More than 5.7 million patients are admitted annually to an intensive care unit (ICU) in the United States, accounting for approximately 20% of all acute care admissions.1 With the aging population and its increasing comorbidity burden, the number of ICU patients and the projected costs associated with their care is expected to rise.2
Alongside the increased number and complexity of ICU patients has been the development and common use of intensivists to staff ICUs. Intensivists are the hospitalists of the ICU— physicians who dedicate much or all of their clinical practice to the ICU, and who take primary responsibility (or an aggressive “consult” comanagement) for patients while they are in the ICU. Although there is only ambiguous evidence of better outcomes with intensivists,3 the practical necessity of having physicians who are readily available for emergencies, capable of handling ventilators, complicated hemodynamics, and coordinating complex multidisciplinary care and quality improvement in the ICU has resulted in their growing adoption.
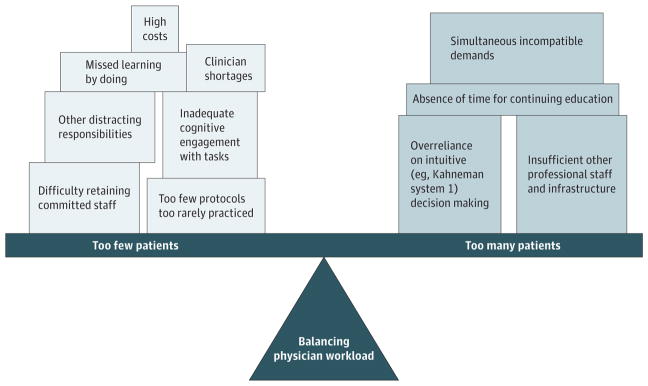
What is not known and has rarely been studied is the ideal ratio of patients to intensivists. If an intensivist has too many patients he or she would not be able to attend to the many complicated issues, potentially resulting in missed details, a slower or less thoughtful response, and less time with the patient and their family. With too few patients, intensivists may not have enough experience for making rapid decisions and perfecting complex procedures, as well as other potential challenges (Figure).
Figure.
Competing Potential Problems That Need to Be Balanced in Setting an Optimal Number of Patients per Physician
In this issue of JAMA Internal Medicine, Gershengorn et al4 provide data to inform decisions on an optimal patient to intensivist ratio (PIR) in ICUs in the United Kingdom (UK) and its association with hospital and ICU mortality. The authors performed a retrospective cohort analysis in ICUs in the UK from 2010–2013 and limited their analysis to ICUs staffed with 1 intensivist during daytime hours. The authors defined PIR for each patient as the number of patients cared for by the intensivist each day averaged over the patients’ stay. In this sample of UK hospitals, the median PIR for patients was 8.5 (inter-quartile range, 6.8–10.8). Provocatively, the association between PIR and hospital mortality was U-shaped, with a reduction in the odds of mortality peaking at 7.5 and no additional association seen above a ratio of 12. Therefore a PIR less than or greater than 7.5 was associated with higher hospital and ICU mortality. The absolute effect sizes of exposure to intensivists who deviated from 7.5 in either direction were nontrivial— perhaps as much as a 4 to 7 percentage point absolute increase in mortality.
These findings shed light on a challenging issue—how many patients can safely be taken care of by a single intensivist based on the ICU census at that specific time. The answer has significant ramifications with regards to policy and staffing of ICUs given the multiple stakeholders involved. The definition of PIR used by Gershengorn et al4 accounts for the often overlooked day-to-day variation in ICU census and the increased workload of new admissions which distracts from the ongoing care of patients already admitted to an ICU. This allows their work to be distinguished from prior work which used number of ICU beds to reflect ICU census5 or the average full-time equivalent (FTE) of the intensivists at the ICU to reflect the number of intensivists caring for the patient.6 Gershengorn and colleagues4 provide an impressive number of alternative approaches to measuring individual physician workload in their sensitivity analyses, and find a consistent general pattern.
The relationship between PIR and mortality is not linear in 2 interesting ways. The first is the presence of a not-enough-work limb, consistent with the above suggested mechanisms. These mechanisms need untangling, because they call for different remedies for different mechanisms. The second interesting aspect is the relative absence of additional mortality once the PIR gets above 12—whereas one might expect pure overload effects to cause excess deaths to continue to rise. While the study intentionally restricted itself to single-intensivist ICUs, it could not account for the presence or expertise of ancillary staff. This flattening of the PIR-mortality curve hints that some overwork might be attenuated by bringing additional nonintensivist resources to bear, consistent with the broader literature emphasizing the fundamentally multidisciplinary nature of critical care. These are, however, just speculation, and certainly limited by the imprecision in the mortality estimates above 12.
However, prior to rearranging one’s ICU staffing to ensure a PIR of 7.5, one should consider the limitations of the work of Gershengorn et al.4 This study was based in ICUs located in the UK with only 1 intensivist present during daytime hours. It is known that ICUs in the UK are different from ICUs in the United States owing to case mix and processes of care, which limits its generalizability.7 The authors have done the important work of demonstrating there is a population-averaged effect of clinically relevant size. But neither intensivists nor ICUs are entirely interchangeable, so this article urgently demands a follow-up to show how the optimal PIR varies by physician characteristics and characteristics of the ICU and hospital-system in which that physician practices.
Identifying the ideal PIR ratio for all ICUs is essential given the perceived short supply of intensivists and the movement (not with standing evidence) to have intensivist physicians present 24 hours a day.8,9 A gauntlet has been thrown down by this important study: how do we incorporate the inherent differences in the multiple ICUs so that the ideal PIR reflects the diversity of the talents of the intensivists who practice and the system supports and institutional frameworks in which they practice? Addressing these issues in this larger context will allow for evidence-based intensivist staffing models to emerge.
Footnotes
Conflict of Interest Disclosures: None reported.
Disclaimer: This article represents the authors’ views and not those of the US Government or the Department of Veterans Affairs.
References
- 1.Barrett ML, Smith MW, Elixhauser A, et al. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, Maryland: 2006. Utilization of Intensive Care Services, 2011: Statistical Brief #185. [Google Scholar]
- 2.Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J, Jr Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS) Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284(21):2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 3.Kahn JM, Rubenfeld GD. Themyth of the workforce crisis. Why the United States does not need more intensivist physicians. Am J Respir Crit Care Med. 2015;191(2):128–134. doi: 10.1164/rccm.201408-1477CP. [DOI] [PubMed] [Google Scholar]
- 4.Gershengorn HB, Harrison DA, Garland A, Wilcox ME, Rowan KM, Wunsch H. Association of intensive care unit patient-to-intensivist ratios with hospital mortality [published online January 22, 2017] JAMA Intern Med. doi: 10.1001/jamainternmed.2016.8457. [DOI] [PubMed] [Google Scholar]
- 5.Iwashyna TJ, Kramer AA, Kahn JM. Intensive care unit occupancy and patient outcomes. Crit Care Med. 2009;37(5):1545–1557. doi: 10.1097/CCM.0b013e31819fe8f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilcox ME, Harrison DA, Short A, Jonas M, Rowan KM. Comparing mortality among adult, general intensive care units in England with varying intensivist cover patterns: a retrospective cohort study. Crit Care. 2014;18(4):491. doi: 10.1186/s13054-014-0491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wunsch H, Angus DC, Harrison DA, Linde-Zwirble WT, Rowan KM. Comparison of medical admissions to intensive care units in the United States and United Kingdom. Am J Respir Crit Care Med. 2011;183(12):1666–1673. doi: 10.1164/rccm.201012-1961OC. [DOI] [PubMed] [Google Scholar]
- 8.Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366(22):2093–2101. doi: 10.1056/NEJMsa1201918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kerlin MP, Small DS, Cooney E, et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209. doi: 10.1056/NEJMoa1302854. [DOI] [PMC free article] [PubMed] [Google Scholar]