Abstract
Problem/Condition
Doctor-diagnosed arthritis is a common chronic condition affecting an estimated 23% (54 million) of adults in the United States, greatly influencing quality of life and costing approximately $300 billion annually. The geographic variations in arthritis prevalence, health-related characteristics, and management among states and territories are unknown. Therefore, public health professionals need to understand arthritis in their areas to target dissemination of evidence-based interventions that reduce arthritis morbidity.
Reporting Period
2015.
Description of System
The Behavioral Risk Factor Surveillance System is an annual, random-digit–dialed landline and cellular telephone survey of noninstitutionalized adults aged ≥18 years residing in the United States. Self-reported data are collected from the 50 states, the District of Columbia, Guam, and Puerto Rico. Unadjusted and age-standardized prevalences of arthritis, arthritis health-related characteristics, and arthritis management were calculated. County-level estimates were calculated using a validated statistical modeling method.
Results
In 2015, in the 50 states and the District of Columbia, median age-standardized prevalence of arthritis was 23.0% (range: 17.2%–33.6%). Modeled prevalence of arthritis varied considerably by county (range: 11.2%–42.7%). In 13 states that administered the arthritis management module, among adults with arthritis, the age-standardized median percentage of participation in a self-management education course was 14.5% (range: 9.1%–19.0%), being told by a health care provider to engage in physical activity or exercise was 58.5% (range: 52.3%–61.9%), and being told to lose weight to manage arthritis symptoms (if overweight or obese) was 44.5% (range: 35.1%–53.2%). Respondents with arthritis who lived in the quartile of states with the highest prevalences of arthritis had the highest percentages of negative health-related characteristics (i.e., arthritis-attributable activity limitations, arthritis-attributable severe joint pain, and arthritis-attributable social participation restriction; ≥14 physically unhealthy days during the past 30 days; ≥14 mentally unhealthy days during the past 30 days; obesity; and leisure-time physical inactivity) and the lowest percentage of leisure-time walking.
Interpretation
The prevalence, health-related characteristics, and management of arthritis varied substantially across states. The modeled prevalence of arthritis varied considerably by county.
Public Health Action
The findings highlight notable geographic variability in prevalence, health-related characteristics, and management of arthritis. Targeted use of evidence-based interventions that focus on physical activity and self-management education can reduce pain and improve function and quality of life for adults with arthritis and thus might reduce these geographic disparities.
Introduction
Doctor-diagnosed arthritis is a common chronic condition that affected an estimated 23% (54 million) of adults in the United States during 2013–2015 (1). Prevalence varies across states (2), counties (2), urban and rural communities (3), and census tracts within the largest U.S. cities (https://www.cdc.gov/500cities). The condition limits activities of 24 million adults (1), is associated with severe joint pain among 15 million adults (4), and is projected to affect 78.4 million adults by 2040 (5). In 2013, total national medical care expenditures and earnings losses attributable to arthritis were $303.5 billion (6). Public health measures focus on increasing physical activity, increasing self-management education, increasing health care provider counseling for physical activity or exercise, and encouraging walking.
Since 2003, CDC has conducted surveillance for arthritis using Behavioral Risk Factor Surveillance System (BRFSS) data (7). The findings in this report can be used by public health professionals to better understand geographic variability in prevalence, health-related characteristics, and management of arthritis between states and territories. Public health professionals can also target evidence-based nonpharmaceutical interventions, such as arthritis self-management education and physical activity, to help decrease the impact of arthritis and perhaps reduce geographic disparities in arthritis health-related characteristics and management.
Methods
To characterize self-reported doctor-diagnosed arthritis in the United States, Guam, and Puerto Rico, CDC analyzed data from the 2015 BRFSS (Box). First, selected area-level prevalences were estimated, including prevalences of arthritis among adults aged ≥18 years with selected comorbid conditions (i.e., coronary heart disease, diabetes, and obesity). Percentages of health-related characteristics among adults with arthritis (i.e., general health, leisure-time physical activity, activity limitations, and pain) also were estimated. Second, for 13 states with available data, self-management measures for adults with arthritis were examined. Third, to examine possible clustering of arthritis health-related characteristics linear trends were tested between increasing prevalence of arthritis and increasing percentages of negative health-related characteristics among adults with arthritis at the state level. Detailed arthritis surveillance estimates for states, the District of Columbia, Guam, and Puerto Rico are available online for 2011, 2013, and 2015 (https://www.cdc.gov/arthritis/data_statistics/state-data-list-current.htm), but are unpublished elsewhere.
BOX. Understanding geographic variations in arthritis prevalence, health-related characteristics, and management.
Aim 1: Estimate prevalence among adults
Prevalence of arthritis among adults with comorbid conditions (coronary heart disease, diabetes, and obesity)
Prevalence of obesity among adults with arthritis
Prevalence of leisure-time walking among adults with arthritis
Prevalence of physical inactivity among adults with arthritis
Prevalence of two types of negative health-related characteristics among adults with arthritis: general health (physically and mentally unhealthy days) and arthritis-attributable impact (activity limitations, severe joint pain, and social participation restriction)
Aim 2: Estimate management among adults with arthritis
Prevalence of participation in arthritis self-management education course
Prevalence of health care provider counseling for weight loss
Prevalence of health care provider counseling for physical activity or exercise
Aim 3: Examine possible state-specific clustering of health-related characteristics among adults with arthritis
Data Source and Measurements
BRFSS is an annual, random-digit–dialed landline and cellular telephone survey of the noninstitutionalized U.S. adult population aged ≥18 years. Self-reported data are collected from the 50 states, the District of Columbia, Guam, and Puerto Rico. In 2015, a total of 441,456 interviews were completed and analyzed for this report. Response rates ranged from 33.9% to 61.1% (median: 47.2%). The response rate was the number of respondents who completed the survey as a proportion of all eligible and likely eligible persons. Response rates for BRFSS were calculated using standards set by American Association for Public Opinion Research response rate formula no. 4. Additional information is available at https://www.cdc.gov/brfss/annual_data/2015/2015_responserates.html.
Respondents were classified as having doctor-diagnosed arthritis (hereafter referred to as arthritis) if they answered yes to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?” Three comorbid conditions were examined: obesity, diabetes, and coronary heart disease. Body mass index (BMI) was computed from self-reported height and weight. Obesity was categorized as BMI ≥30 kg/m2. Doctor-diagnosed diabetes (hereafter referred to as diabetes) was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have diabetes?” Those with prediabetes or borderline diabetes and women who had diabetes only during pregnancy were classified as not having diabetes. Doctor-diagnosed coronary heart disease (hereafter referred to as coronary heart disease) was defined as a yes response to either of the following two questions: 1) “Has a doctor, nurse, or other health professional ever told you that you had a heart attack, also called a myocardial infarction?” or 2) “Has a doctor, nurse, or other health professional ever told you that you had angina or coronary heart disease?”
Prevalence of Arthritis
The prevalence of arthritis was estimated among all adults. Prevalence was estimated separately for adults with comorbid conditions (i.e., obesity, coronary heart disease, and diabetes).
Health-Related Characteristics
General Health. Two measures of health-related quality of life were examined. For physically and mentally unhealthy days, respondents reported the number of days during the past 30 days that their physical or mental health, or both, was not good. For each measure, a standard predetermined cutoff point of ≥14 days during the past 30 days was used to identify respondents with poor physical or mental health, respectively (8).
Leisure-Time Physical Activity and Obesity. Among adults with arthritis, the prevalences of obesity, leisure-time physical inactivity, and leisure-time walking were estimated. Leisure-time physical inactivity was defined as a no response to the question “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Among those who answered yes, leisure-time walking was ascertained via two questions: 1) “What type of physical activity or exercise did you spend the most time doing during the past month?” and 2) “What other type of physical activity gave you the next most exercise during the past month?” For the leisure-time walking measure, the numerator was adults with arthritis who listed walking as one of their top two activities and the denominator included both active and inactive adults with arthritis.
Activity Limitations. Among adults with arthritis, arthritis-attributable activity limitations were identified by a yes response to the question “Are you now limited in any way in any of your usual activities because of arthritis or joint symptoms?” Arthritis-attributable social participation restriction was defined as a response of a lot to the question “During the past 30 days, to what extent has your arthritis or joint symptoms interfered with your normal social activities, such as going shopping, to the movies, or to religious or social gatherings?”
Pain. Arthritis-attributable severe joint pain was defined according to an a priori criterion (9) as a pain level of 7–10 on a scale of 0–10 where 0 is no pain and 10 is pain or aching as bad as it can be for the question “Please think about the past 30 days, keeping in mind all of your joint pain or aching and whether or not you have taken medication. During the past 30 days, how bad was your joint pain on average?”
Arthritis Management
In 2015, a total of 13 states (California, Kansas, Kentucky, Michigan, Minnesota, Missouri, Montana, New York, Oregon, Pennsylvania, Rhode Island, South Carolina, and Utah) administered the BRFSS arthritis management module to respondents with arthritis and ascertained participation in self-management education courses and receipt of health care provider counseling. Among adults with arthritis, attendance at a self-management education course was defined as a yes response to the question “Have you ever taken an educational course or class to teach you how to manage problems related to your arthritis or joint symptoms?” Among those who were overweight (BMI 25 to <30 kg/m2) or obese (BMI ≥30 kg/m2), health care provider counseling for weight loss was defined as a yes response to the question “Has a doctor or other health professional ever suggested losing weight to help your arthritis or joint symptoms?” Health care provider counseling for physical activity or exercise was defined as a yes response to the question “Has a doctor or other health professional ever suggested physical activity or exercise to help your arthritis or joint symptoms?”
Analyses
Direct Estimates
All directly estimated analyses included adjustment for the complex survey design; sampling weights accounted for nonresponse, noncoverage, and cellular-telephone–only households and were derived from an iterative proportional weighting (raking) procedure (https://www.cdc.gov/brfss/annual_data/2015/pdf/weighting_the-data_webpage_content.pdf). Estimates were age standardized to the 2000 U.S. projected population using three age groups (18–44, 45–64, and ≥65 years) (10). Weighted unadjusted and age-standardized prevalences with 95% confidence intervals were estimated for arthritis and arthritis-related characteristics. For each characteristic, the median and range were calculated using prevalence estimates for the 50 states and the District of Columbia (not including Guam and Puerto Rico). The unadjusted prevalence is an estimate of the actual prevalence of a characteristic in a specific area. Age-standardized prevalence estimates are provided to permit comparisons across states. Prevalence estimates of arthritis and percentages of selected characteristics among adults with arthritis that had a relative standard error (RSE) ≥30% or unweighted sample size of <50 did not meet the minimum criteria for precision and were suppressed.
Indirect (Modeled) County-Level Arthritis Prevalence Estimates
Prevalence of arthritis at the county level was estimated with a multilevel regression model and poststratification approach (11) for counties (N = 3,142) in all 50 states and the District of Columbia. The multilevel regression model included individual-level data on age group (13 categories), sex, and race/ethnicity from the 2015 BRFSS; county-level poverty data (percentage below 150% of the federal poverty level) from the American Community Survey 5-year estimates (2011–2015) (12); and random effects at county and state levels. Parameter estimates from the models were applied to Census Vintage 2015 county population estimates to generate county-level estimates of arthritis prevalence. These modeled prevalence estimates were reported in quartiles for the 3,142 counties. High internal validity was established by comparing modeled county-level estimates of arthritis with actual unweighted BRFSS survey estimates in 1,531 counties with ≥50 respondents and RSE <30% (Pearson correlation coefficient: 0.78; p<0.001) and with weighted BRFSS estimates in 205 counties with ≥500 respondents (Pearson correlation coefficient: 0.94; p<0.001).
State-Specific Clustering of Health-Related Characteristics
States and the District of Columbia were divided into quartiles (lowest to highest) according to age-adjusted state-level prevalence of arthritis in 2015. Age-standardized percentages of seven negative health-related characteristics among adults with arthritis (i.e., arthritis-attributable activity limitations, arthritis-attributable severe joint pain, and arthritis-attributable social participation restriction; ≥14 physically unhealthy days; ≥14 mentally unhealthy days; obesity; and leisure-time physical inactivity) and leisure-time walking were calculated for respondents by quartile of arthritis prevalence. A test of trend using orthogonal polynomial contrasts (by partitioning the sums of squares) was performed to determine whether the age-standardized prevalence of negative health-related characteristics increased and leisure-time walking decreased among adults with arthritis living in states with greater age-standardized prevalence of arthritis. To improve data fit and accommodate nonlinear trends, the test for trend included a quadratic term. For each health-related characteristic, a statistically significant trend in age-standardized percentage across arthritis quartiles was determined at the Bonferroni-corrected alpha level of 0.006 (α = 0.05/8) to adjust for testing multiple characteristics.
Results
Arthritis Prevalence
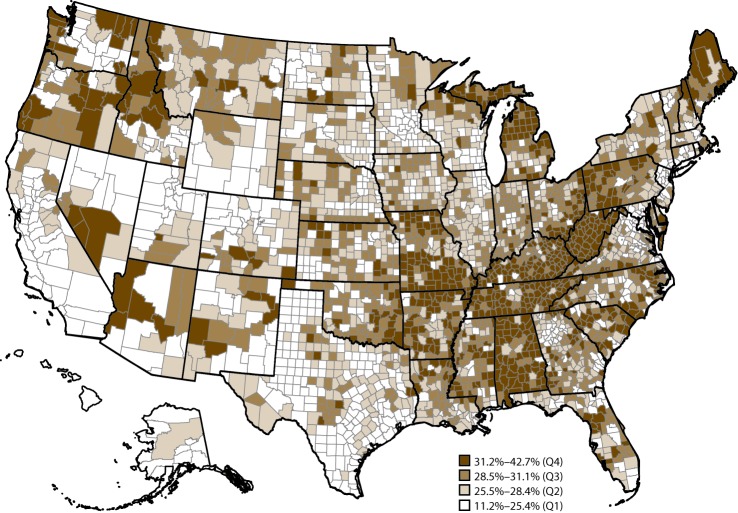
In 2015, for the 50 states and the District of Columbia, age-standardized median prevalence of arthritis was 23.0% (range: 17.2% in Hawaii to 33.6% in West Virginia) (Table 1). The model-based prevalence estimates of arthritis across the 3,142 U.S. counties in 50 states and the District of Columbia ranged from 11.2% to 42.7% (Figure 1). At the county level, counties in Appalachia and along the lower Mississippi River tended to have higher predicted prevalences of arthritis. The majority of counties in Alabama, Arkansas, Kentucky, Michigan, Missouri, Tennessee, and West Virginia were in the highest quartile (31.2%–42.7%).
TABLE 1. Prevalence of arthritis,* by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | No. of respondents | No. of respondents with arthritis | Weighted population with arthritis (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized %† (95% CI) |
|---|---|---|---|---|---|
| Alabama |
7,950 |
3,307 |
1,248,000 |
33.3 (31.9–34.6) |
30.4 (29.2–31.7) |
| Alaska |
3,657 |
1,028 |
117,000 |
21.2 (19.3–23.2) |
21.5 (19.7–23.3) |
| Arizona |
7,946 |
2,663 |
1,222,000 |
23.6 (22.5–24.8) |
21.8 (20.7–22.9) |
| Arkansas |
5,256 |
2,228 |
672,000 |
29.7 (27.8–31.7) |
27.1 (25.4–28.9) |
| California |
12,601 |
2,803 |
5,719,000 |
19.1 (18.3–20.0) |
18.3 (17.6–19.1) |
| Colorado |
13,537 |
4,136 |
949,000 |
22.7 (21.8–23.7) |
21.8 (20.9–22.7) |
| Connecticut |
11,899 |
3,962 |
690,000 |
24.5 (23.5–25.5) |
21.6 (20.8–22.5) |
| Delaware |
4,070 |
1,471 |
207,000 |
28.1 (26.3–29.9) |
24.6 (23.1–26.2) |
| District of Columbia |
3,994 |
1,316 |
101,000 |
18.5 (16.7–20.4) |
19.9 (18.3–21.7) |
| Florida |
9,739 |
3,454 |
4,154,000 |
25.9 (24.8–27.0) |
21.5 (20.6–22.5) |
| Georgia |
4,678 |
1,660 |
1,890,000 |
24.6 (23.1–26.1) |
23.6 (22.3–24.9) |
| Hawaii |
7,163 |
1,757 |
211,000 |
18.9 (17.8–20.1) |
17.2 (16.2–18.3) |
| Idaho |
5,802 |
2,031 |
309,000 |
25.3 (23.8–26.8) |
23.2 (22.0–24.5) |
| Illinois |
5,289 |
1,671 |
2,308,000 |
23.3 (22.0–24.7) |
21.6 (20.4–22.7) |
| Indiana |
6,067 |
2,273 |
1,390,000 |
27.6 (26.1–29.1) |
25.4 (24.1–26.7) |
| Iowa |
6,227 |
2,145 |
619,000 |
25.9 (24.6–27.2) |
23.2 (22.1–24.4) |
| Kansas |
23,236 |
7,320 |
536,000 |
24.5 (23.9–25.2) |
22.7 (22.2–23.3) |
| Kentucky |
8,806 |
3,565 |
1,087,000 |
32.0 (30.5–33.5) |
29.3 (27.9–30.8) |
| Louisiana |
4,716 |
1,748 |
989,000 |
27.9 (26.4–29.5) |
26.2 (24.8–27.7) |
| Maine |
9,063 |
3,459 |
332,000 |
31.0 (29.7–32.3) |
26.4 (25.2–27.6) |
| Maryland |
12,598 |
4,631 |
1,096,000 |
23.5 (22.2–24.9) |
21.5 (20.4–22.8) |
| Massachusetts |
9,294 |
2,842 |
1,300,000 |
24.1 (23.0–25.3) |
22.0 (21.0–23.0) |
| Michigan |
8,935 |
3,224 |
2,305,000 |
30.0 (28.9–31.1) |
27.0 (26.0–28.0) |
| Minnesota |
16,761 |
4,666 |
907,000 |
21.6 (20.9–22.3) |
19.7 (19.1–20.4) |
| Mississippi |
6,035 |
2,431 |
647,000 |
28.6 (27.1–30.1) |
26.6 (25.3–28.0) |
| Missouri |
7,307 |
2,808 |
1,372,000 |
29.3 (27.9–30.8) |
26.8 (25.5–28.2) |
| Montana |
6,051 |
2,123 |
216,000 |
26.8 (25.4–28.3) |
23.9 (22.5–25.4) |
| Nebraska |
17,561 |
5,522 |
334,000 |
23.4 (22.6–24.3) |
21.5 (20.7–22.3) |
| Nevada |
2,926 |
918 |
477,000 |
21.5 (19.5–23.8) |
20.1 (18.2–22.2) |
| New Hampshire |
7,022 |
2,588 |
282,000 |
26.6 (25.3–27.9) |
23.0 (21.9–24.2) |
| New Jersey |
11,465 |
3,442 |
1,590,000 |
22.9 (21.8–24.1) |
20.5 (19.5–21.5) |
| New Mexico |
6,734 |
2,248 |
386,000 |
24.5 (23.1–25.9) |
22.2 (21.0–23.5) |
| New York |
12,357 |
3,921 |
3,629,000 |
23.4 (22.5–24.3) |
21.5 (20.6–22.3) |
| North Carolina |
6,698 |
2,144 |
2,089,000 |
26.9 (25.7–28.2) |
24.9 (23.8–26.0) |
| North Dakota |
4,972 |
1,585 |
134,000 |
22.9 (21.5–24.3) |
21.6 (20.4–22.9) |
| Ohio |
11,929 |
4,730 |
2,547,000 |
28.4 (27.2–29.7) |
25.3 (24.2–26.4) |
| Oklahoma |
6,943 |
2,692 |
813,000 |
27.7 (26.3–29.1) |
25.7 (24.5–27.0) |
| Oregon |
5,359 |
1,828 |
838,000 |
26.8 (25.4–28.2) |
24.5 (23.2–25.8) |
| Pennsylvania |
5,740 |
2,059 |
2,937,000 |
29.2 (27.8–30.7) |
25.7 (24.4–27.0) |
| Rhode Island |
6,206 |
2,244 |
226,000 |
26.9 (25.5–28.4) |
24.2 (22.9–25.6) |
| South Carolina |
11,607 |
4,405 |
1,105,000 |
29.1 (28.1–30.2) |
26.3 (25.3–27.2) |
| South Dakota |
7,221 |
2,389 |
158,000 |
24.3 (22.8–25.9) |
21.8 (20.5–23.2) |
| Tennessee |
5,979 |
2,466 |
1,630,000 |
32.0 (30.3–33.7) |
29.4 (27.9–31.1) |
| Texas |
14,697 |
4,522 |
4,055,000 |
20.0 (19.0–21.1) |
19.8 (18.9–20.8) |
| Utah |
11,401 |
2,929 |
407,000 |
19.6 (18.8–20.4) |
20.8 (20.1–21.6) |
| Vermont |
6,489 |
2,089 |
136,000 |
27.0 (25.7–28.3) |
23.4 (22.3–24.6) |
| Virginia |
8,646 |
2,684 |
1,513,000 |
23.2 (22.1–24.3) |
21.6 (20.6–22.6) |
| Washington |
16,116 |
5,481 |
1,346,000 |
24.5 (23.6–25.3) |
22.6 (21.9–23.4) |
| West Virginia |
5,957 |
2,537 |
557,000 |
38.0 (36.6–39.4) |
33.6 (32.3–34.9) |
| Wisconsin |
6,188 |
1,984 |
1,104,000 |
24.7 (23.3–26.2) |
22.1 (20.8–23.5) |
| Wyoming |
5,492 |
2,021 |
116,000 |
25.9 (24.2–27.5) |
24.1 (22.6–25.8) |
|
Median (Range)§
|
|
|
|
25.3 (18.5–38.0)
|
23.0 (17.2–33.6)
|
| Guam |
1,669 |
270 |
17,000 |
15.8 (13.5–18.4) |
17.9 (15.5–20.6) |
| Puerto Rico | 5,405 | 1,616 | 635,000 | 22.8 (21.5–24.0) | 20.6 (19.5–21.7) |
Abbreviation: CI = confidence interval.
* Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
† Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
§ Median and range were calculated from estimates for the 50 states and the District of Columbia.
FIGURE 1.
Model-based prevalence* of arthritis† among adults aged ≥18 years, by county — Behavioral Risk Factor Surveillance System, United States, 2015
Abbreviation: Q = quartile.
* Prevalence of arthritis at the county level was estimated with a multilevel regression model and poststratification approach for counties (N = 3,142) in all 50 states and the District of Columbia. Prevalence was based on the Behavioral Risk Factor Surveillance System definition of arthritis.
† Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
Arthritis Among Adults With Comorbid Conditions
For the 50 states and District of Columbia, the median age-standardized prevalence of arthritis among adults with obesity was 30.9% (range: 24.6% in Texas to 41.2% in West Virginia) (Table 2). The median age-standardized prevalence of arthritis among adults with coronary heart disease was 44.5% (range: 25.6% in the District of Columbia to 72.6% in Iowa) (Table 3). The median age-standardized prevalence of arthritis among adults with diabetes was 37.3% (range: 27.1% in California to 53.7% in Maine) (Table 4).
TABLE 2. Unadjusted* and age-standardized† prevalences of arthritis§ among adults ≥18 years with obesity,¶ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | No. of respondents with obesity | Weighted population with arthritis and obesity (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
2,626 | 512,000 |
41.4 (38.9–43.9) |
37.9 (35.7–40.2) |
| Alaska |
1,059 |
46,000 |
29.9 (26.1–34.0) |
28.5 (24.9–32.4) |
| Arizona |
1,892 |
398,000 |
30.0 (27.4–32.7) |
27.5 (25.3–29.7) |
| Arkansas |
1,593 |
275,000 |
37.7 (33.9–41.6) |
35.0 (31.5–38.7) |
| California |
2,808 |
1,749,000 |
26.4 (24.4–28.6) |
24.8 (23.1–26.6) |
| Colorado |
2,666 |
250,000 |
32.8 (30.3–35.4) |
29.4 (27.2–31.7) |
| Connecticut |
2,817 |
228,000 |
35.0 (32.7–37.4) |
29.9 (27.8–32.0) |
| Delaware |
1,145 |
70,000 |
35.6 (31.9–39.3) |
30.2 (27.3–33.4) |
| District of Columbia |
899 |
41,000 |
36.8 (31.2–42.8) |
31.6 (26.6–37.0) |
| Florida |
2,296 |
1,381,000 |
34.9 (32.4–37.6) |
28.3 (26.1–30.6) |
| Georgia |
1,340 |
759,000 |
35.4 (32.3–38.8) |
31.3 (28.7–34.0) |
| Hawaii |
1,509 |
67,000 |
27.6 (24.8–30.6) |
26.8 (24.0–29.8) |
| Idaho |
1,596 |
105,000 |
32.0 (29.0–35.1) |
29.0 (26.4–31.8) |
| Illinois |
1,547 |
946,000 |
32.4 (29.7–35.2) |
28.4 (26.1–30.9) |
| Indiana |
1,804 |
537,000 |
36.2 (33.2–39.4) |
32.4 (29.7–35.3) |
| Iowa |
1,805 |
241,000 |
34.4 (31.8–37.2) |
30.5 (28.1–33.0) |
| Kansas |
6,318 |
194,000 |
33.6 (32.2–34.9) |
30.1 (28.9–31.4) |
| Kentucky |
2,871 |
457,000 |
41.7 (38.8–44.7) |
38.0 (35.2–41.0) |
| Louisiana |
1,570 |
419,000 |
35.6 (32.6–38.7) |
33.3 (30.6–36.1) |
| Maine |
2,567 |
122,000 |
40.3 (37.8–43.0) |
34.9 (32.3–37.7) |
| Maryland |
3,437 |
448,000 |
36.9 (33.7–40.1) |
32.5 (29.5–35.7) |
| Massachusetts |
2,061 |
422,000 |
37.2 (34.4–40.2) |
31.5 (28.9–34.2) |
| Michigan |
2,582 |
875,000 |
39.3 (37.0–41.6) |
34.8 (32.7–36.9) |
| Minnesota |
4,213 |
321,000 |
32.0 (30.3–33.7) |
27.7 (26.0–29.5) |
| Mississippi |
1,964 |
260,000 |
34.4 (31.6–37.4) |
32.8 (30.4–35.4) |
| Missouri |
2,219 |
518,000 |
37.2 (34.5–40.0) |
33.7 (31.1–36.3) |
| Montana |
1,430 |
62,000 |
35.7 (32.3–39.1) |
30.4 (27.2–33.8) |
| Nebraska |
5,371 |
134,000 |
32.3 (30.5–34.2) |
28.4 (26.7–30.2) |
| Nevada |
700 |
155,000 |
28.6 (23.9–33.8) |
26.4 (21.9–31.6) |
| New Hampshire |
1,717 |
94,000 |
37.0 (34.1–40.0) |
31.4 (28.7–34.3) |
| New Jersey |
2,778 |
539,000 |
34.3 (31.6–37.0) |
29.2 (26.9–31.7) |
| New Mexico |
1,728 |
127,000 |
30.3 (27.3–33.4) |
29.3 (26.6–32.2) |
| New York |
2,933 |
1,221,000 |
34.6 (32.4–36.9) |
30.9 (28.8–33.2) |
| North Carolina |
1,808 |
780,000 |
37.2 (34.6–39.9) |
33.5 (31.1–36.0) |
| North Dakota |
1,477 |
51,000 |
30.7 (28.0–33.6) |
27.2 (24.8–29.6) |
| Ohio |
3,420 |
947,000 |
38.2 (35.7–40.8) |
32.6 (30.3–35.1) |
| Oklahoma |
2,126 |
329,000 |
35.5 (32.9–38.2) |
33.0 (30.6–35.4) |
| Oregon |
1401 |
302,000 |
35.3 (32.3–38.4) |
32.0 (29.2–34.9) |
| Pennsylvania |
5,740 |
1,114,000 |
39.6 (36.6–42.7) |
33.7 (30.9–36.6) |
| Rhode Island |
6,206 |
74,000 |
36.9 (33.6–40.3) |
31.8 (28.7–35.0) |
| South Carolina |
11,607 |
437,000 |
38.5 (36.3–40.7) |
34.9 (32.9–36.9) |
| South Dakota |
7,221 |
60,000 |
31.7 (28.6–35.0) |
28.3 (25.6–31.1) |
| Tennessee |
5,979 |
640,000 |
40.7 (37.4–44.1) |
37.6 (34.5–40.9) |
| Texas |
14,697 |
1,518,000 |
26.2 (24.0–28.4) |
24.6 (22.9–26.4) |
| Utah |
11,401 |
137,000 |
29.3 (27.3–31.4) |
28.0 (26.2–29.9) |
| Vermont |
6,489 |
43,000 |
37.1 (34.1–40.1) |
31.2 (28.4–34.2) |
| Virginia |
8,646 |
584,000 |
33.0 (30.5–35.5) |
29.6 (27.2–32.0) |
| Washington |
16,116 |
454,000 |
34.5 (32.6–36.5) |
29.8 (28.1–31.5) |
| West Virginia |
5,957 |
223,000 |
46.6 (44.1–49.2) |
41.2 (38.7–43.7) |
| Wisconsin |
6,188 |
417,000 |
32.6 (29.8–35.6) |
28.2 (25.6–31.1) |
| Wyoming |
5,492 |
41,000 |
34.1 (30.6–37.7) |
31.2 (28.1–34.5) |
|
Median (Range)**
|
|
|
35.0 (26.2–46.6)
|
30.9 (24.6–41.2)
|
| Guam |
1,669 |
7,000 |
20.3 (15.9–25.5) |
23.4 (19.0–28.5) |
| Puerto Rico | 5,405 | 215,000 | 27.5 (25.0–30.2) | 25.7 (23.4–28.2) |
Abbreviation: CI = confidence interval.
* The numerator was the estimated number of adults with arthritis and obesity (body mass index ≥30). The denominator was the estimated number of adults with obesity.
† Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Body mass index ≥30; calculated from self-reported height and weight.
** Median and range were calculated from estimates for the 50 states and the District of Columbia.
TABLE 3. Unadjusted* and age-standardized† prevalences of arthritis§ among adults aged ≥18 years with coronary heart disease,¶ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | No. of respondents with coronary heart disease | Weighted population with arthritis and coronary heart disease (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized %* (95% CI) |
|---|---|---|---|---|
| Alabama |
874 |
196,000 |
64.3 (59.7–68.7) |
57.0 (47.0–66.6) |
| Alaska |
223 |
12,000 |
49.1 (38.0–60.2) |
31.3 (21.8–42.6) |
| Arizona |
732 |
164,000 |
51.6 (46.1–57.1) |
36.9 (27.8–47.0) |
| Arkansas |
714 |
122,000 |
64.6 (58.5–70.3) |
57.8 (41.8–72.4) |
| California |
701 |
708,000 |
49.0 (43.8–54.2) |
38.1 (28.7–48.5) |
| Colorado |
857 |
99,000 |
53.4 (48.3–58.4) |
48.2 (35.9–60.7) |
| Connecticut |
945 |
80,000 |
52.1 (47.7–56.5) |
41.2 (30.8–52.4) |
| Delaware |
385 |
30,000 |
57.5 (49.5–65.1) |
44.4 (27.2–63.0) |
| District of Columbia |
286 |
11,000 |
45.9 (34.8–57.3) |
25.6 (20.0–32.3) |
| Florida |
1,031 |
667,000 |
56.2 (51.9–60.5) |
43.0 (31.8–54.9) |
| Georgia |
454 |
301,000 |
59.0 (52.6–65.0) |
48.3 (34.6–62.3) |
| Hawaii |
409 |
22,000 |
43.5 (36.7–50.5) |
39.1 (26.9–52.8) |
| Idaho |
469 |
37,000 |
53.8 (46.4–61.0) |
36.7 (27.2–47.5) |
| Illinois |
457 |
317,000 |
53.0 (47.0–58.9) |
39.1 (26.0–54.1) |
| Indiana |
672 |
239,000 |
60.9 (55.4–66.2) |
52.2 (39.6–64.5) |
| Iowa |
516 |
86,000 |
59.9 (54.6–65.0) |
72.6 (60.6–82.1) |
| Kansas |
1,894 |
72,000 |
56.5 (53.8–59.1) |
43.5 (36.8–50.3) |
| Kentucky |
1,055 |
187,000 |
59.3 (54.3–64.1) |
48.4 (38.9–57.9) |
| Louisiana |
527 |
173,000 |
61.1 (55.4–66.5) |
55.8 (43.2–67.7) |
| Maine |
824 |
51,000 |
60.8 (56.1–65.3) |
52.6 (40.0–65.0) |
| Maryland |
1,126 |
140,000 |
52.3 (46.5–58.0) |
38.9 (27.5–51.7) |
| Massachusetts |
656 |
181,000 |
56.8 (51.0–62.4) |
48.1 (35.1–61.5) |
| Michigan |
788 |
344,000 |
62.1 (57.9–66.2) |
45.7 (35.2–56.6) |
| Minnesota |
1,131 |
110,000 |
50.6 (47.0–54.1) |
35.8 (27.9–44.7) |
| Mississippi |
659 |
110,000 |
58.2 (52.3–63.9) |
43.5 (34.0–53.4) |
| Missouri |
780 |
204,000 |
58.3 (53.3–63.1) |
38.2 (29.2–48.1) |
| Montana |
502 |
26,000 |
57.9 (51.6–63.9) |
44.0 (27.3–62.2) |
| Nebraska |
1,447 |
43,000 |
51.8 (47.9–55.7) |
35.8 (29.5–42.7) |
| Nevada |
247 |
86,000 |
63.0 (52.9–72.0) |
41.6 (27.5–57.3) |
| New Hampshire |
614 |
33,000 |
55.2 (49.9–60.3) |
43.4 (27.6–60.7) |
| New Jersey |
848 |
215,000 |
55.9 (50.6–61.0) |
50.4 (36.5–64.2) |
| New Mexico |
572 |
50,000 |
56.0 (49.8–62.0) |
30.5 (25.8–35.7) |
| New York |
959 |
510,000 |
57.3 (53.0–61.6) |
56.1 (44.4–67.3) |
| North Carolina |
580 |
313,000 |
57.9 (52.8–62.8) |
44.5 (33.4–56.2) |
| North Dakota |
414 |
18,000 |
54.1 (47.9–60.1) |
55.2 (35.8–73.2) |
| Ohio |
1,295 |
382,000 |
61.0 (56.2–65.6) |
45.3 (32.4–58.8) |
| Oklahoma |
838 |
161,000 |
65.3 (60.2–70.2) |
47.9 (36.4–59.6) |
| Oregon |
398 |
97,000 |
56.4 (50.1–62.6) |
46.4 (30.9–62.7) |
| Pennsylvania |
485 |
412,000 |
58.4 (52.4–64.2) |
49.9 (33.5–66.3) |
| Rhode Island |
534 |
30,000 |
59.8 (53.7–65.6) |
60.3 (44.3–74.3) |
| South Carolina |
1,134 |
162,000 |
62.0 (58.0–65.8) |
51.0 (41.3–60.7) |
| South Dakota |
715 |
28,000 |
61.1 (54.9–66.9) |
50.8 (36.6–64.9) |
| Tennessee |
703 |
271,000 |
63.2 (58.1–68.0) |
55.1 (42.7–66.9) |
| Texas |
1,362 |
606,000 |
49.9 (44.3–55.5) |
36.8 (28.7–45.8) |
| Utah |
618 |
44,000 |
53.4 (48.3–58.5) |
40.2 (30.6–50.6) |
| Vermont |
477 |
19,000 |
57.8 (52.0–63.3) |
43.8 (30.9–57.6) |
| Virginia |
637 |
182,000 |
51.5 (46.4–56.5) |
36.5 (28.9–44.8) |
| Washington |
1,310 |
180,000 |
57.4 (53.5–61.3) |
47.1 (38.7–55.8) |
| West Virginia |
755 |
102,000 |
63.8 (59.7–67.7) |
53.7 (44.1–63.1) |
| Wisconsin |
494 |
134,000 |
48.9 (42.6–55.2) |
35.9 (25.7–47.7) |
| Wyoming |
564 |
16,000 |
58.6 (52.0–64.9) |
58.6 (39.4–75.5) |
|
Median (Range)**
|
|
|
57.4 (43.5–65.3)
|
44.5 (25.6–72.6)
|
| Guam |
88 |
3,000 |
49.1 (33.5–64.9) |
42.2 (22.3–65.0) |
| Puerto Rico | 586 | 126,000 | 49.2 (44.3–54.2) | 37.3 (30.2–44.9) |
Abbreviation: CI = confidence interval.
* The numerator was the estimated number of adults with arthritis and coronary heart disease. The denominator was the estimated number of adults with coronary heart disease.
† Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Doctor-diagnosed coronary heart disease was defined as a yes response to either of the following two questions: “Has a doctor, nurse, or other health professional ever told you that you had a heart attack, also called a myocardial infarction?” or “Has a doctor, nurse, or other health professional ever told you that you had angina or coronary heart disease?” Those who answered yes to either question were classified as having coronary heart disease. Those who answered no to both questions were classified as not having coronary heart disease.
** Median and range were calculated from estimates for the 50 states and the District of Columbia.
TABLE 4. Unadjusted* and age-standardized† prevalences of arthritis§ among adults aged ≥18 years with diabetes,¶ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | No. of respondents with diabetes | Weighted population with arthritis and diabetes (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized %* (95% CI) |
|---|---|---|---|---|
| Alabama |
1,355 |
283,000 |
56.4 (52.7–60.0) |
43.8 (38.0–49.7) |
| Alaska |
346 |
19,000 |
44.4 (35.3–53.8) |
46.0 (29.6–63.4) |
| Arizona |
1,095 |
238,000 |
45.7 (41.6–49.9) |
32.6 (27.0–38.8) |
| Arkansas |
951 |
167,000 |
58.9 (53.7–64.0) |
48.6 (38.4–58.9) |
| California |
1,283 |
1,088,000 |
36.4 (32.8–40.2) |
27.1 (23.1–31.5) |
| Colorado |
1,216 |
132,000 |
47.0 (42.9–51.1) |
37.3 (30.3–44.9) |
| Connecticut |
1,379 |
117,000 |
45.5 (41.8–49.2) |
30.1 (25.0–35.6) |
| Delaware |
606 |
42,000 |
50.0 (44.5–55.4) |
35.4 (26.8–44.9) |
| District of Columbia |
544 |
22,000 |
47.0 (39.2–55.0) |
28.2 (22.8–34.2) |
| Florida |
1,394 |
958,000 |
53.0 (49.2–56.7) |
35.6 (28.9–43.0) |
| Georgia |
752 |
453,000 |
52.2 (47.4–56.9) |
40.0 (30.8–49.9) |
| Hawaii |
722 |
37,000 |
38.7 (34.0–43.7) |
32.0 (24.9–40.0) |
| Idaho |
678 |
46,000 |
46.8 (41.7–52.0) |
37.0 (28.6–46.2) |
| Illinois |
680 |
452,000 |
46.1 (41.3–50.9) |
34.2 (25.7–44.0) |
| Indiana |
885 |
297,000 |
51.5 (46.6–56.3) |
37.6 (30.9–44.9) |
| Iowa |
753 |
110,000 |
52.1 (47.4–56.7) |
32.2 (26.3–38.7) |
| Kansas |
2,863 |
106,000 |
50.4 (48.2–52.6) |
37.1 (33.8–40.6) |
| Kentucky |
1,457 |
253,000 |
55.9 (51.5–60.3) |
45.4 (37.9–53.0) |
| Louisiana |
793 |
241,000 |
53.7 (49.1–58.4) |
41.5 (33.7–49.7) |
| Maine |
1,083 |
62,000 |
58.2 (54.0–62.2) |
53.7 (43.8–63.3) |
| Maryland |
1,854 |
207,000 |
43.5 (39.1–48.1) |
34.8 (27.2–43.3) |
| Massachusetts |
983 |
230,000 |
48.4 (43.8–53.0) |
37.0 (30.3–44.2) |
| Michigan |
1,087 |
438,000 |
53.2 (49.5–56.9) |
40.6 (34.9–46.5) |
| Minnesota |
1,637 |
150,000 |
47.8 (44.8–50.9) |
36.9 (30.6–43.6) |
| Mississippi |
1,151 |
172,000 |
51.7 (47.5–55.8) |
39.7 (33.6–46.0) |
| Missouri |
1,154 |
297,000 |
55.5 (51.3–59.6) |
53.7 (44.9–62.2) |
| Montana |
652 |
34,000 |
53.9 (48.2–59.5) |
46.4 (34.2–59.1) |
| Nebraska |
2,046 |
60,000 |
48.0 (44.7–51.3) |
30.7 (26.5–35.1) |
| Nevada |
337 |
89,000 |
41.8 (33.9–50.1) |
28.9 (19.1–41.2) |
| New Hampshire |
834 |
46,000 |
53.2 (48.6–57.8) |
36.3 (28.4–45.0) |
| New Jersey |
1,314 |
302,000 |
48.3 (44.1–52.6) |
38.3 (29.4–48.0) |
| New Mexico |
919 |
83,000 |
46.5 (41.7–51.3) |
33.1 (27.2–39.5) |
| New York |
1,469 |
730,000 |
48.1 (44.6–51.6) |
38.8 (32.4–45.7) |
| North Carolina |
855 |
440,000 |
53.4 (49.4–57.4) |
40.5 (33.9–47.6) |
| North Dakota |
565 |
22,000 |
43.8 (38.6–49.1) |
27.4 (21.7–33.9) |
| Ohio |
1,861 |
531,000 |
53.8 (50.1–57.5) |
39.7 (33.0–46.9) |
| Oklahoma |
1,091 |
188,000 |
55.0 (50.9–59.0) |
44.2 (36.6–52.1) |
| Oregon |
655 |
157,000 |
48.0 (43.1–52.9) |
40.0 (31.1–49.5) |
| Pennsylvania |
715 |
575,000 |
55.2 (50.3–60.1) |
40.0 (31.0–49.7) |
| Rhode Island |
748 |
39,000 |
51.5 (46.4–56.6) |
42.9 (29.9–56.9) |
| South Carolina |
1,837 |
254,000 |
56.9 (53.6–60.2) |
47.6 (41.4–54.0) |
| South Dakota |
862 |
28,000 |
46.9 (41.2–52.6) |
31.6 (25.4–38.4) |
| Tennessee |
998 |
348,000 |
54.3 (49.6–59.0) |
42.2 (35.4–49.4) |
| Texas |
2,269 |
977,000 |
42.4 (38.4–46.6) |
27.8 (24.4–31.5) |
| Utah |
1,018 |
68,000 |
46.7 (42.8–50.6) |
33.0 (27.5–39.0) |
| Vermont |
625 |
20,000 |
49.3 (44.4–54.3) |
37.5 (30.1–45.5) |
| Virginia |
1,129 |
328,000 |
48.8 (44.7–53.0) |
34.3 (29.6–39.4) |
| Washington |
1,782 |
219,000 |
47.8 (44.5–51.0) |
35.4 (30.2–41.1) |
| West Virginia |
962 |
132,000 |
62.4 (58.8–65.9) |
52.3 (46.1–58.4) |
| Wisconsin |
678 |
161,000 |
43.4 (38.2–48.8) |
28.3 (22.9–34.4) |
| Wyoming |
678 |
19,000 |
51.7 (46.1–57.2) |
47.2 (33.6–61.3) |
|
Median (Range)**
|
|
|
49.3 (36.4–62.4)
|
37.3 (27.1–53.7)
|
| Guam |
192 |
5,000 |
39.1 (29.7–49.4) |
26.8 (19.2–36.1) |
| Puerto Rico | 1,084 | 206,000 | 45.3 (41.8–48.9) | 28.1 (23.9–32.8) |
Abbreviation: CI = confidence interval.
* The numerator was the estimated number of adults with arthritis and diabetes. The denominator was the estimated number of adults with diabetes.
† Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Doctor-diagnosed diabetes was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have diabetes?” Those with prediabetes or borderline diabetes and women who had diabetes only during pregnancy were classified as not having diabetes.
** Median and range were calculated from estimates for the 50 states and the District of Columbia.
Health-Related Characteristics
General Health
In 2015, the percentage of poor health-related quality of life among adults with arthritis varied substantially by state. The median age-standardized percentage of ≥14 physically unhealthy days during the past 30 days was 27.7% (range: 16.9% in Alaska to 37.5% in Oklahoma) (Table 5). The median age-standardized percentage of ≥14 mentally unhealthy days during the past 30 days was 22.3% (range: 14.8% in Hawaii to 31.1% Mississippi) (Table 6).
TABLE 5. Unadjusted and age-standardized* percentages of ≥14 physically unhealthy days† during the past 30 days among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | Weighted population with arthritis (rounded to 1,000s) | Weighted population with arthritis and ≥14 physically unhealthy days (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
1,248,000 |
365,000 |
30.5 (28.3–32.7) |
30.6 (27.2–34.2) |
| Alaska |
117,000 |
23,000 |
21.3 (17.9–25.2) |
16.9 (13.4–21.2) |
| Arizona |
1,222,000 |
354,000 |
29.7 (27.2–32.3) |
30.1 (25.8–34.8) |
| Arkansas |
672,000 |
208,000 |
32.3 (29.0–35.8) |
35.7 (29.8–42.1) |
| California |
5,719,000 |
1,383,000 |
24.5 (22.5–26.7) |
24.6 (21.3–28.2) |
| Colorado |
949,000 |
232,000 |
25.1 (23.1–27.3) |
27.7 (23.9–31.7) |
| Connecticut |
690,000 |
157,000 |
23.4 (21.5–25.5) |
25.1 (21.3–29.2) |
| Delaware |
207,000 |
48,000 |
23.9 (21.0–27.0) |
24.8 (19.9–30.5) |
| District of Columbia |
101,000 |
25,000 |
25.6 (21.2–30.6) |
23.0 (15.3–33.1) |
| Florida |
4,154,000 |
1,190,000 |
30.0 (27.8–32.4) |
33.6 (28.8–38.9) |
| Georgia |
1,890,000 |
526,000 |
28.7 (25.8–31.8) |
25.0 (20.7–29.9) |
| Hawaii |
211,000 |
45,000 |
21.4 (18.8–24.3) |
21.0 (16.7–26.2) |
| Idaho |
309,000 |
68,000 |
22.8 (20.3–25.4) |
24.7 (20.3–29.6) |
| Illinois |
2,308,000 |
595,000 |
26.0 (23.2–28.9) |
24.8 (19.9–30.4) |
| Indiana |
1,390,000 |
377,000 |
28.3 (25.6–31.1) |
30.1 (24.9–35.8) |
| Iowa |
619,000 |
131,000 |
21.9 (19.7–24.2) |
20.4 (16.6–24.7) |
| Kansas |
536,000 |
119,000 |
23.0 (21.8–24.2) |
22.9 (20.9–25.1) |
| Kentucky |
1,087,000 |
338,000 |
31.9 (29.4–34.5) |
30.2 (26.2–34.5) |
| Louisiana |
989,000 |
288,000 |
30.5 (27.6–33.4) |
29.8 (25.3–34.7) |
| Maine |
332,000 |
82,000 |
25.2 (23.1–27.5) |
29.1 (24.9–33.7) |
| Maryland |
1,096,000 |
260,000 |
24.7 (22.0–27.5) |
28.7 (23.1–35.0) |
| Massachusetts |
1,300,000 |
325,000 |
26.1 (23.8–28.6) |
29.0 (25.0–33.3) |
| Michigan |
2,305,000 |
622,000 |
27.5 (25.6–29.5) |
29.8 (26.5–33.2) |
| Minnesota |
907,000 |
218,000 |
24.8 (23.1–26.5) |
27.1 (23.7–30.6) |
| Mississippi |
647,000 |
224,000 |
35.6 (32.8–38.5) |
35.5 (30.8–40.6) |
| Missouri |
1,372,000 |
390,000 |
29.1 (26.7–31.7) |
29.3 (24.9–34.0) |
| Montana |
216,000 |
54,000 |
25.5 (22.8–28.4) |
26.7 (21.9–32.1) |
| Nebraska |
334,000 |
70,000 |
21.3 (19.7–23.0) |
20.3 (17.5–23.4) |
| Nevada |
477,000 |
126,000 |
27.5 (22.9–32.5) |
30.6 (22.6–40.0) |
| New Hampshire |
282,000 |
64,000 |
23.1 (20.9–25.6) |
25.5 (20.9–30.8) |
| New Jersey |
1,590,000 |
378,000 |
24.8 (22.5–27.1) |
24.4 (20.9–28.3) |
| New Mexico |
386,000 |
111,000 |
29.3 (26.7–32.1) |
27.8 (23.2–33.0) |
| New York |
3,629,000 |
910,000 |
26.5 (24.5–28.6) |
30.0 (26.0–34.2) |
| North Carolina |
2,089,000 |
607,000 |
30.2 (27.7–32.7) |
27.8 (24.2–31.6) |
| North Dakota |
134,000 |
28,000 |
21.5 (18.8–24.4) |
21.7 (17.1–27.0) |
| Ohio |
2,547,000 |
664,000 |
26.8 (24.6–29.1) |
27.0 (22.8–31.6) |
| Oklahoma |
813,000 |
278,000 |
35.2 (32.5–38.0) |
37.5 (32.7–42.6) |
| Oregon |
838,000 |
238,000 |
29.6 (26.9–32.5) |
30.2 (25.8–35.0) |
| Pennsylvania |
2,937,000 |
682,000 |
23.8 (21.5–26.4) |
24.4 (20.4–28.8) |
| Rhode Island |
226,000 |
61,000 |
28.4 (25.6–31.3) |
32.7 (27.1–38.9) |
| South Carolina |
1,105,000 |
332,000 |
31.1 (29.2–33.2) |
31.3 (27.8–35.0) |
| South Dakota |
158,000 |
35,000 |
22.4 (19.7–25.5) |
20.3 (16.5–24.7) |
| Tennessee |
1,630,000 |
521,000 |
33.0 (30.2–36.0) |
31.9 (27.4–36.8) |
| Texas |
4,055,000 |
1,035,000 |
26.7 (24.2–29.3) |
25.9 (22.0–30.3) |
| Utah |
407,000 |
98,000 |
24.8 (22.8–27.0) |
25.3 (22.4–28.4) |
| Vermont |
136,000 |
33,000 |
25.3 (22.8–28.0) |
26.5 (21.9–31.6) |
| Virginia |
1,513,000 |
359,000 |
24.3 (22.1–26.6) |
24.5 (20.6–28.8) |
| Washington |
1,346,000 |
332,000 |
25.2 (23.5–26.9) |
27.7 (24.3–31.3) |
| West Virginia |
557,000 |
186,000 |
34.1 (32.0–36.4) |
33.1 (29.8–36.5) |
| Wisconsin |
1,104,000 |
264,000 |
24.2 (21.7–27.0) |
21.1 (17.6–25.0) |
| Wyoming |
116,000 |
30,000 |
26.5 (23.3–29.9) |
28.9 (23.1–35.4) |
|
Median (Range)¶
|
|
|
26.0 (21.3–35.6)
|
27.7 (16.9–37.5)
|
| Guam |
17,000 |
4,000 |
23.8 (17.5–31.4) |
21.5 (14.8–30.2) |
| Puerto Rico | 635,000 | 196,000 | 31.0 (28.3–33.8) | 30.6 (25.8–35.9) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Respondents with arthritis who answered 14–30 days to the question “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?”
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Median and range were calculated from estimates for the 50 states and the District of Columbia.
TABLE 6. Unadjusted and age-standardized* percentages of ≥14 mentally unhealthy days† during the past 30 days among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
|
Area
|
Weighted population with arthritis (rounded to 1,000s)
|
Weighted population with arthritis and ≥14 mentally unhealthy days (rounded to 1,000s)
|
Unadjusted % (95% CI)
|
Age-standardized % (95% CI)
|
| Alabama |
1,248,000 |
268,000 |
22.0 (20.0–24.1) |
29.4 (25.8–33.2) |
| Alaska |
117,000 |
19,000 |
16.6 (13.2–20.7) |
18.0 (13.0–24.4) |
| Arizona |
1,222,000 |
210,000 |
17.5 (15.5–19.7) |
21.0 (17.3–25.4) |
| Arkansas |
672,000 |
138,000 |
21.2 (18.2–24.5) |
26.6 (21.2–32.7) |
| California |
5,719,000 |
934,000 |
16.6 (14.8–18.5) |
21.7 (18.4–25.4) |
| Colorado |
949,000 |
145,000 |
15.7 (13.8–17.7) |
23.1 (19.3–27.4) |
| Connecticut |
690,000 |
104,000 |
15.3 (13.7–17.0) |
21.1 (17.7–25.0) |
| Delaware |
207,000 |
36,000 |
17.5 (15.0–20.4) |
20.1 (15.4–25.7) |
| District of Columbia |
101,000 |
17,000 |
17.5 (13.5–22.3) |
20.1 (12.4–31.0) |
| Florida |
4,154,000 |
772,000 |
19.0 (17.1–21.2) |
23.9 (20.0–28.3) |
| Georgia |
1,890,000 |
343,000 |
18.8 (16.2–21.7) |
21.0 (16.1–26.9) |
| Hawaii |
211,000 |
24,000 |
11.7 (9.7–13.9) |
14.8 (10.9–19.9) |
| Idaho |
309,000 |
46,000 |
15.3 (13.0–17.9) |
22.2 (17.5–27.7) |
| Illinois |
2,308,000 |
330,000 |
14.6 (12.4–17.0) |
19.3 (15.0–24.5) |
| Indiana |
1,390,000 |
241,000 |
17.8 (15.5–20.4) |
24.4 (19.4–30.2) |
| Iowa |
619,000 |
85,000 |
13.9 (12.0–16.1) |
22.3 (17.8–27.6) |
| Kansas |
536,000 |
77,000 |
14.6 (13.6–15.7) |
20.3 (18.2–22.6) |
| Kentucky |
1,087,000 |
224,000 |
21.1 (18.6–23.8) |
26.5 (21.9–31.7) |
| Louisiana |
989,000 |
199,000 |
20.6 (18.2–23.3) |
25.6 (21.2–30.6) |
| Maine |
332,000 |
57,000 |
17.6 (15.7–19.6) |
25.0 (21.1–29.4) |
| Maryland |
1,096,000 |
204,000 |
19.0 (16.5–21.9) |
29.9 (24.2–36.2) |
| Massachusetts |
1,300,000 |
238,000 |
18.8 (16.7–21.1) |
26.3 (22.3–30.9) |
| Michigan |
2,305,000 |
408,000 |
18.0 (16.3–19.8) |
24.0 (20.9–27.4) |
| Minnesota |
907,000 |
118,000 |
13.3 (12.0–14.7) |
19.5 (16.6–22.7) |
| Mississippi |
647,000 |
148,000 |
23.6 (21.0–26.4) |
31.1 (26.3–36.3) |
| Missouri |
1,372,000 |
263,000 |
19.6 (17.2–22.1) |
25.8 (21.1–31.1) |
| Montana |
216,000 |
34,000 |
16.0 (13.6–18.7) |
21.8 (16.9–27.7) |
| Nebraska |
334,000 |
43,000 |
13.1 (11.8–14.6) |
16.7 (13.9–20.1) |
| Nevada |
477,000 |
93,000 |
19.9 (15.4–25.3) |
30.0 (21.5–40.2) |
| New Hampshire |
282,000 |
45,000 |
16.3 (14.3–18.5) |
24.1 (19.2–29.8) |
| New Jersey |
1,590,000 |
249,000 |
16.0 (14.1–18.2) |
21.3 (17.2–26.2) |
| New Mexico |
386,000 |
65,000 |
17.2 (15.0–19.7) |
21.6 (17.2–26.8) |
| New York |
3,629,000 |
636,000 |
18.2 (16.4–20.1) |
23.3 (19.9–27.0) |
| North Carolina |
2,089,000 |
404,000 |
19.7 (17.6–22.0) |
24.6 (20.8–28.8) |
| North Dakota |
134,000 |
17,000 |
13.3 (10.7–16.4) |
21.7 (16.2–28.3) |
| Ohio |
2,547,000 |
470,000 |
18.9 (16.8–21.1) |
25.6 (21.3–30.3) |
| Oklahoma |
813,000 |
179,000 |
22.6 (20.2–25.2) |
28.6 (24.1–33.5) |
| Oregon |
838,000 |
167,000 |
20.6 (18.1–23.3) |
27.4 (22.9–32.5) |
| Pennsylvania |
2,937,000 |
478,000 |
16.6 (14.5–18.9) |
21.0 (17.0–25.5) |
| Rhode Island |
226,000 |
41,000 |
18.4 (16.0–21.2) |
26.9 (21.5–33.2) |
| South Carolina |
1,105,000 |
238,000 |
22.3 (20.5–24.2) |
28.4 (24.9–32.3) |
| South Dakota |
158,000 |
18,000 |
11.3 (9.2–13.9) |
15.7 (11.6–21.1) |
| Tennessee |
1,630,000 |
337,000 |
21.0 (18.6–23.7) |
25.8 (21.3–30.8) |
| Texas |
4,055,000 |
658,000 |
16.7 (14.6–19.1) |
23.2 (18.8–28.3) |
| Utah |
407,000 |
66,000 |
16.7 (14.9–18.6) |
20.4 (17.6–23.5) |
| Vermont |
136,000 |
20,000 |
15.1 (13.1–17.2) |
20.3 (16.4–24.9) |
| Virginia |
1,513,000 |
207,000 |
14.0 (12.2–15.9) |
19.7 (16.2–23.8) |
| Washington |
1,346,000 |
211,000 |
15.9 (14.5–17.4) |
20.8 (17.9–24.1) |
| West Virginia |
557,000 |
127,000 |
23.5 (21.5–25.5) |
28.5 (25.3–32.0) |
| Wisconsin |
1,104,000 |
173,000 |
15.8 (13.5–18.4) |
22.0 (17.2–27.6) |
| Wyoming |
116,000 |
18,000 |
15.8 (13.3–18.7) |
20.0 (15.5–25.5) |
|
Median (Range)¶
|
|
|
17.5 (11.3–23.6)
|
22.3 (14.8–31.1)
|
| Guam |
17,000 |
3,000 |
15.5 (10.9–21.5) |
18.1 (11.5–27.3) |
| Puerto Rico | 635,000 | 144,000 | 23.0 (20.5–25.6) | 27.7 (22.9–33.0) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Respondents with arthritis who answered 14–30 days to the question “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?”
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Median and range were calculated from estimates for the 50 states and the District of Columbia.
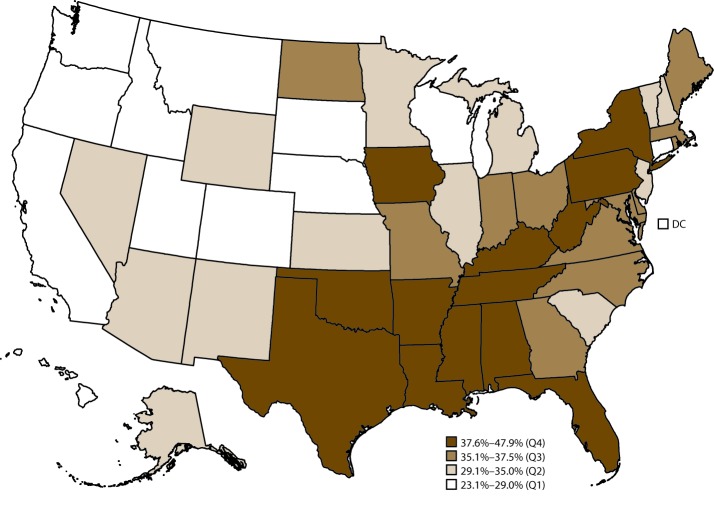
Leisure-Time Physical Activity and Obesity
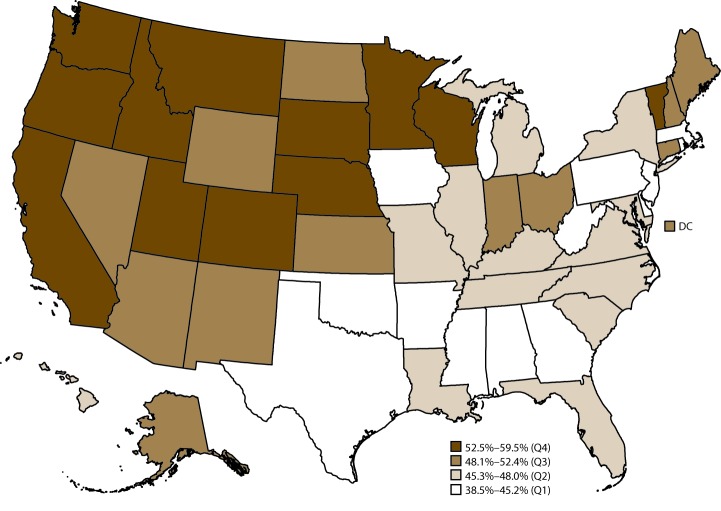
In 2015, for leisure-time physical inactivity, the median age-standardized percentage among adults with arthritis was 35.0% (range: 23.1% in California to 47.9% in Mississippi) (Table 7). States in the western United States (e.g., California, Idaho, Oregon, and Washington) tended to have the lowest prevalence of leisure-time physical inactivity among adults with arthritis, whereas states primarily in Appalachia and along the Ohio River and Mississippi River had the highest percentage of leisure-time physical inactivity (Figure 2). Age-standardized percentage of leisure-time physical inactivity was ≥40% in Alabama, Arkansas, Louisiana, Mississippi, Oklahoma, and Texas. For the 50 states and the District of Columbia, the median age-standardized percentage of leisure-time walking was 48.0% (range: 38.5% in West Virginia to 59.5% in Montana) (Table 8). Leisure-time walking tended to be highest in western states (e.g., California, Idaho, Oregon, and Washington) and lowest in states primarily in Appalachia and along the Ohio River and Mississippi River (e.g., Alabama, Arkansas, Mississippi, and West Virginia) (Figure 3).
TABLE 7. Unadjusted and age-standardized* percentages of physical inactivity† among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | Weighted population with arthritis (rounded to 1,000s) | Weighted population with arthritis and physical inactivity (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
1,248,000 |
488,000 |
43.7 (41.2–46.2) |
40.0 (36.2–44.0) |
| Alaska |
117,000 |
33,000 |
31.8 (27.1–36.9) |
30.8 (24.1–38.5) |
| Arizona |
1,222,000 |
357,000 |
33.7 (31.1–36.4) |
31.8 (27.0–36.9) |
| Arkansas |
672,000 |
280,000 |
47.6 (43.8–51.5) |
44.3 (38.0–50.8) |
| California |
5,719,000 |
1,217,000 |
24.7 (22.5–27.1) |
23.1 (19.8–26.9) |
| Colorado |
949,000 |
218,000 |
27.0 (24.9–29.3) |
25.2 (21.8–28.9) |
| Connecticut |
690,000 |
195,000 |
32.5 (30.4–34.7) |
26.7 (23.4–30.2) |
| Delaware |
207,000 |
78,000 |
41.8 (38.2–45.5) |
37.5 (31.1–44.3) |
| District of Columbia |
101,000 |
25,000 |
30.9 (26.1–36.1) |
24.9 (16.2–36.2) |
| Florida |
4,154,000 |
1,396,000 |
39.1 (36.6–41.7) |
36.6 (31.3–42.2) |
| Georgia |
1,890,000 |
650,000 |
38.9 (35.6–42.3) |
35.9 (29.6–42.6) |
| Hawaii |
211,000 |
50,000 |
26.0 (23.2–29.0) |
29.0 (23.7–34.8) |
| Idaho |
309,000 |
87,000 |
31.1 (28.2–34.1) |
28.6 (23.9–33.8) |
| Illinois |
2,308,000 |
768,000 |
36.4 (33.4–39.5) |
33.4 (28.1–39.0) |
| Indiana |
1,390,000 |
505,000 |
40.9 (37.8–44.0) |
37.0 (31.3–43.1) |
| Iowa |
619,000 |
205,000 |
37.5 (34.7–40.3) |
38.5 (33.0–44.3) |
| Kansas |
536,000 |
173,000 |
36.9 (35.5–38.3) |
33.0 (30.6–35.5) |
| Kentucky |
1,087,000 |
423,000 |
44.1 (41.2–47.0) |
39.9 (35.4–44.7) |
| Louisiana |
989,000 |
375,000 |
44.6 (41.3–48.0) |
40.1 (34.7–45.6) |
| Maine |
332,000 |
111,000 |
36.9 (34.5–39.2) |
36.0 (31.7–40.5) |
| Maryland |
1,096,000 |
355,000 |
38.0 (34.9–41.2) |
37.1 (31.2–43.5) |
| Massachusetts |
1,300,000 |
408,000 |
37.7 (34.9–40.5) |
36.0 (31.3–41.0) |
| Michigan |
2,305,000 |
747,000 |
35.7 (33.5–37.9) |
34.0 (30.5–37.7) |
| Minnesota |
907,000 |
275,000 |
33.1 (31.3–35.0) |
30.7 (27.3–34.3) |
| Mississippi |
647,000 |
297,000 |
50.1 (47.0–53.1) |
47.9 (42.7–53.1) |
| Missouri |
1,372,000 |
466,000 |
37.3 (34.6–40.2) |
36.6 (31.6–41.9) |
| Montana |
216,000 |
61,000 |
30.3 (27.4–33.4) |
28.9 (24.0–34.4) |
| Nebraska |
334,000 |
104,000 |
34.0 (32.1–36.0) |
28.5 (25.2–32.2) |
| Nevada |
477,000 |
140,000 |
33.0 (27.9–38.5) |
31.0 (23.1–40.1) |
| New Hampshire |
282,000 |
87,000 |
35.0 (32.3–37.7) |
33.0 (27.7–38.8) |
| New Jersey |
1,590,000 |
523,000 |
37.1 (34.4–39.8) |
32.8 (28.4–37.4) |
| New Mexico |
386,000 |
104,000 |
30.3 (27.6–33.2) |
29.1 (24.1–34.7) |
| New York |
3,629,000 |
1,241,000 |
41.1 (38.8–43.4) |
39.7 (35.3–44.1) |
| North Carolina |
2,089,000 |
749,000 |
39.9 (37.2–42.7) |
37.1 (32.8–41.6) |
| North Dakota |
134,000 |
45,000 |
37.4 (34.1–40.7) |
35.1 (29.3–41.4) |
| Ohio |
2,547,000 |
884,000 |
39.2 (36.7–41.7) |
35.7 (31.3–40.5) |
| Oklahoma |
813,000 |
340,000 |
45.9 (43.1–48.7) |
41.9 (37.1–46.8) |
| Oregon |
838,000 |
193,000 |
26.8 (24.0–29.7) |
24.0 (19.9–28.7) |
| Pennsylvania |
2,937,000 |
1,010,000 |
39.2 (36.3–42.3) |
38.0 (32.9–43.4) |
| Rhode Island |
226,000 |
75,000 |
38.5 (35.5–41.7) |
36.8 (30.5–43.6) |
| South Carolina |
1,105,000 |
373,000 |
37.6 (35.5–39.7) |
35.0 (31.4–38.7) |
| South Dakota |
158,000 |
43,000 |
29.7 (26.4–33.2) |
23.4 (19.3–28.0) |
| Tennessee |
1,630,000 |
575,000 |
41.2 (38.0–44.5) |
38.9 (33.7–44.3) |
| Texas |
4,055,000 |
1,519,000 |
43.0 (40.0–46.0) |
43.4 (38.5–48.5) |
| Utah |
407,000 |
106,000 |
29.4 (27.2–31.6) |
28.0 (24.8–31.4) |
| Vermont |
136,000 |
40,000 |
32.1 (29.4–35.0) |
31.0 (26.4–36.1) |
| Virginia |
1,513,000 |
520,000 |
38.1 (35.4–40.9) |
36.3 (31.9–40.9) |
| Washington |
1,346,000 |
317,000 |
26.3 (24.6–28.0) |
25.8 (22.6–29.4) |
| West Virginia |
557,000 |
209,000 |
41.0 (38.7–43.4) |
38.6 (35.0–42.3) |
| Wisconsin |
1,104,000 |
281,000 |
29.0 (26.2–32.1) |
24.6 (19.9–30.0) |
| Wyoming |
116,000 |
37,000 |
35.2 (31.8–38.8) |
34.4 (28.6–40.7) |
|
Median (Range)¶
|
|
|
37.1 (24.7–50.1)
|
35.0 (23.1–47.9)
|
| Guam |
17,000 |
7,000 |
45.7 (37.1–54.5) |
39.6 (29.8–50.2) |
| Puerto Rico | 635,000 | 371,000 | 60.5 (57.5–63.5) | 58.1 (52.1–63.8) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Physical inactivity was defined as a no response to the question “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?”
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Median and range were calculated from estimates for the 50 states and the District of Columbia.
FIGURE 2.
Age-standardized prevalence of physical inactivity* among adults aged ≥18 years with arthritis, by state — Behavioral Risk Factor Surveillance System, United States, 2015
Abbreviations: DC = District of Columbia; Q = quartile.
* Physical inactivity was defined as a no response to the question “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?”
TABLE 8. Unadjusted and age-standardized* percentages of walking† among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | Weighted population with arthritis (rounded to 1,000s) | Weighted population with arthritis and walking (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
1,248,000 |
501,000 |
43.6 (41.1–46.0) |
44.8 (40.7–48.9) |
| Alaska |
117,000 |
59,000 |
53.9 (48.9–58.8) |
52.3 (44.8–59.7) |
| Arizona |
1,222,000 |
570,000 |
51.5 (48.7–54.3) |
50.8 (45.3–56.2) |
| Arkansas |
672,000 |
249,000 |
40.6 (37.0–44.3) |
41.8 (35.4–48.4) |
| California |
5,719,000 |
2,996,000 |
59.4 (56.7–62.0) |
55.6 (51.3–59.9) |
| Colorado |
949,000 |
464,000 |
55.4 (52.9–57.7) |
55.4 (50.9–59.8) |
| Connecticut |
690,000 |
308,000 |
49.4 (47.2–51.7) |
51.5 (47.1–55.9) |
| Delaware |
207,000 |
83,000 |
42.9 (39.4–46.4) |
43.1 (36.5–49.9) |
| District of Columbia |
101,000 |
50,000 |
53.6 (48.2–59.0) |
51.9 (40.2–63.5) |
| Florida |
4,154,000 |
1,751,000 |
47.2 (44.7–49.7) |
46.9 (41.4–52.4) |
| Georgia |
1,890,000 |
829,000 |
47.7 (44.4–51.1) |
45.2 (38.8–51.7) |
| Hawaii |
211,000 |
101,000 |
52.1 (48.8–55.4) |
47.2 (41.4–53.1) |
| Idaho |
309,000 |
157,000 |
54.1 (50.9–57.3) |
53.0 (47.3–58.5) |
| Illinois |
2,308,000 |
949,000 |
44.6 (41.5–47.7) |
45.7 (39.9–51.6) |
| Indiana |
1,390,000 |
615,000 |
48.3 (45.2–51.4) |
51.8 (45.8–57.7) |
| Iowa |
619,000 |
268,000 |
47.2 (44.4–50.1) |
43.5 (38.1–49.0) |
| Kansas |
536,000 |
230,000 |
47.4 (46.0–48.9) |
48.9 (46.2–51.5) |
| Kentucky |
1,087,000 |
426,000 |
42.9 (40.0–45.8) |
46.2 (41.2–51.2) |
| Louisiana |
989,000 |
377,000 |
42.3 (39.0–45.6) |
46.3 (40.9–51.9) |
| Maine |
332,000 |
158,000 |
50.7 (48.2–53.1) |
51.0 (46.2–55.7) |
| Maryland |
1,096,000 |
457,000 |
46.5 (43.5–49.6) |
46.2 (40.2–52.3) |
| Massachusetts |
1,300,000 |
539,000 |
46.9 (44.1–49.7) |
43.4 (38.9–48.0) |
| Michigan |
2,305,000 |
1,018,000 |
46.8 (44.6–49.0) |
45.7 (42.1–49.3) |
| Minnesota |
907,000 |
441,000 |
51.6 (49.7–53.5) |
52.6 (48.9–56.2) |
| Mississippi |
647,000 |
248,000 |
40.2 (37.4–43.1) |
40.3 (35.3–45.5) |
| Missouri |
1,372,000 |
592,000 |
46.1 (43.4–49.0) |
48.0 (42.7–53.3) |
| Montana |
216,000 |
120,000 |
57.9 (54.8–60.9) |
59.5 (53.8–64.9) |
| Nebraska |
334,000 |
161,000 |
51.0 (48.9–53.1) |
52.9 (48.7–57.1) |
| Nevada |
477,000 |
226,000 |
51.2 (45.5–56.9) |
49.3 (39.9–58.9) |
| New Hampshire |
282,000 |
129,000 |
49.9 (47.1–52.6) |
49.1 (43.2–55.0) |
| New Jersey |
1,590,000 |
670,000 |
45.3 (42.6–48.1) |
43.6 (38.8–48.6) |
| New Mexico |
386,000 |
185,000 |
52.5 (49.4–55.6) |
52.4 (46.3–58.4) |
| New York |
3,629,000 |
1,540,000 |
48.3 (46.1–50.6) |
47.3 (43.0–51.6) |
| North Carolina |
2,089,000 |
892,000 |
45.2 (42.5–47.9) |
45.6 (41.1–50.2) |
| North Dakota |
134,000 |
67,000 |
52.7 (49.3–56.0) |
52.0 (45.5–58.4) |
| Ohio |
2,547,000 |
1,068,000 |
45.3 (42.9–47.8) |
48.2 (43.4–53.0) |
| Oklahoma |
813,000 |
315,000 |
41.1 (38.4–43.8) |
43.1 (38.3–48.0) |
| Oregon |
838,000 |
413,000 |
54.2 (51.1–57.1) |
53.7 (48.5–58.9) |
| Pennsylvania |
2,937,000 |
1,234,000 |
46.3 (43.4–49.3) |
44.4 (39.3–49.6) |
| Rhode Island |
226,000 |
89,000 |
43.9 (41.0–46.9) |
41.5 (35.6–47.5) |
| South Carolina |
1,105,000 |
479,000 |
46.2 (44.1–48.3) |
45.3 (41.3–49.2) |
| South Dakota |
158,000 |
80,000 |
53.6 (50.0–57.2) |
54.5 (47.9–61.0) |
| Tennessee |
1,630,000 |
680,000 |
46.3 (43.2–49.5) |
46.4 (41.1–51.8) |
| Texas |
4,055,000 |
1,651,000 |
45.2 (42.3–48.2) |
40.3 (36.1–44.7) |
| Utah |
407,000 |
201,000 |
53.6 (51.3–56.0) |
53.1 (49.6–56.7) |
| Vermont |
136,000 |
69,000 |
53.3 (50.4–56.1) |
53.5 (48.3–58.6) |
| Virginia |
1,513,000 |
663,000 |
46.6 (44.0–49.3) |
46.1 (41.2–51.0) |
| Washington |
1,346,000 |
710,000 |
56.4 (54.5–58.3) |
54.6 (50.7–58.5) |
| West Virginia |
557,000 |
208,000 |
39.0 (36.8–41.3) |
38.5 (35.0–42.1) |
| Wisconsin |
1,104,000 |
544,000 |
54.4 (51.0–57.7) |
57.0 (50.2–63.5) |
| Wyoming |
116,000 |
54,000 |
50.2 (46.7–53.8) |
50.0 (43.8–56.3) |
|
Median (Range)¶
|
|
|
47.7 (39.0–59.4)
|
48.0 (38.5–59.5)
|
| Guam |
17,000 |
6,000 |
36.3 (28.6–44.7) |
34.0 (23.5–46.3) |
| Puerto Rico | 635,000 | 173,000 | 27.8 (25.2–30.6) | 28.5 (23.4–34.1) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Respondents with arthritis who reported walking or hiking for one of two questions: 1) “What type of physical activity or exercise did you spend the most time doing during the past month?” and 2) “What other type of physical activity gave you the next most exercise during the past month?” The denominator included adults with arthritis who were either physically active or inactive.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Median and range were calculated from estimates for the 50 states and the District of Columbia.
FIGURE 3.
Age-standardized prevalence of walking* among adults aged ≥18 years with arthritis, by state — Behavioral Risk Factor Surveillance System, United States, 2015
Abbreviations: DC = District of Columbia; Q = quartile.
* Respondents with arthritis who reported walking or hiking for one of two questions: 1) “What type of physical activity or exercise did you spend the most time doing during the past month?” and 2) “What other type of physical activity gave you the next most exercise during the past month?”
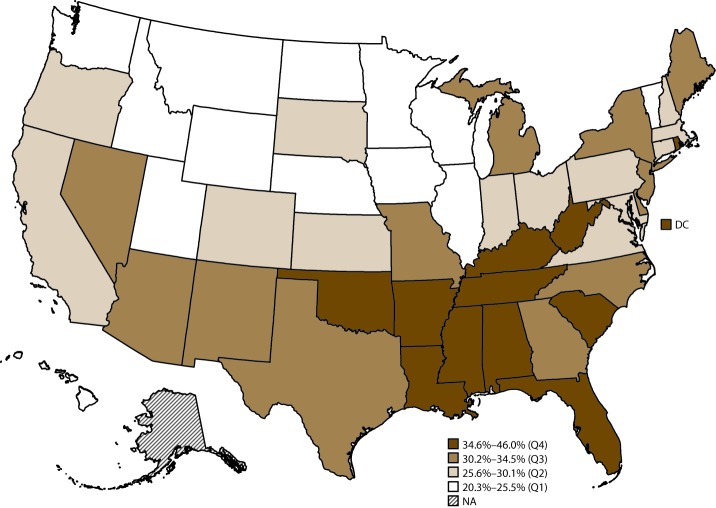
For the 50 states and the District of Columbia, the percentage of obesity among adults with arthritis varied substantially. The median age-standardized percentage of obesity was 41.6% (range: 28.1% in California to 48.9% in Arkansas) (Table 9).
TABLE 9. Unadjusted and age-standardized* percentages of obesity† among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | Weighted population with arthritis (rounded to 1,000s) | Weighted population with arthritis and obesity (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
1,248,000 |
512,000 |
43.8 (41.4–46.2) |
45.9 (42.0–49.9) |
| Alaska |
117,000 |
46,000 |
41.6 (36.9–46.5) |
45.0 (37.8–52.4) |
| Arizona |
1,222,000 |
398,000 |
35.6 (33.0–38.4) |
34.6 (29.9–39.6) |
| Arkansas |
672,000 |
275,000 |
44.2 (40.5–47.9) |
48.9 (42.5–55.4) |
| California |
5,719,000 |
1,749,000 |
33.0 (30.6–35.6) |
33.7 (29.8–37.9) |
| Colorado |
949,000 |
250,000 |
28.9 (26.8–31.1) |
28.1 (24.7–31.9) |
| Connecticut |
690,000 |
228,000 |
35.7 (33.6–37.9) |
37.3 (33.2–41.6) |
| Delaware |
207,000 |
70,000 |
37.5 (34.1–41.0) |
38.4 (32.1–45.1) |
| District of Columbia |
101,000 |
41,000 |
43.9 (38.5–49.5) |
42.4 (30.7–55.0) |
| Florida |
4,154,000 |
1,381,000 |
36.0 (33.6–38.5) |
38.4 (33.2–43.8) |
| Georgia |
1,890,000 |
759,000 |
42.2 (38.9–45.5) |
38.0 (32.6–43.8) |
| Hawaii |
211,000 |
67,000 |
32.5 (29.5–35.8) |
42.2 (36.6–48.0) |
| Idaho |
309,000 |
105,000 |
36.4 (33.3–39.6) |
37.3 (32.1–42.8) |
| Illinois |
2,308,000 |
946,000 |
42.1 (39.0–45.2) |
41.8 (36.2–47.6) |
| Indiana |
1,390,000 |
537,000 |
41.7 (38.7–44.7) |
44.1 (38.3–50.1) |
| Iowa |
619,000 |
241,000 |
42.2 (39.4–45.0) |
44.7 (39.3–50.3) |
| Kansas |
536,000 |
194,000 |
41.1 (39.7–42.6) |
43.2 (40.6–45.9) |
| Kentucky |
1,087,000 |
457,000 |
44.9 (42.0–47.9) |
48.5 (43.5–53.5) |
| Louisiana |
989,000 |
419,000 |
45.3 (42.0–48.6) |
48.5 (43.2–53.9) |
| Maine |
332,000 |
122,000 |
38.7 (36.3–41.1) |
42.3 (37.7–47.0) |
| Maryland |
1,096,000 |
448,000 |
44.4 (41.2–47.6) |
47.9 (41.8–54.1) |
| Massachusetts |
1,300,000 |
422,000 |
36.1 (33.4–38.9) |
35.8 (31.5–40.3) |
| Michigan |
2,305,000 |
875,000 |
40.4 (38.2–42.6) |
42.1 (38.6–45.8) |
| Minnesota |
907,000 |
321,000 |
38.3 (36.5–40.2) |
40.3 (36.6–44.0) |
| Mississippi |
647,000 |
260,000 |
42.0 (39.1–44.9) |
44.3 (39.2–49.5) |
| Missouri |
1,372,000 |
518,000 |
40.7 (38.0–43.5) |
42.9 (37.8–48.2) |
| Montana |
216,000 |
62,000 |
31.1 (28.3–34.1) |
29.6 (24.8–34.8) |
| Nebraska |
334,000 |
134,000 |
42.6 (40.6–44.7) |
45.1 (40.9–49.2) |
| Nevada |
477,000 |
155,000 |
34.4 (29.2–39.9) |
35.2 (26.7–44.7) |
| New Hampshire |
282,000 |
94,000 |
36.9 (34.3–39.6) |
40.7 (35.0–46.6) |
| New Jersey |
1,590,000 |
539,000 |
37.3 (34.6–40.1) |
38.7 (34.1–43.6) |
| New Mexico |
386,000 |
127,000 |
35.2 (32.2–38.3) |
43.1 (37.3–49.1) |
| New York |
3,629,000 |
1,221,000 |
36.4 (34.2–38.6) |
40.1 (36.0–44.4) |
| North Carolina |
2,089,000 |
780,000 |
40.0 (37.3–42.7) |
41.4 (37.0–46.0) |
| North Dakota |
134,000 |
51,000 |
41.3 (38.1–44.7) |
39.7 (34.1–45.6) |
| Ohio |
2,547,000 |
947,000 |
40.2 (37.8–42.7) |
40.4 (35.7–45.2) |
| Oklahoma |
813,000 |
329,000 |
42.9 (40.2–45.7) |
44.9 (40.1–49.8) |
| Oregon |
838,000 |
302,000 |
39.3 (36.4–42.4) |
41.6 (36.6–46.8) |
| Pennsylvania |
2,937,000 |
1,114,000 |
40.8 (37.9–43.7) |
43.3 (38.2–48.5) |
| Rhode Island |
226,000 |
74,000 |
35.1 (32.2–38.1) |
34.7 (29.1–40.7) |
| South Carolina |
1,105,000 |
437,000 |
42.0 (39.9–44.1) |
46.4 (42.6–50.3) |
| South Dakota |
158,000 |
60,000 |
40.4 (36.9–44.0) |
41.8 (35.3–48.5) |
| Tennessee |
1,630,000 |
640,000 |
42.3 (39.2–45.5) |
46.5 (41.3–51.8) |
| Texas |
4,055,000 |
1,518,000 |
41.0 (38.1–43.9) |
37.6 (33.4–42.0) |
| Utah |
407,000 |
137,000 |
36.2 (33.9–38.5) |
36.2 (32.9–39.6) |
| Vermont |
136,000 |
43,000 |
34.2 (31.5–36.9) |
35.7 (30.8–40.9) |
| Virginia |
1,513,000 |
584,000 |
41.1 (38.4–43.9) |
44.0 (39.2–48.9) |
| Washington |
1,346,000 |
454,000 |
36.9 (35.0–38.8) |
36.5 (33.0–40.3) |
| West Virginia |
557,000 |
223,000 |
43.7 (41.4–46.1) |
45.6 (41.9–49.3) |
| Wisconsin |
1,104,000 |
417,000 |
40.2 (37.0–43.5) |
41.0 (34.9–47.4) |
| Wyoming |
116,000 |
41,000 |
37.6 (34.2–41.1) |
36.1 (30.6–42.0) |
|
Median (Range)¶
|
|
|
40.2 (28.9–45.3)
|
41.6 (28.1–48.9)
|
| Guam |
17,000 |
7,000 |
39.3 (31.5–47.6) |
42.6 (31.9–54.1) |
| Puerto Rico | 635,000 | 215,000 | 35.6 (32.6–38.6) | 41.1 (35.3–47.2) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Body mass index ≥30; calculated from self-reported height and weight.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Median and range were calculated from estimates for the 50 states and the District of Columbia.
Activity Limitations
In 2015, for the 50 states and the District of Columbia, the median age-standardized percentage of arthritis-attributable activity limitations among adults with arthritis was 49.7% (range: 40.4% in Iowa to 59.4% in Missouri) (Table 10). The median age-standardized percentage for arthritis-attributable social participation restriction was 19.7% (range: 12.6% in Alaska to 30.4% in Arkansas) (Table 11).
TABLE 10. Unadjusted and age-standardized* percentages of arthritis-attributable activity limitations† among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | Weighted population with arthritis (rounded to 1,000s) | Weighted population with arthritis and arthritis-attributable activity limitations (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
1,248,000 |
640,000 |
56.7 (54.3–59.1) |
59.2 (55.2–63.0) |
| Alaska |
117,000 |
55,000 |
51.2 (46.2–56.1) |
51.1 (43.6–58.6) |
| Arizona |
1,222,000 |
558,000 |
52.1 (49.3–54.9) |
52.5 (46.9–58.0) |
| Arkansas |
672,000 |
345,000 |
57.0 (53.2–60.7) |
56.1 (49.4–62.5) |
| California |
5,719,000 |
2,446,000 |
49.6 (46.9–52.3) |
48.6 (44.2–52.9) |
| Colorado |
949,000 |
398,000 |
48.4 (46.0–50.8) |
47.6 (43.1–52.1) |
| Connecticut |
690,000 |
290,000 |
47.6 (45.3–49.8) |
46.7 (42.3–51.2) |
| Delaware |
207,000 |
90,000 |
47.1 (43.5–50.8) |
46.9 (39.9–54.0) |
| District of Columbia |
101,000 |
48,000 |
53.9 (48.4–59.3) |
57.0 (45.0–68.2) |
| Florida |
4,154,000 |
1,941,000 |
53.1 (50.6–55.6) |
54.5 (48.9–59.9) |
| Georgia |
1,890,000 |
882,000 |
51.9 (48.4–55.3) |
50.9 (44.1–57.6) |
| Hawaii |
211,000 |
81,000 |
42.2 (39.0–45.5) |
42.0 (36.2–48.0) |
| Idaho |
309,000 |
137,000 |
48.0 (44.8–51.2) |
50.4 (44.8–56.0) |
| Illinois |
2,308,000 |
982,000 |
46.5 (43.3–49.6) |
46.3 (40.5–52.2) |
| Indiana |
1,390,000 |
599,000 |
47.7 (44.6–50.8) |
43.7 (38.1–49.5) |
| Iowa |
619,000 |
228,000 |
40.8 (38.1–43.6) |
40.4 (34.9–46.0) |
| Kansas |
536,000 |
228,000 |
48.2 (46.7–49.7) |
46.3 (43.7–49.0) |
| Kentucky |
1,087,000 |
562,000 |
57.2 (54.3–60.0) |
57.7 (52.7–62.6) |
| Louisiana |
989,000 |
472,000 |
53.9 (50.6–57.2) |
50.6 (45.0–56.1) |
| Maine |
332,000 |
149,000 |
48.5 (46.0–50.9) |
51.2 (46.4–56.0) |
| Maryland |
1,096,000 |
405,000 |
42.2 (39.2–45.2) |
42.2 (36.3–48.4) |
| Massachusetts |
1,300,000 |
555,000 |
49.0 (46.2–51.9) |
47.0 (42.2–51.9) |
| Michigan |
2,305,000 |
1,038,000 |
48.8 (46.6–51.1) |
50.3 (46.5–54.0) |
| Minnesota |
907,000 |
393,000 |
46.7 (44.8–48.5) |
47.0 (43.3–50.6) |
| Mississippi |
647,000 |
346,000 |
56.7 (53.7–59.6) |
52.4 (47.2–57.4) |
| Missouri |
1,372,000 |
694,000 |
54.6 (51.8–57.4) |
59.4 (54.5–64.1) |
| Montana |
216,000 |
103,000 |
50.2 (47.0–53.4) |
52.0 (46.3–57.8) |
| Nebraska |
334,000 |
137,000 |
44.0 (41.9–46.1) |
44.3 (40.1–48.6) |
| Nevada |
477,000 |
212,000 |
48.7 (43.0–54.5) |
53.3 (44.2–62.3) |
| New Hampshire |
282,000 |
115,000 |
45.6 (42.8–48.3) |
49.9 (43.8–55.9) |
| New Jersey |
1,590,000 |
675,000 |
46.5 (43.8–49.3) |
47.0 (42.0–52.2) |
| New Mexico |
386,000 |
176,000 |
50.5 (47.4–53.6) |
49.2 (43.1–55.4) |
| New York |
3,629,000 |
1,503,000 |
48.3 (46.0–50.6) |
45.5 (41.2–49.9) |
| North Carolina |
2,089,000 |
1,080,000 |
55.6 (52.9–58.3) |
54.5 (49.9–59.0) |
| North Dakota |
134,000 |
57,000 |
46.3 (42.9–49.6) |
47.2 (40.5–53.9) |
| Ohio |
2,547,000 |
1,136,000 |
49.1 (46.6–51.6) |
46.6 (42.0–51.3) |
| Oklahoma |
813,000 |
419,000 |
55.9 (53.2–58.7) |
56.9 (51.9–61.7) |
| Oregon |
838,000 |
425,000 |
57.1 (54.1–60.1) |
54.0 (48.8–59.2) |
| Pennsylvania |
2,937,000 |
1,118,000 |
42.7 (39.8–45.7) |
42.1 (37.0–47.4) |
| Rhode Island |
226,000 |
89,000 |
45.1 (42.0–48.2) |
44.1 (37.6–50.7) |
| South Carolina |
1,105,000 |
555,000 |
54.8 (52.7–56.9) |
54.4 (50.3–58.4) |
| South Dakota |
158,000 |
73,000 |
48.7 (45.1–52.4) |
49.5 (42.7–56.3) |
| Tennessee |
1,630,000 |
772,000 |
53.8 (50.6–57.0) |
55.2 (49.8–60.5) |
| Texas |
4,055,000 |
1,773,000 |
50.0 (47.0–53.0) |
48.2 (43.3–53.1) |
| Utah |
407,000 |
168,000 |
45.5 (43.1–47.8) |
44.2 (40.8–47.8) |
| Vermont |
136,000 |
61,000 |
49.0 (46.2–51.9) |
48.6 (43.4–53.8) |
| Virginia |
1,513,000 |
631,000 |
44.8 (42.2–47.5) |
46.7 (41.9–51.6) |
| Washington |
1,346,000 |
657,000 |
53.3 (51.4–55.2) |
50.6 (46.6–54.5) |
| West Virginia |
557,000 |
303,000 |
57.3 (55.0–59.6) |
57.5 (53.8–61.2) |
| Wisconsin |
1,104,000 |
479,000 |
49.2 (45.9–52.7) |
50.9 (44.1–57.7) |
| Wyoming |
116,000 |
49,000 |
46.6 (43.0–50.3) |
49.7 (43.4–55.9) |
|
Median (Range)¶
|
|
|
49.0 (40.8–57.3)
|
49.7 (40.4–59.4)
|
| Guam |
17,000 |
7,000 |
43.5 (35.4–52.0) |
44.6 (33.4–56.3) |
| Puerto Rico | 635,000 | 353,000 | 57.0 (54.0–60.0) | 60.8 (54.9–66.4) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Respondents with arthritis who answered yes to the question “Arthritis can cause symptoms like pain, aching, or stiffness in or around the joint. Are you now limited in any way in any of your usual activities because of arthritis or joint symptoms?”
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Median and range were calculated from estimates for the 50 states and the District of Columbia.
TABLE 11. Unadjusted and age-standardized* percentages of arthritis-attributable social participation restriction† among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | Weighted population with arthritis (rounded to 1,000s) | Weighted population with arthritis and arthritis-attributable social participation restriction (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
1,248,000 |
321,000 |
28.5 (26.3–30.9) |
29.3 (25.8–33.0) |
| Alaska |
117,000 |
16,000 |
14.4 (11.3–18.3) |
12.6 (9.3–16.9) |
| Arizona |
1,222,000 |
212,000 |
19.7 (17.6–22.0) |
18.1 (14.8–22.1) |
| Arkansas |
672,000 |
165,000 |
27.3 (24.1–30.9) |
30.4 (24.5–37.0) |
| California |
5,719,000 |
859,000 |
17.4 (15.6–19.4) |
17.6 (14.6–21.0) |
| Colorado |
949,000 |
128,000 |
15.5 (13.7–17.4) |
16.4 (13.4–20.1) |
| Connecticut |
690,000 |
97,000 |
15.9 (14.2–17.8) |
14.5 (12.1–17.4) |
| Delaware |
207,000 |
35,000 |
18.5 (15.7–21.6) |
18.8 (13.4–25.8) |
| District of Columbia |
101,000 |
22,000 |
25.2 (20.4–30.7) |
26.8 (17.4–38.8) |
| Florida |
4,154,000 |
843,000 |
23.3 (21.1–25.6) |
25.7 (21.0–31.1) |
| Georgia |
1,890,000 |
378,000 |
22.3 (19.5–25.3) |
19.8 (15.3–25.3) |
| Hawaii |
211,000 |
26,000 |
13.4 (11.1–16.0) |
15.9 (11.4–21.7) |
| Idaho |
309,000 |
53,000 |
18.7 (16.2–21.6) |
22.4 (17.7–28.0) |
| Illinois |
2,308,000 |
365,000 |
17.4 (15.0–20.1) |
15.0 (11.7–19.0) |
| Indiana |
1,390,000 |
237,000 |
18.8 (16.6–21.4) |
20.0 (15.7–25.2) |
| Iowa |
619,000 |
83,000 |
14.9 (13.0–17.0) |
15.3 (11.6–19.9) |
| Kansas |
536,000 |
84,000 |
17.6 (16.5–18.8) |
17.6 (15.7–19.6) |
| Kentucky |
1,087,000 |
265,000 |
27.1 (24.6–29.9) |
28.3 (23.6–33.6) |
| Louisiana |
989,000 |
234,000 |
26.8 (23.9–29.8) |
25.5 (20.8–30.7) |
| Maine |
332,000 |
52,000 |
16.9 (15.1–18.9) |
21.4 (17.5–25.9) |
| Maryland |
1,096,000 |
160,000 |
16.6 (14.4–19.0) |
19.7 (14.9–25.7) |
| Massachusetts |
1,300,000 |
206,000 |
18.2 (16.1–20.6) |
20.0 (16.2–24.5) |
| Michigan |
2,305,000 |
420,000 |
19.6 (17.8–21.5) |
19.6 (16.8–22.7) |
| Minnesota |
907,000 |
136,000 |
16.1 (14.7–17.7) |
18.5 (15.5–22.0) |
| Mississippi |
647,000 |
172,000 |
28.5 (25.8–31.3) |
26.0 (22.1–30.4) |
| Missouri |
1,372,000 |
255,000 |
20.2 (18.0–22.5) |
23.4 (19.2–28.3) |
| Montana |
216,000 |
33,000 |
16.2 (13.8–18.8) |
18.6 (14.2–24.0) |
| Nebraska |
334,000 |
46,000 |
14.6 (13.2–16.2) |
12.9 (10.7–15.6) |
| Nevada |
477,000 |
98,000 |
22.7 (17.9–28.3) |
26.0 (17.6–36.6) |
| New Hampshire |
282,000 |
40,000 |
15.7 (13.8–17.9) |
20.2 (15.6–25.8) |
| New Jersey |
1,590,000 |
241,000 |
16.8 (14.9–18.9) |
18.5 (15.2–22.3) |
| New Mexico |
386,000 |
71,000 |
20.6 (18.1–23.2) |
21.0 (16.5–26.4) |
| New York |
3,629,000 |
587,000 |
19.0 (17.2–20.9) |
19.8 (16.4–23.7) |
| North Carolina |
2,089,000 |
488,000 |
25.0 (22.7–27.6) |
23.7 (20.1–27.6) |
| North Dakota |
134,000 |
18,000 |
14.7 (12.5–17.3) |
14.8 (10.8–19.9) |
| Ohio |
2,547,000 |
486,000 |
21.1 (19.1–23.2) |
19.7 (16.6–23.2) |
| Oklahoma |
813,000 |
207,000 |
27.5 (24.9–30.3) |
29.9 (25.4–34.7) |
| Oregon |
838,000 |
142,000 |
19.0 (16.6–21.6) |
19.4 (15.7–23.7) |
| Pennsylvania |
2,937,000 |
419,000 |
16.0 (13.9–18.4) |
16.8 (13.0–21.3) |
| Rhode Island |
226,000 |
39,000 |
20.0 (17.4–22.9) |
25.8 (20.0–32.6) |
| South Carolina |
1,105,000 |
245,000 |
24.2 (22.4–26.1) |
23.8 (20.5–27.5) |
| South Dakota |
158,000 |
20,000 |
13.7 (11.3–16.5) |
14.4 (9.5–21.1) |
| Tennessee |
1,630,000 |
372,000 |
26.0 (23.2–28.9) |
24.7 (20.3–29.6) |
| Texas |
4,055,000 |
739,000 |
20.8 (18.5–23.3) |
20.7 (16.9–25.2) |
| Utah |
407,000 |
58,000 |
15.6 (13.9–17.4) |
16.0 (13.6–18.8) |
| Vermont |
136,000 |
21,000 |
16.3 (14.1–18.7) |
18.9 (14.9–23.6) |
| Virginia |
1,513,000 |
251,000 |
17.8 (16.0–19.8) |
18.1 (14.9–21.9) |
| Washington |
1,346,000 |
221,000 |
17.8 (16.3–19.4) |
18.0 (15.3–21.0) |
| West Virginia |
557,000 |
140,000 |
26.7 (24.6–28.9) |
26.6 (23.5–30.0) |
| Wisconsin |
1,104,000 |
153,000 |
15.9 (13.6–18.4) |
16.6 (12.8–21.1) |
| Wyoming |
116,000 |
19,000 |
17.2 (14.3–20.6) |
19.3 (14.1–25.8) |
|
Median (Range)¶
|
|
|
18.5 (13.4–28.5)
|
19.7 (12.6–30.4)
|
| Guam |
17,000 |
2,000 |
12.7 (8.5–18.4) |
13.1 (7.7–21.5) |
| Puerto Rico | 635,000 | 144,000 | 23.2 (20.8–25.9) | 25.9 (21.2–31.2) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Respondents with arthritis who answered a lot to the question “During the past 30 days, to what extent has your arthritis or joint symptoms interfered with your normal social activities, such as going shopping, to the movies, or to religious or social gatherings?”
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Median and range were calculated from estimates for the 50 states and the District of Columbia.
Pain
In 2015, the median age-standardized percentage of arthritis-attributable severe joint pain among adults with arthritis was 29.7% (range: 20.3% in Utah to 46.0% in Mississippi) (Table 12). States with the highest age-standardized percentage of arthritis-attributable severe joint pain among adults with arthritis tended be primarily in Appalachia and in the South (Figure 4).
TABLE 12. Unadjusted and age-standardized* percentages of arthritis-attributable severe joint pain† among adults aged ≥18 years with arthritis,§ by area — Behavioral Risk Factor Surveillance System, United States, 2015.
| Area | Weighted population with arthritis (rounded to 1,000s) | Weighted population with arthritis and arthritis-attributable severe joint pain (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| Alabama |
1,248,000 |
433,000 |
39.2 (36.8–41.6) |
39.7 (35.7–43.8) |
| Alaska |
117,000 |
—¶ |
—¶ |
—¶ |
| Arizona |
1,222,000 |
328,000 |
30.6 (28.0–33.3) |
32.9 (28.0–38.2) |
| Arkansas |
672,000 |
218,000 |
36.3 (32.6–40.1) |
41.6 (35.3–48.3) |
| California |
5,719,000 |
1,510,000 |
30.2 (27.9–32.7) |
29.3 (25.8–33.0) |
| Colorado |
949,000 |
194,000 |
24.0 (21.9–26.2) |
26.2 (22.3–30.4) |
| Connecticut |
690,000 |
153,000 |
25.3 (23.3–27.4) |
25.9 (22.3–29.8) |
| Delaware |
207,000 |
57,000 |
30.8 (27.3–34.4) |
31.6 (25.2–38.7) |
| District of Columbia |
101,000 |
36,000 |
40.5 (35.0–46.3) |
36.5 (26.5–47.9) |
| Florida |
4,154,000 |
1,195,000 |
34.0 (31.5–36.6) |
38.0 (32.7–43.7) |
| Georgia |
1,890,000 |
573,000 |
34.1 (30.8–37.4) |
31.2 (25.7–37.4) |
| Hawaii |
211,000 |
41,000 |
21.7 (19.0–24.7) |
23.6 (18.9–29.2) |
| Idaho |
309,000 |
59,000 |
21.8 (19.1–24.9) |
21.9 (17.4–27.3) |
| Illinois |
2,308,000 |
576,000 |
27.4 (24.6–30.5) |
24.4 (20.2–29.3) |
| Indiana |
1,390,000 |
302,000 |
25.5 (22.8–28.4) |
26.0 (20.6–32.2) |
| Iowa |
619,000 |
122,000 |
22.3 (20.0–24.8) |
24.3 (19.7–29.6) |
| Kansas |
536,000 |
121,000 |
25.7 (24.4–27.1) |
26.2 (23.8–28.6) |
| Kentucky |
1,087,000 |
349,000 |
36.3 (33.5–39.1) |
36.7 (32.0–41.7) |
| Louisiana |
989,000 |
356,000 |
41.1 (37.8–44.4) |
41.2 (35.8–46.9) |
| Maine |
332,000 |
69,000 |
23.9 (21.6–26.3) |
30.3 (25.6–35.4) |
| Maryland |
1,096,000 |
249,000 |
26.1 (23.3–29.1) |
28.5 (22.8–35.0) |
| Massachusetts |
1,300,000 |
310,000 |
28.0 (25.4–30.8) |
28.4 (24.1–33.2) |
| Michigan |
2,305,000 |
605,000 |
28.7 (26.7–30.8) |
30.5 (27.1–34.1) |
| Minnesota |
907,000 |
181,000 |
21.8 (20.1–23.5) |
23.3 (19.9–27.1) |
| Mississippi |
647,000 |
270,000 |
45.5 (42.5–48.5) |
46.0 (40.8–51.3) |
| Missouri |
1,372,000 |
375,000 |
30.1 (27.6–32.8) |
34.0 (29.2–39.2) |
| Montana |
216,000 |
47,000 |
23.2 (20.5–26.1) |
24.3 (19.7–29.6) |
| Nebraska |
334,000 |
67,000 |
21.6 (19.9–23.5) |
22.8 (19.4–26.6) |
| Nevada |
477,000 |
130,000 |
30.6 (25.6–36.1) |
30.2 (22.3–39.3) |
| New Hampshire |
282,000 |
58,000 |
23.0 (20.7–25.6) |
26.6 (21.6–32.3) |
| New Jersey |
1,590,000 |
424,000 |
30.0 (27.5–32.6) |
33.6 (28.9–38.7) |
| New Mexico |
386,000 |
110,000 |
32.2 (29.3–35.2) |
32.7 (27.4–38.5) |
| New York |
3,629,000 |
821,000 |
30.9 (28.6–33.3) |
32.3 (27.8–37.2) |
| North Carolina |
2,089,000 |
687,000 |
35.8 (33.2–38.6) |
34.5 (30.3–38.9) |
| North Dakota |
134,000 |
21,000 |
19.2 (16.3–22.4) |
23.4 (17.8–30.2) |
| Ohio |
2,547,000 |
695,000 |
30.4 (28.1–32.8) |
30.1 (25.8–34.6) |
| Oklahoma |
813,000 |
259,000 |
35.0 (32.3–37.9) |
36.9 (32.2–41.9) |
| Oregon |
838,000 |
178,000 |
24.3 (21.6–27.2) |
25.7 (21.2–30.8) |
| Pennsylvania |
2,937,000 |
723,000 |
28.1 (25.5–30.9) |
28.7 (23.9–34.0) |
| Rhode Island |
226,000 |
59,000 |
29.9 (27.1–33.0) |
34.7 (28.6–41.4) |
| South Carolina |
1,105,000 |
361,000 |
36.1 (34.0–38.2) |
36.7 (32.9–40.7) |
| South Dakota |
158,000 |
36,000 |
24.1 (20.9–27.6) |
27.3 (21.4–34.2) |
| Tennessee |
1,630,000 |
481,000 |
34.2 (31.1–37.4) |
35.3 (30.1–40.8) |
| Texas |
4,055,000 |
1,138,000 |
33.3 (30.5–36.3) |
32.0 (27.5–36.9) |
| Utah |
407,000 |
77,000 |
21.2 (19.4–23.2) |
20.3 (17.7–23.2) |
| Vermont |
136,000 |
29,000 |
23.2 (20.8–25.9) |
25.5 (21.0–30.7) |
| Virginia |
1,513,000 |
381,000 |
27.5 (25.2–29.9) |
26.7 (23.0–30.7) |
| Washington |
1,346,000 |
282,000 |
23.0 (21.3–24.6) |
22.7 (19.6–26.1) |
| West Virginia |
557,000 |
204,000 |
39.8 (37.5–42.1) |
41.6 (37.9–45.3) |
| Wisconsin |
1,104,000 |
232,000 |
24.0 (21.3–27.0) |
23.7 (19.1–28.9) |
| Wyoming |
116,000 |
22,000 |
20.7 (17.7–24.2) |
22.7 (17.3–29.3) |
|
Median (Range)**
|
|
|
28.4 (19.2–45.5)
|
29.7 (20.3–46.0)
|
| Guam |
17,000 |
5,000 |
31.3 (24.0–39.6) |
27.0 (19.8–35.8) |
| Puerto Rico | 635,000 | 340,000 | 56.0 (52.9–59.0) | 58.2 (52.1–64.1) |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Respondents with arthritis who answered 7, 8, 9, or 10 to the question “Please think about the past 30 days, keeping in mind all of your joint pain or aching and whether or not you have taken medication. During the past 30 days, how bad was your joint pain on average? Please answer on a scale of 0 to 10 where 0 is no pain or aching and 10 is pain or aching as bad as it can be.” Severe joint pain was defined as a pain level of 7–10.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Estimates with a relative standard error ≥30% or unweighted denominator <50 were suppressed as unreliable.
** Median and range were calculated from estimates for the 50 states and the District of Columbia.
FIGURE 4.
Age-standardized prevalence of arthritis-attributable severe joint pain* among adults aged ≥18 years with arthritis, by state† — Behavioral Risk Factor Surveillance System, United States, 2015
Abbreviations: DC = District of Columbia; NA = not applicable; Q = quartile.
* Respondents with arthritis who answered 7, 8, 9, or 10 to the question “Please think about the past 30 days, keeping in mind all of your joint pain or aching and whether or not you have taken medication. During the past 30 days, how bad was your joint pain on average? Please answer on a scale of 0 to 10 where 0 is no pain or aching and 10 is pain or aching as bad as it can be.” Severe joint pain was defined as a pain level of 7–10.
† Estimate for one state (Alaska) with a relative standard error >30% or unweighted denominator <50 was suppressed as unreliable.
Arthritis Management
In 2015, among adults with arthritis in 13 states that included the BRFSS arthritis management module, the age-standardized median percentage of attendance at a self-management education course was 14.5% (range: 9.1% in New York to 19.0% in Montana) (Table 13). The median age-standardized percentage of health care provider counseling to lose weight if overweight or obese was 44.5% (range: 35.1% in Montana to 53.2% in New York) (Table 14). The age-standardized percentage of health care provider counseling for physical activity or exercise did not vary considerably among states (median: 58.5%; range: 52.3%–61.9%) (Table 15).
TABLE 13. Unadjusted* and age-standardized† percentages of adults aged ≥18 years with arthritis§ reporting they attended a self-management education course for their arthritis,¶ by selected state — Behavioral Risk Factor Surveillance System, 13 states,** 2015.
| State | No. of respondents with arthritis | Weighted population with arthritis and attendance at self-management education course (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized % (95% CI) |
|---|---|---|---|---|
| California |
2,803 |
818,000 |
15.4 (11.5–20.3) |
13.6 (9.3–19.6) |
| Kansas |
7,320 |
53,000 |
11.2 (9.9–12.7) |
11.9 (9.5–14.8) |
| Kentucky |
3,565 |
110,000 |
11.5 (9.9–13.3) |
12.2 (9.5–15.5) |
| Michigan |
3,224 |
259,000 |
12.2 (10.4–14.1) |
12.5 (9.3–16.5) |
| Minnesota |
4,666 |
116,000 |
14.2 (12.9–15.5) |
15.3 (12.7–18.4) |
| Missouri |
2,808 |
157,000 |
13.5 (11.7–15.5) |
14.5 (11.2–18.7) |
| Montana |
2,123 |
29,000 |
14.5 (12.2–17.0) |
19.0 (14.4–24.6) |
| New York |
3,921 |
323,000 |
10.6 (8.7–12.8) |
9.1 (6.9–11.9) |
| Oregon |
1,828 |
130,000 |
17.2 (13.8–21.3) |
18.1 (12.4–25.5) |
| Pennsylvania |
2,059 |
294,000 |
11.9 (10.0–14.1) |
15.1 (11.3–20.0) |
| Rhode Island |
2,244 |
21,000 |
10.8 (9.1–12.8) |
10.6 (7.7–14.4) |
| South Carolina |
4,405 |
126,000 |
12.9 (11.4–14.5) |
16.5 (13.2–20.4) |
| Utah |
2,929 |
60,000 |
16.6 (13.9–19.8) |
18.0 (13.5–23.5) |
| Median (Range)†† | 12.9 (10.6–17.2) | 14.5 (9.1–19.0) |
Abbreviation: CI = confidence interval.
* The numerator was the estimated number of adults with arthritis who reported ever having taken an educational course or class to learn to manage their arthritis. The denominator was the estimated number of adults with arthritis.
† Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Respondents who answered yes to the question “Have you ever taken an educational course or class to teach you how to manage problems related to your arthritis or joint symptoms?”
** States that administered the Behavioral Risk Factor Surveillance System (BRFSS) arthritis management module: California, Kansas, Kentucky, Michigan, Minnesota, Missouri, Montana, New York, Oregon, Pennsylvania, Rhode Island, South Carolina, and Utah.
†† Median and range were calculated from estimates for the 13 states that administered the BRFSS arthritis management module.
TABLE 14. Unadjusted* and age-standardized† percentages of overweight or obesity§ among adults aged ≥18 years with arthritis¶ reporting health care provider counseling to lose weight to help with their arthritis or joint symptoms,** by selected state — Behavioral Risk Factor Surveillance System, 13 states,†† 2015.
| State | No. of respondents with arthritis | No. of respondents who are overweight or obese | Weighted population with arthritis who are overweight or obese (rounded to 1,000s) | Weighted population with arthritis who are overweight or obese reporting counseling to lose weight (rounded to 1,000s) | Unadjusted % (95% CI) | Age-standardized %* (95% CI) |
|---|---|---|---|---|---|---|
| California |
2,803 |
504 |
5,719,000 |
1,762,000 |
48.9 (41.5–56.4) |
40.1 (30.9–50.1) |
| Kansas |
7,320 |
2,127 |
536,000 |
133,000 |
41.6 (39.0–44.1) |
39.9 (35.7–44.3) |
| Kentucky |
3,565 |
2,289 |
1,087,000 |
339,000 |
48.4 (44.9–52.0) |
52.7 (46.6–58.7) |
| Michigan |
3,224 |
1,375 |
2,305,000 |
734,000 |
48.6 (45.3–52.0) |
49.4 (43.5–55.3) |
| Minnesota |
4,666 |
2,885 |
907,000 |
246,000 |
43.0 (40.7–45.3) |
44.3 (39.7–49.0) |
| Missouri |
2,808 |
1,751 |
1,372,000 |
384,000 |
47.7 (44.4–51.0) |
49.8 (43.0–56.6) |
| Montana |
2,123 |
1,304 |
216,000 |
50,000 |
39.3 (35.6–43.0) |
35.1 (28.7–42.1) |
| New York |
39,21 |
1,112 |
3,629,000 |
1,118,000 |
52.9 (48.7–57.0) |
53.2 (45.2–61.1) |
| Oregon |
1,828 |
528 |
838,000 |
245,000 |
47.8 (42.0–53.7) |
47.5 (36.7–58.5) |
| Pennsylvania |
2,059 |
1,268 |
2,937,000 |
801,000 |
44.6 (41.1–48.2) |
42.4 (35.7–49.4) |
| Rhode Island |
2,244 |
1,271 |
226,000 |
64,000 |
49.9 (46.2–53.6) |
41.5 (34.7–48.6) |
| South Carolina |
4,405 |
2,812 |
1,105,000 |
327,000 |
46.6 (44.0–49.2) |
47.6 (42.9–52.4) |
| Utah |
2,929 |
919 |
407,000 |
114,000 |
45.6 (41.2–50.2) |
44.5 (37.6–51.5) |
| Median (Range)§§ | 47.7 (39.3–52.9) | 44.5 (35.1–53.2) |
Abbreviation: CI = confidence interval.
* The numerator was the estimated number of adults with arthritis who reported being told by their doctor to exercise or get physical activity. The denominator was the estimated number of adults with arthritis.
† Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
§ Overweight: body mass index 25.0–29.9; obese: body mass index ≥30; calculated from self-reported height and weight.
¶ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
** Respondents who were overweight or obese who answered yes to the question “Has a doctor or other health professional ever suggested losing weight to help your arthritis or joint symptoms?”
†† States that administered the Behavioral Risk Factor Surveillance System (BRFSS) arthritis management module: California, Kansas, Kentucky, Michigan, Minnesota, Missouri, Montana, New York, Oregon, Pennsylvania, Rhode Island, South Carolina, and Utah.
§§ Median and range were calculated from estimates for the 13 states that administered the BRFSS arthritis management module.
TABLE 15. Unadjusted* and age-standardized† percentages of adults aged ≥18 years with arthritis§ reporting health care provider counseling for physical activity or exercise,¶ by selected state — Behavioral Risk Factor Surveillance System, 13 states,** 2015.
| State | No. of respondents with arthritis | Weighted population with arthritis reporting counseling for physical activity or exercise (rounded to 1,000s) | Unadjusted % (95% CI) | Age standardized %* (95% CI) |
|---|---|---|---|---|
| California |
2,803 |
3,022,000 |
57.0 (50.9–62.9) |
57.8 (48.2–66.9) |
| Kansas |
7,320 |
247,000 |
52.6 (50.4–54.7) |
52.3 (48.4–56.1) |
| Kentucky |
3,565 |
514,000 |
53.8 (50.8–56.8) |
53.6 (48.3–58.8) |
| Michigan |
3,224 |
1,242,000 |
59.0 (56.2–61.7) |
61.5 (56.5–66.3) |
| Minnesota |
4,666 |
462,000 |
57.1 (55.2–59.0) |
58.1 (54.4–61.7) |
| Missouri |
2,808 |
668,000 |
57.8 (54.9–60.6) |
57.0 (51.1–62.8) |
| Montana |
2,123 |
112,000 |
55.5 (52.3–58.6) |
57.8 (52.0–63.4) |
| New York |
3,921 |
1,925,000 |
63.4 (60.1–66.5) |
61.9 (55.1–68.2) |
| Oregon |
1,828 |
445,000 |
59.6 (54.6–64.4) |
61.7 (52.9–69.9) |
| Pennsylvania |
2,059 |
1,439,000 |
58.5 (55.4–61.4) |
59.8 (54.0–65.4) |
| Rhode Island |
2,244 |
115,000 |
60.9 (57.8–63.8) |
59.6 (53.0–65.8) |
| South Carolina |
4,405 |
586,000 |
60.4 (58.3–62.6) |
61.2 (57.1–65.1) |
| Utah |
2,929 |
207,000 |
58.2 (54.4–61.8) |
58.5 (52.5–64.3) |
| Median (Range)†† | 58.2 (52.6–63.4) | 58.5 (52.3–61.9) |
Abbreviation: CI = confidence interval.
* The numerator was the estimated number of adults with arthritis who report being told by their health care provider to exercise or get physical activity. The denominator was the estimated number of adults with arthritis.
† Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
§ Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
¶ Respondents who answered yes to the question “Has a doctor or other health professional ever suggested physical activity or exercise to help your arthritis or joint symptoms?”
** States that administered the Behavioral Risk Factor Surveillance System (BRFSS) arthritis management module: California, Kansas, Kentucky, Michigan, Minnesota, Missouri, Montana, New York, Oregon, Pennsylvania, Rhode Island, South Carolina, and Utah.
†† Median and range were calculated from estimates for the 13 states that administered the BRFSS arthritis management module.
Possible State-Specific Clustering of Health-Related Characteristics
States in the highest quartile of prevalence for adults with arthritis also had the highest percentages of all seven negative health-related characteristics (arthritis-attributable activity limitations, severe joint pain, and social participation restriction; ≥14 physically unhealthy days during the past 30 days; ≥14 mentally unhealthy days during the past 30 days; obesity; and leisure-time physical inactivity) and the lowest percentages of leisure-time walking compared with states in the lower quartiles (p-trend <0.006 for all characteristics) when both linear and quadratic tests for trends were conducted (Table 16). States in the highest quartile were Maine, Pennsylvania, West Virginia, Kentucky, Tennessee, Arkansas, Missouri, Oklahoma, Louisiana, Mississippi, Alabama, South Carolina, and Michigan.
TABLE 16. Estimates of adults aged ≥18 years with arthritis and age-standardized* percentages of arthritis health-related characteristics among adults with arthritis,† by quartile§ of state-level prevalence of arthritis — Behavioral Risk Factor Surveillance System, United States, 2015.
| Estimate/Characteristic | Q1 (17.2%–21.5%) % (95% CI) | Q2 (21.5%–22.7%) % (95% CI) | Q3 (23.0%–25.4%) % (95% CI) | Q4 (25.7%–33.6%) % (95% CI) | p-trend¶ |
|---|---|---|---|---|---|
| No. of respondents with arthritis |
36,278 |
43,596 |
29,347 |
36,929 |
— |
| Weighted population with arthritis |
21,702,000 |
12,741,000 |
10,866,000 |
15,694,000 |
— |
| Arthritis-attributable activity limitations |
48.7 (46.7–50.6) |
47.8 (46.1–49.5) |
49.1 (47.1–51.2) |
52.9 (51.3–54.4) |
<0.001 |
| Arthritis-attributable severe joint pain |
31.3 (29.5–33.2) |
26.6 (25.2–28.1) |
29.5 (27.7–31.5) |
35.4 (33.9–36.8) |
<0.001 |
| Arthritis-attributable social participation restriction |
20.1 (18.5–21.8) |
17.4 (16.2–18.6) |
20.5 (18.9–22.1) |
23.7 (22.5–25.1) |
<0.001 |
|
≥14 physically unhealthy days during past 30 days |
27.3 (25.6–29.0) |
26.2 (24.7–27.7) |
27.0 (25.3–28.8) |
30.2 (28.9–31.5) |
<0.006 |
|
≥14 mentally unhealthy days during past 30 days |
22.6 (21.0–24.3) |
22.1 (20.7–23.5) |
24.0 (22.2–25.9) |
25.7 (24.4–27.1) |
0.001 |
| Obesity |
37.4 (35.6–39.3) |
39.5 (37.8–41.2) |
40.3 (38.4–42.4) |
45.0 (43.6–46.5) |
<0.001 |
| Leisure-time physical inactivity |
33.8 (32.0–35.8) |
31.4 (29.8–33.0) |
35.0 (33.0–37.0) |
38.4 (37.0–39.9) |
<0.001 |
| Leisure-time walking | 48.2 (46.3–50.1) | 49.5 (47.8–51.2) | 48.0 (46.0–50.1) | 45.1 (43.6–46.6) | 0.001 |
Abbreviations: CI = confidence interval; Q = quartile.
* Age standardized to the 2000 U.S. projected population, using three age groups: 18–44, 45–64, and ≥65 years.
† Doctor-diagnosed arthritis was defined as a yes response to the question “Has a doctor, nurse, or other health professional ever told you that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
§ Quartiles (Q1–Q4) were calculated from age-standardized prevalences of arthritis for the 50 states and the District of Columbia. Q1 (lowest): Hawaii, California, Minnesota, Texas, the District of Columbia, Nevada, New Jersey, Utah, Alaska, Nebraska, Maryland, New York, Florida, and Illinois. Q2: Virginia, North Dakota, Connecticut, Colorado, South Dakota, Arizona, Massachusetts, Wisconsin, New Mexico, Washington, and Kansas. Q3: New Hampshire, Iowa, Idaho, Vermont, Georgia, Montana, Wyoming, Rhode Island, Oregon, Delaware, North Carolina, Ohio, and Indiana. Q4 (highest): Pennsylvania, Oklahoma, Louisiana, South Carolina, Maine, Mississippi, Missouri, Michigan, Arkansas, Kentucky, Tennessee, Alabama, and West Virginia.
¶ p-value for test of linear trend in age-standardized prevalence estimates across quartiles. Bonferroni-corrected alpha level of 0.006 (α = 0.05/8) to adjust for testing multiple characteristics. Quadratic terms were applied to the test of trend to improve fit and were statistically significant at the alpha level of 0.006 for three characteristics (arthritis-attributable severe joint pain, arthritis-attributable social participation restriction, and leisure-time physical inactivity).
Discussion
This is the first report of state-level arthritis prevalence estimates. The large sample size allowed precise estimates for even limited areas and analysis of health-related characteristics and comorbidities. This report also provides model-based county-level arthritis prevalence estimates with high internal validity, which help improve understanding of arthritis disparities at a local level.
In 2015, arthritis affected approximately one in four adults in the United States overall but prevalence, including model-based estimates at the county level, varied substantially by geographic area. The percentage of negative health-related characteristics among adults with arthritis was high in every area, but also varied substantially by geographic area. Arthritis management measures by state indicated both wide variation (e.g., health care provider counseling to lose weight if overweight or obese) and moderate variation (e.g., individual report of ever attending a self-management course and health care provider counseling for exercise or physical activity). Geographic disparities exist across the United States, with arthritis having the greatest impact in southern states (e.g., West Virginia, Kentucky, Tennessee, Arkansas, Missouri, Oklahoma, Louisiana, Mississippi, Alabama, and South Carolina). More detailed estimates for each of the 50 states, the District of Columbia, Guam, and Puerto Rico, along with additional analyses not reported here are available on the CDC Arthritis Program website (https://www.cdc.gov/arthritis/data_statistics/state-data-list-current.htm).
States with greater prevalences of arthritis also had greater percentages of negative health-related characteristics (i.e., arthritis-attributable activity limitations, arthritis-attributable severe joint pain, and arthritis-attributable social participation restriction; ≥14 physically unhealthy days during the past 30 days; ≥14 mentally unhealthy days during the past 30 days; obesity; and physical inactivity) and lesser percentages of leisure-time walking (a recommended management strategy) among adults with arthritis. The reasons for this geographic clustering are unknown but suggest a greater arthritis impact among adults with arthritis who live in those states. Geographic variation in four recognized risk factors for arthritis (i.e., obesity, occupations with high physical workload, smoking, and socioeconomic status) (13–17) that are also associated with negative health consequences among adults with arthritis might account for some of the difference. Geographic variations also might exist in access to medical care, including medications, resources for physical activity, and self-management interventions. Furthermore, because those states also have greater prevalence of coronary heart disease and diabetes, two important comorbid conditions for arthritis, health care providers might focus more on treatment and management of those chronic conditions with less emphasis on treatment and management of arthritis (18).
Adults with arthritis have a complex combination of disease characteristics and negative health consequences that can limit their daily activities; reduce health-related quality of life; and contribute to sustained obesity, leisure-time physical inactivity, and lack of participation in leisure-time walking. Participation in self-management education courses among adults with arthritis remains low (19). Only half of patients with arthritis receive counseling on the self-management behaviors of physical activity and weight loss. More counseling might help reduce the proportion with arthritis reporting obesity or leisure-time physical inactivity (approximately two in five adults) (20,21). Greater use of evidence-based interventions for physical activity and self-management education could reduce pain and improve function and quality of life for all adults with arthritis (22,23).
Nationally, approximately one in four adults with arthritis reported severe joint pain in the National Health Interview Survey (4); however, the geographic variations in this report suggest that the prevalence is higher in certain states (four in 10 might experience severe joint pain). Arthritis-attributable severe joint pain can lead to poor physical function. In a cohort of retirees in the United States with arthritis, approximately three in four reported functional limitations and approximately 65% had mobility limitations (24). Poor physical function is a major risk factor linked to falls (25), and adults with arthritis are more than twice as likely to report fall injuries compared with adults without arthritis (26). In addition to decrements in physical function, adults with arthritis consistently report negative effects on health-related quality of life. One study that examined health-related quality of life measures among adults with and without arthritis found that those with arthritis had higher mean numbers of days in the prior month when physical and mental health were not good (27). In this study, approximately one in four adults with arthritis reported ≥14 physically and ≥14 mentally unhealthy days during the past 30 days.
Evidence-based interventions (https://www.cdc.gov/arthritis/interventions/index.htm) have been reported to have a positive impact on arthritis outcomes (22,23); however, interventions are underused and require more widespread dissemination. Physical activity is a proven strategy for managing arthritis symptoms and many other chronic conditions (22). For instance, a meta-analysis of community-based physical activity interventions indicated that physical activity can decrease pain and improve function by approximately 40% (22). Although persons with arthritis report typical barriers to being physically active (e.g., lack of time and lack of enjoyment), arthritis presents specific barriers (e.g., pain, functional limitations, depression, and fear of falling and injury) (28). Similarly, in a meta-analysis of self-management education interventions, participants experienced improvements of 10%–20% in confidence and skills to manage their condition and reductions in pain, fatigue, and depression (23). However, as this and other analyses illustrate, self-management education interventions are underused by adults with arthritis; nationally, only about 11% report ever having taken a course (19).
Arthritis is a common comorbid condition that might complicate the management of other chronic conditions (e.g., obesity, coronary heart disease, and diabetes), increase the negative outcomes of these conditions, and reduce quality of life (18,29). The combination of arthritis and one of these chronic conditions has been associated with higher levels of physical inactivity (30–32). Moreover, arthritis also might hinder the ability of adults with prediabetes to engage in the level of physical activity recommended to prevent diabetes (33). Counseling persons with arthritis that physical activity can improve these outcomes (e.g., lower risk for diabetes) and improving availability of safe and effective physical activity programs in their local communities can be an effective strategy for reducing physical inactivity among these groups (e.g., adults with prediabetes or other comorbid conditions).
CDC funds arthritis programs in 12 state health departments and with national partners (e.g., Young Men’s Christian Association [YMCA] and National Recreation and Park Association) to disseminate evidence-based interventions in their communities (https://www.cdc.gov/arthritis/partners/funded-states.htm). State health departments, local community-based organizations, policymakers, and others can use the estimates at the state, territory, and county levels in this report to help identify local areas with need for evidence-based interventions. For example, physical activity programs such as EnhanceFitness, Walk With Ease, and Fit & Strong! (https://www.cdc.gov/arthritis/interventions/index.htm) could be disseminated to these areas. Several CDC-funded state health departments have been successful at reaching persons with arthritis with these evidence-based programs by partnering with YMCA of the USA and local parks and recreation departments.
Limitations
The findings in this report are subject to at least seven limitations. First, arthritis was self-reported and not confirmed by a health care professional; however, this case definition has been shown to have sufficient sensitivity for public health surveillance (34). Second, because BRFSS is a cross-sectional survey, a causal relation between risk factors (e.g., obesity) and arthritis cannot be established, although robust evidence exists that links obesity to an increased risk for knee osteoarthritis (the most common form of arthritis) (14). Third, social desirability bias might have a role in certain self-reported characteristics, with underreporting of BMI (35) and overreporting of leisure-time physical activity (36). Fourth, the 2015 BRFSS median response rate was 47.2% and ranged from 33.9% to 61.1%, indicating potential nonresponse bias, although survey weights were applied to address this bias and improve external validity (27). Fifth, some of the morbidities potentially related to arthritis (e.g., physically or mentally unhealthy days) might be primarily affected by other conditions and thus might overestimate arthritis-specific impact. Sixth, the model used for county-level estimates did not account for complex sample design features, including potential geographic correlations between counties or states (i.e., observations for nearby counties and states might be clustered and therefore not independent). Finally, because county representativeness was not captured by BRFSS, model-based estimation other than direct survey estimation was used to generate prevalences at the county level. This approach has limitations that have been described elsewhere (11); however, the method has been tested through a comparison of model-based estimates with direct local survey estimates for certain other chronic conditions at the county level (37).
Conclusion
In 2015, the number of adults with arthritis continued to increase, matched projections of prevalence, and exceeded projections for arthritis-attributable activity limitations at the state level (38). The findings in this report describe the prevalence and health-related characteristics of arthritis across the United States. The findings also highlight geographic variability in these estimates, including gaps in arthritis management. Public health professionals can use this information to better understand and target evidence-based nonpharmaceutical interventions, such as arthritis self-management education and physical activity. These interventions can decrease the impact of arthritis, which in turn might help adults with arthritis better manage comorbid conditions such as obesity, coronary heart disease, and diabetes. These estimates demonstrate the need to create links in clinical and community settings that can enhance health care provider counseling for physical activity and weight loss and facilitate referrals to self-management education and physical activity interventions to address arthritis and related comorbidities.
References
- 1.Barbour KE, Helmick CG, Boring M, Brady TJ. Vital signs: prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2013–2015. MMWR Morb Mortal Wkly Rep 2017;66:246–53. 10.15585/mmwr.mm6609e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbour KE, Helmick CG, Boring M, Zhang X, Lu H, Holt JB. Prevalence of doctor-diagnosed arthritis at state and county levels—United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65:489–94. 10.15585/mmwr.mm6519a2 [DOI] [PubMed] [Google Scholar]
- 3.Boring MA, Hootman JM, Liu Y, et al. Prevalence of arthritis and arthritis-attributable activity limitation by urban-rural county classification—United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66:527–32. 10.15585/mmwr.mm6620a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barbour KE, Boring M, Helmick CG, Murphy LB, Qin J. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep 2016;65:1052–6. 10.15585/mmwr.mm6539a2 [DOI] [PubMed] [Google Scholar]
- 5.Hootman JM, Helmick CG, Barbour KE, Theis KA, Boring MA. Updated projected prevalence of self‐reported doctor‐diagnosed arthritis and arthritis‐attributable activity limitation among U.S. adults, 2015–2040. Arthritis Rheumatol 2016;68:1582–7. 10.1002/art.39692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murphy LB, Cisternas MG, Pasta DJ, Helmick CG, Yelin EH. Medical expenditures and earnings losses among US adults with arthritis in 2013. Arthritis Care Res (Hoboken) 2017. 10.1002/acr.23425 [DOI] [PubMed] [Google Scholar]
- 7.Gamble S, Mawokomatanda T, Xu F, et al. Surveillance for certain health behaviors and conditions among states and selected local areas—Behavioral Risk Factor Surveillance System, United States, 2013 and 2014. MMWR Surveill Summ 2017;66(No. SS-16). 10.15585/mmwr.ss6616a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. Self-reported frequent mental distress among adults—United States, 1993–1996. MMWR Morb Mortal Wkly Rep 1998;47:326–31. [PubMed] [Google Scholar]
- 9.Bolen J, Schieb L, Hootman JM, et al. Differences in the prevalence and severity of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis 2010;7:A64. [PMC free article] [PubMed] [Google Scholar]
- 10.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected US population. Healthy people statistical notes, no. 20. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2001. [Google Scholar]
- 11.Zhang X, Holt JB, Lu H, et al. Multilevel regression and poststratification for small-area estimation of population health outcomes: a case study of chronic obstructive pulmonary disease prevalence using the Behavioral Risk Factor Surveillance System. Am J Epidemiol 2014;179:1025–33. 10.1093/aje/kwu018 [DOI] [PubMed] [Google Scholar]
- 12.Webster BH. Income, earnings, and poverty data from the 2005 American Community Survey. Darby, PA: Diane Publishing; 2010. [Google Scholar]
- 13.Di Giuseppe D, Discacciati A, Orsini N, Wolk A. Cigarette smoking and risk of rheumatoid arthritis: a dose-response meta-analysis. Arthritis Res Ther 2014;16:R61. 10.1186/ar4498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nevitt MC. Obesity outcomes in disease management: clinical outcomes for osteoarthritis. Obes Res 2002;10(Suppl 1):33S–7S. 10.1038/oby.2002.187 [DOI] [PubMed] [Google Scholar]
- 15.Cooper C, McAlindon T, Coggon D, Egger P, Dieppe P. Occupational activity and osteoarthritis of the knee. Ann Rheum Dis 1994;53:90–3. 10.1136/ard.53.2.90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murphy LB, Moss S, Do BT, et al. Annual incidence of knee symptoms and four knee osteoarthritis outcomes in the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken) 2016;68:55–65. 10.1002/acr.22641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moss AS, Murphy LB, Helmick CG, et al. Annual incidence rates of hip symptoms and three hip OA outcomes from a U.S. population-based cohort study: the Johnston County Osteoarthritis Project. Osteoarthritis Cartilage 2016;24:1518–27. 10.1016/j.joca.2016.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Theis KA, Brady TJ, Helmick CG. No one dies of old age anymore: a coordinated approach to comorbidities and the rheumatic diseases. Arthritis Care Res (Hoboken) 2017;69:1–4. 10.1002/acr.23114 [DOI] [PubMed] [Google Scholar]
- 19.Murphy LB, Brady TJ, Boring MA, et al. Self‐management education participation among US adults with arthritis: who’s attending? Arthritis Care Res (Hoboken) 2017;69:1322–30. 10.1002/acr.23129 [DOI] [PubMed] [Google Scholar]
- 20.Barbour KE, Helmick CG, Boring M, Qin J, Pan L, Hootman JM. Obesity trends among adults with doctor‐diagnosed arthritis 2009–2014. Arthritis Care Res (Hoboken) 2017;69:376–83. 10.1002/acr.22958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy LB, Hootman JM, Boring MA, et al. Leisure time physical activity among U.S. adults with arthritis, 2008–2015. Am J Prev Med 2017;53:345–54. 10.1016/j.amepre.2017.03.017 [DOI] [PubMed] [Google Scholar]
- 22.Kelley GA, Kelley KS, Hootman JM, Jones DL. Effects of community-deliverable exercise on pain and physical function in adults with arthritis and other rheumatic diseases: a meta-analysis. Arthritis Care Res (Hoboken) 2011;63:79–93. 10.1002/acr.20347 [DOI] [PubMed] [Google Scholar]
- 23.Brady TJ, Murphy L, O’Colmain BJ, et al. A meta-analysis of health status, health behaviors, and healthcare utilization outcomes of the Chronic Disease Self-Management Program. Prev Chronic Dis 2013;10:120112. 10.5888/pcd10.120112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker NA, Barbour KE, Helmick CG, Zack MM, Al Snih S. Associations between arthritis and change in physical function in U.S. retirees. J Gerontol A Biol Sci Med Sci 2017;72:127–33. 10.1093/gerona/glw075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am 2006;90:807–24. 10.1016/j.mcna.2006.05.013 [DOI] [PubMed] [Google Scholar]
- 26.Barbour KE, Stevens JA, Helmick CG, et al. Falls and fall injuries among adults with arthritis—United States, 2012. MMWR Morb Mortal Wkly Rep 2014;63:379–83. [PMC free article] [PubMed] [Google Scholar]
- 27.Furner SE, Hootman JM, Helmick CG, Bolen J, Zack MM. Health-related quality of life of US adults with arthritis: analysis of data from the behavioral risk factor surveillance system, 2003, 2005, and 2007. Arthritis Care Res (Hoboken) 2011;63:788–99. 10.1002/acr.20430 [DOI] [PubMed] [Google Scholar]
- 28.Brittain DR, Gyurcsik NC, McElroy M, Hillard SA. General and arthritis-specific barriers to moderate physical activity in women with arthritis. Womens Health Issues 2011;21:57–63. 10.1016/j.whi.2010.07.010 [DOI] [PubMed] [Google Scholar]
- 29.Qin J, Theis KA, Barbour KE, Helmick CG, Baker NA, Brady TJ. Impact of arthritis and multiple chronic conditions on selected life domains—United States, 2013. MMWR Morb Mortal Wkly Rep 2015;64:578–82. [PMC free article] [PubMed] [Google Scholar]
- 30.Bolen J, Murphy L, Greenlund K, et al. Arthritis as a potential barrier to physical activity among adults with heart disease—United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep 2009;58:165–9. [PubMed] [Google Scholar]
- 31.CDC. Arthritis as a potential barrier to physical activity among adults with diabetes—United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep 2008;57:486–9. [PubMed] [Google Scholar]
- 32.CDC. Arthritis as a potential barrier to physical activity among adults with obesity—United States, 2007 and 2009. MMWR Morb Mortal Wkly Rep 2011;60:614–8. [PubMed] [Google Scholar]
- 33.Strauss SM, McCarthy M. Arthritis-related limitations predict insufficient physical activity in adults with prediabetes identified in the NHANES 2011–2014. Diabetes Educ 2017;43:163–70. 10.1177/0145721717691849 [DOI] [PubMed] [Google Scholar]
- 34.Sacks JJ, Harrold LR, Helmick CG, Gurwitz JH, Emani S, Yood RA. Validation of a surveillance case definition for arthritis. J Rheumatol 2005;32:340–7. [PubMed] [Google Scholar]
- 35.Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001–2006. BMC Public Health 2009;9:421. 10.1186/1471-2458-9-421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport 2000;71(Suppl 2):1–14. 10.1080/02701367.2000.11082780 [DOI] [PubMed] [Google Scholar]
- 37.Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the behavioral risk factor surveillance system. Am J Epidemiol 2015;182:127–37. 10.1093/aje/kwv002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CDC. Projected state-specific increases in self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitations—United States, 2005–2030. MMWR Morb Mortal Wkly Rep 2007;56:423–5. [PubMed] [Google Scholar]