Abstract
Background:
Acute calcific tendonitis of the longus colli (ACTLC) is an aseptic inflammatory response to deposition of calcium in the longus colli muscle tendons. Although reports in the literature are scarce, ACTLC likely represents an underreported disease process that routinely goes misdiagnosed. We report a case of ACTLC and provide a brief review of the literature.
Case Report:
A 45-year-old otherwise healthy female presented with a 3-day history of progressive neck pain, decreased neck mobility, and odynophagia. She exhibited tenderness over the right posterolateral neck with limited neck flexion and rotation. Flexible fiber-optic laryngoscopy revealed moderate posterior pharyngeal wall edema extending from the palatal-pharyngeal sphincter down to the level of the epiglottis. A computed tomography (CT) scan of the neck with contrast revealed an amorphous calcification in the longus colli muscle and a prevertebral fluid collection without rim enhancement. A diagnosis of ACTLC was presumed. The patient was successfully managed with nonsteroidal antiinflammatory drugs, corticosteroids, and antibiotics and reported complete resolution of symptoms on follow-up.
Conclusion:
The clinical presentation and laboratory findings of ACTLC are nonspecific; however, a CT scan revealing a calcific deposition in the retropharyngeal space confirms the diagnosis. Spontaneous resolution during the course of several weeks warrants conservative treatment with analgesia and antiinflammatory medications. Awareness of ACTLC must be increased to avoid diagnostic errors and prevent unnecessary medical interventions.
Keywords: Calcinosis, neck muscles, neck pain, tendinopathy, torticollis
INTRODUCTION
Acute calcific tendonitis of the longus colli muscle (ACTLC) is an aseptic inflammatory response to the deposition of calcium hydroxyapatite crystals in the superior fibers of the longus colli muscle tendons (C1-C3 vertebral level). Although reports in the literature are scarce, ACTLC likely represents an underreported disease process that routinely goes misdiagnosed. Computed tomography (CT) of the neck with contrast showing calcifications in the prevertebral space confirms the diagnosis. Successful management includes the use of nonsteroidal antiinflammatory drugs (NSAIDs) and corticosteroids.1 We report a case of ACTLC and provide a brief review of the literature.
CASE REPORT
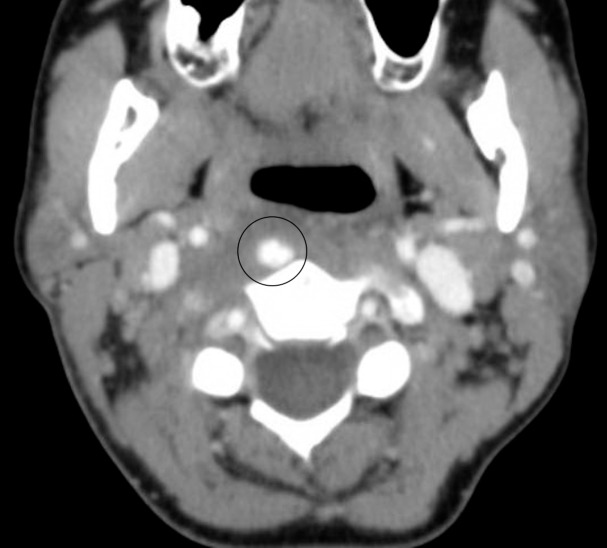
A 45-year-old otherwise healthy female presented with a 3-day history of progressive neck pain, decreased neck mobility, and odynophagia. The patient was afebrile with normal vital signs. She exhibited tenderness over the right posterolateral neck with limited range of motion on flexion and rotation of the neck. Flexible fiber-optic laryngoscopy revealed moderate posterior pharyngeal wall edema extending from the palatal-pharyngeal sphincter down to the level of the epiglottis. Her white blood cell count was in the upper limit of normal. CT scan of the neck with contrast revealed an amorphous calcification in the longus colli muscle and a prevertebral fluid collection without rim enhancement (Figures 1 and 2). A diagnosis of ACTLC was presumed, although retropharyngeal abscess was still in consideration. The patient was managed with naproxen 500 mg by mouth twice daily, dexamethasone (Decadron) 8 mg intravenously (IV) three times daily, morphine 2 mg IV every 2 hours as needed for pain, and clindamycin 900 mg IV three times daily (initiated in emergency room), and she displayed marked improvement on hospital day 1. She was discharged on hospital day 1 on naproxen 500 mg by mouth twice daily for 2 weeks and amoxicillin (Augmentin) 875/125 mg by mouth twice daily for 7 days as a precautionary measure given her associated prevertebral fluid collection. The patient reported complete resolution of symptoms at a telephone interview 4 weeks after presentation.
Figure 1.
Axial computed tomography scan at the C2 level shows calcific deposit in the mass of the longus colli muscle (circled).
Figure 2.
Sagittal reconstructed computed tomography with contrast demonstrates a smooth, lenticular-shaped fluid collection in the prevertebral soft tissues (arrow), with amorphous calcification embedded within the proximal fibers of the longus colli tendon, anterior to the C2 vertebral body (circled).
DISCUSSION
Anatomy
The longus colli muscle is one of the 4 deep cervical flexor muscles and consists of superior oblique, vertical, and inferior oblique fibers. This muscle provides cervical flexion, ipsilateral flexion, and some rotational movement. The superior oblique fibers, which originate from the transverse processes of C3-C5 and fuse into a tendon that inserts onto the anterior tubercle of the atlas, are the most vulnerable to calcific deposits.2
Epidemiology
ACTLC principally affects adults 30-60 years and has no sex predilection. While only a small number of cases have been presented in the literature, some authors suggest that ACTLC may be more prevalent than previously thought because of missed diagnoses and underreporting of the disease.1,3-10 An epidemiologic study published in 2013 estimated an annual incidence of 0.5 cases per 100,000 person-years and concluded that ACTLC is not as rare as the literature indicates.1
Pathophysiology
The etiology of ACTLC is unclear, although repetitive trauma, ischemia, necrosis, and degeneration of the longus colli tendon are hypothesized to precede calcium and hydroxyapatite crystal deposition. The calcium deposition acts as a localized attempt to compensate for decreased tendon strength, while rupture and release of hydroxyapatite crystals into the surrounding soft tissue lead to an acute inflammatory response.8,9
Clinical Presentation
The symptoms of ACTLC include acute-onset neck pain, neck stiffness, dysphagia, odynophagia, mild fever, and decreased neck mobility. These symptoms, however, are nonspecific and this condition presents similarly to various head and neck pathologies, including retropharyngeal abscess, meningitis, cervical disc herniation, and vertebral fractures.5,9,10
Diagnosis
While the diagnosis of ACTLC ultimately relies on radiologic studies, laboratory findings such as mild leukocytosis and increased inflammatory markers support the diagnosis.10 Lateral plain films are helpful but are unable to rule out similarly presenting pathologies such as retropharyngeal infection, cervical disk herniation/infection, cervical vertebral body subluxation/fracture, meningitis, and extradural hemorrhage. Magnetic resonance imaging, useful in detecting prevertebral fluid collection, may not recognize the calcium depositions. CT is the gold standard for diagnosing ACTLC as it can detect calcific deposition at the longus colli and prevertebral edema. Enhancement around the effusion should shift the diagnosis towards an abscess.3,6,7,9,10
Treatment and Outcome
ACTLC resolves spontaneously during the course of several weeks as macrophages and giant cells phagocytose the calcium hydroxyapatite crystal deposits.6 Because of the self-resolving nature of this disease, symptomatic treatment with NSAIDs has been the mainstay of treatment, with corticosteroids and opioids being reserved for more severe cases. Antibiotics, local analgesic therapy, extracorporeal shock wave therapy, and surgical treatments are not indicated. However, our patient received antibiotics as a precautionary measure given her associated prevertebral fluid collection and the fact that the literature regarding treatment of ACTLC is limited to case reports and retrospective reviews. Local recurrence has not been reported.1,9,10
CONCLUSION
ACTLC is an often-misdiagnosed disease of the head and neck with limited reports in the literature. Clinical presentation and laboratory findings are nonspecific; however, a CT scan revealing a calcific deposition in the retropharyngeal space confirms the diagnosis. Spontaneous resolution during the course of several weeks warrants conservative treatment with analgesia and antiinflammatory medications. Awareness of ACTLC must be increased to avoid diagnostic errors and prevent unnecessary medical interventions.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article. This paper was presented as a poster (#116) at the Triological Society Combined Sections Meeting in New Orleans, LA on January 19-21, 2017.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1. Horowitz G., Ben-Ari O., Brenner A., Fliss DM., Wasserzug O. Incidence of retropharyngeal calcific tendinitis (longus colli tendinitis) in the general population. Otolaryngol Head Neck Surg. 2013. June; 148 6: 955- 958. 10.1177/0194599813482289. [DOI] [PubMed] [Google Scholar]
- 2. Gilroy AM. Anatomy: An Essential Textbook.1st ed. New York, NY: Thieme; 2013. [Google Scholar]
- 3. Eastwood JD., Hudgins PA., Malone D. Retropharyngeal effusion in acute calcific prevertebral tendinitis: diagnosis with CT and MR imaging. AJNR Am J Neuroradiol. 1998. October; 19 9: 1789- 1792. [PMC free article] [PubMed] [Google Scholar]
- 4. Park R., Halpert DE., Baer A., Kunar D., Holt PA. Retropharyngeal calcific tendinitis: case report and review of the literature. Semin Arthritis Rheum. 2010. June; 39 6: 504- 509. 10.1016/j.semarthrit.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 5. Rodrigue E., Costa JP. An unusual cause of neck pain: acute calcific tendinitis of the longus colli. J Med Cases. 2014. March; 5 3: 171- 173. [Google Scholar]
- 6. Offiah CE., Hall E. Acute calcific tendinitis of the longus colli muscle: spectrum of CT appearances and anatomical correlation. Br J Radiol. 2009. June; 82 978: e117- e121. 10.1259/bjr/19797697. [DOI] [PubMed] [Google Scholar]
- 7. Ade S., Tunguturi A., Mitchell A. Acute calcific longus colli tendinitis: an underdiagnosed cause of neck pain and dysphagia. Neurol Bull. 2013; 5: 1- 6. [Google Scholar]
- 8. Oliva F., Via AG., Maffulli N. Physiopathology of intratendinous calcific deposition. BMC Med. 2012. August 23; 10: 95 10.1186/1741-7015-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zibis AH., Giannis D., Malizos KN., Kitsioulis P., Arvanitis DL. Acute calcific tendinitis of the longus colli muscle: case report and review of the literature. Eur Spine J. 2013. May; 22 Suppl 3: S434- S438. 10.1007/s00586-012-2584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Southwell K., Hornibrook J., O'Neill-Kerr D. Acute longus colli calcific tendonitis causing neck pain and dysphagia. Otolaryngol Head Neck Surg. 2008. March; 138 3: 405- 406. 10.1016/j.otohns.2007.12.004. [DOI] [PubMed] [Google Scholar]