Abstract
Background:
Opioid prescription drug abuse is a major public health concern. Healthcare provider prescribing patterns, especially among non–pain management specialists, are a major factor. Practice guidelines recommend what to do for safe opioid prescribing but do not provide guidance on how to implement best practices.
Methods:
We describe the implementation of electronic medical record clinical decision support (EMR CDS) for opioid management of chronic noncancer pain in an integrated delivery system. This prospective cohort study will examine relationships between primary care physician compliance with EMR CDS–guided care (vs usual care), delivery of guideline-concordant care, and changes in the morphine equivalent of prescribed opioids. We report baseline characteristics of patients receiving chronic opioid therapy and organizational prescribing trends.
Results:
Between August and October 2016, we identified 2,759 primary care patients who received chronic opioid therapy. Of these patients, approximately 71% had chronic noncancer pain, and 62% had diagnoses of depression/anxiety. Six of 36 primary care clinics each had >100 patients receiving chronic opioid therapy. When the EMR CDS launched in October 2017, we identified 54,200 patients who had received opioid therapy for at least 14 days from various specialty and primary care providers during the prior 24 months. Of these patients, 36% had a benzodiazepine coprescription, and 13% had substance abuse diagnoses.
Conclusion:
Health system research that examines workflow-focused strategies to improve physician knowledge and skills for safely managing opioid therapy is needed. If EMR CDS proves to be effective in increasing adherence to practice guidelines, this EMR strategy can potentially be replicated and scaled up nationwide to improve population health management.
Keywords: Analgesics–opioid, chronic pain, decision support system–clinical, electronic medical records, primary health care
INTRODUCTION
Chronic pain affects more than 100 million adults in the United States, and approximately 20% of outpatient visits are for nonmalignant pain.1 Efforts to improve identification and management of chronic pain and associated disabilities have coincided with a sharp increase in opioid overprescribing, misuse, and abuse.1,2 Between 2000 and 2010, opioid prescription rates doubled from 11.3% to 19.6%.1 Primary care providers account for nearly half of all opioid prescriptions dispensed.3 Fatal drug poisonings now exceed the rate of motor vehicle mortalities, and overdose mortality rates attributable to prescription opioids surpass those from cocaine and heroin.4 Concomitantly, medical expenditures have increased. Opioid abusers are more likely to use medical services at rates exceeding nonabusers for inpatient hospitalizations, emergency department use, and mental health outpatient visits.5
In 2016, the Centers for Disease Control and Prevention (CDC) released an evidence-based practice guideline to help providers identify risky opioid user behaviors, heighten provider awareness of prescribing practices, and promote the use of risk mitigation strategies.6 Nonpharmacologic and nonopioid therapy is the preferred treatment option for chronic noncancer pain. Opioids should only be used when the benefits for pain and function outweigh the risks. Providers should establish realistic treatment goals for pain and function and monitor for recovery; prescribe immediate-release opioids instead of long-acting opioids; prescribe the lowest effective dose; assess the benefits and risks of doses >50 morphine equivalent daily dose (MEDD); and reevaluate the benefits and harms of opioid therapy every 3 months or more frequently. Providers should also conduct periodic assessments of risks for aberrant behavior and incorporate mitigation strategies into the management plan; review state prescription drug monitoring program data when available; perform urine drug testing at least annually; and avoid coprescribing benzodiazepines. Finally, patients with opioid use disorder should be referred to evidence-based treatment programs (eg, Suboxone therapy for addiction). Even though the CDC practice guideline provides recommendations on what to do to safely prescribe opioids, it does not provide guidance on how to translate the recommendations into practice.
Clinical decision support (CDS) tools built in the electronic medical record (EMR) and developed around the guideline can potentially bring prescribers into compliance with new practice recommendations. The primary objective of this research methods paper is to describe the implementation and planned evaluation of EMR CDS for opioid management of chronic noncancer pain within the Ochsner Health System. Ochsner's EMR CDS was designed to help identify patients who are at risk for opioid misuse/abuse, employ mitigation strategies to prevent progression, and refer patients to specialty care in a timely manner in accordance with the CDC practice guideline. Our prospective cohort study will examine whether primary care provider compliance with completion of an opioid risk assessment tool (1) reduces the average total dose of opioid medication prescribed (MEDD in milligrams) and/or (2) increases the rate at which patients receive CDC guideline-concordant care.
METHODS
Study Design, Setting, and Participants
In this prospective observational cohort study, the intervention (described below) targets primary care providers (internal medicine or family medicine) who are practicing in 36 clinic locations within 5 geographic regions of the Ochsner Health System, the largest integrated delivery system in Louisiana. Patients will be included in the data analysis if they meet the following inclusion criteria: are age ≥18 years, have a primary care provider at any of the study clinics, received opioid prescriptions for 3 of the last 4 months, and have no active diagnosis of cancer on their problem list. Patient exclusion criteria include being <18 years, having an active cancer diagnosis, undergoing cancer treatment, having a terminal illness, or receiving hospice care. The Ochsner Institutional Review Board approved this study.
Opioid Stewardship Initiative
In 2016, Ochsner's Chief Quality Officer formed an Opioid Stewardship Workgroup to lead local efforts to address the opioid prescription crisis. The workgroup was charged with using data to raise provider awareness of the problem, developing strategies to promote responsible use of opioids for treatment of chronic noncancer pain, and developing infrastructure for opioid treatment and recovery. The workgroup is composed of physicians from a variety of specialties (eg, primary care, emergency medicine, hospital medicine, and psychiatry) and health system stakeholders representing pharmacy, nursing, clinical information systems (Epic EMR system analysts), and operations management. All system-level opioid stewardship planning, implementation of strategy design, data monitoring, and progress evaluation occur via this workgroup.
Intervention
The EMR CDS is embedded in the Epic Healthy Planet patient registry tool and is congruent with population health maintenance workflow strategies already employed by Ochsner primary care. From April to June 2017, EMR workflows were test piloted in one region of the health system, modified, and subsequently launched systemwide in October 2017.
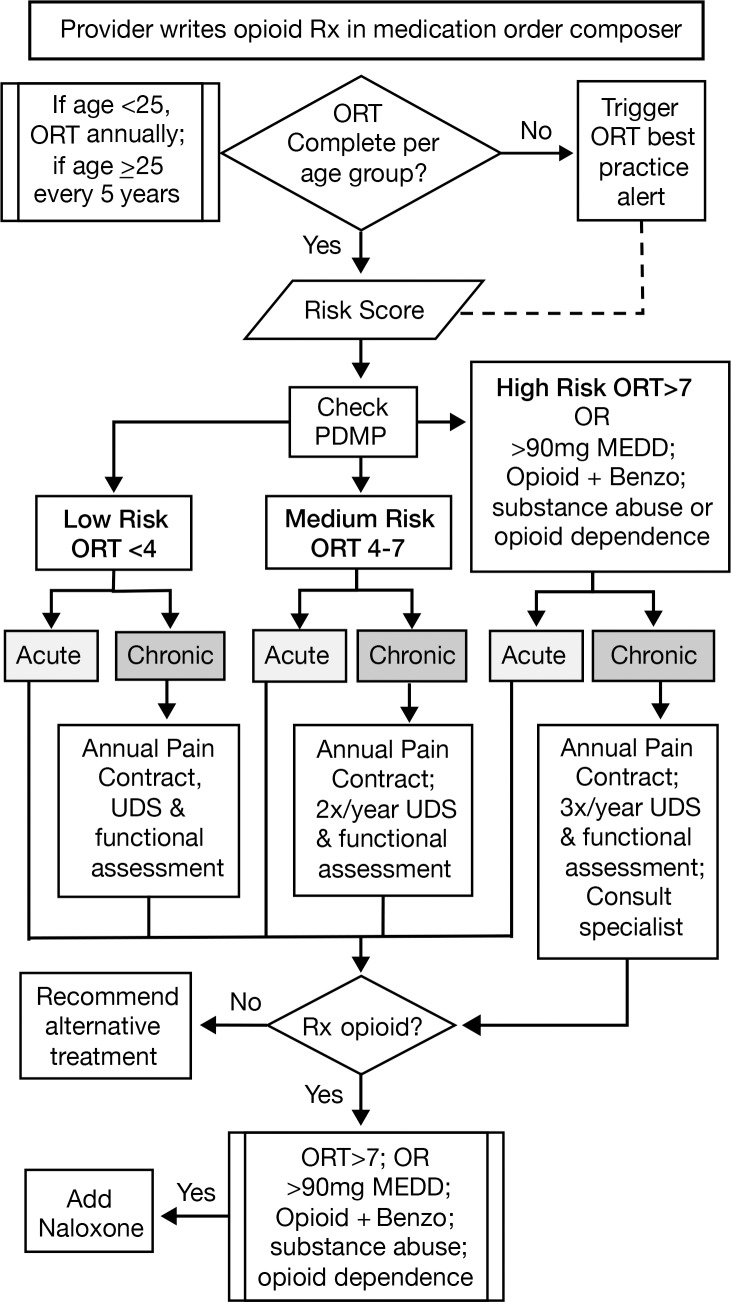
As detailed in Figure 1, providers are prompted to complete the Opioid Risk Tool (ORT) when prescribing opioids if not already documented and up to date according to the patient's age (annually if age <25 years or every 5 years if age ≥25 years). This prompt, however, is not a hard stop in the workflow. The ORT measures the presence/absence of risk factors associated with substance abuse: age, personal and family history of substance abuse, history of preadolescent sexual abuse, and certain psychological conditions. Each questionnaire item has a weighted score. The total ORT score ranges 0-13 for men and 0-16 for women. The score identifies a patient's risk of displaying opioid-aberrant behavior as low (0-3), medium (4-7), or high (>7).7 Additionally, patients who are identified as having at least one of the following conditions are automatically flagged as high risk: (1) coprescriptions for opioids and benzodiazepines, (2) a MEDD >90 mg, or (3) active diagnosis of substance abuse in the last 12 months.
Figure 1.
Opioid prescribing workflow in the electronic medical record. When providers write a prescription for opioid medications, they receive an alert to complete the Opioid Risk Tool (ORT) if not already done according the patient's age group. The ORT score stratifies patients into 3 categories of risk for opioid-aberrant behavior (low, medium, high). The rule engine for the chronic opioid registry then determines the recommended frequency of documenting best practices for safe management (eg, the annual pain contract and functional assessment). The recommended functional assessment includes at a minimum the Pain, Enjoyment, General Activity (PEG) 3-item pain scale and the 4-item Patient Health Questionnaire for Depression and Anxiety (PHQ-4). The chronic opioid health maintenance tool displays if high-risk patients have an active medication order for naloxone. This workflow does not apply to acute pain management. Benzo, benzodiazepines; MEDD, morphine equivalent daily dose; ORT, opioid risk tool; PDMP, prescription drug monitoring program; Rx, prescription; UDS, urine drug screen.
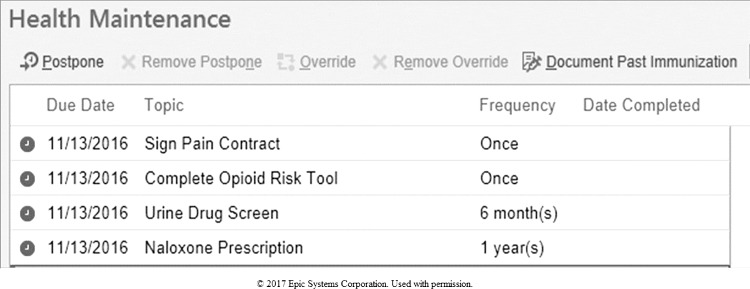
The health maintenance tool displays whether patients are up to date on chronic opioid management best practices based on the ORT-derived risk stratification (eg, documentation of pain management agreement, frequency of urine drug screening/monitoring, naloxone on active medication list). Figure 2 shows a sample display of the health maintenance schedule generated by the patient registry rule engines. Patients who do not have an ORT score documented are automatically classified as unknown risk, and their health maintenance only indicates that the completion of the ORT and pain agreement are overdue. The recommended functional assessment includes at a minimum the Pain, Enjoyment, General Activity (PEG) 3-item pain scale and the 4-item Patient Health Questionnaire for Depression and Anxiety (PHQ-4). We selected these questionnaires because they are short and easy to administer in a busy clinic setting. Patient responses to questionnaire items are documented via the Epic flowsheet tool to facilitate capturing this information as structured data.
Figure 2.
Chronic opioid registry health maintenance tool. The health maintenance tool displays if patients are up to date on chronic opioid management best practices (eg, documentation of pain management agreement, frequency of urine drug screening/monitoring, naloxone on active medication list) based on the Opioid Risk Tool–derived risk stratification described in Figure 1.
The PEG is derived from the Brief Pain Inventory.8,9 It has internal reliability, construct validity, and responsiveness among primary care patients. Each item of the PEG is scaled 0-10, with the final score being the average of the 3 individual item scores. A decrease in score over time with the initiation of therapy is considered to indicate a response to treatment.
The high prevalence of comorbid psychiatric disorders among patients with chronic noncancer pain is well documented.10-12 The PHQ-4 consists of a 2-item measure of depression and a 2-item measure of anxiety.13 The scale has internal reliability, construct validity, and factorial validity. The score indicates normal (0-2), mild (3-5), moderate (6-8), or severe symptoms (9-12). Increasing scores are associated with multiple domains of functional impairment and have a strong dose-response relationship with disability days and physician visits. The PHQ-4 is not diagnostic, and further inquiry to establish the presence of a mental disorder is warranted. If the PHQ-4 score is ≥3, documentation of the PHQ-914 and 7-item Generalized Anxiety Disorder (GAD-7) questionnaire15-17 is recommended for detailed screening and subsequent monitoring of symptoms if a formal diagnosis is made.
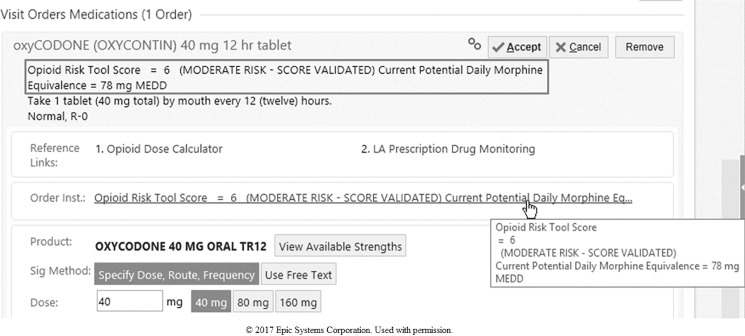
The EMR CDS is designed to minimize the number of clicks needed to access the data required for guideline-concordant care. For example, the ORT score, MEDD of the opioid dose prescribed, and hyperlinks to the Louisiana Board of Pharmacy Prescription Monitoring Program data and pain management agreement (if completed) are visible in the medication order composer (Figure 3). An Epic banner appears in the charts of patients with medium to high risk for opioid misuse/abuse to alert other providers of existing opioid pain management agreements, to limit opioid prescription writing, and to encourage redirection of patients back to their prescribing providers for management. The banner is also a quick link to the opioid management health maintenance tool.
Figure 3.
Medication dosing support in the electronic medical record prescription writer. The Opioid Risk Tool score, morphine equivalent daily dose (MEDD) of the opioid prescribed, and hyperlinks to the Louisiana Board of Pharmacy Prescription Monitoring Program and pain management agreement (if completed) are visible in the medication order composer for ease of accessing this information within the established medication order workflow.
The EMR health maintenance tool contains an information link to the health system's chronic opioid management guide. The guide contains hyperlinks to the following documents for quick referencing: (1) Ochsner pain management agreement, (2) CDC guideline fact sheet, (3) Ochsner opioid management clinical assessment recommendations, (4) ORT overview, (5) CDC fact sheet on nonopioid therapies, (6) CDC fact sheet on interpreting the MEDD, (7) office-based urine drug screening, (8) CDC fact sheet on pharmacy drug monitoring programs, and (9) CDC fact sheet on opioid-tapering strategies.
Outcome Measures
The main study outcomes are changes in the average MEDD and percentage of patients with a MEDD >90 mg. Secondary outcomes include changes in the rates of completion of guideline-concordant care as measured by the proportion of patients with documentation of a validated ORT score, urine drug screening test orders and results, pain contract, pain assessment and monitoring (PEG 3-item pain scale), and screening for depression/anxiety (PHQ-4), as well as rates of prescribing nonopioid medications and specialty consults for pain management (orthopedics, rheumatology, physical medicine and rehabilitation, physical/occupational therapy, psychiatry, psychology, addiction services, functional restoration services). All outcomes data will be extracted from Ochsner's enterprise data warehouse. Covariates of interest will include provider characteristics (age, sex, race/ethnicity, specialty, level of training, years in practice, and clinic location) and patient characteristics (age, sex, race/ethnicity, insurance, marital status, ZIP code, number of comorbidities, and presence of a mental health condition).
Data Analysis
Baseline Opioid Prescribing Trends
In this baseline methods paper, we use descriptive statistics to examine the characteristics of primary care patients receiving chronic opioid therapy for noncancer pain, as well as baseline organizational trends in opioid prescribing patterns prior to launching the EMR CDS.
Planned Statistical Analysis
The primary groups considered for comparison in the statistical analyses of the study data collected prospectively will be patients on chronic opioid therapy for noncancer pain with a validated ORT score vs patients who do not have documentation of an ORT score. This study's main hypothesis is that a higher proportion of patients with an ORT score will have a lower total average MEDD for opioids prescribed and higher rates of signed pain management agreements, urine drug screens, depression/anxiety screening, pain assessments, nonopioid pain medications, and referrals to specialty care as part of the care plan.
For the primary outcome, the differences in opioid dosing will be compared between ORT screening groups. The 2 primary endpoints are a binary indicator of daily dosage above or below MEDD 90 mg and a continuous measure of MEDD. Using a 2-sample t test with a coefficient of variation of 0.5, 80% power to detect a 10% difference in mean prevalence of MEDD ≥90 mg between the 2 study groups will be achieved with a sample size of 2,640. This sample size was adjusted via an inflation factor for expected intraclass correlation of 0.015 among patients within clusters of 5 health system geographic hospital regions. The nonparametric Wilcoxon rank sum test will be used if the distribution of the residuals does not meet the necessary normality assumption. Association of ORT screening group with the proportion of patients prescribed MEDD ≥90 mg will be assessed using a chi-square test or Fisher exact test. Daily opioid dosage will be modeled using a general linear model and least squares means will be compared between study groups via a 2-sample t test.
For secondary outcomes, assessment of receipt of care will be carried out via logistic regression modeling. Separate models will be constructed with the response in each being a binary indicator of administration of a particular component of the guidelines for chronic opioid management. Estimated odds ratios based on the probability of having each component of the guideline administered will be compared between ORT screening groups.
For evaluation of all study aims, model-based analyses will be adjusted for patient-level propensity scores as covariates. To account for patient-level differences that may exist between study groups because of the observational nature of the study, propensity scores will be calculated based on a group of factors related to both patients and their providers that are determined to be influential on ORT screening group membership. A logistic regression model with the response indicating completion of ORT screening will be fit with a pool of predictors made up of patient and provider characteristics. Type 3 tests of the partial effects of each predictor after adjusting for all other predictors will be examined. Additionally, exploratory factor analysis will be carried out on the same group of selected characteristics to attempt to identify unobserved latent variables that may explain collections of patient and/or provider characteristics. These factors will then be used as explanatory variables in a logistic regression model to predict ORT screening completion. The propensity scores will be used in the final analyses to help reduce the effect of selection bias. All analyses will be conducted using SAS/STAT software, v.9.4 of the SAS System for Windows.
RESULTS
Between August and October 2016, the authors (members of the Ochsner Health System Opioid Stewardship Workgroup) reviewed chronic opioid prescription patterns in 36 primary care clinics prior to launching the EMR CDS tools. We identified 2,759 primary care patients (1% of the 250,000 patients served) who received chronic opioid therapy within this 120-day period. Approximately 71% of these patients had chronic noncancer pain, 62% had active diagnoses of depression/anxiety disorders, 56% had Medicare coverage, and 37% were ≥65 years. We further observed that 6 clinics (located in 5 different geographic regions) each had >100 patients receiving chronic opioid therapy in contrast to all other sites.
When the health maintenance registry went live in October 2017, 54,200 unique patients were identified across the entire health system as having received opioid therapy for at least 14 days during the prior 24 months. Eleven percent (n=5,962) of these patients did not have a documented ambulatory visit within the prior 2 years. Thirty-six percent of patients on the registry had a benzodiazepine coprescription on the active medication list, and 13% had an active diagnosis of substance abuse on their problem list. Less than 3% of patients on chronic opioid therapy with a coprescription for benzodiazepines or comorbid substance abuse were prescribed naloxone.
DISCUSSION
This study's preliminary findings substantiate the need for CDS at the point of care to enhance safe opioid care management. The high prevalence of comorbid depression/anxiety among primary care patients and the rates of coprescriptions for benzodiazepines and active substance abuse among the general population highlight the mental and behavioral health complexity of the population served. The importance of increasing provider awareness and providing continuous medical education about safe opioid prescribing practices is also evident.
Integrating structured opioid management strategies across the health system was the logical next step. The CDC practice guideline provides an evidence-based framework by which to do so. Improving provider awareness/familiarity with practice recommendations while enhancing self-efficacy and motivation is a prerequisite to behavior change.18 Practice guidelines that are evidence-based, plausible, goal-oriented, user-friendly and easily accessed at the point of care are likely to be adopted quickly. Organization-level use of computerized decision support systems, reminders, and standing orders and standardization of processes, procedures, and protocols within the context of quality management also improve practice adherence.
Implementation of CDS can easily fail to achieve desired outcomes if not designed well. The five rights of clinical decision support state that the intervention must deliver the right information, to the right person, in the right format, through the right channel, at the right point in the workflow.19 The right information must be evidence-based and pertinent to the provider, patient, and/or circumstance at hand. The intervention must target specific members of the care team for whom certain data are most meaningful. CDS must also be configured and deployed in such a way to align with established workflows while minimizing alert fatigue. Ochsner Health System aligned its EMR CDS with the population health management workflow currently used in its primary care clinics. Success of the decision support tools depends on providers (1) responding to prompts to complete the ORT when prescribing opioids and (2) prioritizing completion of overdue health maintenance items for chronic opioid therapy (eg, urine drug screen) just as they would for other preventive health and chronic disease management measures (eg, hemoglobin A1c for monitoring diabetes).
The mere presence of CDS within the workflow does not mean providers will automatically understand its relevance to clinical practice. Therefore, several strategies for ongoing provider education have been launched simultaneously. Ochsner's Chief Medical Information Officer (coauthor T.B.) conducts lunchtime webinars to review optimal workflows in the EMR with physicians across the entire system. The Opioid Stewardship Workgroup's lead physician (coauthor W.R.) reviews the same information with system primary care leadership. Members of the Opioid Stewardship Workgroup also disseminate information via a series of continuing education lectures.
We recognize that this prospective observational study will have several limitations. First, observational studies are limited by the inherent bias and confounding of results that routinely occur in nonrandomized studies. To minimize threats to internal validity, we provided a priori specification of research questions, targeted a specific patient population, and selected a study design that was appropriate to the study question; selected the appropriate data source; and provided transparency in protocol development. Second, electronic databases contain information collected for operational reasons rather than research purposes and therefore have minimal reporting bias. However, data quality (eg, missing/incomplete data), selection bias, and unmeasured confounding inherent to data collected in clinical practice are major threats to internal validity. Accordingly, we will employ analytic methods (eg, regression, propensity scores) to minimize threats to internal validity.
CONCLUSION
Health system research that examines workflow-focused strategies to improve primary care physicians' knowledge and skills for managing chronic noncancer pain and to change opioid prescribing behavior are needed. Primary care practices desperately need feasible ways to monitor opioid safety (adverse effects and toxicities), efficacy (physical and emotional functioning), and misuse throughout the course of treatment without increasing workloads. Standardized workflow redesigns employed among practices of varying sizes, patient mix, and geographic locations would help healthcare organizations across the country know whether an EMR-based intervention is sufficient to influence opioid prescribing patterns. If this study proves the intervention to be effective in increasing provider adherence to the practice guideline, this EMR strategy has immense potential for being replicated and scaled up across a variety of practice settings nationwide to improve population health management.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
The authors wish to thank Epic analysts of the Ochsner Health System Information Systems Department for programming the clinical decision support tools and staff members of the Center for Applied Health Services Research for their contributions to data management.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Systems-Based Practice, and Practice-Based Learning and Improvement.
REFERENCES
- 1. Daubresse M., Chang HY., Yu Y., et al. Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000-2010. Med Care. 2013. October; 51 10: 870- 878. 10.1097/MLR.0b013e3182a95d86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Quality improvement guidelines for the treatment of acute pain and cancer pain. American Pain Society Quality of Care Committee. JAMA. 1995. December 20; 274 23: 1874- 1880. [DOI] [PubMed] [Google Scholar]
- 3. Manchikanti L., Abdi S., Atluri S., et al. American Society of Interventional Pain Physicians. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: part 2—guidance. Pain Physician. 2012. July; 15 3 Suppl: S67- S116. [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States 1999-2008. MMWR Morb Mortal Wkly Rep. 2011. November 4; 60 43: 1487- 1492. [PubMed] [Google Scholar]
- 5. Meyer R., Patel AM., Rattana SK., Quock TP., Mody SH. Prescription opioid abuse: a literature review of the clinical and economic burden in the United States. Popul Health Manag. 2014. December; 17 6: 372- 387. 10.1089/pop.2013.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dowell D., Haegerich TM. Using the CDC guideline and tools for opioid prescribing in patients with chronic pain. Am Fam Physician. 2016. June 15; 93 12: 970- 972. [PMC free article] [PubMed] [Google Scholar]
- 7. Webster LR., Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med. 2005. Nov-Dec; 6 6: 432- 442. [DOI] [PubMed] [Google Scholar]
- 8. Krebs EE., Bair MJ., Damush TM., Tu W., Wu J., Kroenke K. Comparative responsiveness of pain outcome measures among primary care patients with musculoskeletal pain. Med Care. 2010. November; 48 11: 1007- 1014. 10.1097/MLR.0b013e3181eaf835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tan G., Jensen MP., Thornby JI., Shanti BF. Validation of the brief pain inventory for chronic nonmalignant pain. J Pain. 2004. March; 5 2: 133- 137. [DOI] [PubMed] [Google Scholar]
- 10. Grattan A., Sullivan MD., Saunders KW., Campbell CI., Von Korff MR. Depression and prescription opioid misuse among chronic opioid therapy recipients with no history of substance abuse. Ann Fam Med. 2012. Jul-Aug; 10 4: 304- 311. 10.1370/afm.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Howe CQ., Sullivan MD., Saunders KW., et al. Depression and ambivalence toward chronic opioid therapy for chronic noncancer pain. Clin J Pain. 2012. September; 28 7: 561- 566. 10.1097/AJP.0b013e31823ade59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Merrill JO., Von Korff M., Banta-Green CJ., et al. Prescribed opioid difficulties, depression and opioid dose among chronic opioid therapy patients. Gen Hosp Psychiatry. 2012. Nov-Dec; 34 6: 581- 587. 10.1016/j.genhosppsych.2012.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kroenke K., Spitzer RL., Williams JB., Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009. Nov-Dec; 50 6: 613- 621. 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 14. Kroenke K., Spitzer RL., Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001. September; 16 9: 606- 613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016. Mar-Apr; 39: 24- 31. 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 16. Ruiz MA., Zamorano E., García-Campayo J., Pardo A., Freire O., Rejas J. Validity of the GAD-7 scale as an outcome measure of disability in patients with generalized anxiety disorders in primary care. J Affect Disord. 2011. February; 128 3: 277- 286. 10.1016/j.jad.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 17. Spitzer RL., Kroenke K., Williams JB., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006. May 22; 166 10: 1092- 1097. [DOI] [PubMed] [Google Scholar]
- 18. Fischer F., Lange K., Klose K., Greiner W., Kraemer A. Barriers and strategies in guideline implementation-a scoping review. Healthcare (Basel). 2016. June 29; 4 3 10.3390/healthcare4030036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sirajuddin AM., Osheroff JA., Sittig DF., Chuo J., Velasco F., Collins DA. Implementation pearls from a new guidebook on improving medication use and outcomes with clinical decision support. Effective CDS is essential for addressing healthcare performance improvement imperatives. J Healthc Inf Manag. 2009. Fall; 23 4: 38- 45. [PMC free article] [PubMed] [Google Scholar]