Abstract
Purpose of Review
Sexually transmitted infection (STI) incidence is on the rise in the United States. The increase is especially pronounced in adolescents (15–24 years of age). Despite making up only a quarter of the population, adolescents account for approximately half of new STIs in the United States every year. This review summarizes recent developments in the field of STIs, excluding human immunodeficiency virus, in adolescents.
Recent Findings
In this paper, we examine the epidemiology, screening, management, and prevention of STIs in adolescents. STI rates in adolescents have been rising since 2014, with young women and men who have sex with men at particularly high risk. Barriers to STI screening for adolescents include confidentiality concerns and lack of access to health services. Prevention through STI vaccines represents a promising way to combat the epidemic.
Summary
STIs are a growing concern for adolescents. Proper screening and management are of critical importance. Furthermore, prevention efforts such as human papillomavirus (HPV) vaccination should be prioritized. Much of the current literature on STIs does not address the unique nature of STIs in adolescents, and additional research into effective prevention and treatment strategies of STIs in adolescents is urgently needed.
Keywords: STIs, Adolescents, Epidemiology, STI Screening, HPV Vaccine
Introduction
Of approximately 20 million new sexually transmitted infections (STIs) each year in the United States, half of cases occur among adolescents age 15–24 years. It is estimated that 1 out of 4 sexually active adolescent females have an STI, most commonly Chlamydia trachomatis (CT) infection and human papillomavirus (HPV) infection (see Table 1 for abbreivations). STI rates in the United States are on the rise, in both males and females, and much of this increase is occurring in adolescents [1].
Table 1. Sexualy Transmitted Infection Abbreviations.
Description: The table defines STI abbreviations used throughout the review.
| Chlamydia trachomatis | CT |
| Human papillomavirus | HPV |
| Neisseria gonorrhoeae | NG |
| Herpes simplex virus | HSV |
| Trichomonas vaginalis | TV |
Adolescents are uniquely at risk for STIs from both behavioral and biological perspectives. Behaviorally, adolescents are more likely to engage in high-risk sexual behavior such as concurrent partners or sex without a condom [2]. This is due in part to the fact that the prefrontal cortex, responsible for executive function, is still developing throughout adolescence [3]. Furthermore, adolescents are less likely than adults to access and utilize sexual health services [2]. Those factors lead to a higher chance of exposure and a lower chance of diagnosis and treatment. From a biological perspective, adolescent females are particularly susceptible to STIs like CT and HPV due to lower production of cervical mucous and increased cervical ectopy [2, 4]. Therefore, if exposed to an STI, adolescent females are more likely than adults to get infected.
STIs can cause long term health problems if left untreated. Tertiary stage syphilis can lead to nervous system and cardiovascular system damage, and congenital syphilis can cause serious complications or infant death [5]. CT, Neisseria gonorrhoeae (NG), and Trichomonas vaginalis (TV) can cause adverse birth outcomes and infertility [6, 7, 8]. Certain strains of HPV can lead to cervical, oropharyngeal, or rectal cancer [9]. Additionally, STIs have been associated with increased rates of human immunodeficiency virus (HIV) transmission [10].
Despite the high prevalence and high morbidity, there are relatively limited data on STIs in adolescents. Most studies and guidelines focus on infections and treatment in adults. However, in order to adequately address the STI epidemic, it is essential to understand and prevent adolescent infections.
The aim of this review is to describe current trends and recommendations regarding STIs, excluding HIV, in adolescent populations. Specific attention is given to populations at increased risk of acquiring an STI, including women and young men who have sex with men (YMSM). Future directions of STI screening and prevention are also discussed.
Epidemiology of STIs in Adolescents
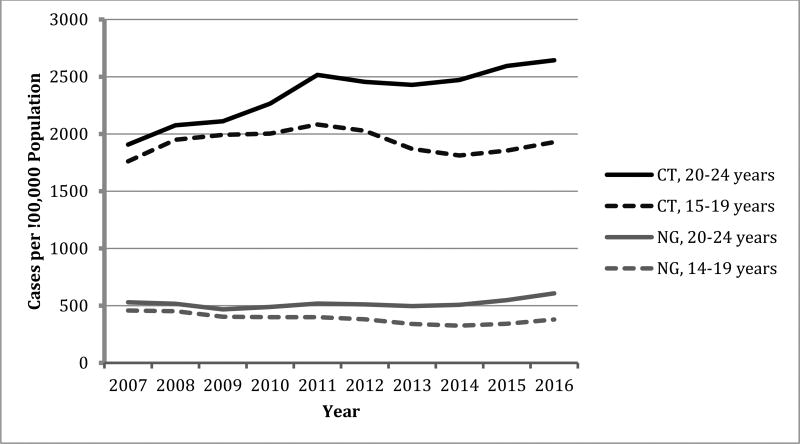
Sexually transmitted infection rates are increasing among adolescents in the United States. However, infection rates vary by sex, geography, and sexual practices. According to the 2016 STD Surveillance report, CT and NG are more common among adolescents than any other age group. The rate of CT infection among females aged 15–19 years increased by 4.1% from 2014–2016, while the rate among males aged 15–19 years increased by 15.3% from 2014–2016. CT infection rates among adolescents aged 20–24 years followed similar patterns. Rates of NG infection, though lower than CT infection, are increasing as well. From 2015–2016 alone, the rate of NG infection increased by 11.3% among adolescents aged 15–19 years and 10.9% among adolescents aged 20–24 years. Primary and secondary syphilis infections have seen the most dramatic increase, with total national rates at their highest since 1993. From 2014–2016, syphilis rates increased by 24.5% among adolescents aged 15–19 years and 25.4% among adolescents aged 20–24 years. Specific prevalence data and trends can be seen in Table 2 and Figure 1 [2].
Table 2. Prevalence of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), and Syphilis Infections among Adolescents in 2016.
Description: The figure describes the 2016 prevalence of CT, NG, and syphilis infections among adolescents, broken down by age group and sex.
| CT Infection (cases / 100,000 population) |
NG Infection (cases / 100,000 population) |
Primary and Secondary Syphilis Infection (cases / 100,000 population) |
||||
|---|---|---|---|---|---|---|
| 15–19 years | 20–24 years | 15–19 years | 20–24 years | 15–19 years | 20–24 years | |
| Females | 3,070.9 | 3,779.0 | 482.1 | 595.5 | 3.3 | 6.7 |
| Males* | 832.6 | 1,558.6 | 280.8 | 616.8 | 8.9 | 37.9 |
Data includes both MSM and heterosexual adolescent males
Data from: CDC Sexually Transmitted Disease Surveillance, 20162
Figure 1. Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) Infection Rates Among Adolescents from 2007–2016.
Description: The figure shows the rate of CT and NG infections in adolescents from 2007–2016
Data from: CDC Sexually Transmitted Disease Surveillance, 20162
There are less data on the total prevalence of HPV in adolescents. In a study of HPV prevalence from 2009–2012, it was estimated that 29.0% of females aged 14–19 years and 58.7% of females aged 20–24 years were infected with HPV [11]. While there are over 150 strains of HPV, the majority present no symptoms and resolve spontaneously. However, HPV types 6 and 11 account for 90% of genital warts, and HPV types 16 and 18 account for 70% of cervical cancer cases [12, 13]. Prevalence of those four strains specifically was 4.3% among females aged 14–19 years and 12.1% among females aged 20–24 years. Notably, the study found that in 2012, only 6 years after the HPV vaccine introduction in 2006, there was a 64% reduction in HPV 6, 11, 16, and 18 prevalence among females aged 14–19 years, and a 34% reduction among females aged 20–24 years [11]. The data suggest high vaccine effectiveness and the importance of continued efforts to increase vaccination coverage. With 2016 HPV vaccination rates in the United States around only 49.5% for females aged 13–17 years and 37.5% for males aged 13–17 years, there is significant opportunity to prevent HPV-related genital warts and cancers [14].
Additional STIs, such as genital herpes simplex virus (HSV) and TV are also common among adolescents [15, 16]. Neither are reported nationally, making it difficult to assess epidemiologic trends [2]. Several studies have shown that, although HSV-2 typically causes genital herpes and HSV-1 typically causes orolabial herpes, the prevalence of genital HSV-1 in adolescents has increased significantly [17, 18]. Previously, only about 20% of genital herpes cases were thought to be caused by HSV-1. However, a 2012 HSV vaccine trial indicated that approximately 60% of genital herpes cases in the United States are now caused by HSV-1, with a higher percentage among younger populations [19]. The increase may be the result of the decreasing prevalence orolabial HSV-1 in adolescents and thus a lack of HSV-1 antibodies upon sexual debut [20]. It may also be due to increasingly common oral sex practices among adolescents [21].
CT and NG rates are consistently highest in the southern United States, while syphilis rates are highest in the western United States. A map of CT prevalence among adolescent females can be seen in Figure 2. CT, NG, and syphilis prevalence is also higher among black, Hispanic, American Indian, and Pacific Islander populations [2]. Geographic and racial differences in STI prevalence reflect higher levels of poverty and decreased access to and utilization of sexual health services [22].
Figure 2. Chlamydia trachomatis Infection — Rates of Reported Cases Among Women Aged 15–24 Years by State, United States and Outlying Areas, 2016.
Description: The figure shows 2016 CT infection rates in adolescent females, broken down by state.
Image from: CDC Sexually Transmitted Disease Surveillance, 20162
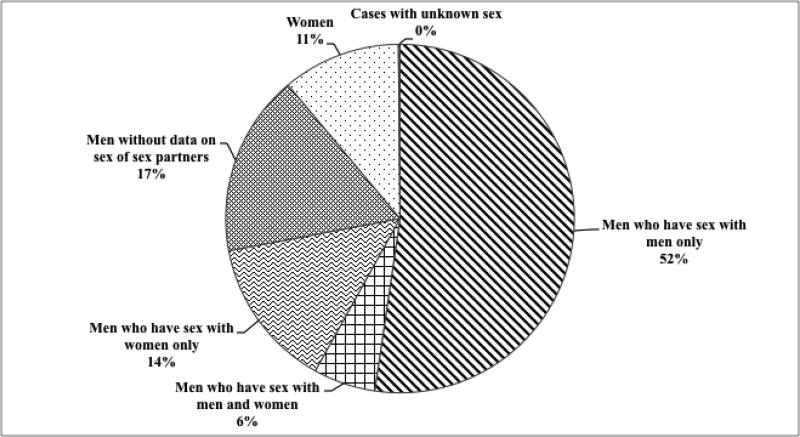
YMSM are at an increased risk for STIs due to both individual-level risk behaviors, such as number of partners and frequency of sex without a condom, as well as population-level factors, such as overlapping sexual networks [2]. With a syphilis rate of 309 cases / 100,000 population, men who have sex with men (MSM) represent over 58% of primary and secondary syphilis cases in the United States (Figure 3) [23]. As syphilis rates are highest among young men aged 20–24, YMSM are at particularly high risk of syphilis infection [2]. YMSM are also at increased risk for CT and NG infections, specifically antibiotic resistant NG. The burden of STIs are higher among HIV-infected YMSM than among HIV-uninfected YMSM [24].
Figure 3. Primary and Secondary Syphilis — Distribution of Cases by Sex and Sexual Behavior, United States, 2016.
Description: The figure highlights the distribution of primary and secondary syphilis infections by sex and sexual behavior.
Data from: CDC Sexually Transmitted Disease Surveillance, 20162
Homeless, incarcerated, and drug-using youth represent additional high-risk populations. A recent review found STIs among homeless adolescents to be associated with length of homelessness, coercive sex, and unmet survival needs [25]. Adolescent drug use and incarceration are also associated with higher rates of STIs due to combination of behavioral risk factors and unequal access to the health care system [26, 27]., More broadly, adverse experiences in childhood, such as sexual abuse or parental incarceration, are associated with increased risk of STIs in adolescence [28].
STI Screening in Adolescents
The Centers for Disease Control and Prevention (CDC) recommends annual CT and NG screening for sexually active adolescent women. Syphilis screening is recommended for YMSM and pregnant women. Cervical cancer screening via a Pap test is recommended in women starting at age 21 years [1].
Urogenital and rectal CT and NG testing, as well as pharyngeal NG testing, are recommended in YMSM [1]. In a study of men screened at a college health clinic, it was found that 26.4% of CT infections and 63.2% of NG infections would have been missed if only urogenital screening had been conducted [29]. Another study found that patient-reported exposure was not necessarily a reliable indicator for anogenital CT and NG screening in young black MSM. While reported anal sexual exposure predicted rectal infection, 19.4% of rectal infections would have been missed in men who denied receptive anal sex [30].
Despite recommendations for widespread screening, a relatively small percentage of adolescents receive the recommended STI screening. A national survey of youth age 15–25 years found that most had never received an STI test: only 16.6% of females and 6.6% of males had been tested in the past 12 months [31]. Confidentiality concerns were a large barrier to testing. Although all 50 states allow adolescents to access STI screening and treatment without parental consent, 18 states allow for parental notification if a minor is seeking STI services [32]. Furthermore, for adolescents who are on their parents’ insurance plans, concerns about confidentiality breaches through insurance billing are common. According to the 2015 National Survey of Family Growth, 12.7% of sexually experienced adolescents covered by their parent’s insurance plan reported they would forgo sexual health services due to concern that their parents would find out. This number was higher, 22.6%, among adolescents age 15–17 years [33]. Others reported foregoing screening because they felt they were not at risk for STIs [31].
Confidentiality concerns are important to address when working with adolescents. Adolescent females who had time alone with a provider were more than twice as likely to receive STI screening than those whose parents were in the room, suggesting the value of private discussions between adolescents and their providers [33]. Other options, such as self-collected swabs or home-based specimen collection and testing, may also reduce confidentiality concerns among adolescents and should be further evaluated [34].
STI Management
STIs in adolescents should be managed according to CDC recommendations.1 There are no unique recommendations for STI treatment in youth specifically, other than adherence counseling. Research into the effectiveness of STI treatment in adolescent populations is needed.
The CDC recommends treating both urogenital and extragenital CT infections with 1 gm oral azithromycin. However, over the past few years, there has been critical appraisal of the effectiveness of treating rectal CT with azithromycin versus doxycycline. Numerous studies have shown doxycycline to be more effective than azithromycin [35, 36, 37]. A retrospective cohort study of rectal CT infection found that azithromycin treatment was associated with a 5-fold higher risk of persistent/recurrent infection 14–90 days after treatment when compared to treatment with doxycycline [38]. Azithromycin failure is more likely in patients with a higher organism load [39]. While European guidelines recommend treating oral and rectal CT infections with doxycycline, the CDC has not yet updated recommendations [1, 40]. Large, randomized controlled trials are urgently needed.
An emerging challenge in the management of STIs is the shortage of penicillin benzathine G, both in the United States and globally. Penicillin benzathine G is the recommended treatment for syphilis, and the only recommended syphilis treatment option for pregnant women [1]. While syphilis rates are at their highest in 20 years, penicillin benzathine G has become unavailable in many hospitals [41]. In Japan, amoxicillin has been successfully used as an alternative to penicillin benzathine G to treat syphilis infection and prevent mother-to-child transmission [42, 43].
The rise of antibiotic resistant NG and even untreatable NG is another important issue in the management of STIs. In 2016, the Gonococcal Isolate Surveillance Project reported that 44.1% of NG isolates were resistant to penicillan, tetracycline, and / or ciprofloxacin [2, 44]. Furthermore, the past decade has shown an increase in isolates with an elevated minimal inhibitory concentration to the cephalosporins cefixime and ceftriaxone [45]. There have also been reports of treatment failures to cefixime and ceftriaxone [46, 47]. Due to the emergence of resistance, two-drug therapy is now recommended, utilizing both 1 gm azithromycin and 250 mg injectable ceftriaxone. There are no data on the rates of resistance in adolescent populations specifically, but the two-drug treatment recommendations apply regardless of age or anatomical site of infection [1].
Partner notification and treatment is another essential aspect of STI management. In adolescent populations, this can be particularly challenging due to the higher frequency of concurrent partners and relationships of shorter duration. However, high rates of STI reinfection among youth indicate the critical importance of partner management [48]. Expedited partner therapy, where the patient delivers medication or a prescription to the partner, has been shown to be a successful option to treat CT or NG infection in heterosexual adult couples. Data are limited regarding the effectiveness of expedited partner therapy in adolescents or MSM. Expedited partner therapy is recommended for MSM in most states, although not universally [2, 49].
Prevention of STIs
The World Health Organization has made STI prevention one of its priorities for 2016–2021 [50]. Prevention efforts are particularly important in adolescents, as sexual health habits are often still developing. Adolescent STI prevention efforts should come from a combination of sources. Traditional sources of information, such as parents and schools, play an important role. Sexual communication between adolescents and their parents has been shown to lead to safer sex behavior [51]. HPV vaccination is also a critical component of adolescent sexual health. It is recommended that both boys and girls age 11–12 years receive the vaccine series. The vaccine is recommended through age 26 for females, MSM, and HIV-infected patients, and through age 21 for heterosexual males [1]. The vaccine is safe and highly effective in preventing most HPV infections [52, 53].
There is also potential for powerful prevention efforts via social media. Social media campaigns are an effective way to communicate prevention messages to specific, targeted audiences [54]. Numerous campaigns promoting STI testing and safe sex practices have been shown to increase STI testing and safer-sex behaviors [55, 56, 57]. As mobile dating apps become more popular, especially among adolescents, they represent a unique venue through which to reach adolescents at high-risk for STIs. A recent study found that it was feasible to use Grindr, a dating app for MSM, to distribute HIV self-testing kits [58]. It would be valuable to evaluate a similar model for home-based STI testing.
Future Directions
Pre-exposure vaccines are the most powerful method for infection prevention. With vaccination rates around 51% for adolescent females aged 14–19 years, the HPV vaccine has led to a substatial reduction in HPV types 6, 11, 16, and 18 [2]. However, broader coverage through HPV vaccination requirements represents the potential for a further significant decrease in HPV-related cancer and associated costs. Rhode Island, Virginia, and Washington DC require HPV vaccination for school entry [59].
Effective vaccines for other STIs would significantly improve sexual health. Vaccine development efforts vary by specific STI. HSV and CT vaccine candidates are in clinical trials, while NG and syphilis vaccine candidates are still in preclinical development [60, 61]. Notably, a recent study showed a serogroup B meningococcal vaccine to be 31% effective against NG, the first instance of a protective vaccine against NG [62, 63]. Meanwhile, a TV vaccine development program will require a better fundamental understanding of the TV parasite and the epidemiology of the infection [60]. STI vaccines represent a worthy research investment due to the high burden of STIs and the increasing challenges posed by antibiotic resistance. A 2016 study indicated high acceptance of a CT vaccine among adolescents [64].
Rapid point-of-care diagnostic testing represents another exciting development in the field of STIs. Numerous rapid diagnostic tests for common STIs such as CT and NG are in development or newly on the market [65]. Rapid point-of-care testing creates a large potential for improved management, as patients could be screened and treated in the same day, reducing loss to follow up [66]. Furthermore, rapid STI testing efforts could be integrated into the current infrastructure for rapid HIV testing, increasing access to testing and treatment of STIs. The advent of rapid diagnostic tests has important implications globally as well. In the majority of low and middle income countries, STIs such as CT and NG are managed through symptom-based management due to the high cost of testing [50]. However, symptom-based management leads to a large number of untreated infections due to the often asymptomatic nature of STIs. Furthermore, it likely leads to unnecessary antibiotic treatment. As new rapid diagnostic tests become available, evaluations will be needed to demonstrate the cost-effectiveness of point-of-care STI testing in the global setting.
Conclusion
STIs are a common cause of disease in adolescents. As STI rates in the United States rise, it is critical to understand and address the epidemic from both medical and public health perspectives. Prevention efforts, ranging from HPV vaccination to social media awareness campaigns, are important to confront the epidemic from a population perspective. Meanwhile, provider-based screening and timely patient and partner treatment are essential to improve adolescent clinical care. Moving forward, research is needed to determine optimal strategies to increase adoption of routine screening among adolescents, particularly among high-risk populations such as young women and YMSM.
Key Points.
STIs in adolescents are on the rise in the United States, with particularly high rates among young women and men who have sex with men
Barriers to health services and concerns about confidentiality often prevent adolescents from receiving recommended STI screening
Vaccines, such as the HPV vaccine, represent a powerful and promising way to prevent STIs and associated morbidities
Research is urgently needed to determine strategies to increase uptake of STI screening among adolescents
Acknowledgments
None
Financial Support and Sponsorship: Center for AIDS Research (NIH grant AI028697). Adolescent Medicine Trials Network for HIV/AIDS Interventions (NIH grant U19HD089886).
Footnotes
Conflicts of Interest: None
References and Recommended Reading
- 1.Workowski KA, Bolan GA. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep. 2015;64(3) [PMC free article] [PubMed] [Google Scholar]
- 2.Sexually Transmitted Disease Surveillance, 2016. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2017 Sep; [Google Scholar]
- 3.Steinberg L. Cognitive and affective development in adolescence. Trends in cognitive sciences. 2005;9(2):69–74. doi: 10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Burchell AN, et al. Epidemiology and transmission dynamics of genital HPV infection. Vaccine. 2006;24:S52–S61. doi: 10.1016/j.vaccine.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 5.Syphilis - CDC Fact Sheet. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2017 Jun; [Google Scholar]
- 6.Chlamydia - CDC Fact Sheet. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2017 Mar; [Google Scholar]
- 7.Gonorrhea - CDC Fact Sheet. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2016 May; [Google Scholar]
- 8.Trichomoniasis - CDC Fact Sheet. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2017 Jul; [Google Scholar]
- 9.What is HPV? Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2016 Dec; [Google Scholar]
- 10.Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nature reviews. Microbiology. 2004;2(1):33. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
- 11••.Markowitz LE, et al. Prevalence of HPV after introduction of the vaccination program in the United States. Pediatrics. 2016 doi: 10.1542/peds.2015-1968. This study describes a significant reduction in prevalence of HPV 6, 11, 16, and 18 among adolescents 6 years after HPV vaccine introduction. It is the first study to show population impact of the HPV vaccination among women in their twenties. [DOI] [PubMed] [Google Scholar]
- 12.Bosch FX, et al. Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine. 2008;26:K1–K16. doi: 10.1016/j.vaccine.2008.05.064. [DOI] [PubMed] [Google Scholar]
- 13.Garland SM, et al. Natural History of Genital Warts: Analysis of the Placebo Arm of 2 Randomized Phase III Trials of a Quadrivalent Human Papillomavirus (Types 6, 11, 16, and 18) Vaccine. J Infect Dis. 2009;199(6):805–814. doi: 10.1086/597071. [DOI] [PubMed] [Google Scholar]
- 14.National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2016. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2017 Aug; [Google Scholar]
- 15.Van Der Pol B, et al. Prevalence, incidence, natural history, and response to treatment of Trichomonas vaginalis infection among adolescent women. The Journal of infectious diseases. 2005;192(12):2039–2044. doi: 10.1086/498217. [DOI] [PubMed] [Google Scholar]
- 16.Xu F, et al. Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. Jama. 2006;296(8):964–973. doi: 10.1001/jama.296.8.964. [DOI] [PubMed] [Google Scholar]
- 17.Roberts CM, Pfister JR, Spear SJ. Increasing proportion of herpes simplex virus type 1 as a cause of genital herpes infection in college students. Sexually transmitted diseases. 2003;30(10):797–800. doi: 10.1097/01.OLQ.0000092387.58746.C7. [DOI] [PubMed] [Google Scholar]
- 18.Ribes JA, et al. Six-year study of the incidence of herpes in genital and nongenital cultures in a central Kentucky medical center patient population. Journal of clinical microbiology. 2001;39(3):3321–3325. doi: 10.1128/JCM.39.9.3321-3325.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belshe RB, et al. Efficacy results of a trial of a herpes simplex vaccine. New England Journal of Medicine. 2012;366(1):34–43. doi: 10.1056/NEJMoa1103151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bradley H, et al. Seroprevalence of herpes simplex virus types 1 and 2—United States, 1999–2010. The Journal of infectious diseases. 2013;209(3):325–333. doi: 10.1093/infdis/jit458. [DOI] [PubMed] [Google Scholar]
- 21.Copen CE, Chandra A, Martinez G. Prevalence and timing of oral sex with opposite-sex partners among females and males aged 15–24 years: United States, 2007–2010. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. 2012 [PubMed] [Google Scholar]
- 22.Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sexually transmitted diseases. 2008;35(12):S13–S18. doi: 10.1097/OLQ.0b013e31818d3cad. [DOI] [PubMed] [Google Scholar]
- 23.de Voux A. State-Specific Rates of Primary and Secondary Syphilis Among Men Who Have Sex with Men—United States, 2015. MMWR. Morbidity and Mortality Weekly Report. 2017;66 doi: 10.15585/mmwr.mm6613a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayer KH. Sexually transmitted diseases in men who have sex with men. Clinical Infectious Diseases. 2011;53(3):S79–S83. doi: 10.1093/cid/cir696. [DOI] [PubMed] [Google Scholar]
- 25.Caccamo A, Kachur R, Williams SP. Narrative Review: Sexually Transmitted Diseases and Homeless Youth—What Do We Know About Sexually Transmitted Disease Prevalence and Risk? Sexually Transmitted Diseases. 2017;44(8):466–476. doi: 10.1097/OLQ.0000000000000633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas JC, Torrone E. Incarceration as forced migration: effects on selected community health outcomes. American journal of public health. 2008;98(Supplement_1):S181–S184. doi: 10.2105/ajph.98.supplement_1.s181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tapert SF, et al. Adolescent substance use and sexual risk-taking behavior. Journal of Adolescent Health. 2001;28(3):181–189. doi: 10.1016/s1054-139x(00)00169-5. [DOI] [PubMed] [Google Scholar]
- 28•.London S, et al. Adverse experiences in childhood and sexually transmitted infection risk from adolescence into adulthood. Sexually transmitted diseases. 2017;44(9):524–532. doi: 10.1097/OLQ.0000000000000640. This study shows that factors such as parental binge drinking, parental incarceration, and sexual abuse are independent correlates of adolescent sexual risk behavior and STIs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29•.Drinkard LN, et al. The Case for Extragenital Screening of Chlamydia trachomatis and Neisseria gonorrhoeae in the College Health Setting. Sexually Transmitted Diseases. 2017;44(5):274–277. doi: 10.1097/OLQ.0000000000000593. This study highlights the importance of extragenital screening among college-age men who have sex with men. [DOI] [PubMed] [Google Scholar]
- 30•.Chamberlain N, et al. Is Patient-Reported Exposure a Reliable Indicator for Anogenital Gonorrhea and Chlamydia Screening in Young Black Men Who Have Sex With Men? Sexually Transmitted Diseases. 2017;44(7):390–392. doi: 10.1097/OLQ.0000000000000619. This study suggests that STI testing based on patient reported exposure may lead to missed infections among black YMSM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31•.Cuffe KM, et al. Sexually transmitted infection testing among adolescents and young adults in the United States. Journal of Adolescent Health. 2016;58(5):512–519. doi: 10.1016/j.jadohealth.2016.01.002. This study describes the low uptake of STI testing among adolescents and examines barriers such as cost and confidentiality concerns. [DOI] [PubMed] [Google Scholar]
- 32.Guttmacher Institute. Guttmacher Institute; Sep 5, 2017. Minors' Access to STI Services. www.guttmacher.org/state-policy/explore/minors-access-sti-services. [Google Scholar]
- 33••.Leichliter JS. Confidentiality Issues and Use of Sexually Transmitted Disease Services Among Sexually Experienced Persons Aged 15–25 Years—United States, 2013–2015. MMWR. Morbidity and Mortality Weekly Report. 2017;66 doi: 10.15585/mmwr.mm6609a1. This article uses data from 2013–2015 National Survey of Family Growth to discuss the significant impact of confidentiality concerns on adolescent STI testing uptake. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wiesenfeld HC, et al. Self-collection of vaginal swabs for the detection of Chlamydia, gonorrhea, and trichomoniasis: opportunity to encourage sexually transmitted disease testing among adolescents. Sexually transmitted diseases. 2001;28(6):321–325. doi: 10.1097/00007435-200106000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Steedman NM, McMillan A. Treatment of asymptomatic rectal Chlamydia trachomatis: Is single-dose azithromycin effective? Int J STD AIDS. 2009;20:16–18. doi: 10.1258/ijsa.2008.008211. [DOI] [PubMed] [Google Scholar]
- 36.Elgalib A, et al. Seven days of doxycycline is an effective treatment for asymptomatic rectal Chlamydia trachomatis infection. Int J STD AIDS. 2011;22:474–477. doi: 10.1258/ijsa.2011.011134. [DOI] [PubMed] [Google Scholar]
- 37.Hathorn E, Opie C, Goold P. What is the appropriate treatment for the management of rectal Chlamydia trachomatis in men and women? Sex Transm Infect. 2012;88(5):352–354. doi: 10.1136/sextrans-2011-050466. [DOI] [PubMed] [Google Scholar]
- 38.Khosropour CM, et al. Comparing azithromycin and doxycycline for the treatment of rectal chlamydial infection: A retrospective cohort study. Sex Transm Dis. 2014;41:79–85. doi: 10.1097/OLQ.0000000000000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kong FYS, et al. Higher organism load associated with failure of azithromycin to treat rectal chlamydia. Epidemiology & Infection. 2016;144(12):2587–2596. doi: 10.1017/S0950268816000996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lanjouw E, et al. 2015 European guideline on the management of Chlamydia trachomatis infections. Int. J. STD AIDS. 2015;27:333–348. doi: 10.1177/0956462415618837. [DOI] [PubMed] [Google Scholar]
- 41.FDA Drug Shortages. U.S. Food and Drug Administration; Accessdata.fda.gov. [Google Scholar]
- 42•.Katanami Y, et al. Amoxicillin and Ceftriaxone as Treatment Alternatives to Penicillin for Maternal Syphilis. Emerging infectious diseases. 2017;23(5):827. doi: 10.3201/eid2305.161936. This article describes alternatives to benzathine penicillin G to treat maternal syphilis infection in the context of the penicillin G shortage. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tanizaki R, et al. High-dose oral amoxicillin plus probenecid is highly effective for syphilis in patients with HIV infection. Clinical Infectious Diseases. 2015;61(2):177–183. doi: 10.1093/cid/civ270. [DOI] [PubMed] [Google Scholar]
- 44.Sexually Transmitted Disease Surveillance 2015: Gonococcal Isolate Surveillance Project (GISP) Supplement & Profiles. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2016 Jul; [Google Scholar]
- 45.Grad YH, et al. Genomic epidemiology of gonococcal resistance to extended-spectrum cephalosporins, macrolides, and fluoroquinolones in the United States, 2000–2013. The Journal of infectious diseases. 2016:jiw420. doi: 10.1093/infdis/jiw420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ison CA, et al. Gonorrhoea treatment failures to cefixime and azithromycin in England 2010. Eurosurveillance. 2011;16(14):7. [PubMed] [Google Scholar]
- 47.Ohnishi M, et al. Is Neisseria gonorrhoeae initiating a future era of untreatable gonorrhea?: detailed characterization of the first strain with high-level resistance to ceftriaxone. Antimicrobial agents and chemotherapy. 2011;55(7):3538–3545. doi: 10.1128/AAC.00325-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Batteiger BE, et al. Repeated Chlamydia trachomatis genital infections in adolescent women. The Journal of infectious diseases. 2010;201(1):42–51. doi: 10.1086/648734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Expedited Partner Therapy in the Management of Sexually Transmitted Diseases. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2006 [Google Scholar]
- 50.Global health sector strategy on sexually transmitted infections, 2016–2021. World Health Organization. 2016 Jul; [Google Scholar]
- 51•.Widman L, et al. Parent-adolescent sexual communication and adolescent safer sex behavior: a meta-analysis. JAMA pediatrics. 2016;170(1):52–61. doi: 10.1001/jamapediatrics.2015.2731. This review shows the impact of parent-adolescent communication, particularly mother-daughter communication, in encouraging safer sex practices. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Human Papillomavirus (HPV) Vaccine Safety. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2017 Jun; [Google Scholar]
- 53.Markowitz LE, et al. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. The Journal of infectious diseases. 2013;208(3):385–393. doi: 10.1093/infdis/jit192. [DOI] [PubMed] [Google Scholar]
- 54.Friedman AL, et al. Health communication and social marketing campaigns for sexually transmitted disease prevention and control: What is the evidence of their effectiveness? Sexually transmitted diseases. 2016;43(2S):S83–S101. doi: 10.1097/OLQ.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 55.Sznitman S, et al. Using culturally sensitive media messages to reduce HIV-associated sexual behavior in high-risk African American adolescents: results from a randomized trial. Journal of Adolescent Health. 2011;49(3):244–251. doi: 10.1016/j.jadohealth.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zimmerman RS, et al. Effects of a televised two-city safer sex mass media campaign targeting high-sensation-seeking and impulsive-decision-making young adults. Health Education & Behavior. 2007;34(5):810–826. doi: 10.1177/1090198107299700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ahrens K, et al. Healthy Penis: San Francisco's social marketing campaign to increase syphilis testing among gay and bisexual men. PLoS medicine. 2006;3(12):e474. doi: 10.1371/journal.pmed.0030474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rosengren AL, et al. Feasibility of using Grindr™ to distribute HIV self-test kits to men who have sex with men in Los Angeles, California. Sexual health. 2016;13(4):389–392. doi: 10.1071/SH15236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.North AL, Niccolai LM. Human papillomavirus vaccination requirements in US schools: recommendations for moving forward. American journal of public health. 2016;106(10):1765–1770. doi: 10.2105/AJPH.2016.303286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60•.Gottlieb SL, et al. The global roadmap for advancing development of vaccines against sexually transmitted infections: update and next steps. Vaccine. 2016;34(26):2939–2947. doi: 10.1016/j.vaccine.2016.03.111. This article provides an informative summary of STI vaccine development efforts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lithgow KV, Cameron CE. Vaccine development for syphilis. Expert review of vaccines. 2017;16(1):37–44. doi: 10.1080/14760584.2016.1203262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62••.Petousis-Harris H, et al. Effectiveness of a group B outer membrane vesicle meningococcal vaccine against gonorrhoea in New Zealand: a retrospective case-control study. The Lancet. 2017 doi: 10.1016/S0140-6736(17)31449-6. This study shows that a serogroup B meningococcal vaccine has an estimated 31% effectiveness against NG infection, the first vaccine to show any protection against NG infection. [DOI] [PubMed] [Google Scholar]
- 63.Seib KL. Gonorrhoea vaccines: a step in the right direction. The Lancet. 2017 doi: 10.1016/S0140-6736(17)31605-7. [DOI] [PubMed] [Google Scholar]
- 64.Trent M, et al. Adolescent Perspectives on Acceptance of a Chlamydia Vaccine and Willingness to participate in vaccine-related research. Sexually Transmitted Diseases. 2016;43 [Google Scholar]
- 65.Herbst de Cortina S, et al. A systematic review of point of care testing for Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. Infectious diseases in obstetrics and gynecology. 2016 doi: 10.1155/2016/4386127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bourgeois-Nicolaos N, et al. Benefits of rapid molecular diagnosis of Chlamydia trachomatis and Neisseria gonorrhoeae infections in women attending family planning clinics. Sexually transmitted diseases. 2015;42(11):652–653. doi: 10.1097/OLQ.0000000000000351. [DOI] [PubMed] [Google Scholar]