Abstract
Increasing numbers of older patients require Emergency admission under General Surgery (EGS). This is a group of heterogeneous and often complex individuals with varying degrees of multimorbidity, polypharmacy, functional, mobility and cognitive impairment. Our article describes the benefits of comprehensive assessment coupled with patient-centred multiprofessional interventions and timely discharge planning. We discuss diverse service models and describe our experience in the planning, development and consolidation of a perioperative service for older EGS patients.
Keywords: Emergency general surgery (EGS), Multidisciplinary, Perioperative Care of Older Persons (POPS), Older, Comprehensive Geriatric Assessment (CGA), Frailty
Introduction
The population is ageing. In 2016, 19.2% and 5.4% of the population were aged over 65 and 80 years, respectively [1]. The unstoppable demographic shift, coupled with drastic decreases in elective surgical interventions after the age of 75 years [2], has resulted in higher numbers of older people being admitted as surgical emergencies [3].
Emergency general surgery (EGS) comprises illnesses of very diverse pathology related only by their urgent nature. The most prevalent conditions are hepatopancreaticobiliary and colorectal disorders which together amount to 43% of all EGS diagnoses. The annual case rate (1290 of 100,000) is higher than the sum of all new cancer diagnoses [4].
Although EGS represents 11% of surgical hospitalisations, these are responsible for 50% of all in-hospital morbidity and mortality [5, 6] and account for 50% of a general surgeon’s workload [7]. Patients aged 70 years and older account for 35% of EGS admissions [8] and individuals over the age of 80 years have a 67% increase in the risk-adjusted odds of mortality compared to their younger counterparts [9].
A third of EGS patients undergo a surgical intervention. Older people represent almost half of patients undergoing emergency laparotomy every year in the United Kingdom [10] and 28.8% of those undergoing major emergency general surgery in the United States. An American study of 421,476 patients requiring EGS between 2008 and 2011 [11] showed that seven procedures including partial colectomy, small-bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendectomy, and laparotomy collectively accounted for 80% of procedures, 80.3% of deaths, 78.9% of complications, and 80.2% of inpatient costs nationwide. The most common complications after surgery are bleeding (6.2%), incisional surgical site infection (SSI) (3.4%), pneumonia (2.7%), and organ/space SSI (2.6%). Bleeding has the greatest overall impact on mortality (95% CI 8.2, 13.1%, p < 0.001) and end-organ dysfunction (95% CI 13.9%, 16.7%, p < 0.001) [12]. The development of complications in the postoperative period increases in-hospital mortality significantly (OR 2.51, 95% CI 1.210–5.187, p = 0.013) [13].
Multimorbidity, polypharmacy and frailty
Although over three-quarters of older EGS patients have multimorbidity (coexistence of two or more chronic medical conditions in one individual) and more than half are affected by polypharmacy, neither of these factors influence the uptake of surgery nor worsen hard clinical outcomes such as mortality, length of stay or readmission to hospital [14, 15].
The OPSOC collaboration in the UK found that frailty was present in 28% of 325 EGS patients and established a significant association with increased length of stay and mortality [16]. Similar figures have been described in North America with frailty present in 37% of 220 EGS patients, who were also demonstrated to have an increased risk of complications [17].
Although it is thought that frailty may be modifiable [18], the evidence advocating routine measurement of frailty in older patients remains limited.
Delivery of care
There are certain interventions proven to be of benefit in managing EGS patients [19, 20]. Amongst these, early review by a consultant surgeon together with urgent imaging of the abdomen reported by a consultant radiologist enabling accurate diagnosis, risk stratification and decision-making. Optimisation of medical problems and pre-operative involvement of a consultant anaesthetist when a surgical intervention is likely to benefit the patient has been shown to improve clinical outcomes. Those patients undergoing major operations and those whose operative mortality risk exceeds 5% should be transferred from theatre into a high dependency area post-surgery.
As shown in Fig. 1, there are a number of models of care aimed at surgical patients requiring medical review [21]. Single organ specialty physicians often provide input to patients admitted to general surgery on an ad hoc basis. This is a reactive service triggered once complications have already developed, and particularly in older surgical patients, it may result in several referrals and even conflicting recommendations.
Fig. 1.
Models of care in emergency general surgery
General physicians, particularly in the United States, advocate a model characterised by joint care of all surgical patients between a physician, anaesthetist and surgeon where the former coordinates the inpatient pathway, whilst the latter provide timely perioperative care [22]. This model appears to work with younger patients; but teams may lack specific skills, training and expertise in the management of complex older people.
In recent years, there has been an upsurge of clinicians with additional subspecialty training in pre-operative assessment, optimisation, and delivery of postoperative care [23]. Whilst adopting this model may be achievable in large NHS Trusts, it may not be feasible in smaller hospitals where team building and consultant retention is challenging. Its expansion will also depend on the establishment of nationwide specialist training programmes.
Older people are a heterogeneous population with a high prevalence of multimorbidity and polypharmacy superimposed on age-related anatomical and physiological changes. This population are at risk of complications such as delirium, functional decline, incontinence, undernutrition and pressure sores [24, 25]. In response, professional bodies and medical societies recognise the importance of Medicine for Care of Older People (MCOP) teams and advocate geriatrician involvement in the care of EGS patients [26]. Comprehensive Geriatric Assessment has become an established multimodal approach to valuation of physical, psychological, functional and social issues in older people [27]. CGA, when coupled with patient-centred multidisciplinary targeted interventions, has been shown to improve outcomes such as length of stay, rates of institutionalisation and readmission, and functional status in oncology [28], vascular [29], orthopaedic [30] and elective general surgery [23]. Unfortunately, only a small proportion of existing geriatric medicine departments (38 of 130 respondents in a 2014 UK study [31]) provide proactive input into EGS patients and only 17% of emergency laparotomy patients over 70 years of age were reviewed by MCOP teams in 2015–16 [10].
Salford-perioperative care of older people-general surgery (Salford-POPS-GS)
Salford Royal NHS Foundation Trust tailored previous guidance [32–34] to address the needs of older EGS patients. We have developed a general surgical in-reach service in the last 3 years, and in this time have had input into more than 1300 older people. Two consultant geriatricians provide five direct clinical care sessions to the general surgical wards weekly.
Overall, responsibility for patients remains with the parent surgical team but during their hospital stay patients undergo multiprofessional assessment and interventions, regular clinical review by geriatricians, and weekly multidisciplinary team (MDT) discussion.
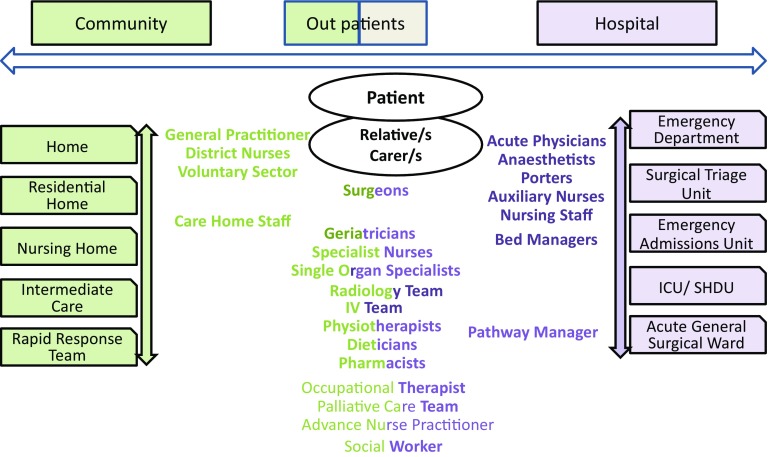
For each older person, our team proactively scrutinise the electronic patient record before clinical assessment is undertaken. Figure 2 shows a schematic representation of the main components of our service. Figure 3 shows different members of the MDT and interactions between primary and secondary care.
Fig. 2.
Main components of Salford-POP-GS Surgical In-reach Team. (1) Proactive, daily case finding via electronic patient records of patients over 74 years of age. (2) Multidisciplinary Team work
Fig. 3.
Members of the Surgical Multidisciplinary Team
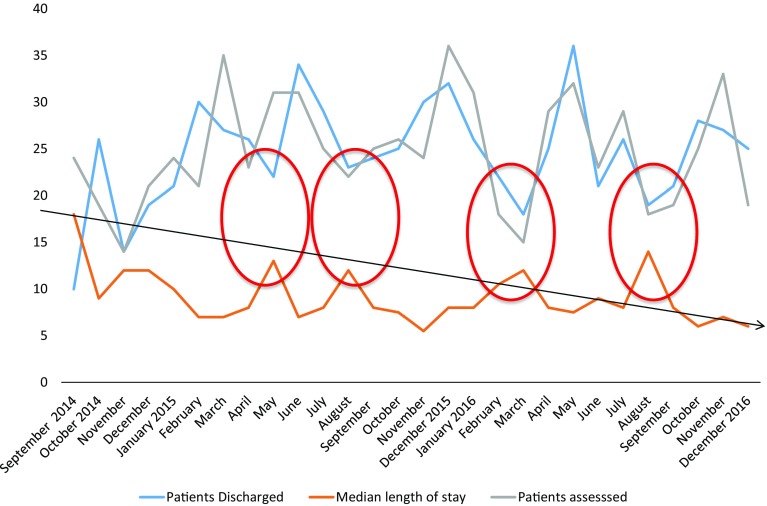
We routinely provide care for patients managed medically or with non-surgical interventions such as therapeutic endoscopy including cholangiopancreatography and stent insertion, and cholecystostomy. We also review the majority of older people managed with a surgical procedure, peri-operatively. Figure 4 demonstrates the number of patients assessed by our service and discharged between September 2014 and December 2016, as well as their median length of stay (LOS). The 1st February 2015, was when our in-reach service was deemed fully consolidated and median LOS was shown to drop from 12.2 days before this date to 9 days after. Our service is reliable except when one of the consultant geriatricians is away on prolonged annual leave. In these circumstances, number of discharges drop and length of stay has been shown to increase as shown in Fig. 4. All four red circles coincide with leave taken by one of the geriatricians.
Fig. 4.
Salford-POPS-GS September 2014 to December 2016. Patients assessed, discharged and their length of stay. Circles represent periods of time with significant reductions in number of patients assessed/discharged and longer LOS
While a majority of older people are reviewed by our service, pre-operative assessment and optimisation prove challenging given our limited resources. We hope that the inclusion to the team of an Advance Nurse Practitioner will allow us to do more of this work as well as providing better continuity of care, and avoid the demonstrated variations in discharge rate and LOS.
Early CGA delivered by our team has allowed stratification of risk, and supported decision making around suitability for surgery. It has also been shown to minimise adverse drug events and polypharmacy, and allowed early identification and treatment of complications when they arose. Working as a multidisciplinary team has streamlined discharge planning, optimised the use of rehabilitative resources, and improved discussions between health professionals, patients, carers and relatives. The team’s efforts have resulted in reductions in hospital length of stay, lower readmission rates and improvements in coding. The service has also reduced involvement of other specialist teams and urgent reviews by the medical on call team, resulting in better continuity of care. Patient and staff satisfaction have improved.
Risk stratification
Older people are a heterogeneous population with a spectrum of pre-hospital states varying from the robust to the very dependent [3, 5]. Currently, with improved pharmacotherapy and interventions to manage co-existing multimorbidity, age should no longer be an absolute contraindication to surgery. Indeed, studies that have demonstrated a causal relationship between age and mortality include significant confounding factors as a caveat to interpretation. There is a significant evidence base supporting the use of both P-POSSUM and American Society of Anaesthetists (ASA) score [35, 36] in predicting in-hospital mortality. However, in our experience, impaired cognition and functional status, and the presence of incontinence also reliably predict in-hospital mortality. These are domains that are rarely considered by surgical teams at patient presentation but are routinely assessed as part of CGA.
There is a subset of patients in which active management is considered unsuitable or futile, for example, patients who are in ASA Class V or who present with inoperable disease. In this setting, patients and/or their family and carers should be encouraged to play an active role in decision making and advanced care planning. The geriatrician has a key role in empowering patients and their caregivers to set realistic goals and avoid futile care or unnecessary procedures if they are approaching the end of their life.
Conundrums in emergency general surgery
There is an insufficient evidence base outlining the best way to assess, manage and rehabilitate older EGS patients and this needs addressing as a matter of urgency.
Randomised controlled and cohort studies are necessary to determine the most efficient models of care and to construct reliable and accurate risk stratification tools when considering emergency surgery. The cost-effectiveness of such services would also need to be determined for sustainability.
Conclusions and key messages
The population is ageing and increasing numbers of older people will require EGS.
While elective surgery rates decrease drastically in patients over the age of 75 years, rates of emergency interventions rise.
Although older EGS patients form a heterogeneous group of individuals, advanced age, polypharmacy and multimorbidity are the norm.
Hospital length of stay and mortality, complication, rehospitalisation and institutionalisation rates are significantly higher in older people compared to younger individuals.
Comprehensive Geriatric Assessment, targeted patient-centred multidisciplinary interventions and timely discharge planning improve clinical outcomes in older EGS patients.
Anaesthetists, surgeons and geriatricians should receive formal training in the assessment and management of older EGS patients.
Collaborative care is the future.
There is an urgent need to carry out high quality research into models of care, risk stratification, pre-operative optimisation and frailty.
We advocate a personalised, multidisciplinary and holistic approach for all older surgical patients, particularly those presenting acutely. Collaborative work involving surgeons, anaesthetists, intensivists, geriatricians and the multidisciplinary team is of paramount importance to optimise clinical outcomes and patient experience.
Compliance with ethical standards
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
References
- 1.Eurostat (2017) Population structure and ageing. http://ec.europa.eu/eurostat/statistics-explained/index.php/Population_structure_and_ageing. Accessed 14 Nov 2017
- 2.Royal College of Surgeons. Access all ages 2: assessing impact of age on access to surgical treatment 2014. https://www.rcseng.ac.uk/library-and-publications/college-publications/docs/access-all-ages-2. Accessed 14 Nov 2017
- 3.Chana P, Joy M, Casey N, et al. Cohort analysis of outcomes in 69490 emergency general surgical admissions across an international benchmarking collaborative. BMJ Open. 2017;7:e014484. doi: 10.1136/bmjopen-2016-014484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gale SC, Shafi S, Dombrovskiy VY, et al. The public health burden of emergency general surgery in the United States: a 10-year analysis of the Nationwide Inpatient Sample–2001 to 2010. J Trauma Acute Care Surg. 2014;77:202–208. doi: 10.1097/TA.0000000000000362. [DOI] [PubMed] [Google Scholar]
- 5.McLean RC, McCallum IJ, Dixon S, et al. A 15-year retrospective analysis of the epidemiology and outcomes for elderly emergency general surgical admissions in the North East of England: a case for multidisciplinary geriatric input. Int J Surg. 2016;28:13–21. doi: 10.1016/j.ijsu.2016.02.044. [DOI] [PubMed] [Google Scholar]
- 6.St-Louis E, Sudarshan M, Al-Habboubi M, et al. The outcomes of the elderly in acute care general surgery. Eur J Trauma Emerg Surg. 2016;42:107. doi: 10.1007/s00068-015-0517-9. [DOI] [PubMed] [Google Scholar]
- 7.The association of Surgeons of Great Britain and Irlean (2015) Emergency surgery: the future. ASGBI, London. https://www.acpgbi.org.uk/content/uploads/2016/07/Future-of-EGS-joint-document_Iain-Anderson_140915.pdf. Accessed 14 Nov 2017
- 8.Health Social Care Information Centre Hospital Episode Statistics: Hospital Admitted Patient Care Activity, 2015 to 2016. http://digital.nhs.uk/pubs/apc1516. Accessed 14 Nov 2017
- 9.Shah AA, Zafar SN, Kodadek LM, et al. Never giving up: outcomes and presentation of emergency general surgery in geriatric octogenarian and nonagenarian patients. Am J Surg. 2016;212:211–220. doi: 10.1016/j.amjsurg.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 10.NELA Project Team. Third patient report of the national emergency laparotomy audit, RCoA, London, 2017. file:///V:/Desktop/The%20Third%20Patient%20Report%20of%20the%20National%20Emergency%20Laparotomy%20Audit%202017%20-%20Full%20Patient%20Report.pdf. Accessed 14 Nov 2017
- 11.Scott JW, Olufajo OA, Brat GA, et al. Use of national burden to define operative emergency general surgery. JAMA Surg. 2016;151:e160480. doi: 10.1001/jamasurg.2016.0480. [DOI] [PubMed] [Google Scholar]
- 12.Scarborough JE, Schumacher J, Pappas TN, et al. Which complications matter most? Prioritizing quality improvement in emergency general surgery. J Am Coll Surg. 2016;222:515–24. doi: 10.1016/j.jamcollsurg.2015.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merani S, Payne J, Padwal RS, et al. Predictors of in-hospital mortality and complications in very elderly patients undergoing emergency surgery. World J Emerg Surg. 2014;9:43. doi: 10.1186/1749-7922-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hewitt J, McCormack C, Tay HS, et al. Prevalence of multimorbidity and its association with outcomes in older emergency general surgical patients: an observational study. BMJ Open. 2016;6:e010126. doi: 10.1136/bmjopen-2015-010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vilches-Moraga A, Fox J, et al. Baseline characteristics and clinical outcomes of older patients admitted as an emergency to general surgical wards. Salford-POPS-GS. Eur Geriat Med. 2017 [Google Scholar]
- 16.Hewitt J, Moug SJ, Middleton M, et al. Older Persons Surgical Outcomes Collaboration. Prevalence of frailty and its association with mortality in general surgery. Am J Surg. 2015;209:254–259. doi: 10.1016/j.amjsurg.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 17.Joseph B, Zangbar B, Pandit V, et al. Emergency general surgery in the elderly: too old or too frail? J Am Coll Surg. 2016;222:805–813. doi: 10.1016/j.jamcollsurg.2016.01.063. [DOI] [PubMed] [Google Scholar]
- 18.Partridge JSL, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing. 2012;41:142–147. doi: 10.1093/ageing/afr182. [DOI] [PubMed] [Google Scholar]
- 19.ASGBI ACGBI, AUGIS. The future of emergency general surgery, a joint document 2015 https://www.acpgbi.org.uk/content/uploads/2016/07/Future-of-EGS-joint-document_Iain-Anderson_140915.pdf. Accessed 14 Nov 2017
- 20.ASGBI, RCSEd. EGS board and national acute surgery forum. Emergency General Surgery, a consensus statement 2017. http://www.asgbi.org.uk/emergency-general-surgery-a-consensus-statement/EGS%20Website%20statement.pdf. Accessed 14 Nov 2017
- 21.Braude P, Partridge JSL, Shipway D, et al. Perioperative medicine for older patients: how do we deliver quality care? Future Hosp J. 2016;3:33–36. doi: 10.7861/futurehosp.3-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wachter RM. The hospitalist movement 5 years later. JAMA. 2002;287:487. doi: 10.1001/jama.287.4.487. [DOI] [PubMed] [Google Scholar]
- 23.Harari D, Hopper A, Dhesi J, et al. Proactive care of older people undergoing surgery (‘POPS’): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing. 2007;36:190–196. doi: 10.1093/ageing/afl163. [DOI] [PubMed] [Google Scholar]
- 24.Desserud KF, Veen T, Søreide K. Emergency general surgery in the geriatric patient. Br J Surg. 2016;103:52–61. doi: 10.1002/bjs.10044. [DOI] [PubMed] [Google Scholar]
- 25.Torrance ADW, Powell SL, Griffiths EA. Emergency surgery in the elderly: challenges and solutions. Open Access Emerg Med OAEM. 2015;7:55–68. doi: 10.2147/OAEM.S68324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colburn JL, Mohanty S, Burton JR. Surgical guidelines for perioperative management of older adults: what geriatricians need to know. J Am Geriatr Soc. 2017;65:1339–1346. doi: 10.1111/jgs.14877. [DOI] [PubMed] [Google Scholar]
- 27.Ellis G, Whitehead MA, Robinson D, et al. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553. doi: 10.1136/bmj.d6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feng MA, McMillan DT, Crowell K, et al. Geriatric assessment in surgical oncology: a systematic review. J Surg Res. 2015;193:265–72. doi: 10.1016/j.jss.2014.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Partridge JS, Harari D, Martin FC, et al. The impact of pre-operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia. 2014;69:8–16. doi: 10.1111/anae.12494. [DOI] [PubMed] [Google Scholar]
- 30.Hawley S, Javaid MK, Prieto-Alhambra D, et al. Judge a the REFReSH study group. Clinical effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: population-based longitudinal study. Age Ageing. 2016;45:236–242. doi: 10.1093/ageing/afv204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Partridge JSL, Collingrige G, Gordon AL, et al. Where are we in perioperative medicine for older surgical patients? A UK survey of geriatric medicine delivered services in surgery. Age Ageing. 2014;43:721–724. doi: 10.1093/ageing/afu084. [DOI] [PubMed] [Google Scholar]
- 32.Mohanty S, Rosenthal RA, Russell MM, et al. Optimal perioperative management of the geriatric patient: a best practices guideline from the American College of Surgeons NSQIP and the American Geriatrics Society. J Am Coll Surg. 2015;222:930–947. doi: 10.1016/j.jamcollsurg.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 33.Griffiths R, Beech F, Brown A, et al. Peri-operative care of the elderly 2014: association of anaesthetists of Great Britain and Ireland. Anaesthesia. 2014;69:81–98. doi: 10.1111/anae.12617. [DOI] [PubMed] [Google Scholar]
- 34.Dhesi JK (2013) Setting up a proactive service to make surgery safer for older people. The Health Foundation, London. http://patientsafety.health.org.uk/sites/default/files/resources/setting_up_a_proactive_service_to_make_surgery_safer_for_older_people_1.pdf. Accessed 14 Nov 2017
- 35.Middleton M, Stechman M, Moug S, et al. Risk prediction tools for older general surgical patients. Rev Clin Gerontol. 2015;25:12–21. doi: 10.1017/S0959259815000027. [DOI] [Google Scholar]
- 36.American Society of Anesthesiologists - ASA Physical Status Classification System [Internet]. http://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system. Accessed 14 Nov 2017