Abstract
Background:
Health services in Kazakhstan have undergone radical reforms since its independence in 1991, but levels of dissatisfaction among patients remain high. We investigated whether healthcare providers and patients at one hospital in Astana, Kazakhstan, believe the doctor-patient interaction should be doctor-centered vs patient-centered.
Methods:
We conducted a cross-sectional study of the responses to various surveys of 200 patients (response rate, 74%) and 201 healthcare providers (response rate, 86%) in a general hospital in Astana, Kazakhstan. The participants completed a questionnaire containing the Patient-Practitioner Orientation Scale (PPOS) and scales assessing life and job satisfaction, job effort-job reward balance, and patient evaluation of communication. Analyses were restricted to those with valid data on the variables age, sex, and PPOS (147 providers and 150 patients).
Results:
An overwhelming majority of doctors (80%), nurses (87%), and patients (93%) were doctor-oriented. Among patients, higher patient-oriented scores were statistically significantly associated with higher satisfaction with communication with healthcare providers (P=0.038) and with life satisfaction (P=0.009).
Conclusion:
Only a small percentage of doctors, nurses, and patients reported that their interaction should be patient-centered. This congruence between providers and patients does not explain dissatisfaction, but the finding that patient-centered patients were more satisfied suggests an area for improvement.
Keywords: Nurse-patient relations, patient-centered care, physician-patient relations
INTRODUCTION
Consultation with a doctor is highly contextual; both doctors and patients expect certain roles to be enacted in particular ways based on experience and preference. These expectations are fulfilled principally through conversation between the doctor and patient, even though awareness of the importance of talking is often low.1 While research in the area of doctor-patient communication has often focused on communication techniques and strategies, research into patient preference reveals a desire to establish relationships of trust in which patients feel their doctors are concerned about them as individuals.2 These preferences, however, are also influenced by cultural and historic factors involving norms of interaction, power relations, and even perceptions of health and healthcare in society. We examined the doctor-patient relationship in the context of the post-Soviet republic of Kazakhstan to investigate how cultural and historic influences may be leading to high dissatisfaction for both doctors and patients in the current healthcare system.
Kazakhstan, like other post-Soviet countries, has undergone dramatic transformation since becoming independent in 1991. Part of the process of transformation has been profound changes in the healthcare system. Current efforts in strengthening the healthcare system involve the inclusion of more patient-centered approaches as advised by the World Health Organization. However, to what extent the hierarchic nature of the system has changed in practice as well as whether the system is becoming more patient-centered is unclear. Many social and historic factors, including norms of power distance and deference to authority, influence doctors and patients in their respective roles in society and in the establishment of a relationship.
The perceptions doctors and patients have of themselves and of one another, not as individuals but as members of social groups, are potential barriers to establishing relationships. Cultural influences on health beliefs and scientific knowledge can be obstacles in communication between doctors and patients;3 however, stereotypes and social categories of both doctors and patients are also significant problems that affect communication.1
Societies vary in their historic and cultural influences; therefore, research in this area should include sociocultural context and past health systems as relevant factors in an examination of effective communication practices between doctors and patients.2
The literature suggests that patients increasingly prefer a patient-centered approach to care; however, such preferences vary by population, as does the definition of patient-centered.4 Patient-centered approaches to care in general start with the understanding that 2 experts are present at the doctor visit: (1) the doctor as an expert in medicine and (2) the patient as the expert in his or her own life.1 A patient-centered approach sees the doctor visit as a partnership that requires doctors to consider the patient's needs, wants, perspectives, and individual experiences to include the patient in decision-making. Patient-centered approaches have been shown to be associated with higher levels of patient satisfaction, increased compliance, and even better clinical outcomes.5
However, not all patients prefer patient-centered care.6,7 Previous research has found that patient-centered care is generally preferred by patients who are younger and more educated and who have a patient-centered doctor. Patients who do not prefer a patient-centered approach tend to be older and desire a more directive, biomedical style of communication.7 Krupat and colleagues found that patient-centered congruence is associated with greater patient trust and compliance.6 Furthermore, patients in this study who felt their preference for patient-centeredness was fulfilled by a doctor reported that they were more likely to recommend that doctor to others for care and even make a special effort to see that same doctor again. If doctors and patients started out with the same worldview about care, the relationship was more satisfying for both parties.
Krupat and colleagues also point out that patient-centeredness in the doctor visit involves more than individual preferences or even social categories.6 While the preference for patient-centeredness is increasing overall in some cultural contexts,8 in societies with different cultural norms governing interactions between people in different social roles, such preferences may vary and congruence alone may not produce better outcomes.
Many assumptions that inform the patient-centered approach, such as patients desiring as much information as possible,1 indicate a connection between the orientation of the provider toward the patient and the communication style used with patients.9,10 Patient-centeredness may not be as influential in contexts where cultural and political histories have shaped health systems and norms of behavior in different ways. For example, Charles et al noted the influence culture may have on patient participation in decision-making, an important aspect of patient-centered care.11
An example of how context influences the doctor-patient relationship is the common occurrence of dissatisfaction and lack of trust in post-Soviet countries. Trust, as mentioned earlier, is important in establishing relationships between doctors and patients. Without trust, patients may not disclose important medical information or may avoid seeing a doctor altogether.12 However, distrust is common because of many Soviet-era characteristics of healthcare that current governments are struggling to change. Healthcare during Soviet times was largely underfunded and included non–evidence based practices and beliefs.13 Corruption was also a problem in the form of informal payments,14 which is one reason why it is still common for people in post-Soviet countries to not seek care when needed.15 Patients with a low level of trust in their doctor are more likely to report dissatisfaction, specifically that requested or needed services were not provided.
In Kazakhstan, the principal reason for patients' complaints is not medical errors but dissatisfaction with how their needs were addressed by medical personnel.16 The Kazakhstani Ministry of Health uses patient complaints, not medical errors, to rate the medical organizations of the country.17 Current policies focus on punishing organizations for high complaint ratings instead of examining the problem for possible solutions. The objective of our study was to examine the orientations of doctors and patients during the doctor visit to explore the role of the perceptions and expectations of doctors and patients about themselves and each other. We hypothesized that a majority of doctors and nurses in Astana, Kazakhstan, would not be patient-centered and a majority of patients would be; thus, the lack of congruence could be leading to patient dissatisfaction with care.
METHODS
Study Design
After receiving approval from our institution's research ethics committee, we conducted a cross-sectional study of patients and healthcare providers (doctors and nurses) in the largest public hospital in Astana, Kazakhstan. After obtaining informed consent from all participants, the participants completed structured questionnaires containing basic demographic questions as well as scales assessing patient-practitioner orientation, life and job satisfaction, job effort-reward (ER) balance of healthcare professionals, and the patients' perceptions of the doctors' and nurses' communication practices. These scales were used to measure the orientation both providers and patients had toward each other to explore any possible relationships between this orientation and other factors dealing with satisfaction with life and work. Upon completion, participants sealed their responses in provided envelopes and deposited them in a locked box located in the hospital to ensure anonymity.
Participants
A total of 234 providers were asked to participate in the study, and 201 agreed to complete the survey; the response rate was 86%. A total of 271 patients were available in the selected departments, and 200 patients agreed to participate; the response rate was 74%. The providers were randomly selected from each department to obtain a representative sample of the hospital staff. Patients were selected randomly as they were leaving the hospital and asked to fill out the survey.
Measures
The Provider-Patient Orientation Scale (PPOS)18 was developed to assess doctors' and patients' orientations toward one another during the doctor visit. We chose the PPOS because it can compare both provider and patient orientations to check for congruence. The original PPOS contains 18 questions; responses are recorded on a 6-point scale (higher score means more patient orientation), and the response scores are summed. We used the original PPOS with 6-point scale for all provider participants. We translated the PPOS into Russian and back into English to check for consistency in meaning.
The use of Likert scales is a relatively new practice in Kazakhstan. On the recommendation of hospital management and with the support of previous research on culture and modified scales,19,20 we modified the survey answers for patients to a 4-point Likert scale (instead of the 6-point scale used for providers) and asked patients to read each item and mark the appropriate circle to indicate how much they agreed or disagreed with each option: strongly agree, slightly agree, slightly disagree, strongly disagree.
Several other potentially relevant scales were included on the questionnaire for doctors, nurses, and patients: the Satisfaction with Life Scale (5 items),21 the Job Satisfaction Scale (16 items),22 and the Effort-Reward Imbalance Questionnaire (22 items). The imbalance between effort and reward was measured by the ER ratio, with the job effort score being the numerator and the reward score the denominator, multiplied by a correction factor to allow for an unequal number of questions in the numerator and denominator, as previously proposed by Siegrist et al.23 For patients only, we included the Communication Assessment Tool for Patients (15 items), which evaluates patients' satisfaction with their providers' communication practices.24 Patients do not consistently see the same provider because of Kazakhstan's healthcare delivery system, so the responses to this scale reflect general experiences rather than experiences with specific providers. In addition to the previous measures, the demographic characteristics age and sex were collected for all participants, and type of provider (doctor or nurse) and department were collected for providers.
Data Analysis
Many values were missing in the survey responses. Among the 201 providers, data were available for 183 participants for sex, 171 for age, and 176 for whether the respondents were doctors or nurses. Among the 200 patients, data were available for 160 patients for sex and 163 for age. Data were also missing on the PPOS, the Satisfaction with Life scale, and all other variables. Statistical analysis was therefore restricted to participants with complete data on age, sex, and PPOS (147 providers and 150 patients).
All questions were recoded in the same direction (higher score means more patient orientation) and summed. The mean score was calculated by dividing the sum by the number of responses (we allowed up to 4 questions with missing responses; participants with missing values in >4 questions were excluded from the analysis). Because the response categories of the PPOS questions differed between providers and patients (6-point vs 4-point scale), we calculated 2 binary measures for providers and patients. Among providers, the PPOS was dichotomized with a cutoff point of the full response scale >3.5 (the midpoint between agree and disagree with patient orientation). The second binary variable was calculated by first collapsing categories: strongly disagree, somewhat disagree, and disagree on the one hand (value 1) and strongly agree, somewhat agree, and agree on the other hand (value 2); the cutoff point was >1.5 (the midpoint between disagree and agree). A similar binary variable was created for patients by collapsing strongly and slightly disagree (value 1) and slightly and strongly agree (value 2); again, the cutoff point was >1.5.
Descriptive analyses of the binary measures of provider-patient orientation were conducted using cross-tabulations, calculation of percentages, and chi-square tests. Associations of the provider-patient orientation with covariates were assessed using Pearson correlation coefficients and linear regression. In additional sensitivity analyses, multivariable logistic regression (binary provider-patient orientation outcome variable) and linear regression (continuous binary provider-patient orientation outcome variable) were used to adjust for all other available covariates, using the maximum number of participants with valid data in a given model. Because of the modest number of subjects, the multivariable analyses were only used to support the bivariate analyses and are not reported in the tables. Differences in mean scores were analyzed by analysis of variance (ANOVA). Stata statistical software (StataCorp, LLC) was used for all analyses.
RESULTS
Demographic Characteristics
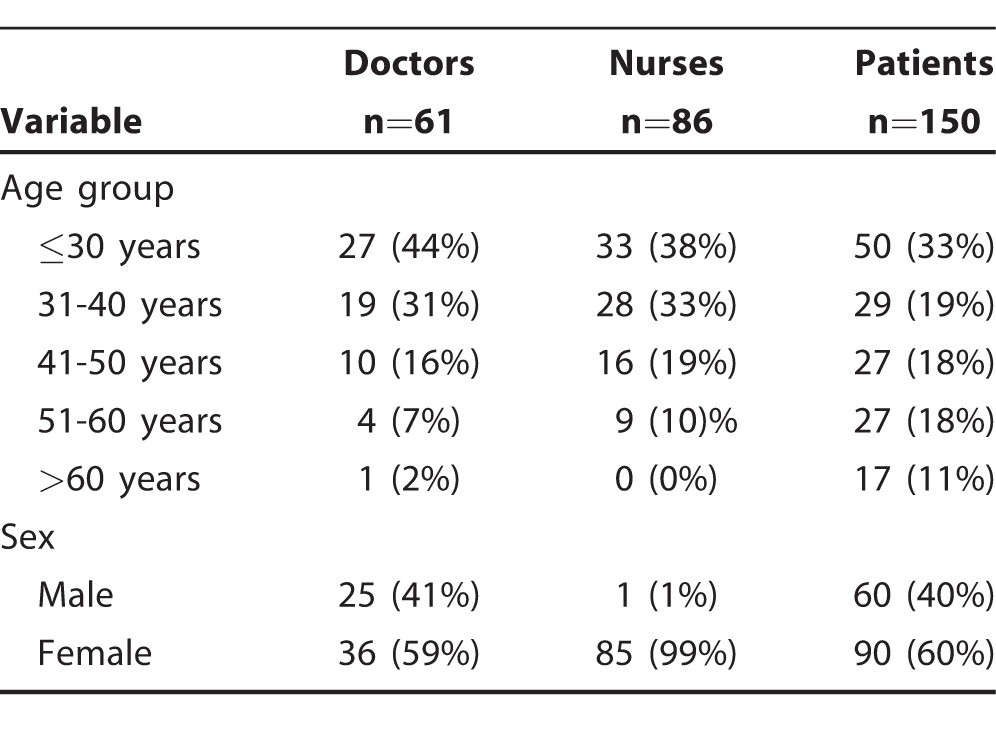
Patients were similarly distributed throughout the age groups. However, doctors and nurses were distributed more heavily in the younger age groups. The nurses were almost all female, while the sex distribution of doctors was similar to that of patients. The distribution of participants by age and sex is shown in Table 1. We found no differences in the sex distribution of providers between different hospital departments.
Table 1.
Distribution of Participants With Valid Data on the Provider-Patient Orientation Scale by Age and Sex
PPOS Data for Providers (Doctors and Nurses)
We found no significant differences in PPOS scores between doctors and nurses or between male and female providers (doctors and nurses).
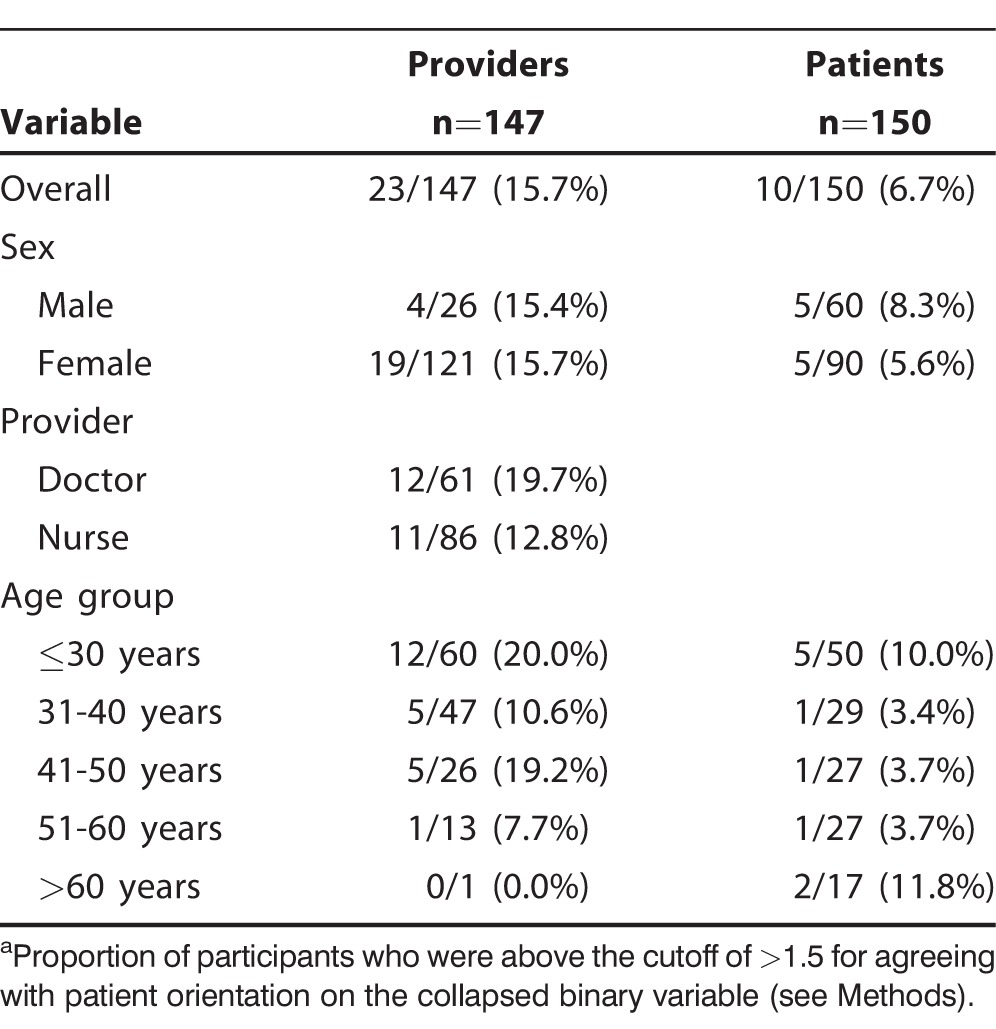
Table 2 shows the proportions of providers who could be characterized as patient-oriented. The data show that the majority of providers were doctor-oriented. Overall, only 15.7% of providers identified themselves as patient-oriented. The proportions were similar between males and females, but the proportion of patient-oriented providers was smaller among nurses than among doctors and among older providers.
Table 2.
Patient-Oriented Providers and Patients With Valid Data on the Provider-Patient Orientation Scalea
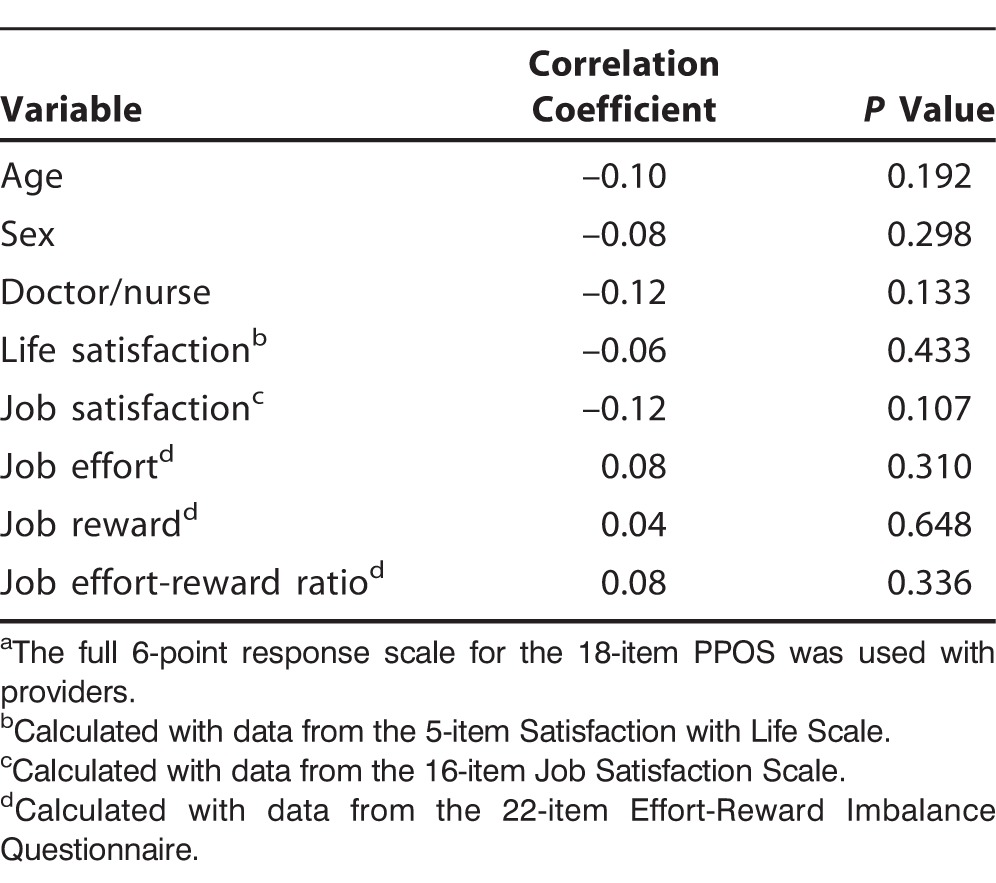
Other Variables for Providers and Correlations With PPOS Data
The other variables collected from providers were life satisfaction, job satisfaction, job effort, job reward, and the ER ratio as a measure of ER imbalance. Most variables were distributed symmetrically, and we found no major differences between doctors and nurses or between males and females. Table 3 shows the correlation coefficients between the PPOS and other factors measured in providers. The correlation coefficient estimates the direction and strength of association between 2 continuous variables; the square of the coefficient indicates the proportion of variation in dependent variables (PPOS) explained by independent variables. All correlation coefficients were not statistically significant, demonstrating that the PPOS was not associated with any of these variables. For example, the correlation coefficient between the PPOS and the age of providers was –0.10, indicating an inverse association (older age is associated with less patient orientation) but a weak one (age explains only approximately 0.1×0.1=0.01, ie, a 1% variation in PPOS), with a statistically nonsignificant P value.
Table 3.
Correlation Between Provider-Patient Orientation Scale (PPOS)a and Covariates for Providers (n=147)
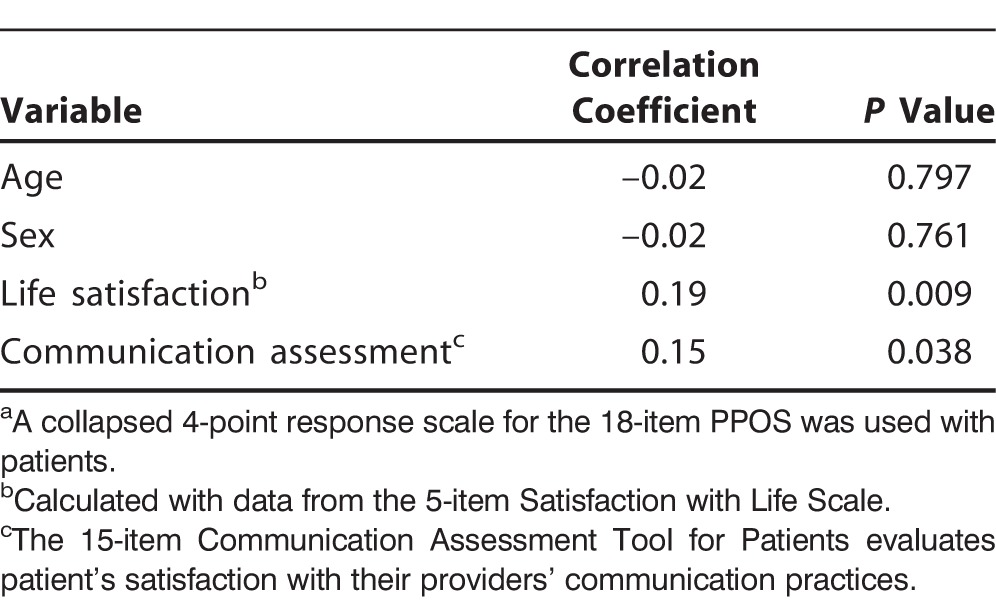
PPOS Data for Patients
Table 2 shows the proportions of patients who could be characterized as patient-oriented. Overall, the proportion of patients who identified as patient-oriented (6.7%) was less than half of the proportion of providers who identified as patient-oriented (15.7%). The correlations between PPOS and other variables for patients suggest that both life satisfaction and the communication assessment were significantly associated with PPOS; patients with higher scores on life satisfaction and communication were more patient-oriented (Table 4).
Table 4.
Correlation Between Provider-Patient Orientation Scale (PPOS)a and Covariates for Patients (n=150)
Comparing the PPOS Between Providers and Patients
Using the dichotomized PPOS scale with a cutoff of >1.5 points, the proportion of patient-oriented participants was highest among doctors (19.7%) compared to 12.8% of nurses and 6.7% of patients. The difference between the 3 groups was marginally statistically significant (P=0.047). Using the continuous PPOS with 4-point response scale, the P value for ANOVA was also statistically significant (P<0.001, not shown). In multivariable analysis, the difference between providers and patients was not explained by adjustment for age group, sex, or life satisfaction (not shown in table).
DISCUSSION
We found that an overwhelming majority of doctors (80%), nurses (87%), and patients (93%) were doctor-oriented. Among healthcare providers, PPOS was not associated with age, sex, life and job satisfaction, or ER imbalance. Among patients, PPOS was not associated with age, sex, or healthcare profession of their providers (doctor or nurse). However, higher PPOS among patients (indicating preference for patient-oriented interaction) was associated with higher satisfaction with communication with healthcare providers (P=0.038) and with their life satisfaction (P=0.009).
Interpretation of Findings
We expected to find a high percentage of doctors and nurses to be doctor-oriented, but we did not expect that an even higher percentage of patients would be doctor-oriented. The high percentages of both patients and providers considered to be doctor-oriented in our study are different than findings in the literature that support an overall preference for patient-centered care.
Research using the PPOS in the United States has generally found providers and patients to be at least slightly patient-oriented in their scores. Krupat et al18 found in their study of doctors and patients that mean scores for both groups were generally high, toward the patient-oriented end of the scale. Another study found that doctors and patients were patient-oriented, but the mean score for doctors was significantly more patient-oriented than the patients' mean score.6 Likewise, medical students in the United States have been shown to be patient-oriented in their mean scores.24-26
Research using the PPOS in other countries has demonstrated variance in scores, but doctors, medical students, and patients still tend to score more toward patient orientation. Carlsen et al27 found general practitioners in Norway to be more patient-oriented than doctor-oriented as other studies have found medical students to be in Greece,28 Brazil,29 and Singapore.30 Patients were likewise often found to be more patient-oriented than doctor-oriented in countries such as Norway27 and Nepal31 although not as strongly as in the United States. Additionally, some studies have found that females are more patient-oriented than males.24,28
The proportions of doctor orientation in providers and patients in our study may reflect the post-Soviet historic legacy of hierarchic organization of society that was apparent in all sectors, including healthcare. During Soviet times, the distribution of resources and the administration of health services were centralized around Moscow, the capital.32 Centralization still exists in Kazakhstan, although changes have been and continue to be made. During the transition period in the 1990s, reforms made access less equitable and even more difficult in terms of proximity of facilities and quantity of available trained professionals than they had been previously. Connections through formal and informal networks became very important.32 As access to healthcare became scarce and marked by social hierarchies, the attitude that the doctor mattered more than the patient in the doctor-patient interaction likely developed.
The fact that PPOS scores in our study did not vary significantly across sex or hospital department and the high level of congruence between doctors and patients regarding their orientations support the notion that orientations in the doctor visit may be influenced by cultural norms and expectations. As previous research suggests, congruence can lead to higher levels of patient satisfaction,6,33 although not always.34 In our case, reported levels of satisfaction were low, and congruence must be understood along with other factors.
For providers, being doctor-oriented can lead to misdiagnosis and ineffective care.35 Doctors may not completely understand a health problem if the patient's lifestyle and ability or willingness to alter behaviors are not taken into account. Being doctor-oriented does not encourage patient involvement and can encourage the patient to believe that his or her role is minimal.
For patients, being doctor-oriented can lead to dissatisfaction with the doctor visit and noncompliance with the doctor's recommendations. Patients who are doctor-oriented may not feel as though they have been treated well because, without their active participation, their concerns and needs are not being addressed, and, as a consequence, these patients are more likely to file complaints about the care they received. Patients who are doctor-oriented may distrust a doctor if they have a negative experience and may delay seeking care when it is necessary, leading to deteriorating health conditions.36
Patient expectations may be an influential factor in the dissatisfaction with care despite the congruence in being doctor-oriented. While patients and doctors in this study overwhelmingly reported being doctor-oriented, the expectations of patients that doctors are responsible for their health may be leading to dissatisfaction. Patients who feel that the doctor visit should be doctor-centered could feel that the doctor is the person who matters and that the doctor alone is responsible for health outcomes. If patient expectations of the doctor are unrealistic or misplaced, even congruence in orientation between doctors and patients may not facilitate a satisfactory experience.
The high percentage of doctor-oriented patients in Kazakhstan may have other implications for health and healthcare. If patients see the doctor or the healthcare system as the responsible party for health, their sense of responsibility and even control over their own health may lead to negative health behaviors. As Bobak et al noted, in postcommunist countries, perceived control is strongly related to self-rated health.37 Patients who perceive a sense of control over their own health are likely to rate their health as very good. Conversely, patients who do not perceive their health to be within their control are not likely to rate their health as good.37 In our case, a perceived lack of control may be related to poor ratings of personal health. Poor ratings of personal health, if health is seen as the responsibility of healthcare providers, may lead to further dissatisfaction with providers. Inaccurate perceptions of healthcare delivery and personal responsibility are a possible explanation for why congruence is not yielding higher satisfaction. Further research should explore the issues of trust and the expectations of patients toward their healthcare providers.
Practice Implications
This study suggests several practice implications for healthcare providers in Kazakhstan. Providers face an uphill battle in moving toward patient-centered care because, based on our results, their patients generally support a patient-centered approach to care even less than providers do. However, the fact that the small percentage of patients in our study who were patient-oriented were also more satisfied with life and with communication during their doctor visit suggests that a move toward patient orientation is worth pursuing.
Communication training for providers is an important first step in encouraging a more patient-centered approach. However, patient education on the patient's role and responsibility is also needed. While the doctor's approach in the visit can positively influence patients' behavior and ultimately their satisfaction, patients' orientation toward the visit beforehand owing to social norms and common beliefs can inhibit progress. Therefore, we recommend patient education on a broad scale to include the general public, as well as provider training. If issues such as trust in healthcare providers are present in society, messages that establish roles for providers and patients in a cooperative relationship should be used to educate the public.
To counter distrust, a patient should be able to establish a relationship with his or her provider. The current healthcare system in Kazakhstan is not conducive to patients seeing the same doctors repeatedly to build a relationship. Although changes in the healthcare system are allowing for more choice in providers, the public has not made changes in their utilization of services. Systemic changes that facilitate building relationships of trust between providers and patients should be made.
Limitations
The relatively small sample size of <200 usable provider and patient responses is a limitation of this study. Furthermore, all participants came from the same hospital, and even though it is the largest hospital in the city, our study population is not a representative sample of the city or of the country. Patients who participated in this study were not matched with their providers because patients in Kazakhstan are not assigned to a specific provider. Consequently, we were not able to draw any conclusions based on specific participant orientations to care and how such orientations are received by the other party in an actual visit.
Another limitation is that PPOS had different numbers of response categories for providers and for patients, making direct comparison difficult. However, the distributions (histograms) of PPOS scores were symmetric in both groups, with means very close to medians; symmetric distribution between groups does not suggest systematic differences in response modes between patients and providers.
In addition, the cultural explanation for our findings is unclear. Although culture is important in examining doctor-patient communication in a non-Western context, why our findings are different than previous research is not entirely explained. Further research might explore the orientations of providers and patients using qualitative research methods to uncover the expectations and explanations of these actors from their own perspectives.
Furthermore, because ours was a pilot study, we did not know beforehand how our results would fit in the broader sociocultural context regarding patient and provider orientations toward one another. Now that this study has given us a better understanding of how dissatisfaction, trust, and the responsibilities of each party interact in the healthcare system in Kazakhstan, future studies should incorporate scales that specifically measure these dimensions compared with the PPOS and provider communication style.
CONCLUSION
The principal finding of this study is the small percentage of doctors, nurses, and patients who believe that the doctor-patient interaction should be patient-oriented. These results highlight the necessity of improving communication among healthcare providers with a patient-oriented approach to decrease miscommunication with and dissatisfaction among patients. The fact that most patients report that the doctor visit should be doctor-oriented may reflect societal beliefs about who is responsible for health. Furthermore, an expectation that the doctor is the center of the visit, combined with a general distrust of healthcare providers, may explain high levels of dissatisfaction with care among patients and even among providers in Kazakhstan.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1. Roter DL., Hall JA. Doctors Talking With Patients/Patients Talking With Doctors: Improving Communication in Medical Visits. 2nd ed. Westport, CT: Praeger; 2006. [Google Scholar]
- 2. Epstein RM., Franks P., Fiscella K., et al. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med. 2005. October; 61 7: 1516- 1528. [DOI] [PubMed] [Google Scholar]
- 3. Vaughn LM., Jacquez F., Baker RC. Cultural health attributions, beliefs, and practices: effects on healthcare and medical education. Open Med Educ J. 2009; 2: 64- 74. [Google Scholar]
- 4. Chewning B., Bylund CL., Shah B., Arora NK., Gueguen JA., Makoul G. Patient preferences for shared decisions: a systematic review. Patient Educ Couns. 2012. January; 86 1: 9- 18. 10.1016/j.pec.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Trummer UF., Mueller UO., Nowak P., Stidl T., Pelikan JM. Does physician-patient communication that aims at empowering patients improve clinical outcome? A case study. Patient Educ Couns. 2006. May; 61 2: 299- 306. [DOI] [PubMed] [Google Scholar]
- 6. Krupat E., Bell RA., Kravitz RL., Thom D., Azari R. When physicians and patients think alike: patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001. December; 50 12: 1057- 1062. [PubMed] [Google Scholar]
- 7. Swenson SL., Buell S., Zettler P., White M., Ruston DC., Lo B. Patient-centered communication: do patients really prefer it? J Gen Intern Med. 2004. November; 19 11: 1069- 1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Otero C., Luna D., Marcelo A., et al. Why patient centered care coordination is important in developing countries? Contribution of the IMIA health informatics for development working group. Yearb Med Inform. 2015. August 13; 10 1: 30- 33. 10.15265/IY-2015-013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moore M. What does patient-centred communication mean in Nepal? Med Educ. 2008. January; 42 1: 18- 26. [DOI] [PubMed] [Google Scholar]
- 10. Street RL, Jr, Gordon H., Haidet P. Physicians' communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007. August; 65 3: 586- 598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Charles C., Gafni A., Whelan T., O'Brien MA. Cultural influences on the physician-patient encounter: the case of shared treatment decision-making. Patient Educ Couns. 2006. November; 63 3: 262- 267. [DOI] [PubMed] [Google Scholar]
- 12. Hall MA., Camacho F., Dugan E., Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002. October; 37 5: 1419- 1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bond A., Beresford G. Healthcare development in the former Soviet Union. Postgrad Med J. 2003. October; 79 936: 551- 552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Radin D. Too ill to find the cure? Corruption, institutions, and health care sector performance in the new democracies of Central and Eastern Europe and Former Soviet Union. E Eur Polit Soc. 2009; 23: 105- 125. [Google Scholar]
- 15. Balabanova D., Roberts B., Richardson E., Haerpfer C., McKee M. Health care reform in the former Soviet Union: beyond the transition. Health Serv Res. 2012. April; 47 2: 840- 864. 10.1111/j.1475-6773.2011.01323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. In the RK, statistics of medical errors are not kept [in Russian]. Diapazon. http://www.diapazon.kz/kazakhstan/kaz-incidents/46360-v-rk-ne-vedetsya-statistika-vrachebnyh-oshibok.html. Accessed May 29, 2014.
- 17. Complaints of patients will be included in rating medical organizations [in Russian]. Zakon. http://www.zakon.kz/4606203-s.kairbekova-zhaloby-pacientov-vojjdut.html. Accessed May 29, 2014.
- 18. Krupat E., Rosenkranz SL., Yeager CM., Barnard K., Putnam SM., Inui TS. The practice orientations of physicians and patients: the effect of doctor-patient congruence on satisfaction. Patient Educ Couns. 2000. January; 39 1: 49- 59. [DOI] [PubMed] [Google Scholar]
- 19. Chang L. A psychometric evaluation of 4-point and 6-point likert-type scales in relation to reliability and validity. Appl Psych Meas. 1994; 18: 205- 215. [Google Scholar]
- 20. Marin G., Gamba RJ., Marin BV. Extreme response style and acquiescence among Hispanics: the role of acculturation and education. J Cross Cult Psychol. 1992; 23: 498- 509. [Google Scholar]
- 21. Diener E., Emmons RA., Larsen RJ., Griffin S. The satisfaction with life scale. J Pers Assess. 1985. February; 49 1: 71- 75. [DOI] [PubMed] [Google Scholar]
- 22. Warr P., Cook J., Wall T. Scales for the measurement of some work attitudes and aspects of psychological well-being. J Occup Psychol. 1979; 52: 129- 148. [Google Scholar]
- 23. Siegrist J., Starke D., Chandola T., Godin I., Marmot M., Niedhammer I., Peter R. The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med. 2004. April; 58 8: 1483- 1499. [DOI] [PubMed] [Google Scholar]
- 24. Makoul G., Krupat E., Chang CH. Measuring patient views of physician communication skills: development and testing of the communication assessment tool. Patient Educ Couns. 2007. August; 67 3: 333- 342. [DOI] [PubMed] [Google Scholar]
- 25. Krupat E., Yeager CM., Putnam S. Patient role orientations, doctor-patient fit, and visit satisfaction. Psychol Health. 2000; 15: 707- 719. [Google Scholar]
- 26. Haidet P., Dains JE., Paterniti DA., Chang T., Tseng E., Rogers JC. Medical students' attitudes toward patient-centered care and standardized patients' perceptions of humanism: a link between attitudes and outcomes. Acad Med. 2001. October; 76 10 Suppl: S42- S44. [DOI] [PubMed] [Google Scholar]
- 27. Carlsen B., Aakvik A. Patient involvement in clinical decision making: the effect of GP attitude on patient satisfaction. Health Expect. 2006. June; 9 2: 148- 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tsimtsiou Z., Kerasidou O., Efstathiou N., Papaharitou S., Hatzimouratidis K., Hatzichristou D. Medical students' attitudes toward patient-centred care: a longitudinal survey. Med Educ. 2007. February; 41 2: 146- 153. [DOI] [PubMed] [Google Scholar]
- 29. Ribeiro MM., Krupat E., Amaral CF. Brazilian medical students' attitudes towards patient-centered care. Med Teach. 2007. September; 29 6: e204- e208. [DOI] [PubMed] [Google Scholar]
- 30. Lee KH., Seow A., Luo N., Koh D. Attitudes towards the doctor-patient relationship: a prospective study in an Asian medical school. Med Educ. 2008. November; 42 11: 1092- 1099. 10.1111/j.1365-2923.2008.03157.x. [DOI] [PubMed] [Google Scholar]
- 31. Field MG. The Soviet legacy: the past as prologue. : Mckee M., Healy J., Falkingham J. Health Care in Central Asia. Philadelphia, PA: Open University; 2002: 67- 76. [Google Scholar]
- 32. Brown JV., Rusinova NL. Russian medical care in the 1990s: a user's perspective. Soc Sci Med. 1997. October; 45 8: 1265- 1276. [DOI] [PubMed] [Google Scholar]
- 33. Carlsen B., Aakvik A., Norheim OF. Variation in practice: a questionnaire survey of how congruence in attitudes between doctors and patients influences referral decisions. Med Decis Making. 2008. Mar-Apr; 28 2: 262- 268. 10.1177/0272989X07311751. [DOI] [PubMed] [Google Scholar]
- 34. Cvengros JA., Christensen AJ., Hillis SL., Rosenthal GE. Patient and physician attitudes in the health care context: attitudinal symmetry predicts patient satisfaction and adherence. Ann Behav Med. 2007. June; 33 3: 262- 268. [DOI] [PubMed] [Google Scholar]
- 35. Ha JF., Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010; 10 1: 38- 43. [PMC free article] [PubMed] [Google Scholar]
- 36. Calnan M., Rowe R., Entwistle V. Trust relations in health care: an agenda for future research. J Health Organ Manag. 2006; 20 5: 477- 484. [DOI] [PubMed] [Google Scholar]
- 37. Bobak M., Pikhart H., Rose R., Hertzman C., Marmot M. Socioeconomic factors, material inequalities, and perceived control in self-rated health: cross-sectional data from seven post-communist countries. Soc Sci Med. 2000. November; 51 9: 1343- 1350. [DOI] [PubMed] [Google Scholar]


