Abstract
Objective
The median age of single homeless adults is over 50, yet little is known about their emergency department (ED) use. We describe use of and factors associated with ED use in a sample of homeless adults 50 and older.
Methods
We recruited 350 participants who were homeless and 50 or older in Oakland, CA. We interviewed participants about residential history in the prior six months, health status, health-related behaviors, and health services use, and assessed cognition and mobility. Our primary outcome was the number of ED visits in the prior six months based on medical record review. We used negative binomial regression to examine factors associated with ED use.
Results
In the six months prior to enrollment, 46.3% of participants spent the majority of their time unsheltered, 25.1% cycled through multiple institutions including shelters, hospitals and jails, 16.3% primarily stayed with family or friends, and 12.3% had become homeless recently after spending much of the prior six months housed. Half (49.7%) of participants made at least one ED visit in the past six months; 6.6% of participants accounted for 49.9% of all visits. Most (71.8%) identified a regular non-ED source of healthcare; 7.3% of visits resulted in hospitalization. In multivariate models, study participants who used multiple institutions (incidence rate ratio [IRR] = 2.27; 95% confidence interval [CI] = 1.08–4.77) and who were unsheltered (IRR = 2.29; 95% CI = 1.17–4.48) had higher ED use rates than participants who had been housed for most of the prior six months. In addition, having health insurance/coverage (IRR= 2.6; CI = 1.5–4.4), a history of psychiatric hospitalization (IRR = 1.80; 95% CI = 1.09–2.99), and severe pain (IRR = 1.72; 95% CI = 1.07–2.76) were associated with higher ED visit rates.
Conclusions
A sample of adults aged 50 and older who were homeless at study entry had higher rates of ED use in the prior six months than the general US age-matched population. Within the sample, ED use rates varied based on individuals’ residential histories, suggesting that individuals’ ED use is related to exposure to homelessness.
Keywords: Hospital emergency service, Homeless persons, Aging
Introduction
Background
Individuals who are homeless visit emergency departments (EDs) at higher rates than the general population1,2 and are more likely to be frequent ED users.3–6 Reasons for high rates of ED use among people experiencing homelessness include a high prevalence of unintentional injuries and exposure to violence while homeless, as well as shared risk factors, including a high prevalence of drug, alcohol, tobacco use and mental health disorders.7–16 Finally, homeless individuals have a higher prevalence of being uninsured and of lacking reliable telephones or transportation; these factors may lead to ED use for complaints that may not necessitate ED care under different life circumstances.17,18
The median age of single homeless individuals has been increasing and is now over 50.19 Older, compared to younger, homeless people have lower rates of illicit substance use and higher rates of chronic diseases.20,21 Homeless individuals aged 50 and older have a prevalence and severity of geriatric conditions (i.e. cognitive impairment, functional impairments) higher than that of the general population in their 70s and 80s.9,20 For this reason, homeless individuals are considered to be “older” at the age of 50.22
The federal definition of homelessness as delineated in the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act, includes as homeless those who lack any shelter, those who stay in emergency shelters, and those who are at imminent risk of losing housing.23 There are a variety of living conditions that meet the definition of homeless. Approximately one third of homeless adults in the United States are unsheltered, whereas others stay in emergency shelters or double-up temporarily with family or friends.24 While some individuals remain homeless for long periods of time, others experience homelessness for short periods only. These varied conditions of homelessness may be associated with differing patterns of healthcare utilization.
Importance
As most prior research was conducted before the aging of the homeless population, there is little known about how homeless adults 50 and older use the ED. In addition, most prior studies of homelessness recruited individuals from shelters, or included only those who sought healthcare at homeless-specific clinics, which limits their generalizability. Finally, most prior studies classified individuals as homeless at one point in time and did not examine how health services utilization differed if individuals regained or lost housing. Understanding the patterns of and factors associated with ED use in adults 50 and over with a broader range of experiences of homelessness may help formulate appropriate interventions that can better serve homeless individuals who use the ED and respond best to the needs of this high risk population.
Goals of this investigation
To describe the patterns of ED use and to identify factors associated with ED use, we recruited a sample of 350 adults aged 50 and older in Oakland, CA who met criteria for homelessness, and examined data on their ED use in the prior six months. We hypothesized that the varied experience of homelessness (e.g. setting, duration) would differentially impact ED use. We also examined the contribution of chronic pain, chronic medical conditions, use of primary care, insurance status, mental health, and substance use problems in our cohort, based on our review of the literature demonstrating that these factors contribute to ED use.4,25
Methods
Subjects & Setting
Between July 2013 and June 2014, we recruited 350 individuals using purposive sampling from a random sample of homeless encampments, one recycling center, all overnight homeless shelters, and all free and low-cost meal programs serving at least 3 prepared meals a week in Oakland, CA.26 We designed our sampling frame in concert with our community advisory board, based on the best available evidence regarding the population experiencing homelessness in Oakland. We had predetermined recruitment targets from each venue, based on the numbers of unique individuals who met our study criteria who were served there over the course of the year. We continued to recruit from each venue until we met our venue-specific targeted enrollment.
We conducted an initial screen for study eligibility at the recruitment venue and invited individuals who met basic eligibility criteria (English speaking, aged 50 and older, homeless) to undergo an eligibility interview at our study site within one week. Most study interviews took place at St Mary’s Center, which is a non-profit community-based organization serving indigent older adults. It is located near a large proportion of the homeless population in West Oakland and is easily accessible by public transportation. After a detailed eligibility interview, we offered enrollment to participants who met the eligibility criteria: English-speaking, aged 50 and over, defined as homeless by the Homeless Emergency Assistance and Rapid Transition to Housing Act,23 and able to give informed consent, as determined by a teach-back method.27 We obtained written informed consent from all study participants.
Participants received gift cards to a major retailer worth $5 for the eligibility interview and $20 for the baseline interview. The University of California, San Francisco Institutional Review Board approved all study procedures.
Baseline Interview
Trained study staff administered a structured interview, which included housing history, demographic information, health history, heath care utilization, drug and alcohol use, mental health, social relationships, and healthcare utilization. Study staff completed assessments of cognitive impairment and physical functioning. We provided all participants with lists of community resources. If participants had acute medical or psychiatric needs, study staff called the study PI (MK) or covering physician to help assess the severity and to determine the appropriate intervention.
Dependent Variable
We defined the dependent variable as the number of emergency department (ED) visits in the 6 months prior to study enrollment, determined via administrative data from the public hospital serving the study area and medical record requests from other hospitals. For the public hospital, we obtained complete records of all ED visits for all study participants. We used participant self-report of ED visits to determine from which other hospitals to request records. At the baseline visit, participants reported how many times they had an ED visit that did not result in a hospitalization in the prior 6 months. For up to 4 visits, we collected the hospital name.
Reasons for ED use (descriptive variable)
Participants self-reported reasons for ED use. For up to four ED visits that did not result in hospitalization and, separately, up to four hospitalizations, we asked participants to report their reason for presenting (new injury, new illness, worsening chronic illness, pain, mental health problem, substance use, pain medication refill, other medication refill, other). We included reasons for all ED visits.
Hospitalizations (Descriptive variable)
We asked participants to report the total number of times they had been hospitalized in the prior 6 months. For up to 4 visits, participants reported the hospital name and whether or not the admission had occurred via the ED. For each hospital reported, we queried the hospital to obtain the dates of all ED and hospital visits by the participant who named it during his or her interview. For a group of three hospitals operated by a single provider, if a participant reported a visit to any of the three, we queried about visits to all. For our dependent variable, we included ED visits for which there was verification, whether or not the visit resulted in admission and whether or not the participant had reported it. We assessed number of hospitalizations in the same manner, and included hospitalizations that were and were not preceded by an ED visit.
Independent Variables
Sociodemographic Characteristics
We asked participants to self-report their age, sex, race/ethnicity, and highest level of education (0–11 years versus high school degree, GED, or more education), and monthly income (sources and amount). We categorized combined monthly income from all sources as $0–150, $151–700, $701–1150, and over $1150. We asked participants to report whether they had current health insurance and if so, which one. We classified participants as insured (Medicaid, Medicare, VA coverage, private insurance) or covered by county non-insurance health coverage plan for indigent adults versus uninsured/no health coverage. Adapting language from a question from the National Health Interview Survey,28 we asked participants if they had a regular, non-emergency department place that they received health care, and a regular health care provider (physician, nurse practitioner or physician assistant).
Residential Categories and History
Participants reported the age at which they first became homeless as an adult (aged 18 or older). To construct a six-month residential history, study staff asked participants where they had stayed the prior night, and then worked backward to construct a 6-month residential history, noting length of stay at each location (outdoors/location not meant for human habitation; emergency shelter; transitional housing; permanent housing for formerly homeless people; hotel or motel room; participant’s own housing; staying with friends or family; and hospital; jail or prison; treatment program or other institution).29 We used these residential histories to perform cluster analysis that allowed us to develop a classification of participants’ residential categories during the six months preceding study enrollment (See Analysis). Participants reported the duration of their current episode of homelessness.
Health status
We asked participants to self-report their health status (fair or poor versus good, very good, or excellent).30 Participants reported whether a health care provider had ever told them they had the following conditions: congestive heart failure, coronary artery disease or myocardial infarction, stroke, high blood pressure, diabetes, asthma or chronic obstructive pulmonary disease, and cancer) or whether they had tested positive for the human immunodeficiency virus.31
Mental Health and Substance Use
We screened participants for post-traumatic stress disorder (PTSD) using the Primary Care PTSD Screen.32 We considered those with a response of 3 or more as screening positive for PTSD. To assess the prevalence of depressive symptoms, we used the Center for Epidemiologic Studies Depression (CES-D) Scale.33 We categorized scores of ≥22 as indicative of moderate to severe depressive symptomatology.34,35 We used questions from the National Survey of Homeless Assistance Providers and Clients to determine if participants had lifetime experiences of : (1) hallucinations, (2) trouble controlling violent behavior, or (3) attempted suicide, categorizing responses as any versus none.36 We asked participants if they had ever been hospitalized for a psychiatric problem.
To assess alcohol use, we administered the Alcohol Use Disorders Identification Test (AUDIT),37 modifying the time frame to six months. We considered scores of 8 or more as indicative of at-risk alcohol use. Using the World Health Organization’s Alcohol, Smoking and Substance Involvement Screening Test (WHO-ASSIST) with an expanded timeframe of six months,38 we assessed participants’ risk of experiencing problems due to their use of cocaine, amphetamines, and non-prescribed opioids. We considered a score of 4 or more for any of the three substances to indicate at-risk substance use.
Functional Status and Cognition
We used the 5-item Katz Activities of Daily Living (ADL) scale to assess functional status.39 We categorized participants as having a difficulty with ADLs if they reported difficulty performing one or more ADL due to a physical, mental, emotional, or memory problem.40 We administered the Modified Mini-Mental State Examination (3MS)41 to screen for cognitive impairment. We adjusted 3MS scores for age and education using a standard reference population.41,42 We categorized participants scoring below the 7th percentile (>1.5 standard deviation below the mean) as cognitively-impaired.43 To assess the lower extremity functioning of participants, we administered the Short Physical Performance Battery (SPPB).31 We categorized participants as having impairment in lower extremity functioning if they scored 10 or less.44
Social Support
Participants indicated instrumental support by reporting if they had someone who would lend money or offer a place to stay if needed.45,46 Participants were dichotomized as having no versus any social network based on whether they reported having at least one friend or relative.
Pain
Using the Brief Pain Inventory,47 we asked participants to rate their average pain in the past week from 0 (no pain) to 10 (worst pain imaginable). We categorized pain ratings as none (0), mild to moderate (1–7), and severe (8–10).48 We asked participants with severe pain in the past week how long they had experienced this pain, and categorized responses as 6 months or less versus more than 6 months. We asked whether participants experienced oral pain and if so, how often (never or hardly ever versus occasionally, fairly often, or very often).
Other experiences
Participants were asked to report whether they had experienced physical or sexual abuse in the previous six months. Participants reported whether they had been incarcerated in jail or prison in the prior six months.
Analysis
To define our independent variable of residential categories, we classified participants into clusters that represented the predominant place that they stayed in the prior six months based on the residential follow-back survey using k-medians cluster methodology.49 Cluster analysis finds existing patterns within data to generate groups by minimizing within-group and maximizing between-group variability. It has been used in other studies of homeless individuals to classify subpopulations.50–52 We performed cluster analysis using Stata version 11.0. For further details of our cluster analysis, see a prior manuscript from our group.49
For statistical modeling of our primary outcome, the number of participant ED visits, we used negative binomial regression to examine factors associated with the number of ED visits in the prior 6 months. We chose to use negative binomial over Poisson modeling because there was substantial overdispersion of the data (mean = 1.8, variance = 14.6). We started with bivariate models based on pre-existing hypotheses, using variables listed above.53,54 For our multivariate model we used backward stepwise elimination, starting with a model containing all independent variables with a bivariate p-value of 0.2 or less and retained independent variables with p-values of less than or equal to 0.05. We conducted all analyses using SAS version 9.4.55
Results
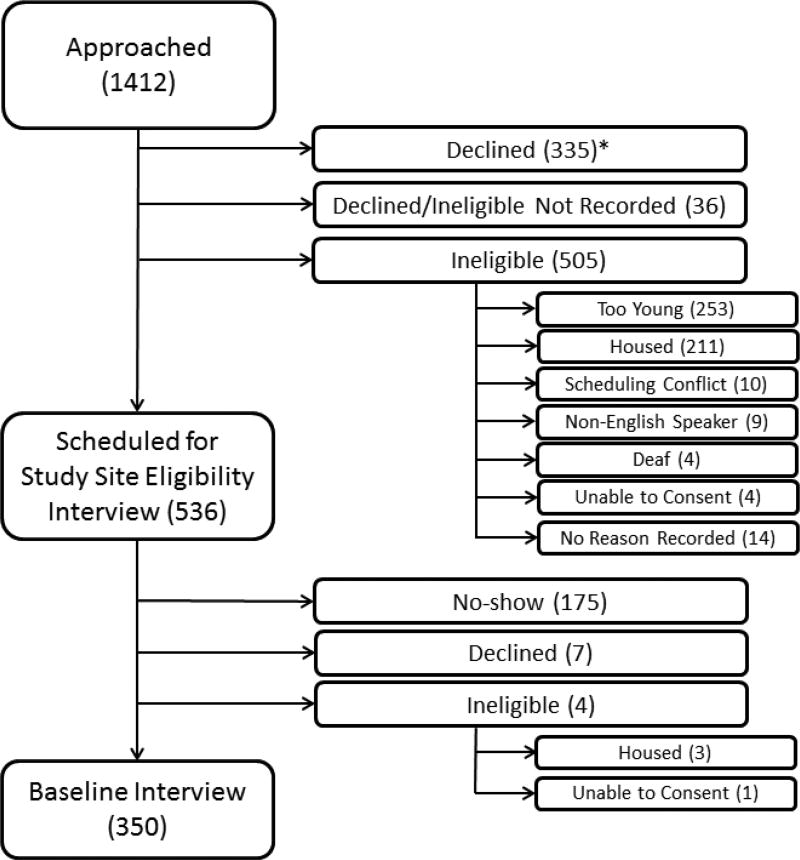
We approached 1412 individuals, of whom we determined that 505 did not meet basic eligibility requirements; an additional 371 declined prior to examining eligibility. We scheduled 536 for further screening, of whom 361 attended their appointment and 350 were eligible and agreed to enrollment (Figure 1). The majority of the 350 participants in the sample were male, African-American, and under 60. The majority of participants (74.3%) had completed high school, GED degree or higher. Over 90% of participants reported less than $1150 per month income from all sources. Most (79.6%) of individuals had insurance or health care coverage provided by the county. More than two-thirds of participants (72.0%) reported having a non-ED regular health care location and 52.9% reported having a regular health care provider. (Table 1)
Figure 1.
Flow-chart of recruitment of 350 homeless adults over the age of 50.
*This figure shows the number of individuals approached, assessed for eligibility, and enrolled in the study, noting specific reasons for inability to enroll. Values represent the number of individuals in each group. Participants who declined after being approached (335) declined before being assessed for eligibility. Therefore, the number of participants who were ineligible for the study may have been higher than the numbers presented in this table.
Table 1.
Participant Characteristics
| Variable* | No ED Visits N=186 |
Any ED Visits N=164 |
Total N=350 |
|---|---|---|---|
|
| |||
| Age, Median (IQR) | 58 (54–62) | 58 (54–61) | 58 (54–61) |
| Sex | |||
| Male | 143 (76.9) | 127 (77.4) | 270 (77.1) |
| Race | |||
| Black | 148 (79.6) | 131 (79.9) | 279 (79.7) |
| Non-Black | 38 (20.4) | 33 (20.1) | 71 (20.3) |
| Education | |||
| Completed High School or GED Degree | 138 (74.2) | 122 (74.4) | 260 (74.3) |
| Monthly Income (All Sources) | |||
| $0 to $150 | 49 (26.9) | 39 (24.0) | 88 (25.6) |
| $151 to $700 | 52 (28.6) | 32 (19.8) | 84 (24.4) |
| $701 to $1150 | 67 (36.8) | 71 (43.8) | 138 (40.1) |
| Over $1150 | 14 (7.7) | 20 (12.4) | 34 (9.9) |
| At-risk Substance Use, Past 6 Months | |||
| Alcohola | 50 (26.9) | 40 (24.5) | 90 (25.8) |
| Cocaine, Opioids, or Amphetaminesb | 81 (43.5) | 96 (58.5) | 177 (50.6) |
| Residential Statusc | |||
| Cohabiter | 31 (16.7) | 26 (15.9) | 57 (16.3) |
| Multiple Institution User | 49 (26.3) | 39 (23.8) | 88 (25.1) |
| Newly Homeless/Renters | 26 (14.0) | 17 (10.4) | 43 (12.3) |
| Unsheltered | 80 (43.0) | 82 (50.0) | 162 (46.3) |
| Mental Health Status | |||
| PTSDd | 58 (31.2) | 56 (34.1) | 114 (32.6) |
| Moderate to Severe Depressive Symptomatologye | 89 (48.4) | 96 (58.9) | 185 (53.3) |
| History of Hallucinations, Violent Impulses, Suicide Attempt | 115 (62.2) | 112 (68.3) | 227 (65.0) |
| Past Mental Health Hospitalization | 24 (12.9) | 42 (25.6) | 66 (18.9) |
| Functional Status and Cognition | |||
| Any ADL Impairmentf | 64 (34.4) | 72 (43.9) | 136 (38.9) |
| Lower Extremity Functioning Impairmentg | 102 (55.4) | 99 (61.9) | 201 (58.4) |
| Cognitive Impairmenth | 44(23.7) | 46 (28.2) | 90 (25.8) |
| Instrumental Social Supporti | |||
| None | 62 (33.7) | 54 (33.3) | 116 (33.5) |
| Self-Rated Health Statusj | |||
| Poor or Fair Health | 99 (53.2) | 96 (58.5) | 195 (55.7) |
| Medical Conditionk | |||
| Hypertension | 100 (54.1) | 95 (58.3) | 195 (56.0) |
| Diabetes | 23 (12.4) | 26 (15.9) | 49 (14.0) |
| Asthma/Chronic Obstructive Pulmonary Disease | 39 (21.0) | 53 (32.3) | 92 (26.3) |
| Cancer | 8 (4.3) | 13 (7.9) | 21 (6.0) |
| Human Immunodeficiency Virus | 10 (5.5) | 9 (5.6) | 19 (5.5) |
| Coronary Artery Disease/Myocardial Infarction | 12 (6.5) | 20 (12.2) | 32 (9.1) |
| Stroke | 16 (8.6) | 23 (14.1) | 39 (11.2) |
| Congestive Heart Failure | 12 (6.5) | 13 (7.9) | 25 (7.1) |
| Oral Painl | |||
| Occasionally/Fairly Often/Very Often | 68 (36.6) | 72 (43.9) | 140 (40.0) |
| Pain, past weekm | |||
| Mild to Moderate | 57 (30.6) | 30 (18.5) | 87 (25.0) |
| Severe | 57 (30.6) | 80 (49.4) | 137 (39.4) |
| Health Care Utilization | |||
| Regular Health Care Location | 129 (69.4) | 123 (75.0) | 252 (72.0) |
| Regular Health Care Provider | 95 (51.4) | 89 (54.6) | 184 (52.9) |
| Abuse, Past 6 Months | |||
| Physicaln | 13 (7.1) | 22(13.5) | 35 (10.1) |
| Sexualo | 5 (2.7) | 1 (0.6) | 6 (1.7) |
| Jail or Prison, Past 6 Months | 21 (11.3) | 16 (9.8) | 37 (10.6) |
| Any Health Insurance Coveragep | 139 (39.9) | 138 (85.2) | 277 (79.6) |
Data presented as N (%) unless otherwise noted
At-risk alcohol use defined as Alcohol Use Disorders Identification Test (AUDIT) score ≥8
At-risk drug use defined as Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) score ≥4
Residential status defined as primary living environment in the past 6 months as determined using cluster analysis; Overall (Type 3) p-value = 0.021
Post-traumatic stress disorder defined as a PTSD Screen score of ≥3
Moderate to severe depressive symptomatology defined as a Center for Epidemiologic Studies Depression Scale score of ≥22
ADL, activities of daily living, impairment defined as self-reported difficulty performing 1 or more ADLs
Lower extremity functioning impairment defined as Short Performance Physical Battery score of ≤10
Cognitive impairment defined as Modified Mini-Mental State Examination score below the 7th percentile (i.e., 1.5 standard deviations below the demographically-adjusted cohort mean)
Instrumental social support defined as having anyone who would lend money or offer a place to stay if needed
Self-rated health status assessed using Ware, et al. 1-item health screen
Medical conditions assessed by self-report of having received a diagnosis from a physician or positive test result for HIV
Oral pain defined as having pain anywhere in the mouth in the past 6 months
Pain assessed using the Brief Pain Inventory; none (0), mild to moderate (1–7), severe (8–10); Overall (Type 3) p-value = 0.021
Physical abuse defined as experiencing physical violence perpetrated by another person using an object or being slapped, hit, punched, kicked, choked, or burned
Sexual abuse defined as being pressured or forced to have sexual contact, to do something sexual, or to have sex
Health insurance coverage includes Medicaid; Medicare; Alameda HealthPAC, a county-run health plan covering low-income residents not eligible for Medicaid; or any other kind of private or public health plan
ED use
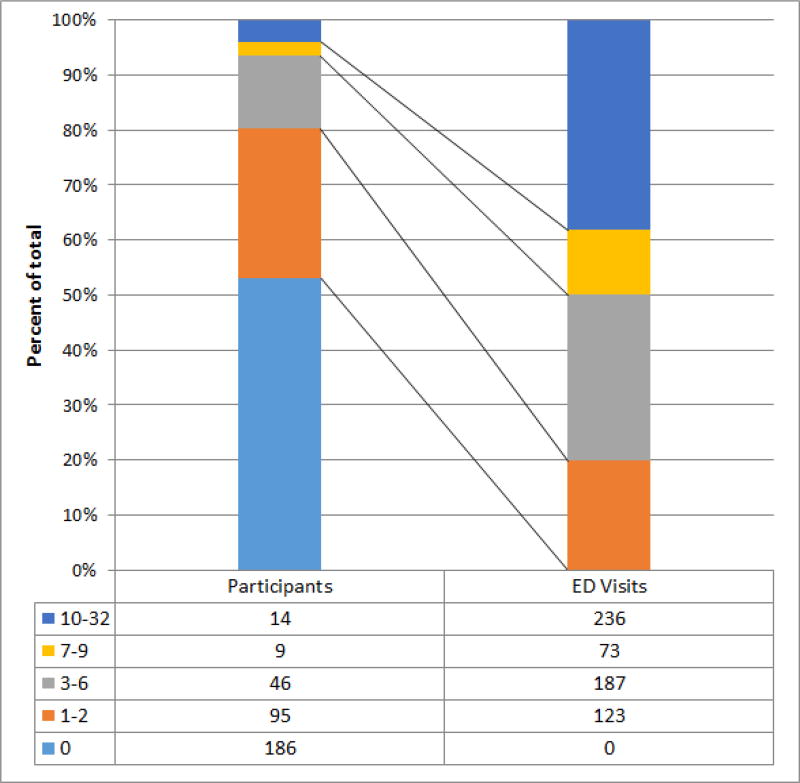
Half of participants (49.7%) had at least one ED visit within the past 6 months. One-fifth (19.1%) had one ED visit, while 27.7% had two or more (range 2–32). The 23 participants (6.6%) who made 7 or more ED visits in the prior six months accounted for 49.9% of all ED visits. (Figure 2) The most common reasons for visiting the ED were worsening of a chronic illness (23.9% of visits), a new illness (21.6%), and pain (19.2%). (Table 2)
Figure 2.
Distribution of emergency department (ED) visits by study population
Table 2.
Reasons for emergency department visits
| Reason for ED Visit | No. | Percentage |
|---|---|---|
|
| ||
| Chronic Illness | 83 | 23.9 |
| New Illness | 75 | 21.6 |
| Pain | 67 | 19.2 |
| Injury | 57 | 16.4 |
| Needed Pain Meds | 29 | 8.3 |
| Mental Health Problem | 20 | 5.8 |
| Other* | 17 | 4.9 |
Other reasons include: Substance Use/Overdose, Needed non-pain meds, Planned surgery, Other/not specified
Hospitalizations
Ten percent of participants had one or more hospital admissions in the prior six months. Most admissions (85.7%) occurred via the ED. Of all ED visits, 7.3% resulted in a hospital admission.
Residential status
While all participants were homeless at the time of enrollment, our cluster analysis divided participants into four groups based on where they had spent the most nights in the prior six months: we classified 46.3% as “unsheltered,” 25.1% as “users of multiple institutions” (shelters, jails, hospitals), 16.3% as “cohabiters” staying with family or friends, and 12.3% as “renters,” having spent the majority of their nights in the prior six months housed before becoming homeless.49 Unsheltered participants and users of multiple institutions were more likely to have experienced longer episodes of homelessness. The majority of renters (90.7%) and cohabiters (57.9%) had been homeless for less than 6 months as compared to only a minority of unsheltered individuals (9.9%) and multiple institution users (28.7%); 69.7% of unsheltered individuals had been homeless for over 1 year.
Health status and conditions
Over half of the participants (55.7%) rated their health as fair or poor. A third (33.4%) had one chronic condition and 41.2% had two or more. The most common conditions were hypertension, asthma or chronic obstructive pulmonary disease, and diabetes. (Table 1)
Pain
Over one-third of participants (39.4%) reported experiencing severe pain in the prior week and 18.0% reported oral pain. Of those who met criteria for severe pain in the past week, 78.8% reported that their pain had lasted longer than 6 months (median = 8 years, IQR = 3.5–15 years).
Mental health and substance use
A third (32.6%) of participants screened positive for PTSD, 53.3% reported moderate to severe symptoms of clinical depression, and 65.0% reported ever having hallucinations, violent impulses, or a suicide attempt. One-fifth of participants (18.9%) reported ever having had a psychiatric hospitalization. Over a quarter (25.8%) of the participants met AUDIT criteria for at-risk alcohol use. Half (50.6%) met criteria for at-risk use of cocaine, opioids, or amphetamines.
Functional Status and Cognition
Over half (58.4%) of participants had limitations in lower extremity function as measured by SPPB; 38.9% reported difficulty with one or more ADLs and a quarter (25.8%) had cognitive impairment. (Table 1)
Other experiences
Thirty-five participants (10.1%) reported physical abuse in the past six months, and 10.6% reported being incarcerated in jail or prison in the prior six months.
Multiple variable models
Our full model included gender, residential status, health coverage, depressive symptoms, history of hallucinations, violent impulses, or suicide attempt, prior psychiatric hospitalization, cognitive impairment, self-reported coronary artery disease or myocardial infarction, hypertension, asthma/COPD, cancer, and stroke, pain in the past week, health insurance coverage, and physical abuse in the past six months (Table 3). Neither having a regular health care provider, a usual source of care, nor having an alcohol substance use problem was significant at the p<0.2 level.
Table 3.
Negative binomial regression models of factors associated with ED use
| Variable | IRR, bivariate (95% CI)a |
P-value, bivariate |
IRR, full model (95% CI) |
P-value, full model |
IRR, reduced model (95% CI) |
P-value, reduced model |
|---|---|---|---|---|---|---|
|
| ||||||
| Sex | ||||||
| Male | 1.4 (0.8–2.2) | 0.198 | 1.5 (0.9–2.4) | 0.134 | ||
| Residential Statusb | ||||||
| Cohabiter | 1.6 (0.7–3.5) | 0.243 | 1.1 (0.5–2.5) | 0.754 | 1.3 (0.6–2.9) | 0.518 |
| Multiple Institution User | 3.2 (1.5–6.5) | 0.002 | 1.7 (0.8–3.6) | 0.136 | 2.1 (1.0–4.5) | 0.042 |
| Unsheltered | 2.6 (1.3–5.1) | 0.006 | 2.0 (1.0–3.9) | 0.050 | 2.5 (1.3–4.9) | 0.008 |
| Mental Health Status | ||||||
| Moderate to Severe Depressive Symptomatologyc | 1.4 (0.9–2.1) | 0.089 | 0.9 (0.6–1.4) | 0.624 | ||
| History of Hallucinations, Violent Impulses, Suicide Attempt | 1.3 (0.9–2.0) | 0.169 | 0.9 (0.6–1.5) | 0.776 | ||
| Past Psychiatric Hospitalization | 1.7 (1.0–2.8) | 0.039 | 1.7 (1.0–3.0) | 0.052 | 1.7 (1.0–2.8) | 0.038 |
| Cognitive Impairmentd | 1.5 (1.0–2.4) | 0.075 | 1.5 (1.0–2.4) | 0.062 | ||
| Medical Conditione | ||||||
| Asthma/Chronic Obstructive Pulmonary Disease | 1.4 (0.9–2.2) | 0.149 | 1.1 (0.7–1.7) | 0.809 | ||
| Cancer | 0.5 (0.2–1.3) | 0.147 | 0.6 (0.2–1.4) | 0.206 | ||
| Coronary Artery Disease/Myocardial Infarction | 1.9 (1.0–3.8) | 0.050 | 2.0 (1.0–4.0) | 0.042 | ||
| Stroke | 1.8 (1.0–3.4) | 0.051 | 1.0 (0.5–2.0) | 0.917 | ||
| Pain, Past Weekf | ||||||
| Mild/Moderate | 0.9 (0.5–1.5) | 0.687 | 0.7 (0.4–1.2) | 0.237 | 0.7 (0.4–1.3) | 0.246 |
| Severe | 1.8 (1.1–2.8) | 0.012 | 1.6 (1.0–2.6) | 0.058 | 1.6 (1.0–2.6) | 0.051 |
| Physical Abuse, Past 6 Monthsg | 1.8 (1.0–3.4) | 0.071 | 1.6 (0.8–3.0) | 0.159 | ||
| Any Health Insurance Coverageh | 2.7 (1.6–4.4) | <.001 | 2.3 (1.3–4.0) | 0.004 | 2.6 (1.5–4.4) | <.001 |
incidence rate ratio (IRR); 95% confidence interval (95% CI)
Residential status defined as primary living environment in the past 6 months as determined using cluster analysis; Newly Homeless used as reference residential status category
Moderate to severe depressive symptomatology defined as a Center for Epidemiologic Studies Depression Scale score of ≥22
Cognitive impairment defined as Modified Mini-Mental State Examination score below the 7th percentile (i.e., 1.5 standard deviations below the demographically-adjusted cohort mean)
Medical conditions assessed by self-report of having received a diagnosis from a physician
Pain assessed using the Brief Pain Inventory; mild to moderate (score of 1–7), severe (score of 8–10)
Physical abuse defined as experiencing physical violence perpetrated by another person using an object or being slapped, hit, punched, kicked, choked, or burned
Health insurance coverage includes Medicaid; Medicare; Alameda HealthPAC, county-run health plan covering low-income residents not eligible for Medicaid; or any other kind of private or public health plan
In our reduced model, we found that, compared to the newly homeless, being a multiple institution user (IRR = 2.1; 95% CI = 1.0–4.5), and being unsheltered (IRR = 2.5; 95% CI = 1.3–4.9) was associated with a higher rate of ED visits in the prior six months, as was having health insurance/coverage (IRR= 2.6, 95% CI = 1.5–4.4). Having a lifetime history of psychiatric hospitalization (IRR = 1.7; 95% CI 1.0–2.8) and reporting severe pain in the prior week (pain score ≥8) (IRR = 1.6; 95% CI 1.0–2.6) were also associated with ED visits. Neither functional nor cognitive impairments, any of the chronic diseases, nor a history of physical abuse was associated.
Discussion
We found, in a sample of adults 50 and older experiencing homelessness, half had visited an ED in the prior six months. This rate is higher than rates of ED use in the general population: in 2014, 18% of the adult general population aged 18–64 visited the ED one or more times over the course of a year.56 In our study, a small proportion of individuals accounted for half of all visits. As in other studies looking at homeless individuals, despite the social deprivation and poor functional status of participants, the proportion of visits leading to hospitalization was lower than the national average.15,57,58
While all participants were homeless at study entry, a small group had spent the majority of the prior six months housed, corresponding with the period of interest. We found that those who had spent the majority of the past six months homeless, either unsheltered or staying in homeless shelters, had significantly higher rates of use than those who had spent most of their time housed. This finding is consistent with research that shows that homeless individuals who regain housing have lower rates of ED use than those who remain homeless.59 Although homelessness is a dynamic process,24 prior studies of the healthcare utilization of people experiencing homelessness have not measured exposure to homelessness during the period of interest, nor did they account for the different ways that individuals could experience homelessness.4,60,61 Our findings suggest that classifying individuals as homeless based on a single point in time may oversimplify the contribution of homelessness to individuals’ use of acute health care services.
We found that severe pain was associated with an increased rate of ED use. Over three-quarters of participants who reported severe pain reported that this pain had lasted at least six months, throughout the duration of the study period. In addition, a quarter of participants with one or more ED visits reported using the ED for complaints related to a chronic illness. These findings suggest that the ED remains a low-barrier access point to seek pain and medical treatment for homeless individuals. Although over two-thirds of the participants reporting having a regular non-ED place for care, neither this nor having a regular provider was associated with use of the ED. Prior literature has found that homeless individuals that have a regular place for healthcare still visit the ED.62 Homeless individuals can face barriers to accessing non-ED ambulatory care, even with an identified primary care provider,17,63,64 and this may contribute to their use of the ED for chronic medical conditions and pain that might otherwise be managed in outpatient settings.
We found an association with a lifetime history of psychiatric hospitalization, but not psychiatric symptoms or substance use problems. Prior literature on homeless adults has found associations with prior psychiatric hospitalizations and ED visits for physical health.25,65,66 In keeping with prior literature, we did not find a high rate of ED visits for mental health problems. The literature on substance use problems as a risk factor for ED visits in homeless adults is mixed.4,65,66 It is possible that in a sample with high prevalence of substance use problems, we were unable to detect an association, or that substance use problems are not associated with ED use among homeless adults over the age of 50.
We found that having health care coverage (both insurance and pre-ACA coverage via the county) was associated with higher rates of ED use. It may be that having coverage indicates a higher degree of engagement with health care, resulting in an effect-cause relationship between ED use and insurance: in Alameda County, eligibility workers in clinics and EDs will link uninsured individuals with insurance at the time of a visit. It may also be that insured individuals in the cohort understood their insurer would cover the cost of their ED visit, whereas uninsured individuals can be subject to large bills.
Limitations
Our study had several limitations. We chose to use a conservative measure of ED visits and include only visits for which we had a hospital record, which may have led to underreporting. However, we took measures to limit missing data. For the most commonly used ED, which accounted for 48.9% of self-reported visits, we accessed complete administrative data. For all other EDs, we requested records only if a participant reported that he or she had been there (or, in the case of three partner hospitals, at any of the three hospitals) in the prior six months. Many of our measurements spanned the same 6-month look-back period as our primary outcomes of interest (ED use). However, in a few cases (PTSD, depressive symptoms, pain), we evaluated measurements on the day of the interview or for a shorter period to correspond with validated measures. We conducted this study in a single city, Oakland. In Alameda County, the county that includes Oakland, approximately 4,000 individuals experience homelessness on a given night, half of whom live in Oakland. Oakland is a mid-sized city (population 400,000) with a diverse population. Oakland has homeless services health clinics, free and low-cost meal programs, and mobile outreach services for homeless individuals, and these characteristics may prevent our findings from being generalized to other jurisdictions. Like many cities across the United States, in the years prior to the study initiation, Oakland’s housing prices increased, placing more individuals at risk of homelessness. While less expensive than other cities in the SF Bay area, Oakland was beginning to experience a period of dramatic rental cost increases during the period of the study recruitment. Our study population was predominantly African American, and this may have limited our ability to detect racial or ethnic differences among study participants. We relied on participants to self-report chronic disease and did not verify these diagnoses with medical records. While all participants were homeless at the time of study entry, we measured ED use in the prior six months, when some participants were not homeless. However, this has allowed us to compare those who spent most of their nights homeless to those who did not.
Conclusions
In this study of adults aged 50 and older who were homeless at study entry, we found that those who were homeless throughout the prior six months had significantly higher rates of ED use than those who had spent much of the prior six months housed. We found elevations in risk of ED use both for those who were unsheltered and those who spent their time in shelters and other institutional settings. Homeless adults who are over age 50 have high rates of ED use when compared to the general population.56,60 The high proportion of visits for chronic disease and pain-related complaints and low likelihood of admission could suggest that outpatient non-ED health care resources for homeless individuals are not easily accessible for people experiencing homelessness, leading individuals to seek out care in the ED for complaints that may be manageable in non-ED settings. This could be due to hours of operation, the need for appointments, the lack of transportation options, or other reasons. Future research should evaluate the impact of accessible and culturally acceptable non–ED alternative sites of care for older homeless individuals. Decreasing homelessness would likely decrease ED use in at-risk populations.
Acknowledgments
Funding Sources: This study was funded by grants from the National Institute on Aging (NIA): R01AG041860 [Kushel, Ponath, Guzman], K24AG046372 [Kushel, Guzman and Tieu], and P30AG044281 [Kushel] and the Agency for Healthcare Research and Quality (AHRQ) under award number K12HS021700 [Raven]. These funding sources had no role in the preparation, review, or approval of the manuscript and do not necessarily represent the official views of the NIH or AHRQ.
The authors gratefully acknowledge their colleagues Angela Allen, Pamela Olsen, Nina Fiellin, Tauni Marin, and Kenneth Perez for their invaluable contributions to the HOPE HOME study. The authors also thank the staff at St. Mary’s Center, and the HOPE HOME Community Advisory Board for their guidance and partnership.
Footnotes
Conflicts of Interest: Dr. Kushel is a member of the leadership board of Everyone Home, which seeks to end homelessness in Alameda County, CA. No other conflicts of interest were reported.
Author Contributions:
Drs. Raven and Kushel and Mr. Guzman had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Drs. Raven and Kushel and Mr. Guzman
Acquisition of data: Dr. Kushel and Ms. Ponath
Statistical analysis: Mr. Guzman and Dr. Lee
Analysis and interpretation of data: Drs. Raven and Kushel and Mr. Guzman
Drafting of the manuscript: Dr. Raven and Ms. Tieu
Critical revision of the manuscript for important intellectual content: Dr. Kushel, Mr. Guzman, Dr. Lee, Ms. Ponath
References
- 1.McInnes DK, Petrakis BA, Gifford AL, et al. Retaining homeless veterans in outpatient care: a pilot study of mobile phone text message appointment reminders. American journal of public health. 2014;104(Suppl 4):S588–94. doi: 10.2105/AJPH.2014.302061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hwang SW, Henderson MJ. Health Care Utilization in Homeless People: Translating Research into Policy and Practice: Agency for Healthcare Research and Quality. 2010 [Google Scholar]
- 3.Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department's frequent users. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2000;7:637–46. doi: 10.1111/j.1553-2712.2000.tb02037.x. [DOI] [PubMed] [Google Scholar]
- 4.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. American journal of public health. 2002;92:778–84. doi: 10.2105/ajph.92.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai J, Rosenheck RA. Risk factors for ED use among homeless veterans. The American journal of emergency medicine. 2013;31:855–8. doi: 10.1016/j.ajem.2013.02.046. [DOI] [PubMed] [Google Scholar]
- 6.Pines JM, Asplin BR, Kaji AH, et al. Frequent users of emergency department services: gaps in knowledge and a proposed research agenda. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2011;18:e64–9. doi: 10.1111/j.1553-2712.2011.01086.x. [DOI] [PubMed] [Google Scholar]
- 7.Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS medicine. 2008;5:e225. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beijer U, Andreasson S. Gender, hospitalization and mental disorders among homeless people compared with the general population in Stockholm. European journal of public health. 2010;20:511–6. doi: 10.1093/eurpub/ckq033. [DOI] [PubMed] [Google Scholar]
- 9.Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric syndromes in older homeless adults. Journal of general internal medicine. 2012;27:16–22. doi: 10.1007/s11606-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mackelprang JL, Graves JM, Rivara FP. Homeless in America: injuries treated in US emergency departments, 2007–2011. International journal of injury control and safety promotion. 2014;21:289–97. doi: 10.1080/17457300.2013.825631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frencher SK, Jr, Benedicto CM, Kendig TD, Herman D, Barlow B, Pressley JC. A comparative analysis of serious injury and illness among homeless and housed low income residents of New York City. The Journal of trauma. 2010;69:S191–9. doi: 10.1097/TA.0b013e3181f1d31e. [DOI] [PubMed] [Google Scholar]
- 12.Kushel MB, Evans JL, Perry S, Robertson MJ, Moss AR. No door to lock: victimization among homeless and marginally housed persons. Archives of internal medicine. 2003;163:2492–9. doi: 10.1001/archinte.163.20.2492. [DOI] [PubMed] [Google Scholar]
- 13.Topolovec-Vranic J, Ennis N, Colantonio A, et al. Traumatic brain injury among people who are homeless: a systematic review. BMC public health. 2012;12:1059. doi: 10.1186/1471-2458-12-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kramer CB, Gibran NS, Heimbach DM, Rivara FP, Klein MB. Assault and substance abuse characterize burn injuries in homeless patients. Journal of burn care & research : official publication of the American Burn Association. 2008;29:461–7. doi: 10.1097/BCR.0b013e31817112b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torchalla I, Strehlau V, Li K, Krausz M. Substance use and predictors of substance dependence in homeless women. Drug and alcohol dependence. 2011;118:173–9. doi: 10.1016/j.drugalcdep.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Gilchrist G, Morrison DS. Prevalence of alcohol related brain damage among homeless hostel dwellers in Glasgow. European journal of public health. 2005;15:587–8. doi: 10.1093/eurpub/cki036. [DOI] [PubMed] [Google Scholar]
- 17.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. Jama. 2001;285:200–6. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 18.Han B, Wells BL. Inappropriate emergency department visits and use of the Health Care for the Homeless Program services by Homeless adults in the northeastern United States. Journal of public health management and practice : JPHMP. 2003;9:530–7. doi: 10.1097/00124784-200311000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Opening Doors Federal Strategic Plan to Prevent and End Homelessness 2010. Washington, D.C.: United States Interagency Council on Homelessness; 2010. [Google Scholar]
- 20.Gelberg L, Linn LS, Mayer-Oakes SA. Differences in health status between older and younger homeless adults. Journal of the American Geriatrics Society. 1990;38:1220–9. doi: 10.1111/j.1532-5415.1990.tb01503.x. [DOI] [PubMed] [Google Scholar]
- 21.Garibaldi B, Conde-Martel A, O'Toole TP. Self-reported comorbidities, perceived needs, and sources for usual care for older and younger homeless adults. Journal of general internal medicine. 2005;20:726–30. doi: 10.1111/j.1525-1497.2005.0142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen CI. Aging and Homelessness. The Gerontologist. 1999;39:5–15. doi: 10.1093/geront/39.1.5. [DOI] [PubMed] [Google Scholar]
- 23.Definition of homelessness. 111th Congress ed: U.S. Congress; 2009. Homeless Emergency Assistance and Rapid Transition to Housing Act of 2009. PL 111-22, Sec 1003. [Google Scholar]
- 24.Opening Doors: Federal Strategic Plan to Prevent and End Homelessness As Amended in 2015. Washington, D.C.: United States Interagency Council on Homelessness; 2015. [Google Scholar]
- 25.Ku BS, Scott KC, Kertesz SG, Pitts SR. Factors associated with use of urban emergency departments by the U.S. homeless population. Public health reports (Washington, DC : 1974) 2010;125:398–405. doi: 10.1177/003335491012500308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burnam MA, Koegel P. METHODOLOGY FOR OBTAINING A REPRESENTATIVE SAMPLE OF HOMELESS PERSONS - THE LOS-ANGELES SKID ROW STUDY. Eval Rev. 1988;12:117–52. [Google Scholar]
- 27.Carpenter WT, Gold JM, Lahti AC, et al. Decisional capacity for informed consent in schizophrenia research. Archives of General Psychiatry. 2000;57:533–8. doi: 10.1001/archpsyc.57.6.533. [DOI] [PubMed] [Google Scholar]
- 28.National Health Interview Survey (NHIS) Adult Access to Health Care and Utilization. Hyattsville, Maryland: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2012. [Google Scholar]
- 29.Tsemberis S, McHugo G, Williams V, Hanrahan P, Stefancic A. Measuring Homelessness and Residential Stability: The Residential Time-Line Follow-Back Inventory. Journal of Community Psychology. 2007;35:29–42. [Google Scholar]
- 30.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 32.Prins A, Ouimette P, Kimerling R, et al. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- 33.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977:385–401. [Google Scholar]
- 34.Cheng ST, Chan AC. The Center for Epidemiologic Studies Depression Scale in older Chinese: thresholds for long and short forms. International journal of geriatric psychiatry. 2005;20:465–70. doi: 10.1002/gps.1314. [DOI] [PubMed] [Google Scholar]
- 35.Haringsma R, Engels GI, Beekman AT, Spinhoven P. The criterion validity of the Center for Epidemiological Studies Depression Scale (CES-D) in a sample of self-referred elders with depressive symptomatology. International journal of geriatric psychiatry. 2004;19:558–63. doi: 10.1002/gps.1130. [DOI] [PubMed] [Google Scholar]
- 36.Burt M, Aran L, Douglas T, Valente J, Lee E, Iwen B. Technical Report. Washington, DC: The Urban Institute; 1999. Homelessness: Programs and the People they Serve: Findings from the National Survey of Homeless Assistance Providers and Clients. [Google Scholar]
- 37.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. World Health Organization; 2001. [Google Scholar]
- 38.Humeniuk R, Henry-Edwards S, Ali R, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for use in primary care. Geneva: World Health Organization; 2010. [Google Scholar]
- 39.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. Journal of the American Geriatrics Society. 1983;31:721–7. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 40.Health and Retirement Study. Section G: Functional Limitations and Helpers. Ann Arbor, MI: University of Michigan Institute for Social Research; 2012. [Google Scholar]
- 41.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–8. [PubMed] [Google Scholar]
- 42.Bravo G, Hebert R. Age- and education-specific reference values for the Mini-Mental and modified Mini-Mental State Examinations derived from a non-demented elderly population. International journal of geriatric psychiatry. 1997;12:1008–18. doi: 10.1002/(sici)1099-1166(199710)12:10<1008::aid-gps676>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 43.Bland RC, Newman SC. Mild dementia or cognitive impairment: the Modified Mini-Mental State examination (3MS) as a screen for dementia. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2001;46:506–10. doi: 10.1177/070674370104600604. [DOI] [PubMed] [Google Scholar]
- 44.Vasunilashorn S, Coppin AK, Patel KV, et al. Use of the Short Physical Performance Battery Score to predict loss of ability to walk 400 meters: analysis from the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2009;64:223–9. doi: 10.1093/gerona/gln022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gielen AC, McDonnell KA, Wu AW, O'Campo P, Faden R. Quality of life among women living with HIV: the importance violence, social support, and self care behaviors. Soc Sci Med. 2001;52:315–22. doi: 10.1016/s0277-9536(00)00135-0. [DOI] [PubMed] [Google Scholar]
- 46.Gielen AC, O'Campo PJ, Faden RR, Kass NE, Xue X. Interpersonal conflict and physical violence during the childbearing year. Soc Sci Med. 1994;39:781–7. doi: 10.1016/0277-9536(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 47.Atkinson TM, Rosenfeld BD, Sit L, et al. Using confirmatory factor analysis to evaluate construct validity of the Brief Pain Inventory (BPI) Journal of pain and symptom management. 2011;41:558–65. doi: 10.1016/j.jpainsymman.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miaskowski C, Penko JM, Guzman D, Mattson JE, Bangsberg DR, Kushel MB. Occurrence and characteristics of chronic pain in a community-based cohort of indigent adults living with HIV infection. The journal of pain : official journal of the American Pain Society. 2011;12:1004–16. doi: 10.1016/j.jpain.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee CT, Guzman D, Ponath C, Tieu L, Riley E, Kushel M. Residential patterns in older homeless adults: Results of a cluster analysis. Soc Sci Med. 2016;153:131–40. doi: 10.1016/j.socscimed.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Danseco ER, Holden EW. Are There Different Types of Homeless Families? A Typology of Homeless Families Based On Cluster Analysis. Family Relations. 1998;47:159–65. [Google Scholar]
- 51.Huntington N, Buckner JC, Bassuk EL. Adaptation in Homeless Children: An Empirical Examination Using Cluster Analysis. American Behavioral Scientist. 2008;51:737–55. [Google Scholar]
- 52.Kuhn R, Culhane DP. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: results from the analysis of administrative data. American journal of community psychology. 1998;26:207–32. doi: 10.1023/a:1022176402357. [DOI] [PubMed] [Google Scholar]
- 53.Doupe MB, Palatnick W, Day S, et al. Frequent users of emergency departments: developing standard definitions and defining prominent risk factors. Ann Emerg Med. 2012;60:24–32. doi: 10.1016/j.annemergmed.2011.11.036. [DOI] [PubMed] [Google Scholar]
- 54.Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48:1–8. doi: 10.1016/j.annemergmed.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 55.Statistical Analysis System (SAS) 9.4. Cary, NC: SAS Institute; [Google Scholar]
- 56.Gindi RM, Black LI, Cohen RA. Reasons for Emergency Room Use Among U.S. Adults Aged 18–64: National Health Interview Survey, 2013 and 2014. National health statistics reports. 2016:1–16. [PubMed] [Google Scholar]
- 57.Pearson DA, Bruggman AR, Haukoos JS. Out-of-hospital and emergency department utilization by adult homeless patients. Ann Emerg Med. 2007;50:646–52. doi: 10.1016/j.annemergmed.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 58.Gindi RM, Cohen RA, Kirzinger WK. Emergency Room Use Among Adults Aged 18–64: Early Release of Estimates From the National Health Interview Survey, January–June 2011. Atlanta, GA: National Center for Health Statistics; 2012. [Google Scholar]
- 59.Brown RT, Miao Y, Mitchell SL, et al. Health Outcomes of Obtaining Housing Among Older Homeless Adults. American journal of public health. 2015;105:1482–8. doi: 10.2105/AJPH.2014.302539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brown RT, Kiely DK, Bharel M, Grande LJ, Mitchell SL. Use of acute care services among older homeless adults. JAMA internal medicine. 2013;173:1831–4. doi: 10.1001/jamainternmed.2013.6627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bharel M, Lin WC, Zhang J, O'Connell E, Taube R, Clark RE. Health care utilization patterns of homeless individuals in Boston: preparing for Medicaid expansion under the Affordable Care Act. American journal of public health. 2013;103(Suppl 2):S311–7. doi: 10.2105/AJPH.2013.301421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. Jama. 1994;271:1909–12. [PubMed] [Google Scholar]
- 63.Fryling LR, Mazanec P, Rodriguez RM. Barriers to Homeless Persons Acquiring Health Insurance Through the Affordable Care Act. The Journal of emergency medicine. 2015;49:755–62.e2. doi: 10.1016/j.jemermed.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hwang SW, Bugeja AL. Barriers to appropriate diabetes management among homeless people in Toronto. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2000;163:161–5. [PMC free article] [PubMed] [Google Scholar]
- 65.Cheung A, Somers JM, Moniruzzaman A, et al. Emergency department use and hospitalizations among homeless adults with substance dependence and mental disorders. Addiction science & clinical practice. 2015;10:17. doi: 10.1186/s13722-015-0038-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lin WC, Bharel M, Zhang J, O'Connell E, Clark RE. Frequent Emergency Department Visits and Hospitalizations Among Homeless People With Medicaid: Implications for Medicaid Expansion. American journal of public health. 2015;105(Suppl 5):S716–22. doi: 10.2105/AJPH.2015.302693. [DOI] [PMC free article] [PubMed] [Google Scholar]