Abstract
Background
People with serious mental illness (SMI) are at elevated risk of HIV infection, but do not receive HIV tests regularly. Inpatient psychiatric admissions provide opportunities for HIV testing.
Objective
This study retrospectively examined the impact of three sequential interventions designed to increase HIV testing on an acute inpatient psychiatry service: (1) advocacy by an administrative champion, (2) an on-site HIV counselor, and (3) a clinician championing HIV testing.
Method
Demographic and HIV testing data were extracted from hospital data systems for 11,360 admissions of HIV negative patients to an inpatient psychiatry service between 2006 and 2012. Relationships between interventions, length of stay, patient demographics and receipt of an HIV test were examined using general estimating equation methods.
Results
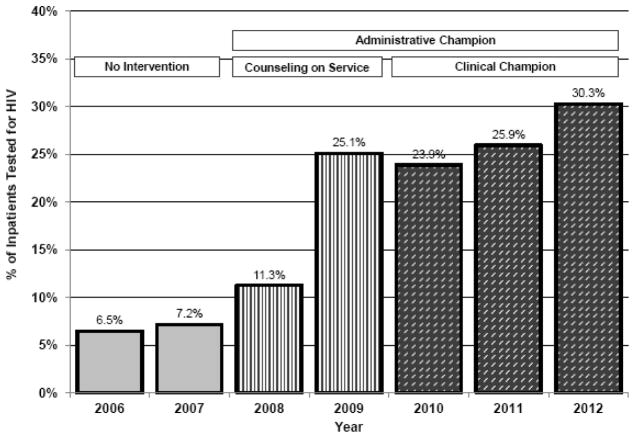
In the year prior to intervention, 7.2% of psychiatric inpatients received HIV tests. After one year of administrative advocacy, 11.2% received tests. Following the HIV counseling intervention, 25.1% of patients were tested. After the counseling intervention ended, continued administrative and clinical advocacy was associated with further increases in testing. In the final year studied, 30.3% of patients received HIV tests. Patients with shorter inpatient stays and those of Black or Asian race/ethnicity were less likely to be tested. 1.6% of HIV tests were positive.
Conclusion
Three interventions of varying intensity were associated with a fivefold increase in HIV testing on an acute inpatient psychiatry service. Nonetheless, 70% of inpatients were not tested. Continued efforts are needed to increase HIV testing in inpatient psychiatric settings.
Keywords: HIV testing, Psychiatry, Inpatient, Serious mental illness
INTRODUCTION
Since the early years of the HIV epidemic, people diagnosed with serious mental illness (SMI) have experienced an increased risk of HIV infection.[1] Currently, in the United States (US), the prevalence of HIV among people with SMI (6%) is ten times the prevalence in the general population (0.6%).[2] Rigorous analyses suggest that mental illness is not an independent risk factor for HIV infection, but that people with SMI are disproportionately impacted by well-established HIV risk factors, such as substance abuse, risky sexual behavior, homelessness, and lower socioeconomic status.[1,2,3] Recent outbreaks of HIV associated with injection of prescription opioids [4] have the potential to further increase risk of HIV infection among people with SMI because mental illness is associated with use, and misuse, of opioid medications.[5,6]
Elevated risk of infection, and the proven benefit of early intervention with antiretroviral medication among those infected [7,8], make regular HIV testing a priority for people with SMI. Recent US data document that people diagnosed with a mental illness are more likely to be tested for HIV than people not diagnosed with a mental illness, yet testing rates remain inadequate given the elevated risk of infection.[9] Analyses of California Medicaid data also document low rates of HIV testing among recipients with SMI (6.7%).[10] People with SMI often have poor access to outpatient medical care [11,12] which may limit opportunities for HIV testing. Increasing HIV testing in mental health care settings could improve testing rates and increase access to HIV care.[13,14]
Acute inpatient psychiatric admissions provide a promising opportunity for HIV testing and linkage to HIV care. In the inpatient setting, laboratory resources are readily available and HIV testing can be integrated with routine laboratory tests. Hospitalizations are typically long enough to obtain and discuss results and to arrange linkage to HIV care. However, there are also challenges associated with testing in inpatient psychiatry. Acute psychiatric symptoms limit patients’ capacity to consent to testing and to discuss results. Other clinical concerns have higher priority and inpatient clinicians often lack expertise in HIV treatment. As lengths of inpatient stays continue to decrease [15], there may be fewer opportunities to obtain and discuss results.
There is some evidence that routine HIV testing is feasible in inpatient psychiatric settings[16], yet national data from the US indicate that only 9.4% of general hospital psychiatry departments conduct HIV testing.[17] One recent study, conducted on an inpatient service in Arizona, demonstrated that modest staff education efforts and structural changes could increase HIV-testing in inpatient psychiatry; testing rates increased from 1% to 60% following a coordinated quality improvement initiative that involved tracking and prompting ordering of HIV tests using an electronic medical record.[18]
This study used existing clinical data to retrospectively evaluate the impact of three sequential, additive interventions that were designed to increase HIV testing on an inpatient psychiatry service. The first intervention was advocacy by an administrative champion, the second was providing HIV test counseling on the inpatient service, and the third was advocacy by a clinical champion.
MATERIALS AND METHODS
Participants and procedure
Demographic and HIV testing data were extracted from the clinical data system at Zuckerberg San Francisco General Hospital (ZSFG) for all admissions to the inpatient psychiatry service between January 2006 and June 2012. ZSFG is an urban safety-net hospital that is internationally recognized for its pioneering work developing models of HIV/AIDS care.[19,20] HIV-related consultation is available to all ZSFG clinicians and linkage to HIV care is available to all HIV positive patients. The ZSFG Psychiatry Department is the primary provider of emergency and acute inpatient psychiatric services for San Franciscans over age 18 and cares especially for those who are uninsured and underserved. The majority of inpatients, approximately 60%, are diagnosed with psychotic disorders; approximately 20% are diagnosed with mood disorders, 10% with bipolar disorders, and 10% with other disorders. Comorbid substance use disorders are common and a notable minority of patients, especially older adults, also suffer from co-morbid medical conditions (e.g., cardiovascular disease, hypertension, diabetes). Additionally, it is not uncommon for patients with neuropsychiatric syndromes secondary to traumatic brain injuries and occasionally other primary neurological disease (e.g., Huntington’s chorea) to be admitted to the psychiatry service. Care is not organized based on diagnosis. Specialized clinical teams target the needs of patients who are African American, Asian, Latino, female, LGBT, and HIV-positive.
During the study period, 6,175 patients had 11,931 admissions. Because HIV testing is not relevant for persons who are HIV positive, 571 admissions of persons known to be HIV positive prior to admission were excluded, leaving an analysis sample of 11,360 admissions by 5,962 patients. Over 85% of admissions were involuntary. All research procedures were approved by the Institutional Review Board at the University of California, San Francisco.
Interventions
Three interventions were sequentially implemented to meet a long range goal of increasing HIV testing on the inpatient psychiatry service. No consistent funding or other resources were available to support a sustained, programmatic quality improvement initiative; interventions were implemented as opportunities arose. The first, low intensity intervention consisted of advocacy by an administrative champion, the service chief, who began highlighting the importance of HIV testing among the SMI with the inpatient psychiatry staff. Ongoing in-service training for inpatient staff and individual consultation to inpatient leadership focused attention on the issue. Trainings focused on the epidemiology of HIV infection among people with serious mental illness, general risk factors for acquiring HIV in this population, and the public health good of early anti-retroviral therapy (ART) for people with HIV. A particular emphasis was placed on helping providers understand the dual benefits of early ART; early intervention to reduce viral load helps people with HIV live longer and healthier lives and also benefits the community by limiting potential for HIV transmission. This intervention started in January 2008 and continued throughout the study period.
The administrative champion also obtained institutional approval to modify the standard admission laboratory request form to simplify and encourage ordering of HIV tests. Before the form was changed, attending psychiatrists had remember to request an HIV test and had to write out the order; after the change, HIV testing was included on the list of recommended admission tests and they could simply check a box to include the test as part of the admission lab work. Consent procedures were updated to use an “opt-out” methodology in which patients were informed that an HIV test was being ordered along with other admission laboratory tests unless the patient had a specific wish not to be tested for HIV. This new process was implemented shortly before the second intervention was initiated and very few patients requested to opt-out of HIV testing.
A short-term grant supported the second, higher intensity intervention which consisted of adding a full-time HIV test counselor to the inpatient service from September 2008 through September 2009. The counselor provided individualized HIV test counseling sessions to patients who were receiving test results (both positive and negative) and also offered a health education group focused on HIV prevention for interested patients. The test counselor attended daily treatment team rounds and worked with the physicians to identify patients who had been tested and strategized with the treatment team on the best times to counsel the patients about their HIV results based on the patient’s clinical condition.
The third, low intensity intervention consisted of advocacy by a clinical champion who was the attending psychiatrist on the HIV-focused inpatient psychiatry team. From July 2010 through June 2012, the clinical champion worked with inpatient staff to increase HIV testing of all newly admitted patients. The clinical champion set an example for other psychiatrists by ordering HIV test for all his patients, raisied questions related to HIV risk and treatment during treatment team discussions, and generally served as the model of a physician who was concerned about his patients’ physical health as well as their mental health.
Data analysis
Descriptive statistics were computed for all variables. A generalized estimating equation (GEE) model (SAS PROC GENMOD), which accounts for multiple admissions per patient, was used to examine the relationship of the three interventions, length of stay, and patient demographics to receipt of an HIV test during each admission. Dichotomous indicators were created for each of the three interventions and coded as 1 if an admission occurred when the intervention was in effect and as 0 when the intervention was not in effect. Patient demographics included gender (male and female), race/ethnicity (Asian, Black, Hispanic/Latino, White, and Other), and age. The number of positive HIV tests was also examined, but was too small for GEE modeling, therefore the Cochran-Armitage trend test was used to examine the rate of positive tests over time.
RESULTS
Admission and patient characteristics
Between January 2006 and June 2012 there were 11,360 admissions of 5,962 unique HIV negative patients. On average there were 1,728 such admissions per year. The mean length of stay was 12.46 days (sd=16.55). Patients ranged in age from 18 to 94, with a mean age of 42.91 (sd=14.44). Sixty-two percent (3,583) were male. Patients were racially and ethnically diverse (15.9% (945) Asian, 21.8% (1,299) Black, 10.8% (645) Latino, 43% (2,566) White, 8.5% (507) of other race/ethnicities).
Impact of interventions and characteristics of admissions and patients on HIV testing
Prior to intervention, 6.5% of inpatients were tested in 2006 and 7.2% were tested in 2007. As illustrated in Figure 1, all three interventions were associated with statistically significant increases in HIV testing relative to the two pre-intervention years. The most intensive intervention, having an HIV test counselor on the inpatient service, had the largest impact on testing (Z=6.14, p<.0001). In 2009, when the 13-month counseling intervention ended, 25.1% of patients were tested, a statistically significant increase from 2007 (Z=14.02, p<.0001). The two lower intensity interventions, the administrative champion (Z=12.22, p<.0001) and the clinical champion (Z=8.73, p<.0001), were also associated with increases in testing. Advocacy by the administrative and clinical champions was associated with continued increases in testing after the counseling intervention ended. In 2012, 30.3% of patients were tested, a 5.2% increase over 2009 (z=2.70, p=.007).
Figure 1.
Percentage of Psychiatric Inpatients Tested for HIV: 2006–2012
HIV tests were completed more frequently during longer admissions (Z=7.83, p<.0001). White patients were more likely to be tested than Asian patients (OR=1.21, p=.02) or Black patients (OR=1.25, p=.002). Gender was not associated with HIV testing. None of the two-way interactions between patient characteristics and the three interventions were statistically significant which suggests that none of the interventions differentially impacted demographic subgroups of patients.
During the study period, 31 (1.6%) of the 1,903 conducted HIV tests were positive. As the total number of tests increased, there was a trend towards a decrease in the proportion of positive tests (Z=1.87, p=.06). The highest percentage of positive tests was detected in 2009 (3.1%) and the lowest percentage in 2011 (0.5%).
DISCUSSION
Retrospective evaluation of three sequential, additive interventions to increase HIV testing on an inpatient psychiatry service in an urban general hospital yielded both encouraging and discouraging findings. It is encouraging that the percentage of inpatients tested increased from 7.2% to 25.1%, more than a 3-fold increase, after an HIV test counselor was integrated into inpatient care for thirteen months. It is also encouraging that these gains were maintained and that testing levels increased further during three years of two low intensity and low cost interventions--advocacy by administrative and clinical champions. Cumulatively, the three interventions were associated with almost a 5-fold increase in testing rates from 6.5% in 2006 to 30.1% in 2012.
At the same time, it is discouraging that HIV testing was not completed during 70% of inpatient admissions. In the studied inpatient setting it appears that two key barriers remain. The first is that over 85% of patients are admitted involuntarily for up to 72 hours of observation because they pose a risk to themselves or others. In the study sample, 23.7% of admissions lasted 72 hours or less. HIV tests were less likely to be completed during admissions lasting 72 hours or less (13%) than during longer admissions (17%) (OR=.72, p<.0001). The clinical complexities of short, acute, involuntary hospitalizations may limit opportunities to increase HIV testing rates in this subgroup of patients in the studied setting and in other inpatient settings where brief admissions are common. Efforts to increase HIV testing among patients who are hospitalized very briefly may not be appropriate if patients are likely to be discharged before test results can be discussed.
The second barrier in the studied setting is that many patients refused to have blood drawn. In this setting, HIV testing is conducted using an “opt out” model in which patients are informed that an HIV test is a standard part of admission blood work and will be performed unless the patient requests that the test not be done. Few patients specifically refused HIV testing, but many refused to have any blood drawn. Some of these refusals were clearly related to acute psychiatric symptoms and some refusals were in response to involuntary admission which tends to reduce patients’ interest in complying with requests of any kind. It is likely that these types of refusals are common across inpatient settings. These refusals are problematic in the studied inpatient psychiatry service because there are no systems to notify clinicians about laboratory tests that were missed at admission (either not ordered or ordered but not completed) so that they can follow-up with patients to complete tests at a later time. Weller and colleagues [18] reported that reminders built into the electronic medical record could be helpful in engaging both physicians and nurses on an inpatient psychiatry service in completing HIV tests. As electronic medical record systems become more sophisticated and widely used, such reminders have considerable potential to increase HIV testing.
The finding that Black patients were less likely than White patients to receive HIV tests is a potential cause for concern. In the general US population, Blacks, who make 13% of the US population,[21] are disproportionately affected by HIV, accounting for 41% of persons living with HIV and 44% of new HIV diagnoses[22]. It is likely that Black persons with SMI are also at heightened risk and it appears that extra effort is needed to insure that these patients are included in inpatient HIV testing. It is worth noting that this specific racial disparity was not observed in a California Medicaid population during the same study period [10].
The finding that Asian patients were less likely to be tested is consistent with published studies documenting that cultural factors common to multiple Asian ethnic groups often limit willingness to provide blood samples.[23] Some patients hold traditional Confucian beliefs related to the loss of blood negatively impacting “Qi” or “life energy.”[24] In the inpatient psychiatric setting, it is not uncommon for patients to integrate traditional beliefs with their personal delusional beliefs. Thus, it is important for culturally informed clinicians to discuss blood draws with Asian patients who initially refuse them.
In considering strategies to increase HIV testing in inpatient psychiatric settings, it is important to consider whether patients can be effectively linked to appropriate HIV care. In the setting where these data were collected, specialized services are available to assist with starting HIV medications in the hospital and to provide supportive linkage to outpatient HIV care. Increasing HIV testing may not be in patients’ best interest if it is not possible to complete referrals to outpatient HIV services during the hospital stay.
This retrospective, observational study is limited in several respects. Analyses were based on administrative data that lack the precision and detail that specifically designed prospective evaluation data would provide. Data also came from a single inpatient psychiatry service in a major urban area. The three interventions overlapped and their individual impact cannot be determined. Also, several years have passed since the study data were collected. Nonetheless, recent evidence documenting consistently elevated risk of HIV infection among persons with SMI [2] and low rates of testing [9,10] highlights the importance of additional efforts to improve HIV testing in mental health settings.
CONCLUSIONS
The results reported here underscore the importance of implementing and evaluating interventions to increase HIV testing among people with SMI in inpatient psychiatric care. The CDC has long recommended routine testing in inpatient settings with an HIV seroprevalence rate of at least 1%.[25] The seroprevalence rate on the studied inpatient psychiatry service was 1.6%, indicating that continued efforts to increase HIV testing are needed. The findings suggest that interventions of varying intensity can meaningfully increase the rate of HIV testing on an inpatient psychiatry service. The three interventions examined--integrating an HIV test counselor into the inpatient service and advocacy by administrative and clinical champions--are generalizable and flexible and could be implemented and prospectively evaluated in diverse inpatient psychiatric settings. The findings also highlight the challenges of HIV testing in the complex context of inpatient psychiatric care. Continued effort is needed to identify additional strategies to improve the rate of HIV testing in inpatient settings.
Footnotes
Disclosure: Dr. Mangurian’s effort was supported in part by National Institutes of Health grant K23 MH093689 and by a UCSF Hellman Fellows Award for Early-Career Faculty. Dr. Momenzadeh’s effort was supported in part by National Institutes of Health grant R25MD006832. The other authors have no disclosures or conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hobkirk AL, Tow SI, Lion R, Meade CS. Primary and secondary HIV prevention among persons with severe mental illness: recent findings. Curr HIV/AIDS Rep. 2015;12:406–412. doi: 10.1007/s11904-015-0294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hughes E, Bassi S, Gilbody S, Bland M, Martin F. Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:40–8. doi: 10.1016/S2215-0366(15)00357-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helleberg M, Pedersen MG, Pedersen CB, Mortensen PB, Obel N. Associations between HIV and schizophrenia and their effect on HIV treatment outcomes: a nationwide population-based cohort study in Denmark. Lancet HIV. 2015;2:e344–50. doi: 10.1016/S2352-3018(15)00089-2. [DOI] [PubMed] [Google Scholar]
- 4.Peters PJ, Pontones P, Hoover KW, Patel MR, Galang RR, Shields J, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med. 2016;375:229–39. doi: 10.1056/NEJMoa1515195. [DOI] [PubMed] [Google Scholar]
- 5.Cochran G, Hruschak V, Bacci JL, Hohmeier KC, Tarter R. Behavioral, mental, and physical health characteristics and opioid medication misuse among community pharmacy patients: a latent class analysis. Res Social Adm Pharm. 2016 doi: 10.1016/j.sapharm.2016.11.005. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davis MA, Lin LA, Liu H, Sites BD. Prescription opioid use among adults with mental health disorders in the United States. J Am Board Fam Med. 2017;30:407–17. doi: 10.3122/jabfm.2017.04.170112. [DOI] [PubMed] [Google Scholar]
- 7.Geretti AM, Tsakiroglou M. HIV: New drugs, new guidelines. Curr Opin Infect Dis. 2014;27:545–53. doi: 10.1097/QCO.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 8.INSIGHT START Study Group. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373:795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yehia BR, Cui W, Thompson WW, Zack MM, McKnight-Eily L, DiNenno E, et al. HIV testing among adults with mental illness in the United States. AIDS Patient Care STDS. 2014;28:628–34. doi: 10.1089/apc.2014.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mangurian C, Cournos F, Schillinger D, Vittinghoff E, Creasman JM, Lee B, et al. Low rates of HIV testing among adults with severe mental illness receiving care in community mental health settings. Psychiatr Serv. 2017;68:443–448. doi: 10.1176/appi.ps.201600248. [DOI] [PubMed] [Google Scholar]
- 11.Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatr Scand. 2008;118:169–71. doi: 10.1111/j.1600-0447.2008.01211.x. [DOI] [PubMed] [Google Scholar]
- 12.Swildens W, Termoreshuizen F, de Ridder A, Smeets H, Engelhard IM. Somatic care with a psychotic disorder. lower somatic health care utilization of patients with a psychotic disorder compared to other patient groups and to controls without a psychiatric diagnosis. Adm Policy Ment Health. 2016;43:650–62. doi: 10.1007/s10488-015-0679-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hilton C, Cohen A, Geoghegan F. HIV testing is needed in mental health settings. BMJ. 2014:349. doi: 10.1136/bmj.g4841. [DOI] [PubMed] [Google Scholar]
- 14.Biradavolu M, Jia Y, Withers K, Kapetanovic S. Factors influence the delivery of HIV-related services to severely mentally ill individuals: the provider’s perspective. Psychosomatics. 2016;57:64–70. doi: 10.1016/j.psym.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tulloch AD, Fearon P, David AS. Length of stay of general psychiatric inpatients in the united states: systematic review. Adm Policy Ment Health. 2011;38:155–168. doi: 10.1007/s10488-010-0310-3. [DOI] [PubMed] [Google Scholar]
- 16.Sanger C, Hayward J, Patel G, Phekoo K, Poots AJ, Howe C, et al. Acceptability and necessity of HIV and other blood-borne virus testing in a psychiatric setting. Br J Psychiatry. 2013;202:307–8. doi: 10.1192/bjp.bp.112.119529. [DOI] [PubMed] [Google Scholar]
- 17.Voetsch AC, Heffelfinger JD, Yonek J, Patel P, Ethridge SF, Torres GW, et al. HIV screening practices in U.S. hospitals, 2009–2010. Public Health Rep. 2012;127:524–31. doi: 10.1177/003335491212700508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weller J, Levitt G, Myers R, Riley A, Gesmundo CK. Challenges in obtaining HIV testing in an acute involuntary inpatient psychiatric setting. J Assoc Nurses AIDS Care. 2016;27:648–53. doi: 10.1016/j.jana.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 19.Silverman M. AIDS care: the San Francisco model. J Ambul Care Manage. 1988;11:14–8. doi: 10.1097/00004479-198805000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Dilley JW. Implications for the San Francisco model of care. AIDS Care. 1990;2:349–52. doi: 10.1080/09540129008257751. [DOI] [PubMed] [Google Scholar]
- 21.United States Census Bureau. [Accessed 9/24/17]; https://www.census.gov/quickfacts/fact/table/US/PST045216.
- 22.Centers for Disease Control and Prevention. [Accessed 1/2/2017];HIV Surveillance Report. 2014 26 http://www.cdc.gov/hiv/library/reports/surveillance/. Published November 2015. [Google Scholar]
- 23.Gao W, Ma GX, Tan Y, Fang C, Weaver J, Jin M, et al. Culturally appropriate education intervention on biospecimen research participation among Chinese Americans. Cancer Epidemiol Biomarkers Prev. 2014;23:383–91. doi: 10.1158/1055-9965.EPI-13-0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tison GH, Liu C, Ren F, Nelson K, Shan H. Influences of general and traditional Chinese beliefs on the decision to donate blood among employer-organized and volunteer donors in Beijing, China. Transfusion. 2007;47:1871–9. doi: 10.1111/j.1537-2995.2007.01410.x. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Recommendations for HIV testing services and outpatients in acute-care hospital settings and technical guidance on HIV counseling. MMWR. 1993;42(RR- 2) [PubMed] [Google Scholar]