Abstract
Background:
Falling and fear of falling are among the most common problems of the elderly, which can cause illness, isolation, dependency and reduced quality of life in elderly. Exercise is recommended to prevent falling injuries in the elderly.
Aim:
This study aimed to examine the effect of Tai Chi exercise on the risk and fear of falling in older adults.
Materials and Methods:
In this randomized clinical trial, a total of 60 male and female elderly were randomly divided into two groups: Tai Chi exercise and control (daily activities) groups. Tai Chi exercise protocol in the intervention group consisted of 3 sessions per week for 10 weeks. The risk and fear of falling were assessed in subjects by using standardized questionnaires, including Berg’s Balance Scale and Fall Efficacy Scale-International (FES-I) before initiating the protocol, at the end of 4th, 8th weeks and at the end of exercise period.
Results:
Two groups were matched in terms of age, gender, education, and body mass index. Baseline values of risk of falling and fear of falling were not significantly different between the two groups (P>0.05). The score of fear of falling at the end of 4th, 8th weeks and at the end of exercise period was significantly different between the two groups (P<0.05) and it decreased in the intervention group, but the risk of falling reduced after 8 and 10 weeks in the intervention group (P<0.001).
Conclusion:
Performing Tai Chi exercises for at least four weeks could reduce fear of falling and reduce the risk of falls in older adults after 8 weeks.
Keywords: Tai Chi, Exercise, Accidental Falls, Aged, Postural Balance
1. INTRODUCTION
Falls are prevalent among older adults, and are a major threat to their health (1). Because of the high risk of falling in the elderly, falling is known as “aging syndrome” (2). Every year, nearly 30% of people over 65 years old, experience falling at least once a year, half of which happen for multiple times (3). Falling in elderly is associated with complications that causes prolonged hospitalization, isolation, dependency, immobility, decreased function, increased mortality rate and increased healthcare costs (4-6). This issue emphasizes the need to implement preventive measures in order to avoid it from happening again in the elderly (4). Various risk factors such as lack of balance, visual impairment, motor impairment, cognitive impairment and fear of falling are associated with falling in the elderly (7). Although some risk factors such as age and gender cannot be modified, other factors are potentially modifiable (8).
About one-third of the elderly who experience falling and half of them who have never fallen have fear of falling (9-10). Fear of falling is a problematic consequence that can create a cyclic pattern of movement disorders, social isolation, and reduced quality of life, even without any experience of falling in the elderly (11). The prevalence of fear of falling has been reported between 20-85% (9, 12). Thus, fear of falling can become a debilitating problem and have numerous consequences such as disability and dependency on others for daily activities, depression, lack of independence and need ingtoassistive devices such as cane for moving, that can lead to further restrictions of the elderly individuals in performing daily activities (13, 14).
Exercise is one of the most important non-pharmacological interventions in preventing falls in elderly (15-17). Although exercise is recommended to reduce the risk of falling in the elderly, if it is not conducted properly, it could lead to negative consequences and injuries (18-20). Tai Chi is an ancient exercise that helps elderly to maintain balance, give them a better body-sense (21) and therefore appears to be associated with less injury in older adults (22). Physical and cognitive coordination in Tai Chi exercise shows the value of this exercise in prevention of falls, compared to other sport programs that focus on muscle strength. On the other hand, Tai Chi exercise increases the awareness of the individual from his balance and can reduce fear of falling (23). Although the results of some clinical trials suggested that Tai Chi exercise can prevent falling in older adults, this finding was not confirmed by other studies (17, 24-26).
Additionally, a recent meta-analysis recommends additional studies to evaluate the efficacy of Tai Chi exercise on fall prevention in older adults (27). Therefore, due to the importance of fall prevention in older adults and likelihood benefit of Tai Chi exercise, as well as controversial evidence to support its efficacy in fall prevention, the aim of this study was to evaluate the effect of Tai Chi exercise on risk and fear of falling in older adults.
2. MATERIALS AND METHODS
After obtaining approval from the North Khorasan University of Medical Sciences ethics committee and informed consents from the participants, a total number of 60 older adults (30 females and 30 males) of both sexes, who referred to health care centers of Mashhad, northeast Iran, between February 2015 and November 2016, were enrolled in this prospective, randomized clinical trial. The inclusion criteria consisted of age over 60, living in society (not nursing home), no regular exercise (especially Tai Chi) in the past 6 months, mental alertness, lack of medical contra indications for exercise, lack of destructive mental disorders such as dementia and Parkinson, and ability to exercise. Older adults with serious disease or life-threatening emergency situation during exercise, those who were not capable of completing the exercise program, referred irregularly for Tai Chi, or had a substantial change in treatment or drug regimens were excluded from the study.
Participants who fulfilled the inclusion criteria were randomly allocated into two equally sized groups (n=30, 15 male and 15 female) by a nurse who was blind to the study groups, using sealed envelope technique and block randomization. In order to homogenize the intervention and control groups, participants were matched in terms of age and body mass index (BMI). Before the study, demographic characteristic questionnaire, Berg’s balance tool, and Fall Efficacy Scale - International (FES-I) were completed for all participants. Also, all elderly groups were visited by a physician for medical indication for exercise. The study population was divided into 15-person groups, according to sex and exercised under coach’s supervision. Tai Chi instructors were certified coaches for Tai Chi (Yang style). For intervention group, sports program was exercised for 30 sessions (three sessions per week for 10 weeks) under the supervision of a coach. The control group continued their daily activities as routine of life. To assess the risk of falling, Berg’s Balance tool, and to measure the fear of falling, FES-I were completed at the end of the week fourth, eighth, and tenth in both intervention and control groups. There liability, and validity of Berg’s tool and have been established in previous studies by Pearson correlation coefficient of >0.7 (28-29). Questionnaires were completed by a person who was unaware of previous evaluation scores. Time of completing the questionnaire in all stages was 9-11 in the morning. This study registered in the Iranian Registry of Clinical Trials Database (IRCT2016120431234N1).
Statistical analysis
Shapiro-Wilk test was used to assess the assumption of normality of data. Baseline characteristics of the study groups were compared using Chi-square or Fisher’s exact tests for categorical and Wilcoxon rank-sum tests for continuous variables. To examine the effect of intervention, including main and interaction effects, a 2x 4 factorial repeated measures ANOVA was conducted, while study group was considered as between subject factor with two levels (intervention vs. control group), and time as within subject factor with four levels (before, 4, 8, and 10 week after protocol). Using Mauchly’s test, the sphericity was examined; and accordingly, the Greenhouse-Geisser estimates of sphericity was used. An alpha level of .05 was considered as statistical significance. Post-hoc analysis, using Bonferroni correction was conducted where the ANOVA model was statistically significant. Data were analyzed using SPSS Version 16.
3. RESULTS
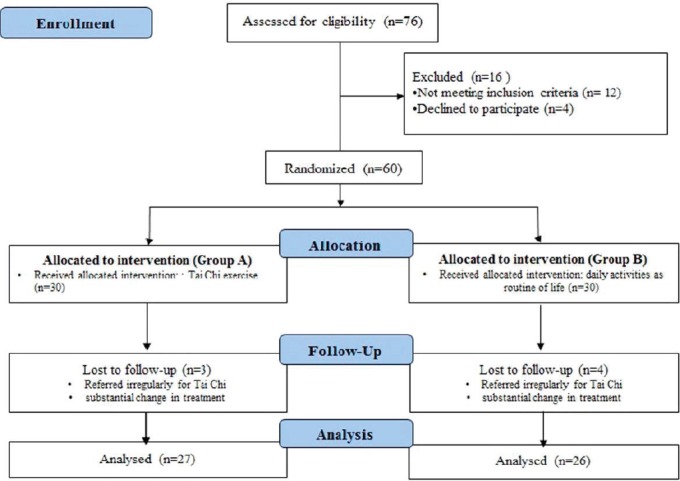
A total of 76 participants were screened during the study period. Of these, 12 participants did not meet the inclusion criteria and 4 patients declined to participate in the study. The remaining 60 participants were randomly allocated to two groups. Of these, 7 patients were lost to follow-up during the study period. In total, 53 participants completed the present study and data from all these participants were analyzed (Figure 1).
Figure 1. Flow chart of the study.
The basic demographic and clinical characteristics of the two groups are presented in Table 1. The results show that no statistically significant difference existed between the two groups (P>0.05).
Table 1. Demographic and clinical characteristics of the two study groups.
| Variable | Group of study | P value | ||
|---|---|---|---|---|
| Tai Chi exercise (n=27) | Control (n=26) | |||
| Age, years | 67.20±5.416 | 68.07±5.232 | 0.53 | |
| Female gender | 14 (51.8%) | 13 (50%) | 0.97 | |
| BMI | 27.15±4.42 | 28±4.83 | 0.48 | |
| Educational level | Uneducated | 3 (11.1) | 5 (19.2) | 0.88 |
| Primary school | 9 (33.4) | 7 (26.9) | ||
| Secondary school | 8 (29.6) | 9 (34.7) | ||
| Diploma and higher | 7 (25.9) | 5 (19.2) | ||
| History of falls | 0.37±0.66 | 0.47±0.776 | 0.59 | |
Evaluation of the mean scores of risk of falling and fear of falling before the implementation of the protocol in the intervention and control groups showed no significant differences between the intervention and control groups before the protocol that confirmed the homogeneity of the groups (Table 2).
Table 2. Mean scores of risk of falling and fear of falling.
| Intervention Group | Control Group | |||
|---|---|---|---|---|
| Time | Risk of Falling Mean (SD) | Fear of Falling Mean (SD) | Risk of Falling Mean (SD) | Fear of Falling Mean (SD) |
| Baseline | 47.10 (4.85) | 21.10 (4.66) | 43.60 (6.91) | 24.43 (6.88) |
| 4th week | 41.67 (4.69) | 26.87 (6.32) | 38.97 (5.30) | 31.07 (6.53) |
| 8th week | 49.93 (2.79) | 19.44 (2.64) | 38.81 (6.19) | 30.23 (6.76) |
| 10th week | 53.59 (2.36) | 17.81 (2.09) | 37.31 (6.05) | 32.50 (7.03) |
Mean scores of risk of falling between the two groups has been shown in Figure 2. To investigate the effect of Tai Chi exercise on risk of falling, based on Berg’s test, mean score of risk of falling was measured in two groups before, and at the end of the fourth, eighth and tenth week, after studying the 4 x 2 Factorial Repeated measures test using time variable at four levels (before, 4, 8, and 10 weeks after the study), and intervention variable at 2 levels of (Tai Chi exercise and normal activity) as independent qualitative variables, and “score of risk of falling”, based on Berg’s balance test, was the dependent variable. The results are shown in Table 3 that shows 44.2% decreased risk of falling in the intervention group (Tai Chi) compared to controls (normal activity) (P<0.001).
Figure 2. Mean scores of fear of falling in two groups.
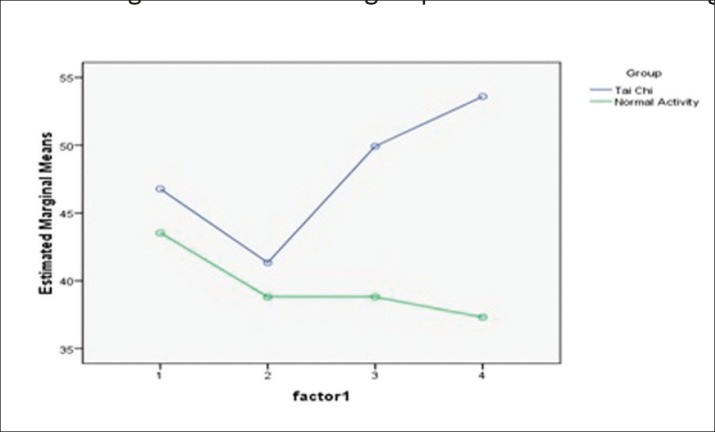
Table 3. Risk of falling based on repeated measures ANOVA.
| Statistical index | Sum of squares | df | Root-mean-square | F | P-value | Eta |
|---|---|---|---|---|---|---|
| Greenhouse-Geisser | 995.61 | 1.99 | 498.86 | 40.34 | 0.000 | 0.442 |
The results of t-test, as shown in Table 4,showed that the mean risk of falling before running the protocol and after the fourth week was not significantly different between the two groups (P>0.05), but there was a significant difference between the two groups at the end of the eighth and tenth week(P<0.001).
Table 4. Comparing mean score of risk of falling at different time periods in the two groups.
| Time intervals | Mean scores | Standard deviation | t | df | P-value |
|---|---|---|---|---|---|
| Before the study | 3.239 | 1.723 | 2.271 | 58 | 0.066 |
| End of the 4th week | 2.526 | 1.443 | 2.90 | 58 | 0.086 |
| End of the 8th week | 11.118 | 1.31 | 8.485 | 51 | <0.001 |
| End of the 10th week | 16.285 | 1.252 | 13.012 | 51 | <0.001 |
Fear of falling, like the risk of falling, was measured in both groups based on FES-I, using Factorial Repeated measures and the results (Table 5) showed 33.6% decreased fear of falling in the intervention group, compared to the control group (P<0.001).
Table 5. Fear of falling, based on repeated measures ANOVA.
| Statistical index | Sum of squares | df | Root-mean-square | F | P-value | Eta |
|---|---|---|---|---|---|---|
| Greenhouse-Geisser | 1107.09 | 1.76 | 625.88 | 25.83 | 0.000 | 0.336 |
Figure 3 shows the trend of mean scores of fear of falling in two groups. No significant differences were found in scores of fear of falling before the intervention, but after the fourth, eighth, and tenth week the differences between groups were significantly different (Table 6) (P<0.05).
Figure 3. Trtend of mean scores of fear of falling between the two groups.
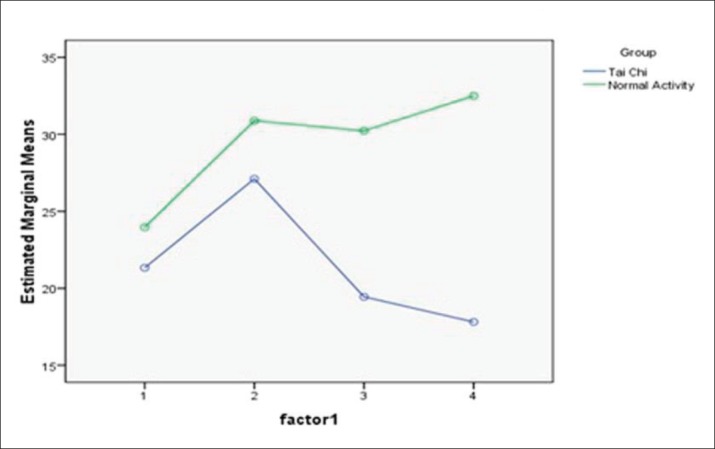
Table 6. Comparing mean score of fear of fallingat different time periods in the two groups.
| Time intervals | Mean scores | Standard deviation | t | df | P-value |
|---|---|---|---|---|---|
| Before the study | -2.628 | 1.665 | -2.196 | 58 | 0.121 |
| End of the 4th week | -3.774 | 1.813 | -2.531 | 58 | 0.042 |
| End of the 8th week | -10.786 | 1.40 | -7.707 | 51 | 0.000 |
| End of the 10th week | -14.685 | 1.413 | -10.393 | 51 | 0.000 |
4. DISCUSSION
The results of this study showed that Yang style Tai Chi exercise reduced risk and fear of falling in older adults. Mean score of risk of falling reduced in the elderly of the intervention group after the eighth week and the end of protocol, compared to controls, but risk of falling score increased in the fourth week in both groups.
Voukelatos et al. evaluated the effect of Tai Chi exercise on preventing fall in the elderly in Sydney, Australia, that included 702 elderly people, who were divided into two groups and received Tai Chi exercise for 16 weeks, 3 sessions per week for 40 minutes, which was 6 weeks more than the present study, while the session duration in our study was 20 minutes less. The results showed that the risk of falling significantly reduced after 16 weeks of Tai Chi, which is consistent with the present study (30). The results of another study by Li et al. showed that Tai Chi exercise reduces the risk of falling and improves walking in elderly, which is similar to the results of the current study (25). Taggart et al. investigate the effect of Tai Chi on balance, motor function and fear of falling in elderly women. Tai Chi was exercised twice a week for 3 months (26 sessions) that was less than the present study. The results indicate that Tai Chi exercise has significant influence on balance, motor function and fear of falling, which is consistent with the results of the present study (31). Song et al. investigated the effect of Tai Chi exercise on lower extremity muscle strength, bone density and balance function in older women. The results showed no significant difference after the fourth week between groups that is in line with the results of the present study. One possible explanation for this may be due to lack of knowledge of Tai Chi among the elderly. Though, after 8 and 12 weeks, significant differences were observed between the intervention and control groups (32). It has been indicated that increases in Tai Chi exercise frequency, and using the Yang style,is more effective in reducing the incidence of falls in older adults (27). Tai Chi exercise seems to integrate of the neural, muscular and skeletal function (15, 18, 21).
In the present study, the results of mean score of fear of falling, based on FES-I, in both intervention and control groups, showed a significant difference in the two groups in the fourth week, eighth week and tenth week, which shows that Tai Chi reduced 33.6% fear of falling in the intervention group than the control group. The result of the present study is consistent with other studies by Kooshiar et al. (33) and Khajavi et al. (34). Duration of both studies was eight weeks, 3 sessions per week for 20 minutes, with emphasis on fear of falls in elderly, using FES-I tool that is similar to the present study. Exercises in Khajavi’s study included training program focusing on central function and the study by Kooshiar et al. included entertaining physical activity that were different from the present study that included Tai Chi exercise, but were similar in terms of results on fear of falling. It can be assumed that Tai Chi and physical activity can help boost the confidence and reduce fear of falling in the elderly. However, reduced fear of falling in the present study was 33.6% that was higher, compared to the other studies (33-34). Tai Chi exercise can improve balance in the elderly, as well as increase their motivation, confidence, happiness, and positive energy, independence in their activities, and thus reduce the risk of falls and more importantly, the fear of falling, which is expected to improve the situation of the elderly and help active and dynamic elderly in the community (20, 23, 27).
Lack of familiarity of the elderly with Tai Chi exercise, lack of an appropriate place for exercise and lack of cooperation of health centers were the limitations of the study.
5. CONCLUSION
The results of the present study showed that Tai Chi exercise significantly reduced the risk and fear of falling in the elderly. It seems that, Tai Chi exercise,as a harmless intervention and complication-free intervention, can play a significant role in improving balance and motor function in elderly and increasing their independence power and enable enjoyable and dynamic elderly.
Acknowledgements
This study is a result of the master’s thesis in Geriatric Nursing, supported financially by North Khorasan University of Medical Sciences, Bojnurd, Iran. We express our fullest gratitude to those who helped us in conducting this research.
Author’s contributions:
Study conception and design: HM, MT, AG, MRA and MRY. Acquisition of data: HM and MRY. Statistical analysis and interpretation of data: MRA and HM. Drafting of the manuscript: HM, MT, AG, MRA and MRY. Critical revision of the manuscript for important intellectual content: HM, MT, AG, MRA and MRY.
Conflicts of interest:
All authors declare no conflict of interest; no conflict of interest exists for any of the authors associated with the manuscript. The funding organization had no role in the design and conduct of the study, or in the collection, analysis, and interpretation of the data.
REFERENCES
- 1.Howcroft J, Kofman J, Lemaire ED. Review of fall risk assessment in geriatric populations using inertial sensors. J Neuroeng Rehabil. 2013;10(1):91. doi: 10.1186/1743-0003-10-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ness KK, Gurney JG, Wall MM, Olsen RA, Boergerhoff LA. Screening for risk of falling in community-dwelling elderly people may increase fear of falling. J Geriatr Phys Ther. 2004;27(3):100–4. [Google Scholar]
- 3.Soriano TA, DeCherrie LV, Thomas DC. Falls in the communitydwelling older adult: a review for primary-care providers. Clin Interv Aging. 2007;2(4):545–54. doi: 10.2147/cia.s1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bretan O. Plantar cutaneous sensitivity as a risk for falls in the elderly. Rev Assoc Med Bras. 2012;58(2):132. [PubMed] [Google Scholar]
- 5.da Costa BR, Rutjes AW, Mendy A, Freund-Heritage R, Vieira ER. Can falls risk prediction tools correctly identify fall-prone elderly rehabilitation inpatients? A systematic review and meta-analysis. PLoS One. 2012;7(7):e41061. doi: 10.1371/journal.pone.0041061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lusardi MM, Fritz S, Middleton A, Allison L, Wingood M, Phillips E, et al. Determining Risk of Falls in Community Dwelling Older Adults: A Systematic Review and Meta-analysis Using Posttest Probability. J Geriatr Phys Ther. 2017;40(1):1–36. doi: 10.1519/JPT.0000000000000099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dionyssiotis Y. Analyzing the problem of falls among older people. Int J Gen Med. 2012;5:805–13. doi: 10.2147/IJGM.S32651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 9.Rao SS. Prevention of falls in older patients. Am Fam Physician. 2005;72(1):81–8. [PubMed] [Google Scholar]
- 10.Jung D. Fear of falling in older adults: comprehensive review. Asian Nurs Res (Korean Soc Nurs Sci) 2008;2(4):214–22. doi: 10.1016/S1976-1317(09)60003-7. [DOI] [PubMed] [Google Scholar]
- 11.Sattin RW, Easley KA, Wolf SL, Chen Y, Kutner MH. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. J Am Geriatr Soc. 2005;53(7):1168–78. doi: 10.1111/j.1532-5415.2005.53375.x. [DOI] [PubMed] [Google Scholar]
- 12.Mane AB, Sanjana T, Patil PR, Sriniwas T. Prevalence and correlates of fear of falling among elderly population in urban area of Karnataka, India. J Midlife Health. 2014;5(3):150–5. doi: 10.4103/0976-7800.141224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brouwer B, Musselman K, Culham E. Physical function and health status among seniors with and without a fear of falling. Gerontology. 2004;50(3):135–41. doi: 10.1159/000076771. [DOI] [PubMed] [Google Scholar]
- 14.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing. 2004;33(3):273–9. doi: 10.1093/ageing/afh077. [DOI] [PubMed] [Google Scholar]
- 15.Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. 2010;24(6):e1–e25. doi: 10.4278/ajhp.081013-LIT-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12-month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. J Am Geriatr Soc. 1995;43(11):1198–206. doi: 10.1111/j.1532-5415.1995.tb07394.x. [DOI] [PubMed] [Google Scholar]
- 17.Faber MJ, Bosscher RJ, Chin A, Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: A multicenter randomized controlled trial. Arch Phys Med Rehabil. 2006;87(7):885–96. doi: 10.1016/j.apmr.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 18.Low S, Ang LW, Goh KS, Chew SK. A systematic review of the effectiveness of Tai Chi on fall reduction among the elderly. Arch Gerontol Geriatr. 2009;48(3):325–31. doi: 10.1016/j.archger.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 19.Wolfson L, Whipple R, Derby C, Judge J, King M, Amerman P, et al. Balance and strength training in older adults: intervention gains and Tai Chi maintenance. J Am Geriatr Soc. 1996;44(5):498–506. doi: 10.1111/j.1532-5415.1996.tb01433.x. [DOI] [PubMed] [Google Scholar]
- 20.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(12):2234–43. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 21.Huston P, McFarlane B. Health benefits of tai chi: What is the evidence? Can Fam Physician. 2016;62(11):881–90. [PMC free article] [PubMed] [Google Scholar]
- 22.Lin MR, Hwang HF, Wang YW, Chang SH, Wolf SL. Communitybased tai chi and its effect on injurious falls, balance, gait, and fear of falling in older people. Phys Ther. 2006;86(9):1189–201. doi: 10.2522/ptj.20040408. [DOI] [PubMed] [Google Scholar]
- 23.Song QH, Shen GQ, Xu RM, Zhang QH, Ma M, Guo YH, et al. Effect of Tai Chi exercise on the physical and mental health of the elder patients suffered from anxiety disorder. Int J Physiol Pathophysiol Pharmacol. 2014;6(1):55–60. [PMC free article] [PubMed] [Google Scholar]
- 24.Woo J, Hong A, Lau E, et al. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing. 2007;36:262–8. doi: 10.1093/ageing/afm005. [DOI] [PubMed] [Google Scholar]
- 25.Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60:187–94. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 26.Taylor-Piliae RE, Hoke TM, Hepworth JT, et al. Effect of Tai Chi on physical function, fall rates and quality of life among older stroke survivors. Arch Phys Med Rehabil. 2014;95:816–24. doi: 10.1016/j.apmr.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 27.Huang ZG, Feng YH, Li YH, Lv CS. Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open. 2017;7:e013661. doi: 10.1136/bmjopen-2016-013661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, et al. Development and initial validation of the Falls Efficacy Scale-International (FES-I) Age Ageing. 2005;34(6):614–9. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- 29.Wirz M, Müller R, Bastiaenen C. Falls in persons with spinal cord injury: validity and reliability of the Berg Balance Scale. Neurorehabil Neural Repair. 2010;24(1):70–7. doi: 10.1177/1545968309341059. [DOI] [PubMed] [Google Scholar]
- 30.Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. J Am Geriatr Soc. 2007;55(8):1185–91. doi: 10.1111/j.1532-5415.2007.01244.x. [DOI] [PubMed] [Google Scholar]
- 31.Taggart HM. Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older women. Appl Nurs Res. 2002;15(4):235–42. doi: 10.1053/apnr.2002.35975. [DOI] [PubMed] [Google Scholar]
- 32.Song QH, Zhang QH, Xu RM, Ma M, Zhao XP, Shen GQ, et al. Effect of Tai-chi exercise on lower limb muscle strength, bone mineral density and balance function of elderly women. Int J Clin Exp Med. 2014;7(6):1569–76. [PMC free article] [PubMed] [Google Scholar]
- 33.Kooshiar H, Najafi Z, Mazlom SR, Azhari A. Comparison of the effects of exhilarating and normal physical activities on the balance and fear of falling in the elderly residing in nursing homes of Mashhad. Evidence Based Care Journal. 2015;5(1):35–46. [Google Scholar]
- 34.Khajavi D, Farokhi A, Jaberi Moghadam A A, Kazemnejad A. The impact of a training intervention program on fall-related psychological factors among male older adults in Arak. Salmand. 2014;9(1):32–9. [Google Scholar]


