Abstract
Introduction:
The protective benefit of male circumcision against spreading HIV is well established.
Aim:
The objective of this Meta-analysis was to investigate behavioral risk compensation measured as the change in condom use behavior in light of knowledge of the benefits of circumcision.
Material and Methods:
A systematic search was conducted from 6 bibliographic databases for studies that quantitatively assessed a link between male circumcision and condom use behavior. Pooled odd ratios (OR) of condom use during any sexual activity were generated from three cohort studies and two Randomized Control Trails (RCT) that were included in the review.
Results:
The pooled effects from cohort and RCTs were not statistically significant at 6 months follow-up (OR=0.91, 95% CI: 0.57–1.45), at 12 months (OR=1.08, 95% CI=0.87–1.34) and 24 or more months (OR=1.11, 95% CI: 0.85, 1.45).
Conclusion:
Male circumcision does not influence condom use behavior in the medium and short term.
Keywords: Condom use, behavioral change, circumcision, sexual health
1. INTRODUCTION
For more than three decades, HIV/AIDS has devastated many parts of the world and in response researchers and policy makers have come together to develop ways of combating its spread. Circumcision is one of the most recent prevention technologies and it entails the surgical removal of the foreskin among males. Circumcision modifies penile biological factors such as the degree of tissue keratinization, density and superficiality of HIV target cells as well as alteration of the penile micro environment. This reduces intercourse related trauma and the possibility of retaining infectious secretions below the foreskin all of which work to reduce the likelihood of infection (1). On 13 December 2006, the United States of America National Institutes of Health announced that two randomized control trials (RCT) (2, 3) were to be halted prematurely because of a clear exhibition of the evidence of the protective benefits of this procedure against spreading HIV infection (2). This resulted into policy level implementation in some countries (3).
However, in one of the trials (4) that are fronted confirming the protective benefits of the procedure, it was found that there were increases in risky behaviors such as unprotected sex and number of sexual partners. Behavioral change preceded by possession of knowledge of protective benefits is referred to as behavioral risk compensation. In general terms, it entails an increase in a risky behavior as a result of someone having knowledge which leads to a perception of reduced vulnerability to the disease (5, 6). In relation to male circumcision (MC) and condom use behavior for example, risk compensation would imply a reduction in condom use following circumcision and knowledge of its protective benefits against infection.
Amongst some individuals and communities, fears that MC may impede other protective sexual behaviors have been expressed (7-9). At the back end of stagnation in HIV infection rates (10), the claim of risky sexual behavior disparities such as condom use between circumcised and uncircumcised individuals may not be completely unfounded. However, the practicability of assessing condom use behavioral risk compensation attributable to MC from existing literature is limited given that very few experimental or longitudinal studies have been conducted after the establishment of clear evidence of the MC’s protective benefits against sexually transmitted infections. The definition of risk compensation (5, 6) warrants that individuals possess knowledge of the protective benefits of circumcision. Nonetheless, in order to investigate whether the prevailing fears about circumcision’s impediment of condom use are founded, evidence can be sourced from currently existing experimental and longitudinal studies on MC and related sexual behavior prior to and after establishment of the veridicality of the knowledge of the procedure’s benefits. With the haste with which circumcision is being implemented in many countries it is imperative to establish whether circumcision and sexual behaviors such as condom use might be related since circumcision only confers partial protection against sexually transmitted infections (11).
The aim of this study is to review and summarize evidence on the association between male circumcision and condom use behavior from existing scientific literature. The results of the review should add to the existing evidence regarding the protective benefits of circumcision and ensure that the protective benefits of the procedure are not disaffirmed by more reckless sexual behavior.
2. METHODS
Identification of studies
Relevant studies were systematically searched in 6 bibliographic databases of: PubMed, Embase, Applied Social Sciences Index & Abstracts (ASSIA), PsycINFO, Scopus and Web of Science. The search terms comprised of subject headings and Boolean operators in titles, abstracts, topics and keywords. The search words used were circumcision, and risk compensation. Additionally, a snowballing technique was applied by searching through reference lists of identified articles to access more articles which had not been identified from the database search. The database search was conducted by the first and second author for studies published until August 15 2017.
Study Eligibility
Cohort and experimental studies that documented both circumcision and condom use behavior were eligible for inclusion in the review. The studies included had to draw samples from general populations, clearly explaining how the assessments for the condom use behavior were conducted, and also explicitly identify in which population group the assessments were conducted. Studies also had to longitudinally assess condom use behavior and as such all cross sectional studies, systematic reviews and studies with results derived from mathematical or theoretical modeling were excluded. Citations that were in form of essays/commentaries or letters to the editor were also excluded.
Data extraction
From each study, data including the author, date of publication, sample size, nature of the condom use behavior, country in which study was conducted, study recruitment period, the length of follow up, the statistical means of measurement and the risk of bias were extracted. A uniform outcome measure was then developed since condom use had originally been assessed in various ways. Some studies (12, 13) had applied a categorical variable of 3 levels i.e. consistent condom use, inconsistent condom use and no condom use while others documented condom use behavior in a binary format i.e. unprotected intercourse in the last six months (4) and condom use at last sex (14). For purposes of consistency, the outcome variable was reconstructed in terms of reported condom use during any sexual activity for respective follow-up period. This implied that the reported condom use that was categorized as consistent, inconsistent and no condom use was re-constructed by merging consistent condom use and inconsistent condom use in to one group to which those that reported no condom use during any sexual activity were compared.
Statistical analysis
Using STATA 13 statistical software package (15), the RCTs and cohort studies were quantitatively combined to generate pooled effects (Odds ratio) of circumcision status on reported condom use during any sexual activity at 6, 12 and 24 or more months periods of follow-up. In order to generate these Odds Ratios, 2x2 tables were extracted from the respective studies as described below: From the study of Bailey and colleagues (4), results presented in Table 4 of that paper were used. From the variable, “Unprotected sexual intercourse with any partner in the previous 6 months,” the OR for protected sexual intercourse with any partner in previous 6 months was computed. This was done for 6, 12 and 24 months follow-up.
From the study of Gray and colleagues (12) results in Table 6 of that paper were used to extract data on condom use. A binary outcome was formed by combining the number of participants for Consistent condom use and Inconsistent condom use into one category to which the second category No condom use was compared in order to compute the OR. This was done for 6, 12 and 24 months follow-up. From the study of Westercamp et al (14), using results in Figure 3 (a) of that paper, we considered the outcome of men that reported using condoms the last time they had sex (among sexually active). The OR for condom use during the last sexual activity was then computed. This was done for 6, 12 and 24 months follow-up
From the study of Kagaayi et al. (16) using results in Table 2 of the paper, we considered the outcome of men that reported using condoms during their last non-marital sex. The OR for condom use during the last non-marital sex was then computed. This was done for 24 or more months’ follow-up period
From the study of Agot and colleagues (13), using results from Table 4 of that paper, the data on condom use were considered. A binary outcome was formed by combining the number of participants who reported consistent condom use and inconsistent condom use into one category to which the second category of those that reported No condom use was compared to compute the OR. This was done for two follow-up periods of: 4 to 6 and 9 to 12 months follow-up.
Three sets of Meta analyses were conducted for results from 6 months, 12 months and 24 months’ follow-up periods. However, one prospective study (13) had follow up periods ranging between 4-6 months and then 9-12 months and so these were classified under 6 months and 12 months follow-up periods respectively. The other prospective study (16) had a follow-up period between 15-21 months and so this was classified under 24 or more months’ follow-up period. Assessment of statistical heterogeneity was done using the Cochran’s Chi square statistic. Upon all the 3 sets of Meta analyses fulfilling heterogeneity, DerSimonian and Laird random effects meta-analysis was conducted. We used the Cochrane collaborations tools (17) for assessing risk of bias in RCTs and cohort studies. Sensitivity analysis was also conducted after reconstructing the outcome variable. For this analysis, the reported condom use that was categorized as consistent, inconsistent and no condom use was re-constructed by leaving out the category of inconsistent thereby obtaining a binary outcome of consistent condom use and no condom use. Three sets of Meta analyses were conducted for results from 6 months, 12 months and 24 months’ follow-up periods similar to that described earlier in the analysis section.
Table 1. Characteristics of studies included in the review.
| Study design | Author | Sample size | Measure | Follow-up (months) | Risk of bias | Country | Recruitment period |
|---|---|---|---|---|---|---|---|
| RCT | Bailey et al 2007 (4) | 2,784 | unprotected sex with any partner in previous 6 months | 1, 3, 6, 12, 18, 24 | Low | Kenya | 2002-2005 |
| Gray et al 2007 (12) | 4,996 | Consistent/ Inconsistent/ No condom use | 6, 12, 24 | Low | Uganda | 2004-2006 | |
| Cohort | Westercamp et al 2014 (14) | 3, 186 | Condom use at the last time of sex | 6, 12, 18, 24 | Low | Kenya | 2008-2010 |
| Agot et al 2007 (13) | 648 | Consistent/inconsistent/No condom use | Between 4-6 Between 9-12 |
Low | Kenya | 2002-2004 | |
| Kagaayi et al 2016 (16) | 4,907 | Condom use at last non-marital sex | Between 15-21 | Low | Uganda | 2008-2011 |
3. RESULTS
Out of the 14 potentially eligible studies that were identified from systematic literature search, 5 studies were included in this review (Figure 1). Of the excluded studies, four studies (11, 18-20) had insufficient or unclear assessment of condom use behavior, three studies (21-23) were excluded because they were longitudinal studies embedded in studies already included in the review and one observational cohort study (24) was excluded because it was conducted between 1993 and 1997 where knowledge about the protective effect of male circumcision may not have been present. To avoid any doubts concerning the lack of knowledge of the protective effect of circumcision among study participants, this study was excluded from the meta-analyses.
Figure 1. Flow chart of literature research.
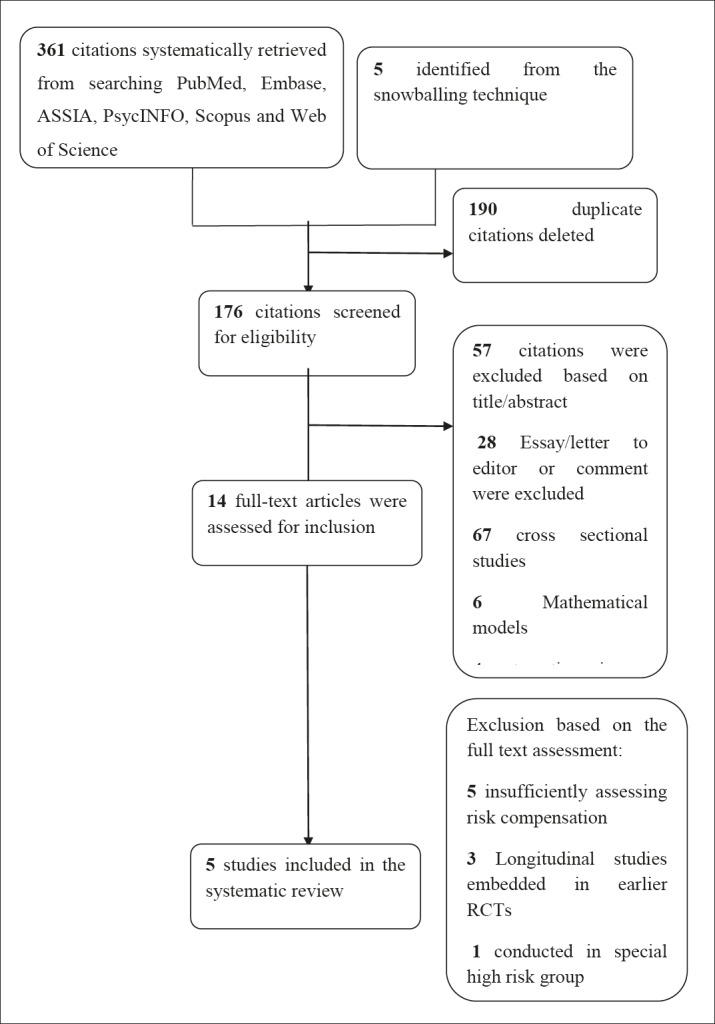
Figure 2c. Circumcision and condom use, 24 months follow up.
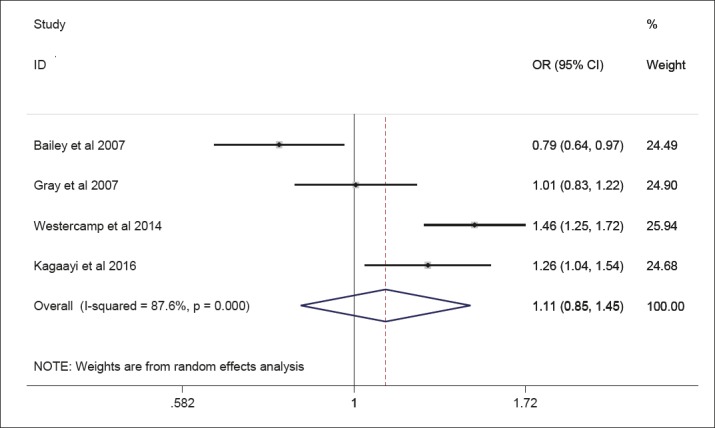
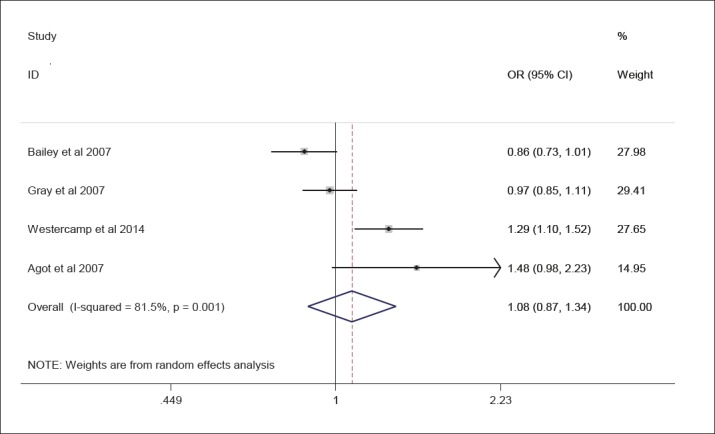
For studies corresponding to the 6 months follow-up period, the pooled Odds ratio was 0.91 (95% CI (0.57-1.45)). Among the 4 studies in the 6 months follow-up period (Figure 2a), one of these studies (14) showed statistical significance for lower odds of condom use among circumcised men (OR=0.51, 95% CI (0.43–0.60)), while another (12) showed statistical significance for higher odds of condom use among circumcised men (OR=1.36, 95% CI (1.19–1.55)) in spite of the pooled effect not being statistically significant. A pooled Odds ratio of 1.08 (95% CI (0.87-1.34)) was obtained for studies that assessed condom use related behavior at 12 months follow-up (Figure 2b). One study (14) among the 4 studies in the 12 months follow-up period showed significant results for higher odds of condom use among circumcised men (OR=1.29, 95% CI (1.10–1.52)) although the overall pooled effect was not significant. In a similar pattern, the results from the meta-analysis corresponding to 24 months follow-up period generated a pooled Odds ratio of 1.11 95% CI (0.85–1.45). The results from the sensitivity analysis were much similar to those obtained from the main study analyses at 6 months follow-up (OR=0.87, 95% CI: 0.55, 1.37), 12 months follow-up (OR=1.04, 95% CI: 0.84, 1.29) and 24 months follow-up (OR=1.03 (0.84, 1.26, 95% CI: 0.84, 1.26). ur assessment of the risk of bias across the studies revealed that there was low risk of bias. The studies included in this review had two potential sources of bias. The first is that it is unclear how long is long enough for the accurate assessment of condom use related behavioral changes after circumcision. Secondly the major outcome (condom use) was self-reported. The overall interpretation of the risk of bias is that there might be some plausible bias within the studies but this is unlikely to seriously alter the findings from the studies.
Figure 2. Three forest plots of studies assessing effect of circumcision status on reported condom use.
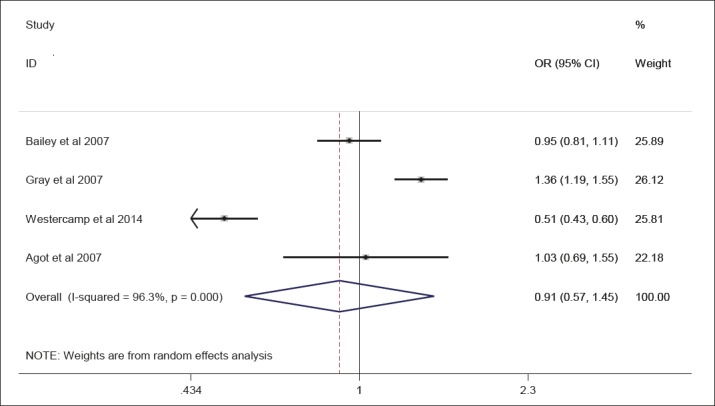
Figure 2b. Circumcision and condom use, 12 month follow up.
4. DISCUSSION
The meta analysis shows that the odds of condom use among circumcised men compared to uncircumcised men at 6, 12 and 24 months follow up were 0.91 (95% CI: 0.57–1.45), 1.08 (95% CI: 0.87–1.34) and 1.11 (95% CI: 0.85, 1.45) respectively. This overall finding implies that there is no significant association between circumcision and condom use behavior among males. Risk compensation is behavioral change that occurs as a result of someone having knowledge which leads to a perception of reduced vulnerability to a disease (7, 8). Particularly for the first RCTs establishing the beneficial effect of male circumcision it is safe to assume that the participants knew about or at least presumed the beneficial effect of their circumcision, because the ethical conduct of research mandates that participants are informed about the study, its potential benefits and harms. To our knowledge there are two intervention studies available, showing increases in risky behaviors such as unprotected sex and number of sexual partners in circumcised men (2, 3). One of them (3) is considered in our meta-analysis. The other RCT had already shown a slightly increased number of sexual contacts among both circumcised and uncircumcised men at baseline, but no difference in condom use (2). Sexual contacts decreased over time compared to baseline and it was always a bit higher among the circumcised as compared to uncircumcised men. However, considering the increased risky sexual behavior of the intervention group before circumcision, this small difference between both groups should be interpreted with caution. Unfortunately, condom use behavior was not followed up over time, and therefore this study (2) could not be considered in the meta-analysis. Additionally, one would expect that risk compensation will be more present, as people are more aware of the benefits of circumcision (25). However, the prospective cohort study that began in 2008 after the first major published RCTs (3, 4), also found no evidence of risk compensation among circumcised men (14). Overall, the results of this meta-analysis support the scale up of medical male circumcision as an HIV prevention intervention as it does not affect existing HIV preventive methods such as condom use.
In spite of the results being statistically insignificant, with in the 6 months follow-up category, two (4, 14) of the 4 studies in the meta-analysis (one of which had statistically significant results) showed lower odds of condom use among circumcised males. Thus, there might be a tendency for newly circumcised participants to engage less in protected sex as compared to their uncircumcised counterparts. One of the possible reasons for this observation at 6 months follow up could be that newly circumcised men will generally engage less in sexual activity due to the healing period following circumcision (13). However after the healing period, circumcised men may engage in risky sexual activities due to the urge to experiment sexual performance after removal of the penile foreskin (13). However, with the pooled OR not being statistically significant, the argument that circumcised men might use condoms less remains, but an assertion.
In the meta-analysis of studies corresponding to longer follow-up periods (i.e. 12 months and 24 or more months); even though the pooled result is not statistically significant, it appears that the lower odds of condom use or the possibility of risky behavior in relation to condom use becomes less apparent compared to the 6 months follow-up period. The odds ratio approaches and crosses over the null at 12 months (OR=1.08 CI: 0.87-1.34), and persists at longer periods of follow up i.e. 1.11 (95% CI: 0.85-1.45). This implies that circumcised and uncircumcised males may not differ in their condom use behavior. In fact, a qualitative study (26) showed that circumcised men are more likely to maintain or improve their condom use behavior after the procedure. Another study (27) done to compare the sexual behaviors of circumcised to uncircumcised men found that although circumcised men were more likely to exhibit risky sexual behavior such as combining drinking alcohol with extra marital sex, they were no more likely to use condoms compared to their uncircumcised counterparts. The first limitation of the review is that while generating our main outcome variable of reported condom use during any sexual activity for the meta-analyses, we merged the group of males that reported consistent condom use with those that reported inconsistent condom use. Additionally, the other 2 binary outcomes that formed this main outcome variable were also quite dissimilar i.e. condom use at last sex and unprotected intercourse in the last six months. This implies that the condom use outcome does not exactly represent sustained condom use practices during the follow-up periods. This also implies that there is a possibility that condom use among males might have been under assessed. These two sources of bias could drive the odds ratio either to or away from the null, which is why in the sensitivity analysis we left out the category of inconsistent condom use. We did not find any major differences between results from our sensitivity analysis and those from main study analyses thus implying that the possibility of under assessment is less likely.
In addition, given that condom use is self-reported, there is a possibility of social desirability bias. It is a bias in reported assessments where respondents answer questions in a way that puts them in a favorable light as a result of ego-defensive or impression management reasons (28). It is difficult to ascertain whether those who reported consistent use of condoms actually used them consistently. However, the review drew consistent evidence from RCT and cohort studies and thus it is unlikely that this bias gravely affected the results of this study.
5. CONCLUSIONS
This review has revealed that, circumcision is not associated with changes in condom use behavior up to 24 months after circumcision took place. However, apart from the randomized control trials that established the biological protective effect of male circumcision, only one longitudinal study has been published reporting the same results. Future research would benefit from investigating the long term benefits and/ or shortcomings of circumcision besides the biological protection that it confers. The review also established that condom use was inconsistently assessed among the studies. Future research should focus on developing a standardized tool for assessing condom use as this could improve comparability as well as the assessment of the success of HIV preventive efforts.
Author contributions:
SNK suggested the research question for the article and developed together with GBB and DS the idea to do a meta-analysis. Literature search was done by SNK and DS. SNK prepared the first draft of the manuscript which was finalized jointly by all authors. SNK is the guarantor of the work.
Conflict of interest:
the authors declare no conflict of interest.
REFERENCES
- 1.Templeton DJ. Male circumcision to reduce sexual transmission of HIV. Curr Opin in HIV and AIDS. 2010;5(4):344–9. doi: 10.1097/COH.0b013e32833a46d3. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO; 2007. New data on male circumcision and HIV prevention: policy and programme implications. [Google Scholar]
- 3.Mwandi Z, Murphy A, Reed J, Chesang K, Njeuhmeli E, Agot K, et al. Voluntary medical male circumcision: translating research into the rapid expansion of services in Kenya, 2008–2011. PLoS Med. 2011;8(11):e1001130. doi: 10.1371/journal.pmed.1001130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369(9562):643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 5.Kalichman S, Eaton L, Pinkerton S. Circumcision for HIV prevention: Failure to fully account for behavioral risk compensation [4] PLoS Med. 2007;4(3):597–8. doi: 10.1371/journal.pmed.0040138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pinkerton SD. Sexual risk compensation and HIV/STD transmission: empirical evidence and theoretical considerations. Risk Anal. 2001;21(4):727–36. doi: 10.1111/0272-4332.214146. [DOI] [PubMed] [Google Scholar]
- 7.Westercamp M, Agot KE, Ndinya-Achola J, Bailey RC. Circumcision preference among women and uncircumcised men prior to scale-up of male circumcision for HIV prevention in Kisumu, Kenya. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV. 2012;24(2):157–66. doi: 10.1080/09540121.2011.597944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eaton L, Cain D, Agrawal A, Jooste S, Udemans N, Kalichman S. The influence of male circumcision for HIV prevention on sexual behaviour among traditionally circumcised men in Cape Town, South Africa. Int J STD AIDS. 2011;22(11):674–9. doi: 10.1258/ijsa.2011.011006. [DOI] [PubMed] [Google Scholar]
- 9.Maughan-Brown B, Venkataramani AS. Learning That Circumcision Is Protective against HIV: Risk Compensation among Men and Women in Cape Town, South Africa. PLos One. 2012;7(7) doi: 10.1371/journal.pone.0040753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamali A, Carpenter LM, Whitworth JAG, Pool R, Ruberantwari A, Ojwiya A. Seven-year trends in HIV-1 infection rates, and changes in sexual behaviour, among adults in rural Uganda. AIDS. 2000;14(4):427–34. doi: 10.1097/00002030-200003100-00017. [DOI] [PubMed] [Google Scholar]
- 11.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2(11):e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369(9562):657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 13.Agot KE, Kiarie JN, Nguyen HQ, Odhiambo JO, Onyango TM, Weiss NS. Male circumcision in Siaya and Bondo Districts, Kenya: prospective cohort study to assess behavioral disinhibition following circumcision. J AIDS. 2007;44(1):66–70. doi: 10.1097/01.qai.0000242455.05274.20. [DOI] [PubMed] [Google Scholar]
- 14.Westercamp N, Agot K, Jaoko W, Bailey RC. Risk compensation following male circumcision: results from a two-year prospective cohort study of recently circumcised and uncircumcised men in Nyanza Province, Kenya. AIDS Behav. 2014;18(9):1764–75. doi: 10.1007/s10461-014-0846-4. [DOI] [PubMed] [Google Scholar]
- 15.StataCorp. College Station, TX: StataCorp LP; 2013. Stata Statistical Software: Release 13. [Google Scholar]
- 16.Kagaayi J, Kong X, Kigozi G, Ssekubugu R, Kigozi G, Nalugoda F, et al. Self-selection of male circumcision clients and behaviors following circumcision in a service program in Uganda. AIDS. 2016;30(13):2125–9. doi: 10.1097/QAD.0000000000001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions Version 5.1. 0 [updated March 2011] The Cochrane Collaboration, 2011. 2012. www.cochrane-handbook.org.
- 18.Reynolds SJ, Shepherd ME, Risbud AR, Gangakhedkar RR, Brookmeyer RS, Divekar AD, et al. Male circumcision and risk of HIV-1 and other sexually transmitted infections in India. Lancet. 2004;363(9414):1039–40. doi: 10.1016/S0140-6736(04)15840-6. [DOI] [PubMed] [Google Scholar]
- 19.Wilson NL, Xiong W, Mattson CL. Is sex like driving? HIV prevention and risk compensation. J Dev Econ. 2014;106:78–91. doi: 10.1016/j.jdeveco.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Govender K, George G, Beckett S, Montague C, Frohlich J. Risk Compensation Following Medical Male Circumcision: Results from a 1-Year Prospective Cohort Study of Young School-Going Men in KwaZulu-Natal, South Africa. Int J Behav Med. 2017. pp. 1–8. [DOI] [PubMed]
- 21.Mattson CL, Campbell RT, Bailey RC, Agot K, Ndinya-Achola JO, Moses S. Risk Compensation Is Not Associated with Male Circumcision in Kisumu, Kenya: A Multi-Faceted Assessment of Men Enrolled in a Randomized Controlled Trial. PLos One. 2008;3(6) doi: 10.1371/journal.pone.0002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gray R, Kigozi G, Kong XR, Ssempiija V, Makumbi F, Wattya S, et al. The effectiveness of male circumcision for HIV prevention and effects on risk behaviors in a posttrial follow-up study. AIDS. 2012;26(5):609–15. doi: 10.1097/QAD.0b013e3283504a3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kong XR, Kigozi G, Nalugoda F, Musoke R, Kagaayi J, Latkin C, et al. Assessment of Changes in Risk Behaviors During 3 Years of Posttrial Followup of Male Circumcision Trial Participants Uncircumcised at Trial Closure in Rakai, Uganda. Am J Epidemiol. 2012;176(10):875–85. doi: 10.1093/aje/kws179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lavreys L, Rakwar JP, Thompson ML, Jackson DJ, Mandaliya K, Chohan BH, et al. Effect of circumcision on incidence of human immunodeficiency virus type 1 and other sexually transmitted diseases: a prospective cohort study of trucking company employees in Kenya. J Infect Dis. 1999;180(2):330–6. doi: 10.1086/314884. [DOI] [PubMed] [Google Scholar]
- 25.Kong X, Ssekasanvu J, Kigozi G, Lutalo T, Nalugoda F, Serwadda D, et al. Male circumcision coverage, knowledge, and attitudes after 4-years of program scale-up in Rakai, Uganda. AIDS Behav. 2014;18(5):880–4. doi: 10.1007/s10461-014-0740-0. [DOI] [PubMed] [Google Scholar]
- 26.Riess TH, Achieng MM, Otieno S, Ndinya-Achola J, Bailey RC. “When I was circumcised I was taught certain things”: risk compensation and protective sexual behavior among circumcised men in Kisumu, Kenya. PLoS One. 2010;5(8):e12366. doi: 10.1371/journal.pone.0012366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bailey RC, Neema S, Othieno R. Sexual behaviors and other HIV risk factors in circumcised and uncircumcised men in Uganda. J AIDS J. 1999;22(3):294–301. doi: 10.1097/00126334-199911010-00012. [DOI] [PubMed] [Google Scholar]
- 28.Fisher RJ. Social desirability bias and the validity of indirect questioning. Journal of Consum Res. 1993. pp. 303–15.


