Abstract
Cancer treatment is rapidly evolving toward personalized medicine, which takes into account the individual molecular and genetic variability of tumors. Sophisticated new in vitro disease models, such as three-dimensional cell cultures, may provide a tool for genetic, epigenetic, biomedical, and pharmacological research, and help determine the most promising individual treatment. Sarcomas, malignant neoplasms originating from mesenchymal cells, may have a multitude of genomic aberrations that give rise to more than 70 different histopathological subtypes. Their low incidence and high level of histopathological heterogeneity have greatly limited progress in their treatment, and trials of clinical sarcoma are less frequent than trials of other carcinomas. The main advantage of 3D cultures from tumor cells or biopsy is that they provide patient-specific models of solid tumors, and they overcome some limitations of traditional 2D monolayer cultures by reflecting cell heterogeneity, native histologic architectures, and cell–extracellular matrix interactions. Recent advances promise that these models can help bridge the gap between preclinical and clinical research by providing a relevant in vitro model of human cancer useful for drug testing and studying metastatic and dormancy mechanisms. However, additional improvements of 3D models are expected in the future, specifically the inclusion of tumor vasculature and the immune system, to enhance their full ability to capture the biological features of native tumors in high-throughput screening. Here, we summarize recent advances and future perspectives of spheroid and organoid in vitro models of rare sarcomas that can be used to investigate individual molecular biology and predict clinical responses. We also highlight how spheroid and organoid culture models could facilitate the personalization of sarcoma treatment, provide specific clinical scenarios, and discuss the relative strengths and limitations of these models.
Keywords: spheroids, tumor microenvironment, sarcomas, precision medicine, personalized medicine
1. Introduction
Sarcomas are a highly heterogeneous group of solid tumors originating from mesenchymal stem cells (MSCs) [1]. MSCs are multipotent precursor cells of mesenchymal tissues, such as bone, cartilage, fat, and muscle. Based on the wide variety of sarcoma subtypes, the origin of sarcomas can be explained by alterations in MSC-committed cells. Their incidence varies from 3.3 cases per 100,000 in Eastern Europe to 4.7 per 100,000 in Northern Europe [2,3] and they account for 15% of all cancers in childhood and adolescence [4]. The five-year survival rate depends on the type, stage, and location, and the age of the patient. It is reported to be about 60% when diagnosed in early stages [2] but dramatically drops to 10% in advanced stages [5]. Given the heterogeneity and complexity of sarcomas, their clinical management has not advanced nearly as fast as that of many other carcinomas. Clearly, a better understanding of human sarcoma oncogenesis, metastasis, and drug resistance is warranted. The availability of new technologies, such as next-generation sequencing and digital western blot, has improved the selection of novel prognostic molecular markers. However, the low incidence of sarcoma subtypes and insufficient case numbers of individual subtypes make it difficult to validate such markers. Consequently, only a small number of molecular markers are currently available for clinical use. The effect of sarcoma drugs is also affected by intratumoral heterogeneity and the microenvironment, which are important determinants of tumor malignancy and metastasis [6,7,8]. Any model used to define sarcoma subtypes and treatment efficacy must, as far as possible, address these limitations. Cell culture models of sarcoma suffer from the fact that available cell lines are limited to the most common groups, such as osteosarcoma, leiomyosarcoma, and rhabdomyosarcoma, whereas none are available for such subtypes as alveolar soft-part sarcoma and giant-cell tumor of bone [9]. Furthermore, the success rate of sarcoma cell isolation and long-term 2D culture is very limited, mainly because they do not attach well directly on plates and have high genomic instability, particularly aggressive phenotypes. Studies that used 2D cultured tumor cell lines often yielded conflicting results, indicating that culture conditions and the number of cell passages are important. Bruland et al. were the first to develop an alternative to the classical monolayer culture procedure, based on nonadherent cell cultivation. Using this method, they generated 11 sarcoma cell lines from a patient with a 50% success rate [10]. More recently, Salawu further improved this method, increasing the success rate and stability of long-term cell growth, thus making it suitable for studies of the progression of osteosarcoma [9]. Although 2D in vitro models are inexpensive and relatively easy to generate and maintain, they do not accurately reflect the solid tumor characteristics and the complex cross-talk between tumor cells and their microenvironment (Table 1). Therefore, researchers are currently developing novel patient-derived 3D tumor cultures to reproduce the molecular complexity of sarcoma carcinogenic mechanisms and the environment, and to increase sensitivity to pharmacologic treatments. Currently, 3D models are widely used to model different cancers, including breast [11], cervical [11], colon [12], lung [13], pancreatic [14,15], and prostate [16]. Here, we review three-dimensional models of sarcoma that have been recently proposed to study the impact of the tumor microenvironment on its pathogenesis, growth kinetics, and gene expression, and for drug testing. We discuss current applications and future directions, focusing on sarcomas. However, this also may be of interest for other forms of cancer that metastasize to bone and may be applicable to rare cancers.
Table 1.
Comparison of various tumor models.
| Models | General Properties/Advantages | Cost and Reproducibility | Disadvantages | References |
|---|---|---|---|---|
|
2D cell cultures Monolayers cultured on polystyrene or other adherent flat surfaces |
|
|
|
[108,109] |
|
3D scaffold-based cell cultures Cells seeded in structures of different materials: hydrogels, 3D life biomimetic, 3D Insert™ scaffolds (synthetic bone derivatives), Alvetex® |
|
|
|
[109,110,111] |
|
3D nonscaffold-based cell cultures Spheroids from single or multiple cell types; Low-adhesion plates; Micropatterned surfaces (Scivax NanoCulture® multiwell plates); Hanging drop plates (Perfecta3D®, Gravity-PLUS™ 3D) |
|
|
|
[108,109] |
|
Animal models Patient-derivative xenograph (PDX) |
|
|
|
[47,70] |
2. Three-Dimensional Models of Tumors
2.1. Tumor Spheroids
Tumor spheroids are spherical aggregates of tumor cells that are self-organizing and self-renewing. They may originate from single-cell suspensions of tumor cell lines, patient-derived tumor cells, or tumor stem cells cultured in nonadherent substrates [17]. In addition to tumor cells, endothelial cells, and possibly also mesenchymal cells and monocytes, may be included in the co-culture to better sustain and model the tumor microenvironment [18] (see paragraph below). The resulting tumor spheroids have three distinct zones: (1) a central core of necrotic cells, (2) an inner layer of nonproliferating quiescent cells, and (3) an outer nutrient-rich layer of proliferating cells interacting with the surrounding extracellular matrix (ECM) [19]. Although one cannot exclude that established culture conditions may be suitable for particular subpopulations of tumor cells, spheroids more closely reflect the phenotypic behavior of original tumors than conventional cell cultures [20]. Generation of spheroids is particularly important for sarcomas, because growth rates, cell morphology, cell–cell junctions, and kinase activation of spheroids closely mimic those of primary tumors [21]. Their potential use ranges from tumor drug tests [22,23,24,25] and cell proliferation studies [21,26] to investigations of the role of the microenvironment [27,28]. Furthermore, stem cell spheroids have proven useful for modeling micrometastatic disease and have contributed to our understanding of tumor anoikis, a form of programmed cell death that occurs upon loss of ECM contact [29,30]. Great effort is being expended to develop spheroids in co-culture with endothelial cells, to better study osteosarcoma angiogenesis and metastatic progression [31,32]. Co-cultures composed of tumor spheroids and mesenchymal stem cells are also being used to test novel compounds against tumor dormancy [33,34]. The methods that yield tumor spheroids can be classified into two broad categories: anchorage-dependent and -independent (see Table 1). Anchorage-dependent models utilize engineered scaffolds designed to simulate the ECM and provide structural or physical support. Among the most widespread materials are hydrogels containing proteins and ECM components used to encapsulate cancer cells in microporous scaffolds that mimic the native ECM and enable cells to adhere, proliferate, spread, and migrate in 3D. Generally, hydrogel derivative materials limit the penetration of compounds and exhibit considerable batch-to-batch variability. Some of these limitations may be overcome by the use of covalently modified synthetic hydrogels, often based on polyethylene glycol. Polyethylene glycol dimethacrylate hydrogel microarrays produce homogeneous spheroids with a median size of 50 μm in two to three days. Recently, several groups have developed 3D tumor models in hydrogel scaffolds and used them to assess the potency of a small number of cancer drugs or for small pilot screens of 1500 compounds [35].
Anchorage-independent models are based on the use of mechanical equipment that induces turbulence in the cell culture medium and prevents cells from adhering to solid surfaces or altering the cell–ECM interaction [36]. Another approach is based on the use of nonadherent microculture plates or various semisolid gel-coated Petri dishes that prevent cell binding, or the use of hanging drops [37,38] or microfluid chips [39]. Although these techniques potentially generate thousands of consistent copies of suitable spheroids, not all tumor cell lines spontaneously form 3D spheroids under these conditions [40,41]. Furthermore, many of these methods (e.g., agarose Petri dishes, hanging drops, and rotary cell cultures) generate irregular 3D cellular aggregates with a wide range of morphologies and sizes, whereas regular size is obtained with microfluid chips (see Table 1). More importantly, the time to obtain colonies ranges from one to two weeks (based on tumor type and method) when using 10% fetal calf serum in media, as suggested for single cell lines, and media need to be changed at least two times per week [42]. Moreover, some of these anchorage-independent 3D tumor spheroid methods are rather labor-intensive (e.g., microfluid chips and rotary cultures). Ultra-low-attachment microplates (ULA-plates) are the most promising approach [41]. These plates are coated with a hydrophilic gelatin, are neutrally charged, and support the growth and formation of tight spheroids, compact aggregates, or loose aggregates for a variety of human tumor cell lines. Tumor spheroids formed in 96-well U-bottomed ULA-plates exhibit similar morphology and immunohistochemical staining as spheroids grown in agar, and could be used for tumor cell migration and invasion assays [41]. With this technique, hundreds of homogeneous spheroids can be produced within two to three days in regular tumor cell media. It is therefore currently being adopted for high-throughput drug screening.
2.2. Tumor Organoids
Organoids are three-dimensional models of primary tumor tissue obtained from fresh biopsies. Organoids are generated by mechanical or enzymatic digestion of the original tumor section into small pieces. These are embedded in an extracellular matrix, such as Matrigel, or different types of collagen, where cell–cell interactions predominate over cell–substrate interactions and resemble avascular tumor nodules, or micrometastases, and mimic growth kinetics, gradients of nutrient distribution, oxygen concentration, and cell proliferation. Studies have demonstrated that ultra-low-attachment microplates generate organoids of larger size (300–400 μm), one per well, in a few days (three days if at least 5 × 103 cells are plated), but they were never tested in sarcoma [43]. Organoids retain the structure, morphology, stromal composition, genetic mutations, and heterogeneity of the original tumor [44]. Furthermore, when organoids are transplanted into mice, they form carcinomas that histologically resemble the tumor of origin [44,45]. The opportunity to reproduce in vitro and within a few days both the complex structure of the microenvironment and the chromosome aneuploidies characteristic of individual sarcomas is of great interest, mainly because the environment changes the tumor’s cellular responses to drugs. Numerous assays have been employed to study aspects of 3D tumor organoids, including genetics, biochemistry, and imaging. These techniques have also been used to characterize the effect of anticancer therapeutics in 3D organoids [44,46]. Based on these studies, organoids represent a suitable platform for testing potential drugs on patient-specific tumors. The hypothetical workflow for a clinical organoid screen would be: (1) tumor biopsy, (2) organoid generation and growth, (3) genetic and drug panel screening, (4) response assessment, and (5) selection of the optimal drug for treatment of the patient (Figure 1). The entire process can be completed in a few weeks. This approach overcomes many of the limitations of traditional cancer models and patient-specific xenograft tumors in immunocompromised mice, in particular the high cost, low take-rate, and multi-month experiments required to obtain drug response data [47,48].
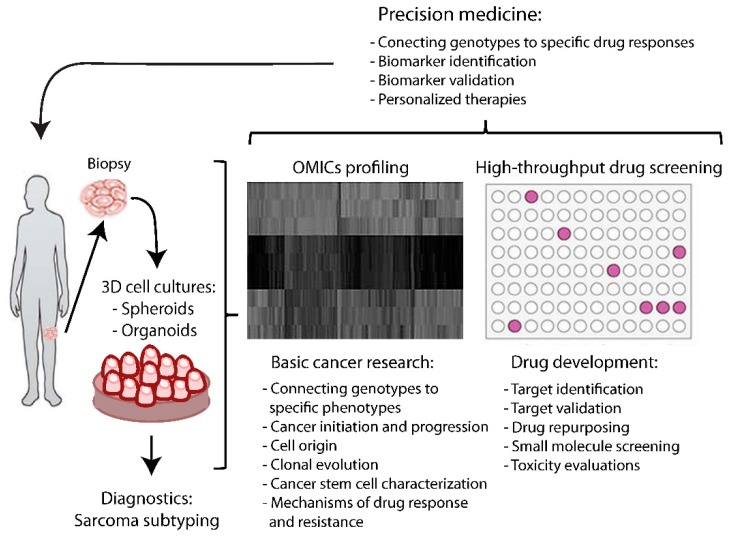
Figure 1.
Workflow from biopsy to personalized medicine. From biopsy, it is possible obtain organoid and spheroid models that are sources of patient-specific DNA, RNA, and proteins (omics profiling). Patient omics may help in connecting genotype to phenotype, in order to select specific mutations, genes, and proteins and identify targets. Spheroids may be directly used for patient drug sensitivity screening and target validation. Integrating omics data and high-throughput drug screening can provide specific molecular and clinical scenarios for better personalized therapy.
3. Implementation of 3D Microenvironments (Hybrid Models for Investigating Angiogenesis, Influence of Immune Cells, and Tumor Dormancy)
Many papers have discussed the differences between two- and three-dimensional cultures and emphasized that the latter model the tumor microenvironment. Several groups have proposed three-dimensional models in which endothelial and fibroblastic cells are co-cultured in the presence of substrates derived from human tumors, such as basement membrane and/or gels rich in collagen or laminin [49,50,51]. One of the most suitable is based on the use of ultra-low-attachment (ULA) plates in combination with the new technologies of automated imaging and analysis. The method consists of plating monolayers of endothelial cells or fibroblasts from different sources and letting tumor cells self-assemble. The ratio between endothelial and tumor cells is generally 1:1. In five days, endothelial cells begin to differentiate, as indicated by the presence of CD34 antigen, and sprout in the inner layer of spheroids [39]. Co-cultures of breast cancer spheroids and human umbilical vein endothelial cells (HUVEC) have already been used to test anticancer drugs targeting epidermal growth factor receptor [52]. However, each tumor type generates different interactions with its neighboring cells and endothelial cells, suggesting the need for a platform for personalized medicine that would account for these differences [53].
Chaddad et al. combined, for the first time, a monolayer of HUVEC with osteosarcoma 3D MG-63 cells using hanging drop techniques. Within five days, co-cultured 3D spheroids expressed extracellular matrix proteins, such as osteocalcin and osteopontin, and led to the establishment of an organized architecture similar to that of tumors encountered in vivo. Furthermore, MG-63 cells cultured in 3D spheroids expressed more bone proteins and vascular endothelial growth factor (VEGF) than in monolayer culture. The architecture of co-cultured spheroids showed cellular activity at the periphery and quiescent cells embedded in matrix at the center of the spheroid. Moreover, the hypoxic core favored the secretion of VEGF, which attracts endothelial cells to the spheroid tumor and promotes formation of vessel-like structures and organization of a vascular network [54]. Spheroids also indicated that the skeletal vascular microenvironment is involved in controlling the fate of tumor cells, active and dormant, and can influence multiple steps within the metastatic cascade [55]. Hybrid models composed of tumor cells, fibroblasts, and immune cells are a novel hot topic. They were primarily developed to investigate reciprocal interactions of regulatory T cell lymphocytes and natural killer cells with luminal and basal phenotype breast cancers [56]. Furthermore, they seem to provide novel efficacy tools for in vitro evaluation of cancer immunotherapy agents, and for investigation of immune cell infiltration and drug targeting [57]. However, they have not yet been tested for sarcomas. Another application of co-cultures and three-dimensional models expected to have a great impact in the near future is the use of mesenchymal stem cell and tumor spheroids to study tumor dormancy [34]. Bone marrow disseminated tumor cells are dormant cancer cells that are harbored in bone marrow niches for years after cancer remission, before potentially returning to a proliferative state and causing cancer recurrence. Currently, there are very few models that recapitulate the dormant phenotype. Buschhaus and co-workers recently used a three-dimensional spheroid-based model co-cultured with mesenchymal stem cells and integrated dual-color bioluminescence imaging to quantify differential cell viability in response to various compounds. They successfully screened for compounds that selectively eliminated cancer cells versus supportive stromal cells, and validated the results by comparing them to efficacy in vivo [34].
4. Bone Tumor Niche
Bone constitutes the microenvironment of several groups of sarcomas and modulates primary tumor growth and metastasis [58]. To recapitulate their features in vitro, several bioengineering methods have been developed to improve 3D models [58]. In bone, mechanical forces generated either from external sources or by cell contractions play important roles in cancer invasion of the bone [59]. Three-dimensional models reproduce the architectural, mechanical, and biochemical elements of the bone microenvironment [60]. These models combine tumor cells from patients and bone scaffolds from different sources [61]. In some models, the scaffold consists of decellularized bovine bone precoated with human mesenchymal cells, a peculiar system that allows prolonged culture (four weeks) [62]. Cell proliferation within scaffolds more closely approximates the real Ewing sarcoma cell growth rate, which is significantly less than that of monolayer cultures [63]. Scaffolds also reproduce the physiological exchange of nutrients, oxygen, and metabolic waste byproducts, and ideally are compatible with standard experimental techniques (e.g., microscopy, immunohistochemistry, cell proliferation assays) [64]. A three-dimensional bone model of Ewing sarcoma was shown to maintain the immunohistochemical biomarkers normally expressed (CD99+, IGF-1R+, keratin−, and SMA−) [65]. Furthermore, proteomic expression profiles along the IGF-1R/PI3K/mTOR signaling pathway suggest that 3D scaffolds can reliably mimic critical signaling cascades in human Ewing sarcoma tumors [66]. Similar observations were made in breast cancer metastasis cells grown in 3D cultures [67]. This bioengineered human tumor model can potentially improve upon the current preclinical drug-screening paradigm by providing valuable information about new therapeutic targets and anticancer drug efficacy in primary bone tumor and metastasis. However, one of the most important questions yet to be resolved is whether the 3D bone model shares enough hypoxic fidelity to be useful as a preclinical high-throughput drug testing platform. Hypoxia per se stimulates blood cell proliferation and blood vessel formation, and modulates the expression of extracellular matrix components. To date, only a few reports have considered bone hypoxic conditions in preclinical studies and three-dimensional in vitro models [68].
5. Applications for Sarcoma Biology Research
5.1. Functional Genomic Analysis
The sarcoma genome is complex, with a large number of chromosomal variations and a relatively small number of recurring exonic mutations [69]. Some mutations and genomic rearrangements contribute diagnostic information and may help to identify targeted treatment [69]. Assessing drug effects in 2D cultures is difficult, mainly because the small number of available tumor cell lines cannot represent the genetic diversity of highly heterogeneous sarcomas. Such cancer cell lines are generally limited to the most common subtypes, and most of the cell lines available were isolated from very aggressive tumors that do not represent low-grade tumors. Specific cell lines or cells isolated from a small number of patients therefore cannot truly represent the pathology, and data from a larger number of tumors and more diverse tumors are necessary to establish their carcinogenic mechanisms and drug responses. In recent years, patient-derived xenograft (PDX) models have proven useful to study the histology of some sarcomas [70]. For these PDX models, a tumor mass from a patient is directly implanted into the subcutaneous tissue of a severe combined immunodeficiency mouse, which is followed by tumor growth. Upon reaching a sufficient mass, tumors are explanted, divided into smaller samples, and reimplanted for subsequent passage in mice. Therefore, a small piece of tumor can be propagated to achieve a tumor mass manyfold greater than that of the original tumor. Comprehensive genomewide gene expression analyses have shown that tumors from PDX models at an early passage have expression profiles that are very close to those of the original tumors [70]. Some investigators have integrated PDX with in vitro genome profile to identifying factors that underlie heterogeneous patient responses, and have thus identified associations between a genotype and drug response, as well as mechanisms of resistance in breast cancer [47]. This approach could therefore be useful for personalized patient treatment, especially in tumors with low numbers of mutations, such as gastrointestinal stromal tumor sarcomas. The same approach, however, is less practicable for some tumors with higher chromosome instability and a prominent involvement of immune cells, such as giant-cell tumors of bone.
One opportunity for such sarcomas could be the use of multicellular spheroids and organoids from patients to assess both genetic profiling and drug responses. This combination therefore provides a promising approach to assess the relevance of specific mutations and to test patient-specific drug responses at the bedside. In fact, sequences of spheroids from sarcomas showed that they retain the genetic signature of the patient’s tumor and are a readily available source of high-quality DNA and RNA for next-generation sequencing [71]. Furthermore, gene-specific silencing may be introduced in spheroids by different techniques, such as small interfering RNA or CRISPR-Cas9, in order to assess their functional role in the pathogenesis of sarcomas [72,73]. The latter approach can be particularly useful to study genetic variants, epigenetic alterations, or even changes in chromatin structure, and to develop specific treatments. For example, Hanes and colleagues selected targetable substrates based on tumor genomic profiling. Using patient-derived cell lines, they first profiled the genomes and selected a target. They then tested cell sensitivity to target-specific drugs in vitro, and thus demonstrated the benefit of combining tumor genomic profiles and in vitro drug testing [74]. These results also support the idea that better classification of patients based on a personalized model could help in choosing the best treatment for sarcomas [75]. Proteomics represents another molecular approach to selecting biomarkers of sarcoma progression and therapy. Several research groups have focused on differential expression of proteins in tumor tissues, using various approaches [74,76], and stratified patients based on histology and grade [77]. Toward this goal, a multi-institutional consortium has been established that will provide in-depth analysis of existing genomic databases, proteomic data analysis, and statistical support, and prioritize and track the discovered targets.
However, these integrated approaches do not select therapies, nor do they indicate the best treatment for a single patient. Spheroid models offer the opportunity to profile both genomic and proteomic profiles individually and to determine the best drug from the same biopsy. Therefore, they seem to be a more promising way toward more effective treatment of rare sarcomas.
5.2. Preclinical Drug Screening
As previously emphasized, the drug sensitivity of tumor cells is strongly affected by microenvironmental factors [78,79]. The spheroid approach is of special interest for the treatment of bone sarcomas, which are particularly drug resistant due to the presence of the bone barrier and tumor heterogeneity [80]. As proof of concept, a multicellular spheroid model of osteosarcoma was used to evaluate the anticancer efficacy of VOchrys compared to cis-platinum [81]. In this study, a vanadium (IV) complex with the flavonoid chrysin displayed better effect than cis-platinum in osteosarcoma spheroids, because VOchrys altered the shape of spheroids and decreased their viability. The pharmacological effects were also confirmed in a xenograft model, which showed a significant reduction of tumor size. These results demonstrate that spheroid models can be predictive of drug activity and that it is possible to measure drug efficacy in multiple cells that compose osteosarcomas [81].
Another particular aggressive and drug-resistant sarcoma type is the chondrosarcoma. The chemoresistance of cartilage tumors results from phenotypic microenvironmental features of the tumor tissue, mainly the chondrogenic extracellular matrix (ECM) and hypoxia. In an interesting study by Voissiere et al., both 2D and 3D chondrosarcoma models were tested with doxorubicin alone or in combination with TH-302, a pro-drug activated in hypoxia [25]. Spheroids developed much earlier resistance to doxorubicin than two-dimensional cell cultures, due to a limited penetration of the drug into the deeper layers of spheroids as a result of cell adhesion between tumor and stroma cells in the 3D systems [82,83]. In contrast, spheroids were sensitive to TH-302. Interestingly, larger spheroids were more sensitive to TH-302 (multicellular resistance index (MCRI) = 7.7) than smaller hypoxic spheroids (MCRI = 9.1) [25]. The authors speculated that the drug resistance could also be due to the presence of layers of cells in different stages of the cell cycle [84]. It therefore seems that a better understanding of the molecular pathways governing cell adhesion and ECM in sarcomas would be of interest and may lead to the identification of new targets in the stroma, including stromal cells, ECM entities, matrix-degrading proteases and inhibitors, and regulatory substances [85]
Most studies on spheroids as models for in vitro tumor drug tests indicate several advantages (also see Table 1). The first is the possibility to generate, from a single biopsy, multiple spheroids identical in structure, morphology, and microenvironment. The second advantage is that drug response can be measured in microenvironments or on cell subpopulations isolated from different spheroid regions [40,86,87,88,89,90]. Spheroids cultured on confluent endothelial cells were used to test drugs that affect tumor cell evasion and sprouting phenomena in vitro [91]. Incubation of spheroid cultures with immune cell suspensions is another interesting approach to mimic local immune responses, and to test penetration, local distribution, and the effect on tumor cells of antibody-based treatments [92,93]. The third advantage is that the spherical symmetry simplifies the mathematical analysis to predict radiation response [94], drug penetration, and binding/activity [30,94,95]. Another area of interest is the use of spheroids derived from normal untransformed cells, such as hepatocytes/liver [96,97] or chondrocytes/cartilage [98], to study organ or tissue development, or to evaluate drug selectivity and specificity, by comparing them to tumor spheroids [86]. Following drug uptake in individuals, spheroids could also be used to evaluate the effective diffusion coefficients. Analogous to monolayer cellular assays, easy multiwell systems are available to screen drug effects, such as cytotoxicity, proliferation, binding, apoptosis, and adenosine triphosphate levels in spheroids [99].
Given the similarities between results in 3D models and xenographs, pharmaceutical companies have developed platforms and chips to screen several different therapeutics. Large-scale 3D tumor spheroids represent a preclinical testing pipeline to determine a drug candidate’s activity, toxicity, and pharmacokinetic profile in high-throughput drug screens [100]. Additionally, they may also help to reduce side effects. Furthermore, maintaining multiple organoids from the same patients in culture allows later investigation of treatment-induced selection processes and potential resistance mechanisms [101] to be carried out. A preliminary analysis of the SpheroNEO breast cancer study cohort (172 patient spheroids) showed a predictive response to trastuzumab-based therapy, but was also selective in discerning ineffective from effective treatment options [102].
Some limitations of laboratory methodology have to be acknowledged. The main difficulty is obtaining the minimal number of cells required for a reliable assay outcome from surgical specimens that vary from patient to patient and depend on the anatomical location. The minimum number of tumor cells used in all studies cited here was 5000. Furthermore, the methods have to be customized based on tumor histology. Ultra-low-attachment plates seem to be the best to obtain a homogeneous size of organoids in four to five days. From a clinical standpoint, cancer spheroids have to be stable for two to three weeks in order to be able to perform all screening. This may not always be possible, except for engineered bone scaffold models that can survive for one month. In this regard, it is noteworthy that several groups are working to establish organoid banks [103,104,105].
Three-dimensional models to assess patients’ individual responses to radiotherapy may also become a future tool for personalized treatment [99,100,101]. Chemoradiation currently serves as first-line therapy for advanced and chemoresistant chondrosarcoma, while new chemotherapy regimens are emerging. However, response rates for any treatment are difficult to predict and have broad variation, which could be improved by using 3D models.
6. Clinical Opportunities
Several studies have indicated that short-term 3D cell cultures have superior predictive value in the preclinical arena over in vitro models and are comparable to xenographs. Therefore, several cancer centers around the world have started to determine patient-specific 3D cell culture data [106]. Some have explored the molecular characteristics of individual patients’ tumor spheroids or organoids, using them as a platform for drug screening in an automated setup to identify new biomarkers and potential drug targets [107]. Because the screening, integration of genotype-specific drug discovery, and in silico validation take a few weeks, these approaches have the potential to select the most appropriate individual treatment concurrent with the initial treatment and may then influence further therapy. However, it should be emphasized that personalized medicine could not only offer therapeutic value to patients and their oncologists, but at the same time help to gain a better understanding of their specific tumors. Although a perfect preclinical cancer model may be unattainable within the limitations imposed by the amount of fresh tissue that can be safely obtained, spheroid models greatly expand the spectrum of cancer subtypes that can be modeled and offer new possibilities for drug discovery and personalized medicine for rare cancers, such as sarcomas.
Acknowledgments
We thank AIRC for Cimmino’s Grant MFAG 11510.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Mohseny A.B., Hogendoorn P.C. Concise review: Mesenchymal tumors: When stem cells go mad. Stem Cells. 2011;29:397–403. doi: 10.1002/stem.596. [DOI] [PubMed] [Google Scholar]
- 2.Stiller C.A., Trama A., Serraino D., Rossi S., Navarro C., Chirlaque M.D., Casali P.G., The RARECARE Working Group Descriptive epidemiology of sarcomas in europe: Report from the rarecare project. Eur. J. Cancer. 2013;49:684–695. doi: 10.1016/j.ejca.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 3.Gatta G., Ciccolallo L., Kunkler I., Capocaccia R., Berrino F., Coleman M.P., De Angelis R., Faivre J., Lutz J.M., Martinez C., et al. Survival from rare cancer in adults: a population-based study. Lancet Oncol. 2006;7:132–140. doi: 10.1016/S1470-2045(05)70471-X. [DOI] [PubMed] [Google Scholar]
- 4.Mastrangelo G., Coindre J.M., Ducimetiere F., Dei Tos A.P., Fadda E., Blay J.Y., Buja A., Fedeli U., Cegolon L., Frasson A., et al. Incidence of soft tissue sarcoma and beyond: A population-based prospective study in 3 european regions. Cancer. 2012;118:5339–5348. doi: 10.1002/cncr.27555. [DOI] [PubMed] [Google Scholar]
- 5.Dancsok A.R., Asleh-Aburaya K., Nielsen T.O. Advances in sarcoma diagnostics and treatment. Oncotarget. 2017;8:7068–7093. doi: 10.18632/oncotarget.12548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerlinger M., Rowan A.J., Horswell S., Math M., Larkin J., Endesfelder D., Gronroos E., Martinez P., Matthews N., Stewart A., et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N. Engl. J. Med. 2012;366:883–892. doi: 10.1056/NEJMoa1113205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanahan D., Coussens L.M. Accessories to the crime: Functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309–322. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 8.Fazioli F., Colella G., Miceli R., Di Salvatore M.G., Gallo M., Boccella S., De Chiara A., Ruosi C., de Nigris F. Post-surgery fluids promote transition of cancer stem cell-to-endothelial and akt/mtor activity, contributing to relapse of giant cell tumors of bone. Oncotarget. 2017;8:85040–85053. doi: 10.18632/oncotarget.18783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salawu A., Fernando M., Hughes D., Reed M.W., Woll P., Greaves C., Day C., Alhajimohammed M., Sisley K. Establishment and molecular characterisation of seven novel soft-tissue sarcoma cell lines. Br. J. Cancer. 2016;115:1058–1068. doi: 10.1038/bjc.2016.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruland O., Fodstad O., Pihl A. The use of multicellular spheroids in establishing human sarcoma cell lines in vitro. Int. J. Cancer. 1985;35:793–798. doi: 10.1002/ijc.2910350616. [DOI] [PubMed] [Google Scholar]
- 11.Costa E.C., Gaspar V.M., Coutinho P., Correia I.J. Optimization of liquid overlay technique to formulate heterogenic 3D co-cultures models. Biotechnol. Bioeng. 2014;111:1672–1685. doi: 10.1002/bit.25210. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig K., Tse E.S., Wang J.Y. Colon cancer cells adopt an invasive phenotype without mesenchymal transition in 3-D but not 2-D culture upon combined stimulation with EGF and crypt growth factors. BMC Cancer. 2013;13:221. doi: 10.1186/1471-2407-13-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amann A., Zwierzina M., Gamerith G., Bitsche M., Huber J.M., Vogel G.F., Blumer M., Koeck S., Pechriggl E.J., Kelm J.M., et al. Development of an innovative 3d cell culture system to study tumour—Stroma interactions in non-small cell lung cancer cells. PLoS ONE. 2014;9:e92511. doi: 10.1371/journal.pone.0092511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dufau I., Frongia C., Sicard F., Dedieu L., Cordelier P., Ausseil F., Ducommun B., Valette A. Multicellular tumor spheroid model to evaluate spatio-temporal dynamics effect of chemotherapeutics: Application to the gemcitabine/CHK1 inhibitor combination in pancreatic cancer. BMC Cancer. 2012;12:15. doi: 10.1186/1471-2407-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shankar S., Nall D., Tang S.N., Meeker D., Passarini J., Sharma J., Srivastava R.K. Resveratrol inhibits pancreatic cancer stem cell characteristics in human and KrasG12D transgenic mice by inhibiting pluripotency maintaining factors and epithelial-mesenchymal transition. PLoS ONE. 2011;6:e16530. doi: 10.1371/journal.pone.0016530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takagi A., Watanabe M., Ishii Y., Morita J., Hirokawa Y., Matsuzaki T., Shiraishi T. Three-dimensional cellular spheroid formation provides human prostate tumor cells with tissue-like features. Anticancer Res. 2007;27:45–53. [PubMed] [Google Scholar]
- 17.Clevers H. Modeling development and disease with organoids. Cell. 2016;165:1586–1597. doi: 10.1016/j.cell.2016.05.082. [DOI] [PubMed] [Google Scholar]
- 18.Lamichhane S.P., Arya N., Kohler E., Xiang S., Christensen J., Shastri V.P. Recapitulating epithelial tumor microenvironment in vitro using three dimensional tri-culture of human epithelial, endothelial, and mesenchymal cells. BMC Cancer. 2016;16:581. doi: 10.1186/s12885-016-2634-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kolb E.A., Gorlick R., Maris J.M., Keir S.T., Morton C.L., Wu J., Wozniak A.W., Smith M.A., Houghton P.J. Combination testing (stage 2) of the anti-IGF-1 receptor antibody IMC-A12 with rapamycin by the pediatric preclinical testing program. Pediatr. Blood Cancer. 2012;58:729–735. doi: 10.1002/pbc.23157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamilton G. Multicellular spheroids as an in vitro tumor model. Cancer Lett. 1998;131:29–34. doi: 10.1016/S0304-3835(98)00198-0. [DOI] [PubMed] [Google Scholar]
- 21.Lawlor E.R., Scheel C., Irving J., Sorensen P.H. Anchorage-independent multi-cellular spheroids as an in vitro model of growth signaling in Ewing tumors. Oncogene. 2002;21:307–318. doi: 10.1038/sj.onc.1205053. [DOI] [PubMed] [Google Scholar]
- 22.Villaverde M.S., Gil-Cardeza M.L., Glikin G.C., Finocchiaro L.M. Interferon-β lipofection I. Increased efficacy of chemotherapeutic drugs on human tumor cells derived monolayers and spheroids. Cancer Gene Ther. 2012;19:508–516. doi: 10.1038/cgt.2012.27. [DOI] [PubMed] [Google Scholar]
- 23.Awad O., Yustein J.T., Shah P., Gul N., Katuri V., O’Neill A., Kong Y., Brown M.L., Toretsky J.A., Loeb D.M. High ALDH activity identifies chemotherapy-resistant Ewing's sarcoma stem cells that retain sensitivity to EWS-FLI1 inhibition. PLoS ONE. 2010;5:e13943. doi: 10.1371/journal.pone.0013943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zanoni M., Piccinini F., Arienti C., Zamagni A., Santi S., Polico R., Bevilacqua A., Tesei A. 3D tumor spheroid models for in vitro therapeutic screening: A systematic approach to enhance the biological relevance of data obtained. Sci. Rep. 2016;6:19103. doi: 10.1038/srep19103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Voissiere A., Jouberton E., Maubert E., Degoul F., Peyrode C., Chezal J.M., Miot-Noirault E. Development and characterization of a human three-dimensional chondrosarcoma culture for in vitro drug testing. PLoS ONE. 2017;12:e0181340. doi: 10.1371/journal.pone.0181340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strauss S.J., Ng T., Mendoza-Naranjo A., Whelan J., Sorensen P.H. Understanding micrometastatic disease and anoikis resistance in Ewing family of tumors and osteosarcoma. Oncologist. 2010;15:627–635. doi: 10.1634/theoncologist.2010-0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holmes T.D., El-Sherbiny Y.M., Davison A., Clough S.L., Blair G.E., Cook G.P. A human NK cell activation/inhibition threshold allows small changes in the target cell surface phenotype to dramatically alter susceptibility to NK cells. J. Immunol. 2011;186:1538–1545. doi: 10.4049/jimmunol.1000951. [DOI] [PubMed] [Google Scholar]
- 28.Kailayangiri S., Altvater B., Meltzer J., Pscherer S., Luecke A., Dierkes C., Titze U., Leuchte K., Landmeier S., Hotfilder M., et al. The ganglioside antigen Gd2 is surface-expressed in Ewing sarcoma and allows for MHC-independent immune targeting. Br. J. Cancer. 2012;106:1123–1133. doi: 10.1038/bjc.2012.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang H.G., Jenabi J.M., Zhang J., Keshelava N., Shimada H., May W.A., Ng T., Reynolds C.P., Triche T.J., Sorensen P.H. E-cadherin cell-cell adhesion in ewing tumor cells mediates suppression of anoikis through activation of the ErbB4 tyrosine kinase. Cancer Res. 2007;67:3094–3105. doi: 10.1158/0008-5472.CAN-06-3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Graff C.P., Wittrup K.D. Theoretical analysis of antibody targeting of tumor spheroids: Importance of dosage for penetration, and affinity for retention. Cancer Res. 2003;63:1288–1296. [PubMed] [Google Scholar]
- 31.De Nigris F., Rossiello R., Schiano C., Arra C., Williams-Ignarro S., Barbieri A., Lanza A., Balestrieri A., Giuliano M.T., Ignarro L.J., et al. Deletion of Yin Yang 1 protein in osteosarcoma cells on cell invasion and CXCR4/angiogenesis and metastasis. Cancer Res. 2008;68:1797–1808. doi: 10.1158/0008-5472.CAN-07-5582. [DOI] [PubMed] [Google Scholar]
- 32.De Nigris F., Crudele V., Giovane A., Casamassimi A., Giordano A., Garban H.J., Cacciatore F., Pentimalli F., Marquez-Garban D.C., Petrillo A., et al. CXCR4/YY1 inhibition impairs VEGF network and angiogenesis during malignancy. Proc. Natl. Acad. Sci. USA. 2010;107:14484–14489. doi: 10.1073/pnas.1008256107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hassell B.A., Goyal G., Lee E., Sontheimer-Phelps A., Levy O., Chen C.S., Ingber D.E. Human organ chip models recapitulate orthotopic lung cancer growth, therapeutic responses, and tumor dormancy in vitro. Cell. Rep. 2017;21:508–516. doi: 10.1016/j.celrep.2017.09.043. [DOI] [PubMed] [Google Scholar]
- 34.Buschhaus J.M., Luker K.E., Luker G.D. A facile, in vitro 384-well plate system to model disseminated tumor cells in the bone marrow microenvironment. Methods Mol. Biol. 2018;1686:201–213. doi: 10.1007/978-1-4939-7371-2_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh M., Mukundan S., Jaramillo M., Oesterreich S., Sant S. Three-dimensional breast cancer models mimic hallmarks of size-induced tumor progression. Cancer Res. 2016;76:3732–3743. doi: 10.1158/0008-5472.CAN-15-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu G., Li D. Three-dimensional modeling of transport of nutrients for multicellular tumor spheroid culture in a microchannel. Biomed. Microdevices. 2007;9:315–323. doi: 10.1007/s10544-006-9035-1. [DOI] [PubMed] [Google Scholar]
- 37.Timmins N.E., Nielsen L.K. Generation of multicellular tumor spheroids by the hanging-drop method. Methods Mol. Med. 2007;140:141–151. doi: 10.1007/978-1-59745-443-8_8. [DOI] [PubMed] [Google Scholar]
- 38.Kelm J.M., Timmins N.E., Brown C.J., Fussenegger M., Nielsen L.K. Method for generation of homogeneous multicellular tumor spheroids applicable to a wide variety of cell types. Biotechnol. Bioeng. 2003;83:173–180. doi: 10.1002/bit.10655. [DOI] [PubMed] [Google Scholar]
- 39.Caplin J.D., Granados N.G., James M.R., Montazami R., Hashemi N. Microfluidic organ-on-a-chip technology for advancement of drug development and toxicology. Adv. Healthc. Mater. 2015;4:1426–1450. doi: 10.1002/adhm.201500040. [DOI] [PubMed] [Google Scholar]
- 40.Friedrich J., Seidel C., Ebner R., Kunz-Schughart L.A. Spheroid-based drug screen: Considerations and practical approach. Nat. Protoc. 2009;4:309–324. doi: 10.1038/nprot.2008.226. [DOI] [PubMed] [Google Scholar]
- 41.Vinci M., Gowan S., Boxall F., Patterson L., Zimmermann M., Court W., Lomas C., Mendiola M., Hardisson D., Eccles S.A. Advances in establishment and analysis of three-dimensional tumor spheroid-based functional assays for target validation and drug evaluation. BMC Biol. 2012;10:29. doi: 10.1186/1741-7007-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lovitt C.J., Shelper T.B., Avery V.M. Advanced cell culture techniques for cancer drug discovery. Biology (Basel) 2014;3:345–367. doi: 10.3390/biology3020345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fatehullah A., Tan S.H., Barker N. Organoids as an in vitro model of human development and disease. Nat. Cell. Biol. 2016;18:246–254. doi: 10.1038/ncb3312. [DOI] [PubMed] [Google Scholar]
- 44.Gaebler M., Silvestri A., Haybaeck J., Reichardt P., Lowery C.D., Stancato L.F., Zybarth G., Regenbrecht C.R.A. Three-dimensional patient-derived in vitro sarcoma models: Promising tools for improving clinical tumor management. Front. Oncol. 2017;7:203. doi: 10.3389/fonc.2017.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stewart E., Federico S.M., Chen X., Shelat A.A., Bradley C., Gordon B., Karlstrom A., Twarog N.R., Clay M.R., Bahrami A., et al. Orthotopic patient-derived xenografts of paediatric solid tumours. Nature. 2017;549:96–100. doi: 10.1038/nature23647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hong A.L., Tseng Y.Y., Cowley G.S., Jonas O., Cheah J.H., Kynnap B.D., Doshi M.B., Oh C., Meyer S.C., Church A.J., et al. Integrated genetic and pharmacologic interrogation of rare cancers. Nat. Commun. 2016;7:11987. doi: 10.1038/ncomms11987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gao H., Korn J.M., Ferretti S., Monahan J.E., Wang Y., Singh M., Zhang C., Schnell C., Yang G., Zhang Y., et al. High-throughput screening using patient-derived tumor xenografts to predict clinical trial drug response. Nat. Med. 2015;21:1318–1325. doi: 10.1038/nm.3954. [DOI] [PubMed] [Google Scholar]
- 48.Aparicio S., Hidalgo M., Kung A.L. Examining the utility of patient-derived xenograft mouse models. Nat. Rev. Cancer. 2015;15:311–316. doi: 10.1038/nrc3944. [DOI] [PubMed] [Google Scholar]
- 49.Reddy K., Zhou Z., Jia S.F., Lee T.H., Morales-Arias J., Cao Y., Kleinerman E.S. Stromal cell-derived factor-1 stimulates vasculogenesis and enhances Ewing's sarcoma tumor growth in the absence of vascular endothelial growth factor. Int. J. Cancer. 2008;123:831–837. doi: 10.1002/ijc.23582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee T.H., Bolontrade M.F., Worth L.L., Guan H., Ellis L.M., Kleinerman E.S. Production of VEGF165 by Ewing's sarcoma cells induces vasculogenesis and the incorporation of CD34+ stem cells into the expanding tumor vasculature. Int. J. Cancer. 2006;119:839–846. doi: 10.1002/ijc.21916. [DOI] [PubMed] [Google Scholar]
- 51.De Nigris F., Mancini F.P., Schiano C., Infante T., Zullo A., Minucci P.B., Al-Omran M., Giordano A., Napoli C. Osteosarcoma cells induce endothelial cell proliferation during neo-angiogenesis. J. Cell. Physiol. 2013;228:846–852. doi: 10.1002/jcp.24234. [DOI] [PubMed] [Google Scholar]
- 52.Howes A.L., Richardson R.D., Finlay D., Vuori K. 3-dimensional culture systems for anti-cancer compound profiling and high-throughput screening reveal increases in EGFR inhibitor-mediated cytotoxicity compared to monolayer culture systems. PLoS One. 2014;9:e108283. doi: 10.1371/journal.pone.0108283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shoval H., Karsch-Bluman A., Brill-Karniely Y., Stern T., Zamir G., Hubert A., Benny O. Tumor cells and their crosstalk with endothelial cells in 3D spheroids. Sci. Rep. 2017;7:10428. doi: 10.1038/s41598-017-10699-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chaddad H., Kuchler-Bopp S., Fuhrmann G., Gegout H., Ubeaud-Sequier G., Schwinte P., Bornert F., Benkirane-Jessel N., Idoux-Gillet Y. Combining 2D angiogenesis and 3D osteosarcoma microtissues to improve vascularization. Exp. Cell. Res. 2017;360:138–145. doi: 10.1016/j.yexcr.2017.08.035. [DOI] [PubMed] [Google Scholar]
- 55.Kusumbe A.P. Vascular niches for disseminated tumour cells in bone. J. Bone Oncol. 2016;5:112–116. doi: 10.1016/j.jbo.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Augustine T.N., Dix-Peek T., Duarte R., Candy G.P. Establishment of a heterotypic 3D culture system to evaluate the interaction of TREG lymphocytes and NK cells with breast cancer. J. Immunol. Methods. 2015;426:1–13. doi: 10.1016/j.jim.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 57.Herter S., Morra L., Schlenker R., Sulcova J., Fahrni L., Waldhauer I., Lehmann S., Reislander T., Agarkova I., Kelm J.M., et al. A novel three-dimensional heterotypic spheroid model for the assessment of the activity of cancer immunotherapy agents. Cancer Immunol. Immunother. 2017;66:129–140. doi: 10.1007/s00262-016-1927-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Villasante A., Vunjak-Novakovic G. Tissue-engineered models of human tumors for cancer research. Expert Opin. Drug Discov. 2015;10:257–268. doi: 10.1517/17460441.2015.1009442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tse J.M., Cheng G., Tyrrell J.A., Wilcox-Adelman S.A., Boucher Y., Jain R.K., Munn L.L. Mechanical compression drives cancer cells toward invasive phenotype. Proc. Natl. Acad. Sci. USA. 2012;109:911–916. doi: 10.1073/pnas.1118910109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gill B.J., West J.L. Modeling the tumor extracellular matrix: Tissue engineering tools repurposed towards new frontiers in cancer biology. J. Biomech. 2014;47:1969–1978. doi: 10.1016/j.jbiomech.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 61.Rocco G., Martucci N., La Rocca A., La Manna C., De Luca G., Fazioli F., Mori S. Postoperative local morbidity and the use of vacuum-assisted closure after complex chest wall reconstructions with new and conventional materials. Ann. Thorac. Surg. 2014;98:291–296. doi: 10.1016/j.athoracsur.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 62.Marturano-Kruik A., Villasante A., Vunjak-Novakovic G. Bioengineered models of solid human tumors for cancer research. Methods Mol. Biol. 2016;1502:203–211. doi: 10.1007/7651_2016_353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fong E.L., Lamhamedi-Cherradi S.E., Burdett E., Ramamoorthy V., Lazar A.J., Kasper F.K., Farach-Carson M.C., Vishwamitra D., Demicco E.G., Menegaz B.A., et al. Modeling ewing sarcoma tumors in vitro with 3D scaffolds. Proc. Natl. Acad. Sci. USA. 2013;110:6500–6505. doi: 10.1073/pnas.1221403110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Infanger D.W., Lynch M.E., Fischbach C. Engineered culture models for studies of tumor-microenvironment interactions. Annu. Rev. Biomed. Eng. 2013;15:29–53. doi: 10.1146/annurev-bioeng-071811-150028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Santoro M., Lamhamedi-Cherradi S.E., Menegaz B.A., Ludwig J.A., Mikos A.G. Flow perfusion effects on three-dimensional culture and drug sensitivity of Ewing sarcoma. Proc. Natl. Acad. Sci. USA. 2015;112:10304–10309. doi: 10.1073/pnas.1506684112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lamhamedi-Cherradi S.E., Santoro M., Ramammoorthy V., Menegaz B.A., Bartholomeusz G., Iles L.R., Amin H.M., Livingston J.A., Mikos A.G., Ludwig J.A. 3D tissue-engineered model of Ewing's sarcoma. Adv. Drug Deliv. Rev. 2014;79–80:155–171. doi: 10.1016/j.addr.2014.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dit Faute M.A., Laurent L., Ploton D., Poupon M.F., Jardillier J.C., Bobichon H. Distinctive alterations of invasiveness, drug resistance and cell-cell organization in 3D-cultures of MCF-7, a human breast cancer cell line, and its multidrug resistant variant. Clin. Exp. Metastasis. 2002;19:161–168. doi: 10.1023/A:1014594825502. [DOI] [PubMed] [Google Scholar]
- 68.Infante T., Mancini F.P., Lanza A., Soricelli A., de Nigris F., Napoli C. Polycomb YY1 is a critical interface between epigenetic code and miRNA machinery after exposure to hypoxia in malignancy. Biochim. Biophys. Acta. 2015;1853:975–986. doi: 10.1016/j.bbamcr.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 69.Barretina J., Taylor B.S., Banerji S., Ramos A.H., Lagos-Quintana M., Decarolis P.L., Shah K., Socci N.D., Weir B.A., Ho A., et al. Subtype-specific genomic alterations define new targets for soft-tissue sarcoma therapy. Nat. Genet. 2010;42:715–721. doi: 10.1038/ng.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Qi Y., Hu Y., Yang H., Zhuang R., Hou Y., Tong H., Feng Y., Huang Y., Jiang Q., Ji Q., et al. Establishing a patient-derived xenograft model of human myxoid and round-cell liposarcoma. Oncotarget. 2017;8:54320–54330. doi: 10.18632/oncotarget.17352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jour G., Scarborough J.D., Jones R.L., Loggers E., Pollack S.M., Pritchard C.C., Hoch B.L. Molecular profiling of soft tissue sarcomas using next-generation sequencing: A pilot study toward precision therapeutics. Hum. Pathol. 2014;45:1563–1571. doi: 10.1016/j.humpath.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 72.Horman S.R., To J., Orth A.P., Slawny N., Cuddihy M.J., Caracino D. High-content analysis of three-dimensional tumor spheroids: Investigating signaling pathways using small hairpin RNA. Nature Methods. 2013;10:v–vi. doi: 10.1038/nmeth.f.370. [DOI] [Google Scholar]
- 73.Liu T., Shen J.K., Li Z., Choy E., Hornicek F.J., Duan Z. Development and potential applications of CRISPR-Cas9 genome editing technology in sarcoma. Cancer Lett. 2016;373:109–118. doi: 10.1016/j.canlet.2016.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hanes R., Grad I., Lorenz S., Stratford E.W., Munthe E., Reddy C.C., Meza-Zepeda L.A., Myklebost O. Preclinical evaluation of potential therapeutic targets in dedifferentiated liposarcoma. Oncotarget. 2016;7:54583–54595. doi: 10.18632/oncotarget.10518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Drost J., van Jaarsveld R.H., Ponsioen B., Zimberlin C., van Boxtel R., Buijs A., Sachs N., Overmeer R.M., Offerhaus G.J., Begthel H., et al. Sequential cancer mutations in cultured human intestinal stem cells. Nature. 2015;521:43–47. doi: 10.1038/nature14415. [DOI] [PubMed] [Google Scholar]
- 76.Treindl F., Ruprecht B., Beiter Y., Schultz S., Dottinger A., Staebler A., Joos T.O., Kling S., Poetz O., Fehm T., et al. A bead-based western for high-throughput cellular signal transduction analyses. Nat. Commun. 2016;7:12852. doi: 10.1038/ncomms12852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kondo T., Kawaib A. A proteomics approach for the development of sarcoma biomarkers. EuPA Open Proteom. 2014;4:121–128. doi: 10.1016/j.euprot.2014.06.004. [DOI] [Google Scholar]
- 78.Oudar O. Spheroids: Relation between tumour and endothelial cells. Crit. Rev. Oncol. Hematol. 2000;36:99–106. doi: 10.1016/S1040-8428(00)00080-9. [DOI] [PubMed] [Google Scholar]
- 79.Furbert-Harris P.M., Laniyan I., Harris D., Dunston G.M., Vaughn T., Abdelnaby A., Parish-Gause D., Oredipe O.A. Activated eosinophils infiltrate MCF-7 breast multicellular tumor spheroids. Anticancer Res. 2003;23:71–78. [PubMed] [Google Scholar]
- 80.Arai K., Sakamoto R., Kubota D., Kondo T. Proteomic approach toward molecular backgrounds of drug resistance of osteosarcoma cells in spheroid culture system. Proteomics. 2013;13:2351–2360. doi: 10.1002/pmic.201300053. [DOI] [PubMed] [Google Scholar]
- 81.Leon I.E., Cadavid-Vargas J.F., Resasco A., Maschi F., Ayala M.A., Carbone C., Etcheverry S.B. In vitro and in vivo antitumor effects of the VO-chrysin complex on a new three-dimensional osteosarcoma spheroids model and a xenograft tumor in mice. J. Biol. Inorg. Chem. 2016;21:1009–1020. doi: 10.1007/s00775-016-1397-0. [DOI] [PubMed] [Google Scholar]
- 82.Westhoff M.A., Fulda S. Adhesion-mediated apoptosis resistance in cancer. Drug Resist. Updat. 2009;12:127–136. doi: 10.1016/j.drup.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 83.McMillin D.W., Negri J.M., Mitsiades C.S. The role of tumour-stromal interactions in modifying drug response: Challenges and opportunities. Nat. Rev. Drug Discov. 2013;12:217–228. doi: 10.1038/nrd3870. [DOI] [PubMed] [Google Scholar]
- 84.Benien P., Swami A. 3D tumor models: History, advances and future perspectives. Future Oncol. 2014;10:1311–1327. doi: 10.2217/fon.13.274. [DOI] [PubMed] [Google Scholar]
- 85.Hiscox S., Barrett-Lee P., Nicholson R.I. Therapeutic targeting of tumor-stroma interactions. Expert Opin. Ther. Targets. 2011;15:609–621. doi: 10.1517/14728222.2011.561201. [DOI] [PubMed] [Google Scholar]
- 86.Kunz-Schughart L.A., Freyer J.P., Hofstaedter F., Ebner R. The use of 3-D cultures for high-throughput screening: The multicellular spheroid model. J. Biomol. Screen. 2004;9:273–285. doi: 10.1177/1087057104265040. [DOI] [PubMed] [Google Scholar]
- 87.Walenta S., Doetsch J., Mueller-Klieser W., Kunz-Schughart L.A. Metabolic imaging in multicellular spheroids of oncogene-transfected fibroblasts. J. Histochem. Cytochem. 2000;48:509–522. doi: 10.1177/002215540004800409. [DOI] [PubMed] [Google Scholar]
- 88.Oloumi A., MacPhail S.H., Johnston P.J., Banath J.P., Olive P.L. Changes in subcellular distribution of topoisomerase IIα correlate with etoposide resistance in multicell spheroids and xenograft tumors. Cancer Res. 2000;60:5747–5753. [PubMed] [Google Scholar]
- 89.Pervez S., Kirkland S.C., Epenetos A.A., Mooi W.J., Evans D.J., Krausz T. Effect of polarity and differentiation on antibody localization in multicellular tumour spheroid and xenograft models and its potential importance for in vivo immunotargeting. Int. J. Cancer. 1989;44:940–947. doi: 10.1002/ijc.2910440532. [DOI] [PubMed] [Google Scholar]
- 90.Roose T., Netti P.A., Munn L.L., Boucher Y., Jain R.K. Solid stress generated by spheroid growth estimated using a linear poroelasticity model. Microvasc. Res. 2003;66:204–212. doi: 10.1016/S0026-2862(03)00057-8. [DOI] [PubMed] [Google Scholar]
- 91.Lichtenbeld H.H., Muller A.D., van Dam-Mieras M.C., Blijham G.H. Tumor spheroid-induced vesicle formation on endothelial cells is associated with procoagulant properties. Pt 2J. Cell. Sci. 1993;106:657–662. doi: 10.1242/jcs.106.2.657. [DOI] [PubMed] [Google Scholar]
- 92.Konur A., Kreutz M., Knuchel R., Krause S.W., Andreesen R. Cytokine repertoire during maturation of monocytes to macrophages within spheroids of malignant and non-malignant urothelial cell lines. Int. J. Cancer. 1998;78:648–653. doi: 10.1002/(SICI)1097-0215(19981123)78:5<648::AID-IJC20>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 93.Gottfried E., Faust S., Fritsche J., Kunz-Schughart L.A., Andreesen R., Miyake K., Kreutz M. Identification of genes expressed in tumor-associated macrophages. Immunobiology. 2003;207:351–359. doi: 10.1078/0171-2985-00246. [DOI] [PubMed] [Google Scholar]
- 94.Ward J.P., King J.R. Mathematical modelling of drug transport in tumour multicell spheroids and monolayer cultures. Math. Biosci. 2003;181:177–207. doi: 10.1016/S0025-5564(02)00148-7. [DOI] [PubMed] [Google Scholar]
- 95.Wenning L.A., Murphy R.M. Coupled cellular trafficking and diffusional limitations in delivery of immunotoxins to multicell tumor spheroids. Biotechnol. Bioeng. 1999;62:562–575. doi: 10.1002/(SICI)1097-0290(19990305)62:5<562::AID-BIT8>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 96.Abu-Absi S.F., Friend J.R., Hansen L.K., Hu W.S. Structural polarity and functional bile canaliculi in rat hepatocyte spheroids. Exp. Cell. Res. 2002;274:56–67. doi: 10.1006/excr.2001.5467. [DOI] [PubMed] [Google Scholar]
- 97.Tong J.Z., Sarrazin S., Cassio D., Gauthier F., Alvarez F. Application of spheroid culture to human hepatocytes and maintenance of their differentiation. Biol. Cell. 1994;81:77–81. doi: 10.1016/0248-4900(94)90058-2. [DOI] [PubMed] [Google Scholar]
- 98.Anderer U., Libera J. In vitro engineering of human autogenous cartilage. J. Bone Miner. Res. 2002;17:1420–1429. doi: 10.1359/jbmr.2002.17.8.1420. [DOI] [PubMed] [Google Scholar]
- 99.Jedeszko C., Sameni M., Olive M.B., Moin K., Sloane B.F. Visualizing protease activity in living cells: From two dimensions to four dimensions. Curr. Protoc. Cell. Biol. 2008 doi: 10.1002/0471143030.cb0420s39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bai C., Yang M., Fan Z., Li S., Gao T., Fang Z. Associations of chemo- and radio-resistant phenotypes with the gap junction, adhesion and extracellular matrix in a three-dimensional culture model of soft sarcoma. J. Exp. Clin. Cancer Res. 2015;34:58. doi: 10.1186/s13046-015-0175-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sachs N., Clevers H. Organoid cultures for the analysis of cancer phenotypes. Curr. Opin. Genet. Dev. 2014;24:68–73. doi: 10.1016/j.gde.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 102.Halfter K., Ditsch N., Kolberg H.C., Fischer H., Hauzenberger T., von Koch F.E., Bauerfeind I., von Minckwitz G., Funke I., Crispin A., et al. Prospective cohort study using the breast cancer spheroid model as a predictor for response to neoadjuvant therapy—The spheroneo study. BMC Cancer. 2015;15:519. doi: 10.1186/s12885-015-1491-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Van Oosterwijk J.G., Herpers B., Meijer D., Briaire-de Bruijn I.H., Cleton-Jansen A.M., Gelderblom H., van de Water B., Bovee J.V. Restoration of chemosensitivity for doxorubicin and cisplatin in chondrosarcoma in vitro: Bcl-2 family members cause chemoresistance. Ann. Oncol. 2012;23:1617–1626. doi: 10.1093/annonc/mdr512. [DOI] [PubMed] [Google Scholar]
- 104.Monderer D., Luseau A., Bellec A., David E., Ponsolle S., Saiagh S., Bercegeay S., Piloquet P., Denis M.G., Lode L., et al. New chondrosarcoma cell lines and mouse models to study the link between chondrogenesis and chemoresistance. Lab. Invest. 2013;93:1100–1114. doi: 10.1038/labinvest.2013.101. [DOI] [PubMed] [Google Scholar]
- 105.Hamdi D.H., Barbieri S., Chevalier F., Groetz J.E., Legendre F., Demoor M., Galera P., Lefaix J.L., Saintigny Y. In vitro engineering of human 3D chondrosarcoma: A preclinical model relevant for investigations of radiation quality impact. BMC Cancer. 2015;15:579. doi: 10.1186/s12885-015-1590-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pauli C., Hopkins B.D., Prandi D., Shaw R., Fedrizzi T., Sboner A., Sailer V., Augello M., Puca L., Rosati R., et al. Personalized in vitro and in vivo cancer models to guide precision medicine. Cancer Discov. 2017;7:462–477. doi: 10.1158/2159-8290.CD-16-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Boehnke K., Iversen P.W., Schumacher D., Lallena M.J., Haro R., Amat J., Haybaeck J., Liebs S., Lange M., Schafer R., et al. Assay establishment and validation of a high-throughput screening platform for three-dimensional patient-derived colon cancer organoid cultures. J. Biomol. Screen. 2016;21:931–941. doi: 10.1177/1087057116650965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Breslin S., O'Driscoll L. Three-dimensional cell culture: The missing link in drug discovery. Drug Discov. Today. 2013;18:240–249. doi: 10.1016/j.drudis.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 109.Ricci C., Moroni L., Danti S. Cancer tissue engineering—New perspectives in understanding the biology of solid tumours—A critical review. OA Tissue Eng. 2013;1:4. doi: 10.13172/2052-9643-1-1-607. [DOI] [Google Scholar]
- 110.Tibbitt M.W., Anseth K.S. Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol. Bioeng. 2009;103:655–663. doi: 10.1002/bit.22361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fischbach C., Chen R., Matsumoto T., Schmelzle T., Brugge J.S., Polverini P.J., Mooney D.J. Engineering tumors with 3D scaffolds. Nat. Methods. 2007;4:855–860. doi: 10.1038/nmeth1085. [DOI] [PubMed] [Google Scholar]