture (Coated Polyglactin 910 Suture with Triclosan) on wound healing in guinea pig linear incisional skin wounds. Surg Infect (Larchmt) 2002;3(Suppl 1):S89–98. doi: 10.1089/sur.2002.3.s1-89. [DOI] [PubMed] [Google Scholar]
- 25.Price PB. Stress, strain and sutures. Ann Surg. 1948;128:408–21. [PubMed] [Google Scholar]
- 26.Ronco V, Dard M. A novel suturing approach for tissue displacement within minimally invasive periodontal plastic surgery. Clin Case Rep. 2016;4:831–7. doi: 10.1002/ccr3.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirschfeld L, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;49:225–37. doi: 10.1902/jop.1978.49.5.225. [DOI] [PubMed] [Google Scholar]
- 28.Loos B, Nylund K, Claffey N, Egelberg J. Clinical effects of root debridement in molar and non-molar teeth. A 2-year follow-up. J Clin Periodontol. 1989;16:498–504. doi: 10.1111/j.1600-051x.1989.tb02326.x. [DOI] [PubMed] [Google Scholar]
- 29.Nordland P, Garrett S, Kiger R, Vanooteghem R, Hutchens LH, Egelberg J, et al. The effect of plaque control and root debridement in molar teeth. J Clin Periodontol. 1987;14:231–6. doi: 10.1111/j.1600-051x.1987.tb00972.x. [DOI] [PubMed] [Google Scholar]
- 30.Pihlstrom BL, Ortiz-Campos C, McHugh RB. A randomized four-years study of periodontal therapy. J Periodontol. 1981;52:227–42. doi: 10.1902/jop.1981.52.5.227. [DOI] [PubMed] [Google Scholar]
- 31.Lindhe J, Westfelt E, Nyman S, Socransky SS, Haffajee AD. Long-term effect of surgical/non-surgical treatment of periodontal disease. J Clin Periodontol. 1984;11:448–58. doi: 10.1111/j.1600-051x.1984.tb01344.x. [DOI] [PubMed] [Google Scholar]
- 32.Lindhe J, Nyman S. Long-term maintenance of patients treated for advanced periodontal disease. J Clin Periodontol. 1984;11:504–14. doi: 10.1111/j.1600-051x.1984.tb00902.x. [DOI] [PubMed] [Google Scholar]
- 33.Reinhardt RA, Johnson GK, Tussing GJ. Root planing with interdental papilla reflection and fiber optic illumination. J Periodontol. 1985;56:721–6. doi: 10.1902/jop.1985.56.12.721. [DOI] [PubMed] [Google Scholar]
- 34.Perumal MP, Ramegowda AD, Lingaraju AJ, Raja JJ. Comparison of microsurgical and conventional open flap debridement: A randomized controlled trial. J Indian Soc Periodontol. 2015;19:406–10. doi: 10.4103/0972-124X.156884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kwan JY. Enhanced periodontal debridement with the use of micro ultrasonic, periodontal endoscopy. J Calif Dent Assoc. 2005;33:241–8. [PubMed] [Google Scholar]
- 36.Mamoun J. Use of high-magnification loupes or surgical operating microscope when performing prophylaxes, scaling or root planing procedures. N Y State Dent J. 2013;79:48–52. [PubMed] [Google Scholar]
- 37.Cortellini P, Prato GP, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restorative Dent. 1999;19:589–99. [PubMed] [Google Scholar]
- 38.Takei HH, Han TJ, Carranza FA, Jr, Kenney EB, Lekovic V. Flap technique for periodontal bone implants. Papilla preservation technique. J Periodontol. 1985;56:204–10. doi: 10.1902/jop.1985.56.4.204. [DOI] [PubMed] [Google Scholar]
- 39.Cortellini P, Prato GP, Tonetti MS. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Periodontol. 1995;66:261–6. doi: 10.1902/jop.1995.66.4.261. [DOI] [PubMed] [Google Scholar]
- 40.Murphy KG. Interproximal tissue maintenance in GTR procedures: Description of a surgical technique and 1-year reentry results. Int J Periodontics Restorative Dent. 1996;16:463–77. [PubMed] [Google Scholar]
- 41.Aimetti M, Ferrarotti F, Mariani GM, Romano F. A novel flapless approach versus minimally invasive surgery in periodontal regeneration with enamel matrix derivative proteins: A 24-month randomized controlled clinical trial. Clin Oral Investig. 2017;21:327–37. doi: 10.1007/s00784-016-1795-2. [DOI] [PubMed] [Google Scholar]
- 42.Harrel SK, Rees TD. Granulation tissue removal in routine and minimally invasive procedures. Compend Contin Educ Dent. 1995;16:960, 962, 964. [PubMed] [Google Scholar]
- 43.Harrel SK, Nunn ME. Longitudinal comparison of the periodontal status of patients with moderate to severe periodontal disease receiving no treatment, non-surgical treatment, and surgical treatment utilizing individual sites for analysis. J Periodontol. 2001;72:1509–19. doi: 10.1902/jop.2001.72.11.1509. [DOI] [PubMed] [Google Scholar]
- 44.Wachtel H, Schenk G, Böhm S, Weng D, Zuhr O, Hürzeler MB, et al. Microsurgical access flap and enamel matrix derivative for the treatment of periodontal intrabony defects: A controlled clinical study. J Clin Periodontol. 2003;30:496–504. doi: 10.1034/j.1600-051x.2003.00013.x. [DOI] [PubMed] [Google Scholar]
- 45.Cortellini P, Tonetti MS. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: A novel approach to limit morbidity. J Clin Periodontol. 2007;34:87–93. doi: 10.1111/j.1600-051X.2006.01020.x. [DOI] [PubMed] [Google Scholar]
- 46.Cortellini P, Tonetti MS. Minimally invasive surgical technique and enamel matrix derivative in intrabony defects. I: Clinical outcomes and morbidity. J Clin Periodontol. 2007;34:1082–8. doi: 10.1111/j.1600-051X.2007.01144.x. [DOI] [PubMed] [Google Scholar]
- 47.Jepsen S, Topoll H, Rengers H, Heinz B, Teich M, Hoffmann T, et al. Clinical outcomes after treatment of intra-bony defects with an EMD/synthetic bone graft or EMD alone: A multicentre randomized-controlled clinical trial. J Clin Periodontol. 2008;35:420–8. doi: 10.1111/j.1600-051X.2008.01217.x. [DOI] [PubMed] [Google Scholar]
- 48.Cortellini P, Pini-Prato G, Nieri M, Tonetti MS. Minimally invasive surgical technique and enamel matrix derivative in intrabony defects: 2.Factors associated with healing outcomes. Int J Periodontics Restorative Dent. 2009;29:257–65. [PubMed] [Google Scholar]
- 49.Cortellini P, Tonetti MS. Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J Clin Periodontol. 2009;36:157–63. doi: 10.1111/j.1600-051X.2008.01352.x. [DOI] [PubMed] [Google Scholar]
- 50.Fickl S, Thalmair T, Kebschull M, Böhm S, Wachtel H. Microsurgical access flap in conjunction with enamel matrix derivative for the treatment of intra-bony defects: A controlled clinical trial. J Clin Periodontol. 2009;36:784–90. doi: 10.1111/j.1600-051X.2009.01451.x. [DOI] [PubMed] [Google Scholar]
- 51.Harrel SK, Wilson TG, Nunn ME. Prospective assessment of the use of enamel matrix proteins with minimally invasive surgery. J Periodontol. 2005;76:380–4. doi: 10.1902/jop.2005.76.3.380. [DOI] [PubMed] [Google Scholar]
- 52.Cortellini P, Nieri M, Prato GP, Tonetti MS. Single minimally invasive surgical technique with an enamel matrix derivative to treat multiple adjacent intra-bony defects: Clinical outcomes and patient morbidity. J Clin Periodontol. 2008;35:605–13. doi: 10.1111/j.1600-051X.2008.01242.x. [DOI] [PubMed] [Google Scholar]
- 53.Cortellini P, Tonetti MS. Microsurgical approach to periodontal regeneration. Initial evaluation in a case cohort. J Periodontol. 2001;72:559–69. doi: 10.1902/jop.2001.72.4.559. [DOI] [PubMed] [Google Scholar]
- 54.Cairo F, Carnevale G, Billi M, Prato GP. Fiber retention and papilla preservation technique in the treatment of infrabony defects: A microsurgical approach. Int J Periodontics Restorative Dent. 2008;28:257–63. [PubMed] [Google Scholar]
- 55.Ribeiro FV, NocitiJúnior FH, Sallum EA, Sallum AW, Casati MZ. Use of enamel matrix protein derivative with minimally invasive surgical approach in intrabony periodontal defects: Clinical and patient-centered outcomes. Braz Dent J. 2010;21:60–7. doi: 10.1590/s0103-64402010000100010. [DOI] [PubMed] [Google Scholar]
- 56.Harrel SK. A minimally invasive surgical approach for periodontal bone grafting. Int J Periodontics Restorative Dent. 1998;18:161–9. [PubMed] [Google Scholar]
- 57.Harrel SK. A minimally invasive surgical approach for periodontal regeneration: Surgical technique and observations. J Periodontol. 1999;70:1547–57. doi: 10.1902/jop.1999.70.12.1547. [DOI] [PubMed] [Google Scholar]
- 58.Harrel SK, Nunn ME, Belling CM. Long-term results of a minimally invasive surgical approach for bone grafting. J Periodontol. 1999;70:1558–63. doi: 10.1902/jop.1999.70.12.1558. [DOI] [PubMed] [Google Scholar]
- 59.Steffer MR, Harel SK, Rossmann JA, Kerns DG, Rivera-Hidalgo F, Abraham CM, et al. Comparison of minimally invasive and conventional flap surgery for treatment of intrabony periodontal defects: A pilot case controlled study. J Contemp Dent. 2013;3:61–7. [Google Scholar]
- 60.Liu S, Hu B, Zhang Y, Li W, Song J. Minimally invasive surgery combined with regenerative biomaterials in treating intra-bony defects: A meta-analysis. PLoS One. 2016;11:e0147001. doi: 10.1371/journal.pone.0147001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nibali L, Pometti D, Chen TT, Tu YK. Minimally invasive non-surgical approach for the treatment of periodontal intrabony defects: A retrospective analysis. J Clin Periodontol. 2015;42:853–9. doi: 10.1111/jcpe.12443. [DOI] [PubMed] [Google Scholar]
- 62.Aslan S, Buduneli N, Cortellini P. Entire papilla preservation technique in the regenerative treatment of deep intrabony defects: 1-year results. J Clin Periodontol. 2017;44:926–32. doi: 10.1111/jcpe.12780. [DOI] [PubMed] [Google Scholar]
- 63.Camargo PM, Melnick PR, Kenney EB. The use of free gingival grafts for aesthetic purposes. Periodontol 2000. 2001;27:72–96. doi: 10.1034/j.1600-0757.2001.027001072.x. [DOI] [PubMed] [Google Scholar]
- 64.Zuhr O, Fickl S, Wachtel H, Bolz W, Hürzeler MB. Covering of gingival recessions with a modified microsurgical tunnel technique: Case report. Int J Periodontics Restorative Dent. 2007;27:457–63. [PubMed] [Google Scholar]
- 65.Burkhardt R, Lang NP. Coverage of localized gingival recessions: Comparison of micro- and macrosurgical techniques. J Clin Periodontol. 2005;32:287–93. doi: 10.1111/j.1600-051X.2005.00660.x. [DOI] [PubMed] [Google Scholar]
- 66.Andrade PF, Grisi MF, Marcaccini AM, Fernandes PG, Reino DM, Souza SL, et al. Comparison between micro- and macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative. J Periodontol. 2010;81:1572–9. doi: 10.1902/jop.2010.100155. [DOI] [PubMed] [Google Scholar]
- 67.Francetti L, Del Fabbro M, Testori T, Weinstein RL. Periodontal microsurgery: Report of 16 cases consecutively treated by the free rotated papilla autograft technique combined with the coronally advanced flap. Int J Periodontics Restorative Dent. 2004;24:272–9. [PubMed] [Google Scholar]
- 68.Kumar A, Bains VK, Jhingran R, Srivastava R, Madan R, Rizvi I, et al. Patient-centered microsurgical management of gingival recession using coronally advanced flap with either platelet-rich fibrin or connective tissue graft: A comparative analysis. Contemp Clin Dent. 2017;8:293–304. doi: 10.4103/ccd.ccd_70_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Agarwal SK, Jhingran R, Bains VK, Srivastava R, Madan R, Rizvi I, et al. Patient-centered evaluation of microsurgical management of gingival recession using coronally advanced flap with platelet-rich fibrin or amnion membrane: A comparative analysis. Eur J Dent. 2016;10:121–33. doi: 10.4103/1305-7456.175686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nordland WP, Sandhu HS, Perio C. Microsurgical technique for augmentation of the interdental papilla: Three case reports. Int J Periodontics Restorative Dent. 2008;28:543–9. [PubMed] [Google Scholar]
- 71.Bittencourt S, Del Peloso Ribeiro E, Sallum EA, Nociti FH, Jr, Casati MZ. Surgical microscope may enhance root coverage with subepithelial connective tissue graft: A randomized-controlled clinical trial. J Periodontol. 2012;83:721–30. doi: 10.1902/jop.2011.110202. [DOI] [PubMed] [Google Scholar]
- 72.Jindal U, Pandit N, Bali D, Malik R, Gugnani S. Comparative evaluation of recession coverage with sub-epithelial connective tissue graft using macrosurgical and microsurgical approaches: A randomized split mouth study. J Indian Soc Periodontol. 2015;19:203–7. doi: 10.4103/0972-124X.148641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nizam N, Bengisu O, Sönmez Ş. Micro- and macrosurgical techniques in the coverage of gingival recession using connective tissue graft: 2 years follow-up. J Esthet Restor Dent. 2015;27:71–83. doi: 10.1111/jerd.12124. [DOI] [PubMed] [Google Scholar]
- 74.Rossi R, Pilloni A, Morales RS. Qualitative assessment of connective tissue graft with epithelial component. A microsurgical periodontal plastic surgical technique for soft tissue esthetics. Eur J Esthet Dent. 2009;4:118–28. [PubMed] [Google Scholar]
- 75.Pandey S, Mehta DS. Treatment of localized gingival recession using the free rotated papilla autograft combined with coronally advanced flap by conventional (macrosurgery) and surgery under magnification (microsurgical) technique: A comparative clinical study. J Indian Soc Periodontol. 2013;17:765–70. doi: 10.4103/0972-124X.124500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shanelec DA. Anterior esthetic implants: Microsurgical placement in extraction sockets with immediate plovisionals. J Calif Dent Assoc. 2005;33:233–40. [PubMed] [Google Scholar]
- 77.Duello GV. The use of surgical microscopes in contemporary implant therapy. Pract Proced Aesthet Dent. 2005;17:717–8. [PubMed] [Google Scholar]
- 78.Steiner GG, Steiner DM, Herbias MP, Steiner R. Minimally invasive sinus augmentation. J Oral Implantol. 2010;36:295–304. doi: 10.1563/AAID-JOI-D-09-00010. [DOI] [PubMed] [Google Scholar]
- 79.Engelke W, Schwarzwäller W, Behnsen A, Jacobs HG. Subantroscopic laterobasal sinus floor augmentation (SALSA): An up-to-5-year clinical study. Int J Oral Maxillofac Implants. 2003;18:135–43. [PubMed] [Google Scholar]
- 80.Gennaro P, Chisci G, Gabriele G, Iannetti G. Conservative surgical and microsurgical techniques for the management of dental implants that impinge on the inferior alveolar nerve. Br J Oral Maxillofac Surg. 2014;52:566–8. doi: 10.1016/j.bjoms.2014.03.026. [DOI] [PubMed] [Google Scholar]
- 81.Hegde R, Sumanth S, Padhye A. Microscope-enhanced periodontal therapy: A review and report of four cases. J Contemp Dent Pract. 2009;10:E088–96. [PubMed] [Google Scholar]
- 82.Burkhardt R, Hürzeler MB. Utilization of the surgical microscope for advanced plastic periodontal surgery. Pract Periodontics Aesthet Dent. 2000;12:171–80. [PubMed] [Google Scholar]
- 83.Cosyn J, Pollaris L, Van der Linden F, De Bruyn H. Minimally invasive single implant treatment (M.I.S.I.T.) based on ridge preservation and contour augmentation in patients with a high aesthetic risk profile: One-year results. J Clin Periodontol. 2015;42:398–405. doi: 10.1111/jcpe.12384. [DOI] [PubMed] [Google Scholar]
- 84.Franken RJ, Gupta SC, Banis JC, Jr, Thomas SV, Derr JW, Klein SA, et al. Microsurgery without a microscope: Laboratory evaluation of a three-dimensional on-screen microsurgery system. Microsurgery. 1995;16:746–51. doi: 10.1002/micr.1920161109. [DOI] [PubMed] [Google Scholar]
- 85.Ryo M, Schigeaki K. HDTV single camera 3D system and its application in microsurgery. Stereoscopic displays and virtual reality systems. Proc SPIE. 2001;2177:31–4. [Google Scholar]
- 86.Doornbusch H, Veenstra K. The microscope in dentistry. Editorial. Germany: Carl Zeiss Surgical GmbH; 2007. Frequently asked questions about the dental microscope. [Google Scholar]


