Abstract
Young children are at significant risk of exposure to intimate partner violence (IPV), and vulnerable to exposure-related psychopathology, yet few studies investigate the effects of exposure to IPV on children under the age of 5 years. The current study investigated the role of maternal PTSD symptoms and parenting strategies in the relationship between mothers’ IPV experiences and psychopathology in their young children, ages 3 to 6 years in a community-based cohort of 308 mother-child dyads at high risk for family violence. Data were collected from 2011 to 2014. IPV history and maternal PTSD symptoms were assessed by self-report questionnaires. Children’s symptoms were assessed with a developmentally-sensitive psychiatric interview administered to mothers. Punitive/restrictive parenting was independently-coded from in-depth interviews with mothers about their disciplinary practices. Hypothesized direct and indirect pathways between physical and psychological IPV, maternal PTSD, maternal parenting style, and children’s internalizing and externalizing symptoms were examined with mediation models. Results indicated that neither physical nor psychological IPV experienced by mothers was directly associated with children’s symptoms. However, both types of victimization were associated with maternal PTSD symptoms. Examination of indirect pathways suggested that maternal PTSD symptoms mediated the relationship between mothers’ psychological and physical IPV experiences and children’s internalizing and externalizing symptoms and mothers’ restrictive/punitive parenting mediated the relationship between mothers’ psychological IPV and children’s externalizing symptoms. In addition, there was a path from maternal physical IPV to child externalizing symptoms through both maternal PTSD symptoms and restrictive/punitive parenting. Findings highlight the importance of supporting parents in recovering from the sequelae of their own traumatic experiences, as their ensuing mental health symptoms and parenting behaviors may have a significant impact on their children’s emotional health.
Keywords: intimate partner violence, parenting style, posttraumatic stress disorder, early childhood, developmental psychopathology
Introduction
It’s estimated that 29% of children and adolescents in the U.S. live in homes where physical intimate partner violence (IPV) has occurred, and an estimated 12% of young children (up to age 5 years) have directly witnessed physical violence between adults in their home (Hamby, Finkelhor, Turner, & Ormrod, 2011; McDonald, Jouriles, Ramisetty-Mikler, Caetano, & Green, 2006). Rates are even higher when IPV is broadly defined to include families experiencing verbal or psychological aggression (McDonald, Jouriles, Briggs-Gowan, Rosenfield, & Carter, 2007).
That IPV has adverse effects on children is well-recognized. However, the specificity of IPV’s effects on children’s exposure-related psychopathology is not clear. Numerous studies have found associations between IPV exposure and externalizing behavior, traumatic stress, internalizing problems, and social problems in children. However, there is substantial variation in findings across studies with respect to the types of symptoms that are associated with IPV and the types of IPV that appear to be most predictive (Evans, Davies, & DiLillo, 2008; Graham-Bermann & Levendosky, 1998; Grasso et al., 2016; Gustafsson, Coffman, & Cox, 2015; Kitzmann, Gaylord, Holt, & Kenny, 2003; Olaya, Expeleta, de la Osa, Granero, & Domenech, 2010). This is perhaps due, in part, to a number of methodological issues. First, there is little consistency among studies on how IPV is defined, with many studies assessing solely physical violence, and others utilizing a broader, composite definition that includes psychological aggression. Associations of IPV exposure with internalizing and externalizing symptoms in children are stronger when IPV is defined broadly to include multiple facets of exposure (Vu, Jouriles, McDonald, & Rosenfield, 2016), suggesting that the impact of other types of violence may be important factors to consider. In particular, psychological IPV has been demonstrated to have effects that are independent of physical IPV on maternal mental health (Coker et al., 2002; Lawrence, Yoon, Langer, & Ro, 2009; Nathanson, Shorey, Tirone, & Rhatigan, 2012; Pico-Alfonso, 2005), yet psychological IPV exposure’s unique contribution to children’s adjustment has rarely been examined. The current study will investigate the impact of physical and psychological IPV, offering novel insight into their contributions to women’s mental health, parenting, and children’s symptoms.
Further, while much of the extant research examines the effects of exposure to IPV in school age and adolescent youth, few studies have investigated these processes in young children. The small body of studies that exist suggests that young children are at greater risk of exposure to IPV due to their disproportionate representation in households experiencing physical aggression (Fantuzzo, Boruch, Beriama, Atkins, & Marcus, 1997), and that they may be equally or more vulnerable to IPV’s impact, compared to older children (Evans et al., 2008; Kitzmann et al., 2003; Yates, Dodds, Sroufe, & Egeland, 2003). The limited amount of young child research in this area is likely in part due to challenges distinguishing clinically-significant mental health problems from normative variation in this developmental period (Wakschlag et al., 2007). Consideration of severity, developmental timing, and social context are critical to differentiating among normative patterns, transient problems, and behaviors of clinical concern in young children (Campbell, 2015; Wakschlag et al., 2007). In this study, preschool psychopathology will be assessed with a developmentally-sensitive semi-structured interview.
In addition to these gaps, little is known about the mechanisms by which exposure to IPV affects young children’s development. Understanding and identifying young children’s exposure-related psychopathology at an early age, before problems become entrenched, is critical. While the fear and distress elicited by witnessing violence may directly affect young children’s sense of safety and emotional well-being, e.g. via hypervigilance or dysregulation (Davies & Cummings, 1994), it is also likely that there are substantial indirect effects that exacerbate, and/or buffer the effect of IPV exposure on mental health problems in young children in violent homes. In particular, IPV experiences may negatively impact maternal mental health (e.g., PTSD) and parenting behaviors, which are well-established influences on children’s health and developmental outcomes (Levendosky & Graham-Bermann, 2001).
PTSD is one of the most common mental health diagnoses among women who are victims of IPV (Becker, Stuewig, & McCloskey, 2010; Nathanson et al., 2012), with rates among women who have experienced IPV ranging from 16.3 to 57.4 % (Ahlfs-Dunn & Huth-Bocks, 2014). Both physical and psychological forms of IPV have been linked with PTSD (Becker et al., 2010; Pico-Alfonso, 2005), with some studies suggesting that psychological aggression may have a stronger effect on PTSD symptoms than physical aggression (Pico-Alfonso, 2005; Street & Arias, 2001). Further, children with parents who are experiencing PTSD symptoms are at greater risk for emotion regulation difficulties, anxiety, depression, and disruptive behavior, even when the children have not been exposed to the traumatic event (for a review, see Leen-Feldner et al., 2013). When children of adults with PTSD are exposed to trauma, they are more likely to develop posttraumatic stress reactions themselves (Leen-Feldner et al., 2013). Although most of this research has been conducted with school aged and adolescent children, studies with young children have found consistent results (Chemtob et al., 2010; Enlow et al., 2011).
Despite the significant effect that parental PTSD has on children, few studies have examined its moderating or mediating role on emotional and behavioral outcomes for young children in the context of IPV. In one such study of mothers and their preschool aged children, severity of maternal posttraumatic stress symptoms partially mediated the relationship between paternal physical violence toward the mother and preschool children’s posttraumatic stress and externalizing symptoms (Schechter et al., 2011). Psychological IPV was not assessed in this study, and children’s internalizing symptoms were not associated with paternal violence, but were moderately predicted by maternal posttraumatic stress symptoms.
One potential pathway through which parental PTSD may affect children’s wellbeing is parenting. The presence of posttraumatic stress symptoms can interfere with positive parenting behaviors, modelling of regulated emotions and responding effectively to their children, and reactivity to stress resulting from traumatic experiences may lead to increased use of harsh, maladaptive or physically aggressive parenting strategies (Ammerman, Putnam, Chard, Stevens, & Van Ginkel, 2012; Chemtob & Carlson, 2004; Gewirtz, Polusny, DeGarmo, Khaylis, & Erbes, 2010; Katz & Gurtovenko, 2015; Lauterbach et al., 2007; Leen-Feldner, Feldner, Bunaciu, & Blumenthal, 2011; Sherman, Smith, Straits-Troster, Larsen, & Gewirtz, 2016). Although only two of these studies focused on parents of young children, the results are consistent with those of the larger literature in linking PTSD symptoms with harsh/reactive parenting (Ammerman et al.., 2012; Chemtob & Carlson, 2004) as well as insensitivity to infant cues (Ammerman et al., 2012).
The research examining the relationship between maternal IPV experiences and parenting behaviors is inconsistent, and largely focuses on the effects of physical IPV. A number of studies have reported a substantially increased risk for physically abusive parenting among mothers within domestically violent families, with rates ranging from 11–46% (for a review, see Jouriles, McDonald, Slep, Heyman, & Garrido, 2008). In a longitudinal study, Huang and colleagues (2015) found a dose effect such that the more physical violence the mothers experienced when the child was a toddler, the more likely they were to engage in physical punishment of the child at 5 years of age. Although less frequently examined within this context, other forms of compromised parenting – including neglectful, rejecting, harsh, and psychologically aggressive parenting – are also more prevalent among mothers of children (from preschool through adolescence) who have experienced physical IPV (Banyard, Williams, & Siegel, 2003; Gustafsson, Cox, & Blair, 2012; Huang et al., 2015; Kelleher et al., 2008; Olaya et al., 2010), and are likewise associated with poor outcomes for children (de la Vega, de la Osa, Granero, & Ezpeleta, 2013; Schwerdtfeger, Larzelere, Werner, Peters, & Oliver, 2013).
However, not all investigations support the relationship between domestic violence and abusive, harsh or neglectful parenting. Indeed, positive parenting has been found to buffer the effects of combined physical and psychological IPV exposure on children (Levendosky, Huth-Bocks, Shapiro, & Semel, 2003; Miller-Graff, Cater, Howell, & Graham-Bermann, 2016). Graham-Bermann, Gruber, Howell, and Girz (2009), for example, found that parental warmth and effective parenting behaviors (such as the use of limit-setting and appropriate discipline) differentiated resilient children from those with more social and emotional problems among school-aged children exposed to physical violence and threats of violence toward their mothers. Likewise, Greeson et al. (2014) found a protective effect of parenting behaviors that were characterized by warmth, firmness, and acceptance, with authoritative parenting mediating the relationship between physical IPV and later child externalizing problems. In the current study, parenting style was examined on a continuum from non-punitive/authoritative to punitive/restrictive based on independent coding of mothers’ reports in an in-depth interview.
Pathways between IPV and both problematic and supportive parenting behaviors also may be explained or influenced by other maternal factors. Given PTSD’s association with both IPV and parenting, its role as a potential mediator is worth investigating. Loucks and Shaffer (2014), for example, found that parenting stress mediated the relationship between a combined measure of physical, psychological, and sexual IPV and emotionally unsupportive parenting behavior among mothers of school-aged children. That is, higher levels of IPV were associated with increased parenting stress, which in turn, was associated with the greater use of emotionally unsupportive parenting behaviors. While parenting stress reflects emotional distress specific to the parenting role, it tends to correlate with other indicators of maternal psychological functioning, such as depression and PTSD (Ammerman et al., 2012; Salloum, Stover, Swaidan, & Storch, 2015). Thus, it stands to reason that stress reactivity associated with posttraumatic stress may affect a mother’s ability to provide sensitive parenting to her children. Among young children, a series of studies conducted by Levendosky and colleagues (2001; 2003) further suggests the role of maternal mental health in the relationship between IPV and varied aspects of parenting. In these investigations, a combined measure of maternal depression and PTSD symptoms partially mediated the impact of broadly measured IPV on parenting behaviors.
In the current study we utilize several serial mediation models to examine the role of maternal PTSD symptoms and parenting strategies in the relationship between mothers’ intimate partner violence experiences and the internalizing and externalizing problems of their young children in a community-based cohort at high risk for family violence. Our primary hypotheses are that (1) both maternal posttraumatic stress symptoms and restrictive/punitive parenting behaviors will be associated with children’s internalizing and externalizing problems, (2) maternal physical and psychological IPV experiences each will be associated with maternal PTSD, restrictive/punitive parenting, and children’s internalizing and externalizing symptoms, and (3) there will be an indirect pathway from mothers’ IPV experiences to their children’s mental health problems through mothers’ posttraumatic stress symptoms and their parenting strategies. More specifically, physical and psychological IPV will be each directly associated with mothers’ PTSD; mothers’ PTSD will be associated with increased use of restrictive/punitive parenting strategies, which will in turn be associated with increased risk of child internalizing and externalizing symptoms. Such indirect pathways would suggest that mothers’ PTSD symptoms and parenting strategies might function as mediators.
Method
Participants
The current study’s participants were part of an enriched sub-study of 497 families recruited by stratified random sampling of a survey sample of 1,857 3–5 year olds in the Multidimensional Assessment of Preschoolers (MAPS) Study originally recruited from pediatric practices (Wakschlag et al., 2014). Participants were restricted to children with no significant cognitive delays or neurocognitive conditions and English-speaking children and mothers. As the goal of the sub-study was to investigate behavioral and environmental risk for psychopathology, families were oversampled based on past-year intimate partner violence (IPV) or elevated child disruptive behavior (44% of selected sample were high on disruptive behavior and 23% reported past year IPV). For further details about this sampling, please see Nichols et al. (2015).
The analytic sample for the current study consists of 308 mothers who completed two lab visits in which child psychiatric interviews, family violence, parenting and maternal symptoms were assessed, had a partner about whom they completed an IPV measure, and had complete data for key study measures used in analyses. This analytic sample was evenly distributed by sex (52% boys) and diverse with respect to household income (46% poverty) and child’s race/ethnicity (47% African American/Black, 30% Hispanic, 21% non-Hispanic Caucasian/White and 2% other). Mean maternal age at the birth of the target child was 26.1 years (SD = 6.0, range, 15–42). Mean child age was 55.4 months (SD =10.2). This analytic sample was comparable to the excluded 189 families in terms of child sex, respondent education, employment status, poverty, minority ethnicity, and rates of MAP-DB disruptive behavior scores (p>.10). However, the children in the analytic sample were slightly younger than those without partner data [Mean = 60.2 months (SD=11.2), t=4.93, p<.001].
Procedures
Participants attended two laboratory visits between 2011 and 2014 that included maternal interviews and questionnaires to assess children’s mental health, family environment, and child-rearing practices. Mothers were compensated for participation and transportation, and they provided informed consent. Study protocols were approved by two institutional review boards. Mandated child abuse and neglect reporting procedures were followed, with 4 reports of suspected maltreatment made to Child Protective Services over the course of the study. All mothers were given parenting resource and referral information at the end of the visit, and additional consultative follow-up was provided for families in distress.
Measures
Intimate partner violence
The Revised Conflict Tactics Scale (CTS-2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996) measured the presence and chronicity (i.e., Never, Once, Twice, 3–5 Times, 6–10 Times, 11–20 Times,) of the caregiver’s victimization of psychological and physical violence by her partner during the 12 months prior to the interview. Past year psychological and physical IPV severity scores, calculated as the sums of item frequency ratings within each scale, were used in analyses (α= 0.74 and 0.91, respectively).
Maternal PTSD symptoms
Maternal PTSD symptoms were assessed with the PTSD Checklist civilian version (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993). Mothers rated how much they have been bothered by that problem in the past month (0 = Not at All, 1 =A Little Bit, 2 = Moderately, 3 = Quite a Bit, 4 = Extremely). A total PTSD symptom score was calculated as the sum of all 17 items (α= 0.92).
Parenting
The Family Socialization Interview –Revised (FSI-R) is a semi-structured interview designed to obtain a history of family life stress and child-rearing practices from the child’s birth to the present, with established reliability and validity (O'Dor et al., 2017). The FSI-R takes approximately 60 minutes. The interview begins with questions about the child’s disposition and about household composition, followed by sections focused on family stressors, parenting and conflict from birth to the past year and in the past year. The FSI-R employs open-ended questions and probes to gather information about the methods of discipline used, both positive and harsh. Querying is designed to elicit descriptions of the methods used typically and the methods used when episodes are more intense or extreme. Querying was designed to elicit detailed information about the use of mild to severe forms of verbal and psychological discipline (e.g., raised voice, yelling, screaming, use of insults), as well as mild to severe forms of physical discipline (e.g., swatting, spanking with an open hand, hitting with an object). Videotaped interviews were coded by trained interviewers, with 20% reliability monitored throughout the coding process and bi-weekly consensus meetings to maintain reliability.
Restrictive/Punitive parenting was coded based on all of the information obtained from the discussion of discipline methods, including descriptions about the severity and frequency of psychological and physical forms of discipline. Restrictive/Punitive Parenting was coded on a five-point scale where 0 reflects authoritative/non-punitive methods and characterizes a mother who is often authoritative and addresses misbehavior with controlled and appropriate, non-physical punishments. A rating of 4 indicates restrictive/punitive methods and characterizes a mother who is highly punitive and enforces strict obedience. This code has demonstrated acceptable inter-rater reliability (Weighted Kappa = .77) and its validity is supported by significant associations with other indicators of harsh/punitive parenting (O'Dor et al., 2017).
Child psychiatric symptoms
During the laboratory visits, parents completed the Preschool-Age Psychiatric Assessment (PAPA; Egger et al., 2006), a semi-structured diagnostic interview about the child’s psychiatric symptoms. The interview asks about the presence and frequency of symptoms in the past three months. All interviews were administered by trained research assistants. Twenty percent of interviews were reviewed for interrater reliability by a clinical psychologist (percent agreement = 81% to 98%). Analyses employ domain-level internalizing and externalizing symptom composites. Internalizing problems included specific and social phobia, separation anxiety, generalized anxiety, and depression/dysthymia. Externalizing problems included oppositional defiant, conduct and attention deficit hyperactivity disorder symptoms.
Analytic Plan
A special class of Structural Equation Model (SEM)—Serial Mediation Model, which is also known as PROCESS Model 6 (Hayes, 2013)), was used to examine the hypothesized pathways: from the predictor (past year IPV experienced by mothers) to the outcome (children’s internalizing/externalizing symptoms during the past three months) via two potential mediators (maternal PTSD symptoms and maternal parenting style). Separate analyses were conducted for physical and psychological IPV as the predictors and for children’s internalizing and externalizing symptoms as the outcomes, resulting in four models (Figures 1, 2, 3, and 4). This class of models is particularly well-suited for process-oriented research. It allows investigators to explore several direct and indirect paths and differential impact of specific types of IPV on children’s symptoms. All serial mediation models were fitted in SAS using the PROCESS macro (Hayes, 2013) and PROC CALIS controlling for children’s gender, age, and race as covariates. The PROCESS macro employs bootstrapping to estimate standard error of all indirect effects, as well as to construct bias-corrected confidence intervals for testing all interested paths. Proc CALIS reports standard SEM model fit indices such as Goodness of Fit Index (GFI), Root Mean Square Error of Approximation (RMSEA), Akaike Information Criterion (AIC), Schwarz Bayesian Criterion (SBC), and Bentler Comparative Fit Index (BCFI), as well as standardized direct path coefficients. Due to positive skewness of the “raw Z” internalizing and externalizing scores (range = −1 to 3.6, with approximately 10% scored greater than one), these scores were log transformed prior to model fitting.
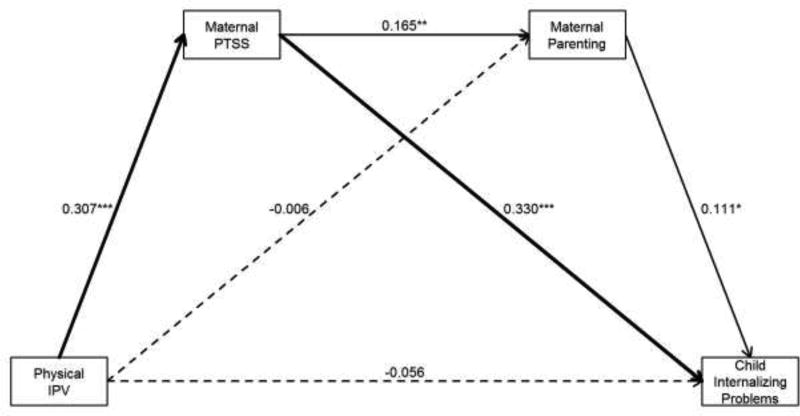
Figure 1. Physical IPV - Internalizing Problems Model.
Serial mediation model examining indirect pathways between maternal physical IPV victimization and child internalizing problems. Solid lines indicate significant direct paths. Thick solid lines indicate significant indirect paths. * p < .05, ** p < .01, *** p < .001. PTSS = PTSD symptoms. Model Fit: n = 299; GFI = 0.983, Adjusted GFI = 0.919; RMSEA = 0.086 (90% CI [0.04, 0.13]), AIC = 63.1, BCAIC = 166.5, SBC = 144.5, BCFI = 0.858, BBNFI = 0.832
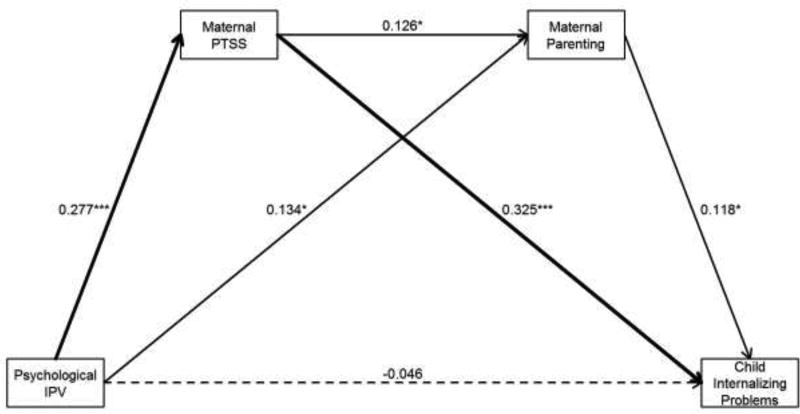
Figure 2. Psychological IPV - Internalizing Problems Model.
Serial mediation model examining indirect pathways between maternal psychological IPV victimization and child internalizing problems. Solid lines indicate significant direct paths. Thick solid lines indicate significant indirect paths. * p < 0.05, ** p < 0.01, *** p < 0.001. PTSS = PTSD symptoms. Model Fit: n = 299; GFI = 0.982, Adjusted GFI = 0.916; RMSEA = 0.088 (90% CI [0.05, 0.13]), AIC = 63.8, BCAIC = 167.2, SBC = 145.2, BCFI = 0.846, BBNFI = 0.821
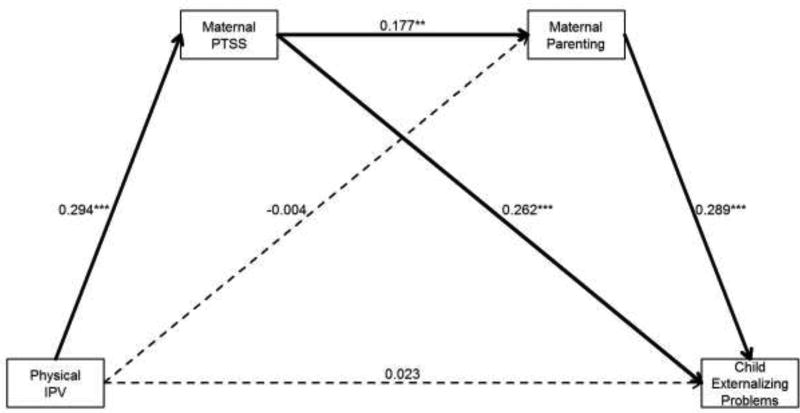
Figure 3. Physical IPV - Externalizing Problems Model.
Serial mediation model examining indirect pathways between maternal physical IPV victimization and child externalizing problems. Solid lines indicate significant direct paths. Thick solid lines indicate significant indirect paths. * p < 0.05, ** p < 0.01, *** p < 0.001. PTSS = PTSD symptoms. Model Fit: n = 308; GFI = 0.982, Adjusted GFI = 0.916; RMSEA = 0.088 (90% CI [0.05, 0.13]), AIC = 64.3, BCAIC = 168.4, SBC = 146.4, BCFI = 0.882, BBNFI = 0.857
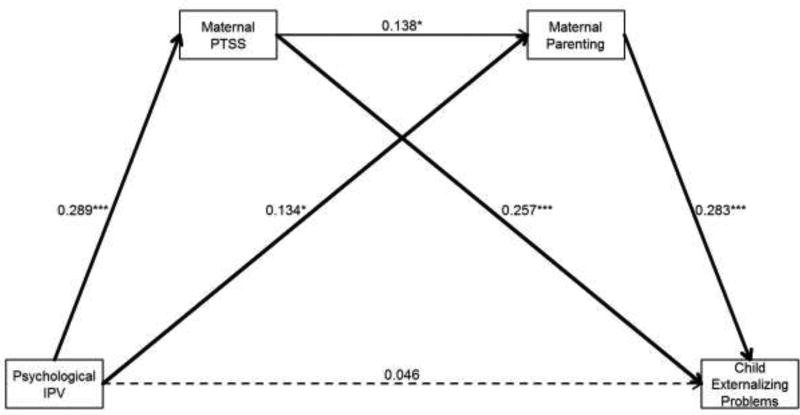
Figure 4. Psychological IPV to Externalizing Problems.
Serial mediation model examining indirect pathways between maternal psychological IPV victimization and child externalizing problems. Solid lines indicate significant direct paths. Thick solid lines indicate significant indirect paths. * p < 0.05, ** p < 0.01, *** p < 0.001. PTSS = PTSD symptoms. Model Fit: n = 308; GFI = 0.981, Adjusted GFI = 0.913; RMSEA = 0.091 (90% CI [0.05, 0.13]), AIC = 65.2, BCAIC = 169.3, SBC = 147.3, BCFI = 0.878, BBNFI = 0.854
Each Serial Mediation Model included one primary direct path (from IPV to child symptoms), five other direct paths (1: from IPV to PTSD; 2: from IPV to parenting style; 3: from PTSD to parenting style; 4: from PTSD to child symptoms; 5: from parenting style to child symptoms), and three indirect paths (1: from IPV via PTSD to child symptoms; 2: from IPV via parenting style to child symptoms; 3: from IVP via PTSD and then parenting style to child symptoms. In Figures 1 to 4, standardized coefficients for the six direct paths are displayed. Significant indirect paths (p < .05, i.e., 95% Bootstrap bias-corrected CI does not include zero) are shown by connecting chains of two or three thick solid arrows.
To assess the robustness of the primary models, a sensitivity analysis was conducted to determine whether the same findings were observed when both forms of IPV were included in the same model. Four additional serial mediation models were examined: two models with physical IPV as predictor and psychological IPV as an additional covariate and vice versa.
Results
Descriptive statistics
Twenty-two percent of mothers reported experiencing one or more form of physical IPV in the past year. Among mothers who endorsed physical IPV, the mean severity score was 10.4 (SD = 20.7). The majority of the sample (81%) reported experiencing psychological IPV in the past year, with a mean severity score of 18.4 (SD = 20.8) among mothers reporting any psychological IPV. The mean maternal PTSD symptom score was 26.1 (SD = 10.6). The first quartile fell at 18 and the third quartile at 29. Maternal parenting styles fell along the full range of the coding system. Most mothers were rated on the authoritative/non-punitive end of the scale, with 24% rated as using authoritative, non-punitive methods and 40% using predominantly authoritative, rarely punitive methods. However, approximately one third of mothers were rated as displaying a more harsh parenting style, with 20% using a mixed parenting style characterized by both authoritative and punitive features, and 16% rated as using predominantly restrictive/punitive parenting methods.
Table 1 presents Bivariate Spearman Correlations among key study variables. As expected, physical and psychological IPV were strongly correlated with one another, as well as with maternal PTSD. Children’s internalizing and externalizing symptoms also correlated strongly, as is common in child studies. Although poverty correlated modestly with physical IPV and restrictive/punitive parenting, it was not significantly associated with other key variables, including maternal PTSD or child symptoms and thus was not included as a covariate in models.
Table 1.
Bivariate Spearman Correlation Coefficients
| Black | Child Age |
Maternal Age |
Poverty | Physical IPV |
Psychological IPV |
Maternal PTSD |
Parenting higher score = more punitive) |
Child Internalizing |
Child Externalizing |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Male | 0.06 | 0.07 | 0.08 | −0.04 | 0.09 | 0.06 | −0.05 | 0.10 | −0.05 | 0.05 |
| black | −0.14* | 0.11* | 0.29*** | 0.09 | −0.03 | 0.02 | 0.22*** | 0.10 | 0.11 | |
| Child age | 0.10 | 0.07 | 0.02 | 0.06 | −0.01 | −0.03 | −0.02 | −0.13* | ||
| Maternal age | −0.39*** | 0.14* | −0.10 | −0.05 | −0.12* | 0.03 | −0.01 | |||
| Poverty | 0.15** | 0.03 | 0.09 | 0.12* | 0.11 | 0.05 | ||||
| Physical IPV | 0.47*** | 0.32*** | 0.22*** | 0.04 | 0.11 | |||||
| Psychological IPV | 0.30*** | 0.24*** | 0.05 | 0.17** | ||||||
| Maternal PTSD | 0.17** | 0.25*** | 0.28*** | |||||||
| Parenting | 0.17** | 0.34*** | ||||||||
| Child Internalizing | 0.55*** |
p <.05,
p<.01,
p<.001
Examination of these correlations provides preliminary support for the first two study hypotheses. Significant positive associations between children’s internalizing and externalizing symptoms and maternal PTSD and restrictive/punitive parenting supported Hypothesis 1. Partially supporting Hypothesis 2, physical and psychological IPV were associated with maternal PTSD and restrictive/punitive parenting. However, the only significant association between IPV and child symptoms was for child externalizing symptoms and psychological IPV.
Serial Mediation Models
All four SEMs provided good fit to the data: all GFI > 0.98, RMSEA < 0.09, and BCFI > 0.85.
Direct Pathways among IPV, Mothers’ Posttraumatic Stress Symptoms, Parenting Strategies and Children’s Mental Health Symptoms
Consistent with the patterns observed in Table 1, in all four models (Figures 1 – 4), there were four significant direct paths: (1) from IPV to maternal PTSD, (2) from maternal PTSD to restrictive/punitive parenting behaviors, (3) from maternal PTSD to child symptoms, and (4) from restrictive/punitive parenting behaviors to child symptoms. However, the direct path from IPV to parenting was only significant for Psychological IPV (Figures 2 and 4). Notably, the direct path from IPV to child symptoms was not significant in any of the four models.
Indirect Pathways from Maternal IPV to Child Mental Health Symptoms
There was one consistently significant indirect pathway: from IPV via PTSD to child symptoms (Figures 1 – 4, estimated indirect effects and 95% Bootstrap CIs = 0.0032 [0.0016, 0.0073], 0.0015 [0.0008, 0.0025], 0.0027 [0.0014, 0.0055], and 0.0014 [0.0007, 0.0023], respectively). In Figure 1, this significant indirect pathway was the connection of two standardized direct paths: 0.307 from physical IPV to PTSD and 0.330 from PTSD to internalizing symptoms. Hence the indirect pathway indicated that an increase of one standard deviation in physical IPV experienced by mother was associated with an increase in PTSD symptoms of 0.31 standard deviations and resulted in an increase of 0.307 × 0.330 = 0.101 standard deviations in child internalizing symptoms. This indirect pathway in Figure 2 implied that an increase of one standard deviation of psychological IPV experienced by mother was associated with an increase in PTSD symptoms by 0.277 standard deviations and resulted in an increase of 0.277 × 0.325 = 0.090 standard deviations in child internalizing symptoms. Figure 3 suggested that an increase of one standard deviation of physical IPV experienced by mother was associated with an increase in PTSD symptoms by 0.294 standard deviations and results in an increase of 0.294 × 0.262 = 0.077 standard deviations in child externalizing symptoms. Figure 4 implied that an increase of one standard deviation of psychological IPV experienced by mother was associated with an increase in PTSD symptoms by 0.289 standard deviations and results in an increase of 0.289 × 0.257 = 0.074 standard deviations in child externalizing symptoms.
With child externalizing symptoms as the outcome, there were two additional significant indirect pathways. The first indirect path started from physical IPV via PTSD and then parenting to child symptoms (Figure 3, estimated indirect effect and 95% Bootstrap CI = 0.0005 (0.0001, 0.0012)) such that an increase of one standard deviation in physical IPV experienced by mother was associated with an increase in PTSD symptoms by 0.294 standard deviations, and then an increase in restrictive/punitive parenting strategies by 0.294 × 0.177 = 0.052 standard deviations and ultimately resulted in an increase of 0.294 × 0.177 × 0.289 = 0.015 standard deviations in child externalizing symptoms. The second indirect path started from psychological IPV via parenting to child symptoms (Figure 4, estimated indirect effect and 95% Bootstrap CI = 0.0007 (0.0001, 0.0014)) such that an increase of one standard deviation in psychological IPV experienced by mother was associated with an increase in restrictive/punitive parenting strategies by 0.134 standard deviations and ultimately an increase of 0.134 × 0.283 = 0.038 standard deviations in child externalizing symptoms.
Finally, results of the sensitivity analysis indicated the same pattern of results when the model for physical IPV controlled for psychological IPV and vice versa. Results were consistent with the main models described above with very similar standardized coefficients and no changes in the statistical test results regarding both direct and indirect pathways. Moreover the main models were better based on all model fit indices (data available upon request).
Discussion
It is well documented that children exposed to intimate partner violence are at increased risk for numerous socioemotional concerns, including internalizing and externalizing problems. Yet the mechanisms by which this risk is incurred are less well understood, especially among young children. Elucidating risk and protective factors for children exposed to violence is essential to providing effective interventions. Given the strong influence of family processes on children’s adjustment following trauma exposure, this study set out to examine the effects of maternal posttraumatic stress symptoms and punitive parenting behaviors on young children’s internalizing and externalizing symptoms within the context of maternal IPV victimization. The results of this study suggest a complex relationship of family physical and emotional climate that affects both mothers’ and young children’s emotional and behavioral functioning following IPV. While the only direct association between IPV and child mental health outcomes was a bivariate correlation between mothers’ psychological IPV experiences and child externalizing symptoms, our other hypothesized direct associations among IPV, maternal PTSD symptoms, punitive parenting strategies, and children’s internalizing and externalizing symptoms were supported in all four models. In addition, we identified several significant indirect pathways from IPV to children’s symptoms in both domains. All models underscored the importance of maternal PTSD symptoms in these pathways. Finally, for externalizing (but not internalizing) symptoms, maternal punitive/restrictive parenting also played a role in increasing risk associated with maternal IPV.
These findings demonstrate that both psychological and physical IPV are associated with an increased risk for developing PTSD, consistent with the small body of literature that looks at the differential effects of forms of violence exposure on women (Pico-Alfonso, 2005), and adds to the small but growing literature that documents the serious, independent effects of psychological aggression on women’s PTSD symptoms, independent of physical victimization (Lagdon, Armour, & Stringer, 2014; Norwood & Murphy, 2012). In turn, maternal posttraumatic stress reactions may have a detrimental effect on young children. In fact, significant indirect effect pathways identified PTSD as a potential mediator between maternal IPV and young children’s mental health in all 4 models. This is consistent with recent research that documents a strong relationship between maternal PTSD and children’s mental health problems (Enlow et al., 2011; Leen-Feldner et al., 2013; Pat-Horenczyk et al., 2017), and suggests that mothers who are struggling with their own reactions to their victimization may be less able to regulate their response to their children (Katz & Gurtovenko, 2015). Prior work suggests that mothers who are experiencing posttraumatic stress may be unavailable or unable to provide their child with supportive, instructional, and empathic responses to their emotional distress (Kim, Trickett, & Putnam, 2010). They are also apt to inadvertently model reactive (harsh or helpless) emotional responses that are likely to increase their child’s distress and emotion dysregulation – and thus place them at risk for developing affective and behavioral problems (Shipman et al., 2007; Valiente, Lemery-Chalfant, & Reiser, 2007). On the other hand, mothers with fewer posttraumatic stress symptoms, who may be more affectively regulated, may be better able to assist their child in using adaptive emotion regulation skills when distressed and thereby support resilient outcomes (Morris, Silk, Steinberg, Myers, & Robinson, 2007). Thus, this study demonstrates the importance of considering maternal PTSD symptoms to emergent mental health symptoms in young children and the need for better understanding of how PTSD may manifest within the mother-child relationship.
Our results suggest that in the case of child externalizing symptoms, maternal IPV experiences may also indirectly affect young children through their mothers’ parenting style, as suggested by the spillover hypothesis. Consistent with our hypotheses, women who had experienced psychological aggression were rated as using more restrictive/punitive parenting strategies with their children. These parenting strategies were associated with an increase in mothers’ ratings of externalizing problems in their children, and to a lesser degree, with internalizing problems. The indirect pathway from maternal psychological IPV to children’s mental health through parenting was significant only for children’s externalizing symptoms, suggesting that among mothers who are the victims of psychological aggression, their parenting behaviors may mediate the relationship between their IPV victimization and their children’s behavioral problems, independent of their PTSD symptoms. The absence of similar findings for children’s internalizing symptoms may reflect the stronger relationship between restrictive/punitive parenting style and young children’s externalizing behavior problems (Pinquart, 2016; Williams et al., 2009). Alternately, a shared genetic risk for externalizing behaviors could underlie both mothers’ harsher parenting styles as well as their children’s disruptive behaviors (Mcgrath et al, 2012).
Somewhat surprisingly, in each of the models only psychological IPV was directly associated with mothers’ use of punitive parenting strategies in this sample. This was unexpected given the literature supporting a link between physical IPV victimization and use of harsh parenting strategies. Kelleher et al (2008) for example, found an association between physical IPV and psychologically and physically aggressive and neglectful parenting practices. The difference between these findings and our own, however, may be that Kelleher did not control for maternal PTSD. Indeed, while physical IPV was not directly associated with punitive parenting in this sample, it was indirectly linked though mothers’ PTSD symptoms, suggesting that once maternal PTSD is taken into account, physical IPV is no longer related to parenting behavior. In the only model to support our serial mediation hypothesis, the more physical IPV mothers reported, the greater their PTSD symptoms, which in turn increased the likelihood of their using restrictive/punitive parenting strategies, which were associated with greater reports of externalizing behaviors among their children.
Although beyond the scope of this paper, examining specific clusters of PTSD symptoms would help us to understand better how mothers’ stress reactions may be affecting their parenting and their young children (Ahlfs-Dunn & Huth-Bocks, 2014). It is possible that physical and psychological IPV are associated with different symptom clusters, which in turn differentially affect their behaviors and their children. For example, Ammerman et al. (2012) found only avoidance and emotional numbness symptoms to be associated with restrictive parenting among mothers of infants. Ahlfs-Dunn and Huth-Bocks (2014) found that mothers’ hyperarousal and re-experiencing symptoms moderated the relationship between IPV and infant social-emotional problems at 12 months of age. Thus, while limited, these patterns suggest that more nuanced understanding of how maternal PTSD manifests within the parent-child relationship will help to identify key treatment targets.
Clinical Implications
The findings reported here support an approach to working with young children and their families that considers the treatment needs for the entire family. Mental health providers working with children should routinely inquire about maternal history of physical and psychological violence and screen for maternal posttraumatic stress. Our findings suggest that knowing only about IPV exposure is likely insufficient for understanding young children’s risks; the presence of maternal PTSD symptoms may place children at increased risk for both internalizing and externalizing symptoms. Young children may be particularly vulnerable to the effects of maternal PTSD, as disruptions in maternal functioning may interfere with mothers’ ability to support young children’s attainment of self-regulation and autonomy, key developmental tasks of early childhood. Further, many young children are not yet in school full-time, and likely spend most of their time with their mothers. Thus, interventions with young children should consider and address maternal mental health problems. Parents have a profound impact on their children’s health and development, and often play a key role in child mental health interventions. However, their ability to provide support and security to their children, and to engage in responsive parenting practices, may be compromised when they are experiencing posttraumatic stress or other mental health challenges. A family-focused approach to child treatment such as this is consistent with recommendations for a trauma-informed care approach put forth by Harris and Fallot (2001) and Knight (2015) which include universal screening for traumatic experiences by all human service agencies, regardless of their primary mission, and recognition by practitioners of the role that past trauma may play in their clients’ current difficulties.
Limitations
The data used in this study were cross-sectional, which allows for the examination of indirect effects (Hayes, 2013), but temporally ordered, longitudinal data are needed to test for prospective mediational pathways (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001). Nevertheless, the multiple indirect pathways identified in this study suggest that PTSD and parenting strategies may be mediators of the relationship between maternal IPV victimization and young children’s mental health problem and warrant longitudinal examination.
There were a few design factors that may have affected our findings. Data for the study came exclusively from mothers and focused solely on mothers’ mental health symptoms and parenting behaviors. In addition to the risk of shared method variance stemming from a single reporter, maternal reports of child symptoms may have been influenced by the mothers’ own mental health status, and paternal mental health and parenting behaviors may also influence children’s outcomes. Future research would benefit from multi-informant reports, direct observation of children’s emotional responses and behaviors and parent-child interactions, and the inclusion of information about fathers. In addition, although the study sample was derived from an ethnically, racially, and socioeconomically diverse pediatric primary care population, we oversampled for IPV exposure and disruptive behaviors in order to increase the study’s power. Thus, there may be more IPV exposure in our sample of children than in the general population, and likely less than would be found in a sample of children recruited from a domestic violence shelter. Future work in a general population sample is needed to ensure that patterns fully generalize to young children more broadly.
Finally, we did not examine the cumulative effect of both childhood and adult victimization on mothers’ symptoms. Because there is some evidence that among women experiencing IPV childhood abuse is an added risk factor for worse psychological functioning and greater use of negative parenting strategies (Levendosky & Graham-Bermann, 2001; Margolin, Gordis, Medina, & Oliver, 2003), looking at the cumulative effect of victimization will be an important next step.
Conclusions
Findings highlight the importance of maternal PTSD symptoms and parenting behavior on young children’s symptoms of psychopathology following IPV exposure, and underscores the need for further examination and refinement of the mechanisms of transmission of risk. Supporting parents in recovering from the sequelae of their own traumatic experiences is critical, for their own emotional health, as well as that of their children.
Acknowledgments
This research was supported in part by funding from the National Institute of Mental Health: MH090301 (Briggs-Gowan), MH082830 (Wakschlag), and MH082830 (Wakschlag & Briggs-Gowan).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahlfs-Dunn SM, Huth-Bocks AC. Intimate partner violence and infant socioemotional development: the moderating effects of maternal trauma symptoms. Infant Mental Health Journal. 2014;35(4):322–335. doi: 10.1002/imhj.21453. [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Chard KM, Stevens J, Van Ginkel JB. PTSD in depressed mothers in home visitation. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(2):186–195. doi: 10.1037/a0023062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banyard VL, Williams LM, Siegel JA. The impact of complex trauma and depression on parenting: An exploration of mediating risk and protective factors. Child Maltreatment. 2003;8(4):334–349. doi: 10.1177/1077559503257106. [DOI] [PubMed] [Google Scholar]
- Becker KD, Stuewig J, McCloskey LA. Traumatic stress symptoms of women exposed to different forms of childhood victimization and intimate partner violence. Journal of Interpersonal Violence. 2010;25(9):1699–1715. doi: 10.1177/0886260509354578. [DOI] [PubMed] [Google Scholar]
- Campbell SB. Comments on the measurement of social and emotional development in early childhood (sub-focus: behavior problems) 2015 Retrieved from https://www.childstats.gov/forum/deliverables.asp.
- Chemtob CM, Carlson JG. Psychological effects of domestic violence on children and their mothers. International Journal of Stress Management. 2004;11(3):209–226. doi: 10.1037/1072-5245.11.3.209. [DOI] [Google Scholar]
- Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, Abramovitz R. Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children's behavior. Child Development. 2010;81(4):1129–1141. doi: 10.1111/j.1467-8624.2010.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Smith PH. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;23(4):260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Davies PT, Cummings EM. Marital conflict and child adjustment: An emotional security hypothesis. Psychological Bulletin. 1994;116(3):387–411. doi: 10.1037/0033-2909.116.3.387. [DOI] [PubMed] [Google Scholar]
- de la Vega A, de la Osa N, Granero R, Ezpeleta L. Severity of psychological maltreatment and accumulative risk forpsychopathology in children of mothers exposed to intimate partner violence. Journal of Family Violence. 2013;28(5):427–434. doi: 10.1007/s10896-013-9521-1. [DOI] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-Retest Reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Enlow MB, Kitts RL, Blood E, Bizarro A, Hofmeister M, Wright RJ. Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behavior & Development. 2011;34(4):487–503. doi: 10.1016/j.infbeh.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SE, Davies C, DiLillo D. Exposure to domestic violence: A meta-analysis of child and adolescent outcomes. Aggression and Violent Behavior. 2008;13:131–140. doi: 10.1016/j.avb.2008.02.005. [DOI] [Google Scholar]
- Fantuzzo J, Boruch R, Beriama A, Atkins M, Marcus S. Domestic violence and children: Prevalence and risk in five major cities. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(1):116–122. doi: 10.1097/00004583-199701000-00025. [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, Erbes CR. Posttraumatic stress symptoms among national guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology. 2010;78(5):599–610. doi: 10.1037/a0020571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham-Bermann SA, Gruber G, Howell KH, Girz L. Factors disriminating among profiles of resilience and psychopathology in children exposed to intimate partner violence (IPV) Child Abuse & Neglect. 2009;33(648–660) doi: 10.1016/j.chiabu.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Graham-Bermann SA, Levendosky AA. Traumatic stress symptoms in children of battered women. Journal of Interpersonal Violence. 1998;13(1):111–128. [Google Scholar]
- Grasso DJ, Henry D, Kestler J, Nieto R, Wakschlag LS, Briggs-Gowan MJ. Harsh parenting as a potential mediator of the association between intimate partner violence and child disruptive behavior in families with young children. Journal of Interpersonal Violence. 2016;31(11):2102–2126. doi: 10.1177/0886260515572472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeson MR, Kennedy AC, Bybee D, Beeble ML, Adams AE, Sullivan C. Beyond deficits: Intimate partner violence, maternal parenting, and child behavior over time. American Journal of Community Psychology. 2014;54:46–58. doi: 10.1007/s10464-014-9658-y. [DOI] [PubMed] [Google Scholar]
- Gustafsson HC, Coffman JL, Cox MJ. Intimate partner violence, maternal sensitive parenting behaviors, and children's executive functioning. Psychology of Violence. 2015;5(3):266–274. doi: 10.1037/a0037971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson HC, Cox MJ, Blair C. Maternal parenting as a mediator of the relationship between intimate partner violence and effortful control. Journal of Family Psychology. 2012;26(1):115–123. doi: 10.1037/a0026283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamby S, Finkelhor D, Turner H, Ormrod R. Children's exposure to intimate partner violence and other family violence. Washington, D.C.: U.S. Department of Justice; 2011. [Google Scholar]
- Harris M, Fallot RD. Envisioning a trauma-informed service system: A vital paradigm shift. New Directions for Mental Health Services. 2001;89:3–22. doi: 10.1002/yd.23320018903. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis. New York, NY: Guildford Press; 2013. [Google Scholar]
- Huang C-C, Vikse JH, Lu S, Yi S. Children's exposure to intimate partner violence and early delinquency. Journal of Family Violence. 2015;30:953–965. doi: 10.1007/s10896-015-9727-5. [DOI] [Google Scholar]
- Jouriles EN, McDonald R, Slep AMS, Heyman RE, Garrido E. Child abuse in the context of domestic violence: Prevalence, explanations, and practice implications. Violence and Victims. 2008;23(2):221–235. doi: 10.1891/0886-6708.23.2.221. [DOI] [PubMed] [Google Scholar]
- Katz LF, Gurtovenko K. Posttraumatic stress and emotion regulation in survivors of intimate partner violence. Journal of Family Psychology. 2015;29(4):528–536. doi: 10.1037/fam0000128. [DOI] [PubMed] [Google Scholar]
- Kelleher KJ, Hazen AL, Coben J, Wang Y, McGeehan J, Kohl PL, Gardner WP. Self-reported disciplinary practices among wome in the child welfare system: Association with domestic violence victimization. Child Abuse & Neglect. 2008;32:811–818. doi: 10.1016/j.chiabu.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Kim K, Trickett PK, Putnam FW. Childhood experiences of sexual abuse and later parenting practices among non-offending mothers of sexually abused and comparison girls. Child Abuse & Neglect. 2010;34(8):610–622. doi: 10.1016/j.chiabu.2010.01.007. [DOI] [PubMed] [Google Scholar]
- Kitzmann KM, Gaylord NK, Holt AR, Kenny ED. Child witnesses to domestic violence: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2003;71(2):339–352. doi: 10.1037/022-006X.71.2.339. [DOI] [PubMed] [Google Scholar]
- Knight C. Trauma-informed social work practice: Practice considerations and challenges. Clinical Social Work Journal. 2015;43:25–37. [Google Scholar]
- Kraemer HC, Stice E, Kazdin AE, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators and indpendent, overlapping and proxy risk factors. American journal of Psychiatry. 2001;158(6):848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Lagdon S, Armour C, Stringer M. Adult experience of mental health outcomes as a result of intimate partner violence victimisation: a systematic review. Eur J Psychotraumatol. 2014;5 doi: 10.3402/ejpt.v5.24794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauterbach D, Bak C, Reiland S, Mason S, Lute MR, Earls L. Quality of parental relationships among persons with a lifetime history of posttraumatic stress disorder. Journal of Traumatic Stress. 2007;20(2):161–172. doi: 10.1002/jts.20194. [DOI] [PubMed] [Google Scholar]
- Lawrence E, Yoon J, Langer A, Ro E. Is psychological aggression as detrimental as physical aggression? The independent effects of psychological aggression on depression and anxiety symptoms. Violence and Victims. 2009;24(1):20–35. doi: 10.1891/0886-6708.24.1.20. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Bunaciu L, Blumenthal H. Associations between parental posttraumatic stress disorder and both offspring internalizing problems and parental aggression within the National Comorbididty Survey-Replication. Journal of Anxiety Disorders. 2011;25(2):169–175. doi: 10.1016/j.janxdis.2010.08.017. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Knapp A, Bunaciu L, Blumenthal M, Amstadter AB. Offspring psychological and biological correlates of parental posttraumatic stress: Review of the literature and research agenda. Clinical Psychology Review. 2013;33(8):1106–1133. doi: 10.1016/j.cpr.2013.09.001. [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Graham-Bermann SA. Parenting in battered women: The effects of domestic violence on women and their children. Journal of Family Violence. 2001;16(2):171–192. [Google Scholar]
- Levendosky AA, Huth-Bocks AC, Shapiro DL, Semel MA. The impact of domestic violence on the maternal-child relationship and preschool-age children's functioning. Journal of Family Psychology. 2003;17(3):275–287. doi: 10.1037/0893-3200.17.3.275. [DOI] [PubMed] [Google Scholar]
- Loucks LA, Shaffer A. Joint relation of intimate partner violence and parenting stress to observed emotionally unsupportive parenting behavior. Couple and Family Psychology: Research and Practice. 2014;3(3):178–192. doi: 10.1037/cfp0000023. [DOI] [Google Scholar]
- Margolin G, Gordis EB, Medina AM, Oliver PH. The Co-Occurrence of Husband-to-Wife Aggression, Family-of-Origin Aggression, and Child Abuse Potential in a Community Sample: Implications for Parenting. Journal of Interpersonal Violence. 2003;18(4):413–440. doi: 10.1177/0886260502250835. [DOI] [Google Scholar]
- McDonald R, Jouriles EN, Briggs-Gowan MJ, Rosenfield D, Carter AS. Violence toward a family member, angry adult conflict, and child adjustment difficulties: Relations in families with 1- to 3-year-old children. Journal of Family Psychology. 2007;21(2):176–184. doi: 10.1037/0893-3200.21.2.176. [DOI] [PubMed] [Google Scholar]
- McDonald R, Jouriles EN, Ramisetty-Mikler S, Caetano R, Green CE. Estimating the number of American children living in partner-violent families. Journal of Family Psychology. 2006;20(1):137–142. doi: 10.1037/0893-3200.20.1.137. [DOI] [PubMed] [Google Scholar]
- Miller-Graff LE, Cater AK, Howell KH, Graham-Bermann SA. Parent-child warmth as a potential mediator of childhood exposure to intimate partner violence and positive adulthood functioning. Anxiety, Stress, & Coping. 2016:1–15. doi: 10.1080/10615806.2015.1028030. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The Role of the Family Context in the Development of Emotion Regulation. Social Development. 2007;16(2):361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathanson AM, Shorey RC, Tirone V, Rhatigan DL. The prevalence of mental health disorders in a community sample of female victims of intimate partner violence. Partner Abuse. 2012;3(1):59–75. doi: 10.1891/1946-6560.3.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols SR, Briggs-Gowan MJ, Estabrook R, Burns JL, Kestler J, Berman G, Wakschlag LS. Punishment insensitivity in early childhood: A developmental, dimensional approach. Journal of Abnormal Child Psychology. 2015;43(6):1011–1023. doi: 10.1007/s10802-014-9950-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwood A, Murphy C. What forms of abuse correlate with PTSD symptoms in partners of men being treated for intimate partner violence? Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(6):596–604. doi: 10.1037/a0025232. [DOI] [Google Scholar]
- O'Dor SL, Grasso DJ, Forbes D, Bates JE, McCarthy K, Wakschlag LS, Briggs-Gowan MJ. The Family Socialization Interview-Revised (FSI-R): a Comprehensive Assessment of Parental Disciplinary Behaviors. Prevention Science. 2017;18(3):292–304. doi: 10.1007/s11121-016-0707-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaya B, Expeleta L, de la Osa N, Granero R, Domenech JM. Mental health needs of children exposed to intimate partner violence seeking help from mental health services. Children and Youth Services Review. 2010;32:1004–1011. doi: 10.1016/j.childyouth.2010.03.028. [DOI] [Google Scholar]
- Pat-Horenczyk R, Cohen S, Ziv Y, Achituv M, Brickman S, Blanchard T, Brom D. Stability and change in posttraumatic distress: A 7-Year follow-up study of mothers and young children exposed to cumulative trauma. Journal of Traumatic Stress. 2017;30(2):115–124. doi: 10.1002/jts.22177. [DOI] [PubMed] [Google Scholar]
- Pico-Alfonso MA. Psychological intimate partner violence: the major predictor of posttraumatic stress disorder in abused women. Neuroscience and Biobehavioral Reviews. 2005;29(1):181–193. doi: 10.1016/j.neubiorev.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Pinquart M. Associations of parenting dimensions and styles with internalizing symptoms in children and adolescents: A meta-analysis. Marriage & Family Review. 2016:1–28. doi: 10.1080/01494929.2016.1247761. [DOI] [Google Scholar]
- Salloum A, Stover CS, Swaidan VR, Storch EA. Parent and child PTSD and parent depression in relation to parenting stress among trauma-exposed children. Journal of Child & Family Studies. 2015;24:1203–1212. doi: 10.1007/s10826-014-9928-1. [DOI] [Google Scholar]
- Schechter DS, Willheim E, McCaw JE, Turner JB, Myers MM, Zeanah CH. The relationship of violent fathers, posttraumatically stressed mothers and symptomatic children in a preschool-age inner-city pediatrics clinic sample. J Interpers Violence. 2011;26(18):3699–3719. doi: 10.1177/0886260511403747. [DOI] [PubMed] [Google Scholar]
- Schwerdtfeger KL, Larzelere RE, Werner D, Peters C, Oliver M. Intergenerational transmission of trauma: The mediating role of parenting styles on toddlers' DSM-related symptoms. Journal of Aggression, Maltreatment & Trauma. 2013;22(2):211–229. doi: 10.1080/10926771.2013.743941. [DOI] [Google Scholar]
- Sherman MD, Smith JL, Straits-Troster K, Larsen J, Gewirtz AH. Veterans' perceptions of the impact of PTSD on their parenting and children. Psychological Services. 2016;13(4):401–410. doi: 10.1037/ser0000101. [DOI] [PubMed] [Google Scholar]
- Shipman KL, Schneider R, Fitzgerald MM, Sims C, Swisher L, Edwards A. Maternal Emotion Socialization in Maltreating and Non-maltreating Families: Implications for Children's Emotion Regulation. Social Development. 2007;16(2):268–285. doi: 10.1111/j.1467-9507.2007.00384.x. [DOI] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy SUE, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. doi: 10.1177/019251396017003001. [DOI] [Google Scholar]
- Street AE, Arias I. Psychological abuse and posttraumatic stress disorder in battered women: Examining the roles of shame and guilt. Violence and Victims. 2001;16(1):65–78. [PubMed] [Google Scholar]
- Valiente C, Lemery-Chalfant K, Reiser M. Pathways to Problem Behaviors: Chaotic Homes, Parent and Child Effortful Control, and Parenting. Social Development. 2007;16(2):249–267. doi: 10.1111/j.1467-9507.2007.00383.x. [DOI] [Google Scholar]
- Vu NL, Jouriles EN, McDonald R, Rosenfield D. Children's exposure to intimate partner violence: A meta-analysis of longitudinal associations with child adjustment problems. Clinical Psychology Review. 2016;46:25–33. doi: 10.1016/j.cpr.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Carter AS, Hill C, Danis B, Keenan K, Leventhal BL. A developmental framework for distinguishing disruptive behavior from normative misbehavior in preschool chidren. Journal of Child Psychology and Psychiatry. 2007;48(10):976–987. doi: 10.1111/j.1469-7610.2007.01786.x. [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Choi SW, Nichols SR, Kestler J, Burns JL, Henry D. Advancing a multidimensional, developmental spectrum approach to preschool disruptive behavior. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(1):82–96. doi: 10.1016/j.jaac.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist: reliability, validity, & diagnostic utility; Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Williams LR, Degnan KA, Perez-Edgar KE, Henderson HA, Rubin KH, Pine DS, Fox NA. Impact of behavioral inhibition and parenting style on internalizing and externalizing problems from early childhood through adolescence. Journal of Abnormal Child Psychology. 2009;37(8):1063–1075. doi: 10.1007/s10802-009-9331-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yates TM, Dodds MF, Sroufe A, Egeland B. Exposure to partner violence and child behavior problems: A prospective study controlling for child physical abuse and neglect, child cognitive ability, socioeconomic status, and life stress. Development & Psychopathology. 2003;15:199–218. doi: 10.1017/s0954579403000117. doi: 10.1017.S0954579403000117. [DOI] [PubMed] [Google Scholar]