Abstract
Several surgical techniques including pedicle flaps and free soft-tissue grafts have been indicated for the treatment of gingival recession defects with different success rates. Localized gingival recessions can be managed with various root coverage procedures, more specifically, using the coronally advanced flap with distinct designs. Predictable and consistent periodontal plastic surgical results can be achieved by using microsurgical instruments. Periodontal microsurgery involves the use of magnifying devices, microsurgical instruments, and materials in existing basic surgical techniques. It offers definitive advantages in terms of predictability, postoperative morbidity, and patient approval. This case report aims at comparing the modified approach with a triangular type of coronally advanced flap, using conventional and microsurgical approach, for treating bilateral isolated Miller's class I defect in both the maxillary canines by a split-mouth design.
Key words: Coronally advanced flap, gingival recession, periodontal microsurgery, root coverage
INTRODUCTION
Over the past few decades, a myriad of surgical techniques that include pedicle and free soft-tissue grafting techniques have been introduced to correct recession defects. These techniques have exhibited varying degrees of success owing to the selection of the appropriate technique. Coronally advanced flap (CAF) is a suitable technique that produces good results in treating gingival recession with adequate apical keratinized tissue. Some of the pioneers who have proposed different CAF techniques are Allen, Miller, Zucchelli, and De Sanctis. In the technique as demonstrated by Allen and Miller,[1] the starting point of the lateral incisions were not indicated precisely. Subsequently, de Sanctis and Zucchelli introduced the trapezoidal CAF that resulted in adequate root coverage in many cases.[2] Relatively recently, Zucchelli et al. described a modified CAF with a triangular design and compared its effectiveness with the trapezoidal CAF.[3]
In addition to obtaining complete root coverage, the clinician should be mindful of performing the surgery as minimally invasive as possible. This can be achieved by periodontal microsurgery that employs the use of magnifying devices and microsurgical instruments. Certain approaches such as the tunnel technique,[4] laterally moved, CAF,[5] and other mucogingival surgical techniques have been evaluated using microsurgery.[6] However, the comparison of triangular CAF design with and without the microsurgical approach is not yet known in literature.
Therefore, this case report presents bilateral Miller's class I recession defects in maxillary canines treated with a triangular CAF using the conventional and microsurgical approach.
CASE REPORT
A 30-year-old male patient with no relevant medical history reported to the Department of Periodontology with a chief complaint of sensitivity in the right and left upper front tooth region for the past 2 months. On clinical examination, Miller's class I recession in both the maxillary canines was noted [Figures 1 and 2]. A thorough case history was taken, and the periodontal parameters such as probing depth, recession depth, clinical attachment level, and height of keratinized gingiva were recorded. An informed consent and routine blood investigation reports were obtained from the patient. Scaling and root planing was performed 1-week before the surgical procedure.
Figure 1.

Preoperative clinical view of 23
Figure 2.

Preoperative clinical view of 13
Surgical procedure
Conventional (macrosurgical approach)
The aseptic surgical protocol was maintained throughout the surgical procedure. Before the surgery, extraoral disinfection with Povidone-Iodine solution and intraoral disinfection was performed using 0.2% chlorhexidine solution. The maxillary left canine region was anesthetized using buccal infiltration containing 2% Lidocaine and 1:80,000 adrenaline.
An orthodontic wire was placed along the cementoenamel junction (CEJ), and the tip of the interdental papillae on either side of the canine was marked on the wire [Figure 3]. The wire was then moved apically along the gingival margin and the corresponding papillae tip points were marked to ascertain the starting point of the two oblique incisions [Figure 4]. The incisions were drawn parallel to the mesial and distal incline of mesial and distal papillae, respectively and were extended surpassing the mucogingival junction (MGJ). After adequate anesthesia was obtained, using a 15-blade, the oblique incisions were given followed by the sulcular incision. A full-thickness mucoperiosteal flap was then elevated up to the MGJ followed by a split-thickness flap to liberate muscle tension and enable passive coronal displacement of the triangular flap. De-epithelization of the interdental papilla was done sequentially [Figure 5].
Figure 3.

Orthodontic wire placed along the cementoenamel junction and tip of papillae marked (23)
Figure 4.

Orthodontic wire moved to the gingival margin and oblique incisions marked (23)
Figure 5.

Flap elevation with de-epithelization of interdental papillae (23)
The flap was then coronally repositioned over the exposed root surface to achieve the desired root coverage and was sutured using 4-0 Mersilk suture (Ethicon) [Figure 6]. Periodontal dressing was given over the treated site, and the patient was informed not to brush the surgical site until the sutures were removed. Amoxicillin 500 mg 3 times a day for 5 days and analgesic (aceclofenac 100 mg + paracetamol 500 mg) 2 times a day for 3 days was prescribed. The patient was recalled 1 week after the surgical procedure and the sutures were removed [Figure 7]. Adequate healing was noted.
Figure 6.

Flap coronally advanced and sutured (23)
Figure 7.

One-week postoperative: Sutures removed (23)
Microsurgical approach
A week after the conventional procedure following suture removal, the microsurgical approach was performed in relation to the maxillary right canine using microsurgical loupes under 2.3x magnification, microsurgical instruments (scalpel, tweezer, elevator, needle holder, and scissors), and 6-0 Ethilon (Ethicon) suture material.
The surgical procedure was performed using the technique as previously mentioned [Figures 8 and 9]. The microsurgical approach provided enhanced visual acuity of the surgical field, better illumination and with the aid of microsurgical instruments, the incisions, flap design and elevation were more precise. After the surgical procedure, postoperative instructions were given. The patient was recalled one week later and the sutures were removed [Figure 10]. Follow-up was done for both the treated canines at 1 month and 6 months after the surgical procedure [Figures 11–14].
Figure 8.

Flap elevation with de-epithelization of interdental papillae (13)
Figure 9.

Flap coronally advanced and sutured (13)
Figure 10.

One-week postoperative: Sutures removed (13)
Figure 11.

One-month postoperative clinical view (13)
Figure 14.

Six months postoperative clinical view (23)
Figure 12.

Six months postoperative clinical view (13)
Figure 13.

One month postoperative clinical view (23)
Outcome
After surgery, the clinical parameters were evaluated at 1 month and 6 months. Similar results were noted at both intervals [Tables 1 and 2]. By the 6th month, complete root coverage was acquired in both the procedures. The recession depth was reduced from 3 mm at baseline to 1 mm at 1 month and 0 mm at 6th month in both the surgical sites postoperatively. The probing depth remained the same, and there was a gain in the CAL in both the canines. There was also an increase in the height of keratinized gingiva. Good color match and no scar formation were evident. The patient was satisfied with the esthetics and a drastic reduction in sensitivity was obtained after both the procedures.
Table 1.
Conventional approach in 23: Clinical parameters at baseline, 1 month and 6 months
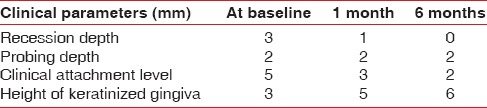
Table 2.
Microsurgical approach in 13: Clinical parameters at baseline, 1 month and 6 months

DISCUSSION
Over the years, quite a few CAF techniques have been substantiated to treat recession defects. One such technique is the triangular CAF that was described in comparison with the trapezoidal CAF. In the triangular CAF, the rotation of the papillae is towards the periphery to reach the tip of the corresponding papillae, whereas in the trapezoidal CAF, the papillae simply move in a coronal direction.[3] The use of an orthodontic wire in the triangular CAF technique, helps in precisely denoting the initial point of the oblique incisions. In addition, the triangular CAF offers precise soft-tissue adaptation, better color match and contiguity. However, the drawback of this design is the need to dissect the triangular papillae and the technical difficulty during suturing with the possibility of placing the suture material into the sulcus.[3]
Various mucogingival surgical techniques have been assessed using microsurgery but as far as we know, this is the first report to compare the triangular CAF design with and without microsurgical approach. This case report showed similar results with respect to the depth of gingival recession, probing pocket depth, clinical attachment level, and height of keratinized gingiva. Significant reduction was noted in the recession depth with a gain in the height of keratinized gingiva in both the procedures. Zucchelli et al., in 2016 also compared the triangular design with the trapezoidal design in CAF procedures and found similar results with regard to root coverage and contiguity.[3] It is observed that root coverage may also occur as a result of creeping attachment which is described as the postoperative migration of the gingival marginal tissue in the coronal direction on the already denuded root surface. This can be observed from 1 to 12 months after the root coverage procedure and is noted to be 1 mm approximately. Even though the creeping attachment seems to occur, the root coverage is still achieved. Well-designed surgical technique, patient's proper maintenance, and long-term follow-up are few factors that enhance the predictability of root coverage despite the creeping attachment.[7]
The application of periodontal microsurgical instruments has been proven in effectively treating gingival recession by increasing the predictability of root coverage procedures with a minimally invasive approach.[8,9,10] The distinct advantages of periodontal microsurgery include illumination, magnification, and increased precision. This also facilitates minimal postoperative discomfort and favors rapid healing with greater esthetic satisfaction. Nonetheless, microsurgical procedures are time consuming, expensive and involve a greater degree of manual dexterity, which are the most common setbacks that clinicians encounter.
CONCLUSION
The present case report shows similar results in both, conventional and microsurgical approach with optimal color match and precise flap proximity. However, the microsurgical approach showed better view of the surgical field with more accuracy during the surgery and less postoperative patient discomfort. Furthermore, extensive and long-term studies are required to elucidate the effects of microsurgical approach with the triangular CAF technique to prove its efficacy in treating isolated recession defects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Allen EP, Miller PD., Jr Coronal positioning of existing gingiva: Short term results in the treatment of shallow marginal tissue recession. J Periodontol. 1989;60:316–9. doi: 10.1902/jop.1989.60.6.316. [DOI] [PubMed] [Google Scholar]
- 2.de Sanctis M, Zucchelli G. Coronally advanced flap: A modified surgical approach for isolated recession-type defects: Three-year results. J Clin Periodontol. 2007;34:262–8. doi: 10.1111/j.1600-051X.2006.01039.x. [DOI] [PubMed] [Google Scholar]
- 3.Zucchelli G, Stefanini M, Ganz S, Mazzotti C, Mounssif I, Marzadori M, et al. Coronally advanced flap with different designs in the treatment of gingival recession: A Comparative controlled randomized clinical trial. Int J Periodontics Restorative Dent. 2016;36:319–27. doi: 10.11607/prd.2698. [DOI] [PubMed] [Google Scholar]
- 4.Zuhr O, Fickl S, Wachtel H, Bolz W, Hürzeler MB. Covering of gingival recessions with a modified microsurgical tunnel technique: Case report. Int J Periodontics Restorative Dent. 2007;27:457–63. [PubMed] [Google Scholar]
- 5.Ucak O, Ozcan M, Seydaoglu G, Haytac MC. Microsurgical instruments in laterally moved, coronally advanced flap for miller class III isolated recession defects: A Randomized controlled clinical trial. Int J Periodontics Restorative Dent. 2017;37:109–15. doi: 10.11607/prd.2547. [DOI] [PubMed] [Google Scholar]
- 6.Francetti L, Del Fabbro M, Calace S, Testori T, Weinstein RL. Microsurgical treatment of gingival recession: A controlled clinical study. Int J Periodontics Restorative Dent. 2005;25:181–8. [PubMed] [Google Scholar]
- 7.Otero-Cagide FJ, Otero-Cagide MF. Unique creeping attachment after autogenous gingival grafting: Case report. J Can Dent Assoc. 2003;69:432–5. [PubMed] [Google Scholar]
- 8.Shanelec DA, Tibbetts LS. Periodontal microsurgery. Periodontal Insights. 1994;1:4–7. [PubMed] [Google Scholar]
- 9.Cairo F, Carnevale G, Billi M, Prato GP. Fiber retention and papilla preservation technique in the treatment of infrabony defects: A microsurgical approach. Int J Periodontics Restorative Dent. 2008;28:257–63. [PubMed] [Google Scholar]
- 10.Andrade PF, Grisi MF, Marcaccini AM, Fernandes PG, Reino DM, Souza SL, et al. Comparison between micro- and macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative. J Periodontol. 2010;81:1572–9. doi: 10.1902/jop.2010.100155. [DOI] [PubMed] [Google Scholar]


