Abstract
Objective
This scoping review aimed to summarize the existing knowledge base regarding depression and depressive symptoms in pediatric TBI and to identify gaps in the literature in an effort to guide future research.
Method
Medline Ovid and PsycINFO Ovid databases were each searched by the authors using search terms intended to identify any original research study that examined depressive symptoms in children (i.e., ages 0–18 years) with TBI.
Results
A total of 14 published studies were included in the review. The studies included examined the prevalence of depression, risk factors associated with depression, and depression as a predictor of other TBI-related outcomes.
Conclusion
Existing research suggests that depressive symptoms are more common in a TBI population compared to a healthy or orthopedically injured population. Injury-related factors such as lesions in the brain and the presence of pain, as well as non-injury factors such as older age at injury and low socioeconomic status, may be predictive of depressive symptoms. Depression is likely a secondary outcome of pediatric TBI rather than a direct result of the injury itself. Overall, a relative dearth of research exists on this topic; thus, the review concludes by proposing future research directions.
Keywords: traumatic brain injury, depression, child, pediatric, outcome, review
Introduction
Traumatic brain injury (TBI) is a significant health concern among children and adolescents.1 Over half a million children present to the emergency department for TBI-related visits in the United States, annually,2 with highest incident rates seen in children aged 0–4 years3 and adolescents aged 15–19 years.2 A large body of research has focused on understanding factors related to risk, prognosis, and outcomes following TBI in children and youth.
Pediatric TBI is associated with an array of negative outcomes, including impaired cognitive and academic abilities,4 social impairments,5 and behavioural problems.6 Another outcome often associated with TBI in children is depression. Studies have estimated the rate of depression in children post-TBI to be as high as 33–50%.7,8 Depression is characterized by chronic low mood that can be recurrent in nature.9 Type and severity of symptoms of depression can vary widely, though often include low mood, feelings of worthlessness, weight loss/weight gain, anhedonia, sleeping more or less than usual, and/or recurrent thoughts of death.10 Importantly, depression is a significant risk factor for suicide in children, and estimates indicate that suicide is the third leading cause of death among children aged 10–14 years.11 With a lifetime prevalence of approximately 11% in children 13 to 18 years of age,12 coupled with a high prevalence in children with TBI, depression represents a significant health concern in this population.
Research on depression in the general population suggests that an earlier age of onset results in greater severity and impairment,13 and that more severe first episodes can result in recurrent depression.14 Furthermore, depression is often complicated by a high comorbidity with other disorders. For example, anxiety and conduct disorder are associated with an estimated 4-fold increase in risk for major depressive disorder in adolescents.12 The risk for comorbid disorders is further compounded within medical populations.
The relationship between TBI and depression, while not well understood in children, has been more widely studied among adults. Studies have suggested that the emergence of depression after adult TBI may be physiological in nature, perhaps due to the disruption of neural circuits (e.g., limbic-frontal circuitry15) or post-traumatic changes of neurotransmitters in the brain (see Jorge & Robinson16 for a review). However, less is known regarding the mechanisms responsible for the occurrence of depression in children after TBI.
We identified only two systematic reviews that have been conducted to date that examine psychosocial outcomes, including depressive symptoms, in pediatric TBI. One examined outcomes within 2-years post-injury and identified only three studies that reported on depressive symptomatology.17 The second review was limited to outcomes in children with mild TBI.18 Notably, both reviews found depressive symptoms to be more common among children with TBI than non-head injured control groups. However, a review focusing exclusively on depressive symptoms in children across all TBI severities that includes studies examining long-term outcome (i.e., greater than 2 years) has yet to be published.
Therefore, the overall goal of this scoping review was to examine the literature pertaining to depression and depressive symptoms in childhood TBI in order to summarize the existing knowledge base as well as to identify areas requiring further research. Specifically, we aimed to examine the rates of depressive disorder and/or depressive symptoms in this population, pre- and post-injury risk factors associated with depressive symptoms following TBI, the role of depressive symptoms as risk factors for other functional outcomes following TBI, and to elucidate whether depressive symptoms are a primary or secondary outcome following TBI.
One challenge to studying depression in children following TBI is the substantial overlap between symptoms that often occur after TBI, often called post-concussive symptoms (PCS), and those that define depression (e.g., difficulty concentrating, fatigue, and irritability). A second challenge in the study of depression in childhood TBI is the hetereogeneity in outcomes associated with TBI. TBI ranges in severity from mild to severe, and severity often predicts outcomes in a dose-response fashion; however, outcomes are also impacted by pre- and post-injury psychosocial factors.19 Thus, our review attempts to explore whether depressive symptoms exceed or differ from those that occur after TBI, as well as whether depressive symptoms vary across TBI severities.
For the purposes of this review, depressive symptoms refer to any symptoms listed in the Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition20 and/or Fifth Edition21 under the category of Major Depressive Disorder (e.g., low mood, anhedonia, fatigue, feelings of worthlessness, difficulty thinking, thoughts of death or suicide). Depression, as described in this review, refers either to a diagnosis of a depressive disorder or to scores on self/parent report measures of depressive symptoms in the clinically significant range, as specified by the authors of the identified study.
Method
The review procedure adhered to Arksey and O’Malley’s22 methodological framework for scoping reviews. Specifically, the procedure was as follows: (1) identified the research question, (2) performed a literature search to locate relevant studies, (3) selected studies pertaining to our research question, (4) charted the data, and (5) collated, summarized, and reported the results.
In September 2016, searches of Medline Ovid and PsycINFO Ovid were conducted with the following keywords: ((depression OR mood disorder OR affective disorder OR low mood) AND (children OR adolescent OR pediatric OR paediatric) AND (TBI OR traumatic brain injury)) OR ((brain injuries OR brain concussion OR brain injury, chronic) AND (child, preschool OR child OR paediatric OR adolescent) AND (depression OR low mood)) OR ((traumatic brain injury OR brain injury) AND child AND (depression OR low mood)). Review articles (i.e., scoping reviews, systematic reviews, meta analyses) as well as articles written in languages other than English were excluded from the review.
Following the initial search, titles were scanned and articles were selected based on relevance to the topic. The selected studies were then exported from the database to an Excel file, where abstracts were read to ensure relevance to the review, based on the following inclusion criteria: (a) participants must be 18 years of age or younger at the time of study; (b) participants must have suffered a TBI (i.e., no other type of acquired brain injury); (c) the study must have included a measure of depression, and (d) the study of depression must have pertained to children in the study (i.e., not parents). Studies for which a specific measure of depression was not derived (e.g., examined internalizing symptoms that encompassed both anxiety and depressive symptoms) were excluded. Following abstract review, 31 studies were selected for full text review. During the full text review, 17 were excluded due to not meeting inclusion criteria. Thus, the full text review resulted in a final inclusion of 14 articles. Figure 1 outlines the literature search process.
Figure 1.
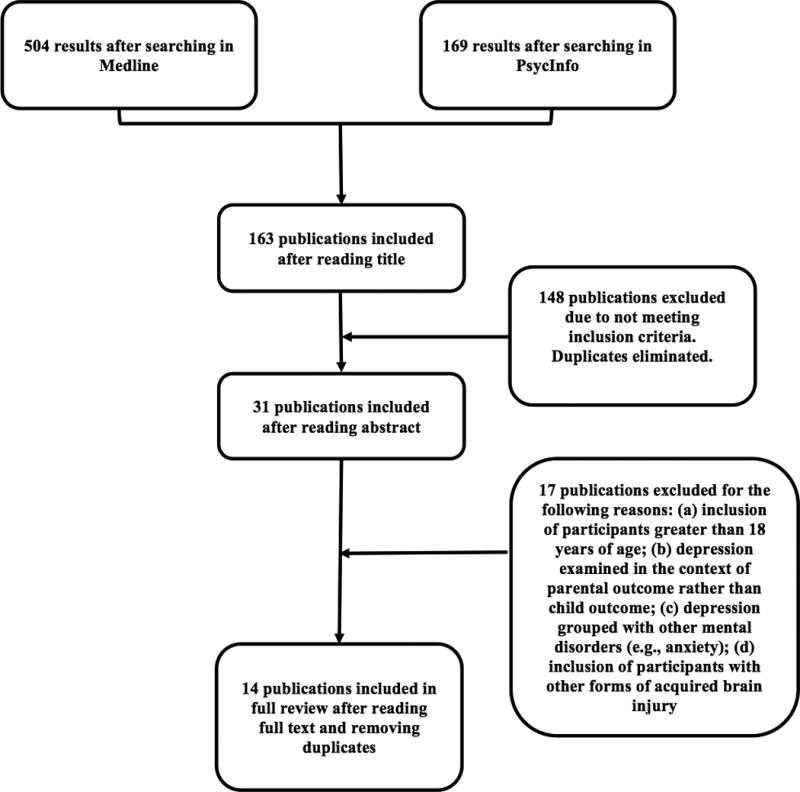
Literature review process.
Results
Study characteristics
An overview of the aims, methodology, and key findings of each of the 14 studies is provided in Table 1. The countries where studies were conducted included the United States of America (9), Canada (2), United Kingdom (2), and Australia (1), and the dates of publication ranged from year 2000 to 2015. All publications were original research studies, of which 7 recruited participants retrospectively (4 studies with cross-sectional designs, 3 studies with longitudinal designs) and 7 employed a prospective, longitudinal design. Participants ranged in age from 0 to 18 years (one study specified an age range of 0–18 years in the study inclusion criteria but did not specify the exact age range of the sample analysed; the age range of all other studies was 5 to 18 years), and severity of TBI ranged from mild to severe. The Glasgow Coma Scale (GCS23) was used to classify injury severity in 13 studies (one study relied solely on self-report of history of a concussion). Mild TBI was defined as a GCS score of 13–15; moderate TBI was defined by (a) a GCS score of 9–12, or (b) a GCS score of 13–15 if accompanied by neuroimaging findings; severe TBI was defined as a GCS score of 8 or less, or (b) a GCS score of 6–12 with accompanied endotracheal intubation, mechanical ventilation, and admission to a pediatric intensive care unit. Five studies included a control group (orthopaedic injury or healthy control). Nine different parent/self-report measures were used to rate depression (see Table 1). Only one study utilized both self-and parent-report measures of depression, whereas 11 studies included self-report only and 2 studies included parent-report only.
Table 1.
Overview of studies included in scoping review
| Author, year, country |
Aims | Study design | Study population | Measured variables |
Main findings* |
|---|---|---|---|---|---|
| Peterson et al24, 2015; USA |
|
|
Children (N = 278) with mild TBI Age = 8–17 years (M = 14.63, SD = 2.24) Norming sample: normative rates of at risk or clinical range scores. | BASC-2 Depression Scale (parent report) |
|
| Tham et al25, 2015; USA |
|
Study materials (instructions, questionnaires, electronic sleep diary, and sleep watch) were mailed to participants. Sleep diary was completed twice daily. Sleep was monitored for 10 days. | Adolescents (N = 100) with mild TBI (n = 50) and healthy controls (n = 50) Age = 12–18 years (M = 15.6, SD = 2.0) | CES-D, NRS, ASWS, PSA, actigraphy sleep assessment |
|
| Keightley et al38, 2014; Canada | Examine and compare working memory performance and related brain activity using fMRI in concussed youths and healthy age-matched controls. | Participants completed tasks assessing working memory while undergoing fMRI. Study included administration of a self-report measure of depression. | Adolescents (N = 30) with mild TBI (n = 15) and healthy controls (n = 15) Age = 10–17 years (mild TBI M = 14.47, SD = 2.29; healthy controls M = 14, SD = 2.3) | BDI total score |
|
| Chrisman et al26, 2013; USA | Examine the prevalence of depression in youth with a history of concussion using a nationally representative sample. | Phone survey asking parents if their child had ever been diagnosed with depression and/or brain injury or concussion. | Children (N = 36,060) Group 1: Age 12–14 years Group 2: Age 15–17 years | Presence of concussion and current diagnosis of depression, age, sex, parental mental health |
|
| Smyth et al28 2013; Canada | Investigated the relationship between the HTR1A G (−1019) allele, depression, childhood life stressors, and PCS after pediatric mild TBI. | Participants recruited prospectively from a database. PCS, depression, stressful life events, and DNA were analyzed. PCSI was administered 7–10 days post injury and then again with all other questionnaires 1–3 years post-injury. | Children (N = 89) with symptomatic mild TBI (n = 47) or asymptomatic mild TBI (n = 42) Age = 0–18 years (symptomatic M = 14, SD = 3.3; asymptomatic M = 13.6, SD = 3.1) | CDI, PCSI |
|
| Tham et al29, 2013; USA |
|
Assessments were conducted at enrolment and at 3, 12, 24, and 36 months after TBI. One parent and the adolescent completed a battery of questionnaires on pain, depressive symptoms, posttraumatic stress disorder symptoms, and HRQOL by mail or via phone interview. | Adolescents (N = 144) with mild TBI (n = 119), moderate TBI (n = 22), or severe TBI (n = 3) Age = 14–17 years (M = 15.70, SD = 1.20) | PHQ-9, persistent pain, HRQOL |
|
| Max et al30, 2012; USA | Examine the demographic, psychosocial, and lesion predictors, as well as the occurrence and phenomenology of new onset depressive symptomatology in children after TBI. | Measures were administered at baseline to record pre-injury diagnoses and repeated 6 months post-injury to record new-onset diagnoses. MRI was conducted 3 months post-injury. | Children (N = 141) with mild TBI (n = 69), moderate TBI (n = 18), or severe TBI (n = 54) Age = 5–14 years (M = 10.13, SD = 2.77) | Age at injury, family history of anxiety or mood disorder, personality change due to TBI, pre-injury anxiety disorder, lesions on MRI, K-SADS-PL, NPRS |
|
| O’Connor et al27, 2012; USA |
|
Baseline assessment battery administered by phone in the weeks following the injury (median = 37 days), in which parents and children were asked to rate pre-injury functioning. Phone or online follow-up assessments with parent and child were conducted at 3, 12, and 24 months post-injury. | Adolescents (N = 228) with mild TBI I (no intracranial haemorrhage, n = 125), mild TBI II (presence of intracranial haemorrhage, n = 33), moderate to severe TBI (n = 31), and arm-injured controls (n = 39) Age = 14–18 years (M = 15.88, SD = 0.93) | PHQ-9, UCLA PTSD reaction index for DSM-IV-R, PedsQL (parent report), FAD-GF (parent report) |
|
| Slawik et al32, 2009; UK | Examine whether individuals with severe TBI with raised intracranial pressure (ICP) immediately after the injury exhibit dysfunction in executive tasks. | At an average of 3.9 years post-injury, participants were administered a battery of neuropsychological tests focused on prefrontal function and underwent MRI. | Children (N = 33) with severe TBI who had ICP (n = 13) or no ICP (n = 20) Median age = 15.2 years, interquartile range = 8.4–13.0 | BDI-Y |
|
| Calvert et al33, 2008; UK | Determine if KOSCHI score at hospital discharge relates to measures of injury severity, cognition, behaviour/emotional status, health status, and HRQOL. | Participants were assessed for TBI severity at admission to hospital. Two follow-up assessments completed at 3- and 6- months post-injury. | Children (N = 81) with mild TBI (n = 37), moderate TBI (n = 15), or severe TBI (n = 29) Age = 5–16 years (M = 11.8) | KOSCHI, BDS |
|
| Wade et al39, 2008; USA |
|
Children with TBI and their families underwent a baseline assessment in the first session and then went on to complete 16 TOPS online, self-guided sessions (which required family involvement). | Children (N = 9) with moderate TBI (n = 7) or severe TBI (n = 2) sustained within the past 24 months, and their families Age = 11–18 years (M = 15.04) | CDI – 10 item short-form |
|
| Wade et al40, 2005; USA | Examine the feasibility and efficacy of a self-guided web-based family intervention for children with TBI. | Children with TBI and their families underwent assessment in the first session and at the 6 week follow-up. The family completed the self-guided materials on the provided website and weekly sessions with a therapist were conducted. | Children (N = 6) with moderate TBI (n = 2) or severe TBI (n = 4) sustained within the past 15 months, and their families Age = 5–16 years (M = 10.5, SD = 3.62) | CDI – 10 item short-form |
|
| Mather et al34, 2003; Australia | Examine the frequency and course of PTSD and comorbid psychological symptomatology in children and adolescents with and without mild TBI as a result of traffic accidents. | Examined symptoms of depression and PTSD at 6 weeks post-accident and again at 13 weeks post-accident. | Children (N = 43) involved in traffic accidents with mild TBI (n = 14) and without mild TBI (n = 29) Age = 6–15 years (M = 9.7, SD = 2.5) | CDI |
|
| Kirkwood et al31, 2000; USA | Examine the prevalence and correlates of depression following childhood TBI using child and parent ratings of depressive symptoms. | Children rated post-injury depressive symptoms at baseline (shortly after injury), as well as 6 and 12 months post-injury. Parents rated children's pre-injury functioning at baseline and their post-injury functioning at the 6 and 12 month follow-ups. | Children (N = 144) with moderate TBI (n = 51) or severe TBI (n = 38), and orthopedically-injured controls (n = 55) Age = 6–12 years (moderate TBI M = 9.87, SD =1.91; severe TBI M = 9.68, SD = 2.16; orthopaedic injury M = 9.40, SD =1.91) | Race, SES, FAD-GF, time since injury, CDI |
|
ANOVA = analysis of variance; ASWS = Adolescent Sleep Wake Scale; BASC-2 = Behaviour Assessment System for Children – Second Edition; BDI = Beck Depression Inventory; BDI-Y = Beck Depression Inventory – Youth; BDS = Birleson Depression Scale; CDI = Children’s Depression Inventory; CES-D = Center for Epidemiological Studies Depression Scale; DSM-IV-R = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Revised; FAD-GF = McMaster Family Assessment Device, General Functioning subscale; fMRI = functional magnetic resonance imaging; HRQOL = Health-Related Quality of Life; K-SADS-PL = Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version; KOSCHI = King’s Outcome Scale for Childhood Head Injury; NPRS = Neuropsychiatric Rating Schedule; NRS = Numerical Rating Scale; OI = orthopaedic injury; PCS = post-concussive symptoms; PCSI = Post-Concussion Symptom Inventory; PedsQL = Pediatric Quality of Life Inventory; PHQ-9 = Patient Health Questionnaire–9; PSA = Pre-Sleep Arousal; PTSD = post-traumatic stress disorder; SES = socioeconomic status; TBI = traumatic brain injury
p < .05 interpreted as significant
Prevalence and risk of depression following TBI
Four studies reported the prevalence of depression among children between the ages of 8 to 18 years with a history of TBI at varying time points post-injury. Prevalence of depression in the TBI population was reported to range from 5.3 to 36%, depending on the time of assessment, assessment instrument, and TBI severity. Among children with mild TBI, prevalence was estimated to range from 5.3% at 4–26 weeks post-injury (M = 8.21, SD = 4.7124) to 36% at 5–12 months post-injury (M = 8.7, SD = 1.725). Compared to risk rates for clinically elevated symptoms of depression in a normative sample, Peterson et al24 reported no significant differences in parent-reported depression risk for those with mild TBI. Conversely, Chrisman et al26 reported that a history of mild TBI corresponded with a 3.2-fold greater risk for depression, compared to those who had never sustained a mild TBI. Finally, O’Connor et al27 reported slightly higher prevalence rates of depression in a mild TBI group (i.e., 6%, 4,%, 5% at 3, 12, and 24 months, respectively) in comparison to the moderate/severe TBI or arm-injured groups, but group differences were not significant. Prevalence rates of depression were not reported in any study for children with TBI under the age of 8 years.
Injury factors associated with depression following TBI
Several studies addressed injury-related risk factors associated with the onset of depressive symptoms following TBI. Smyth et al28 examined the association of the presence of post-concussive symptoms (PCS) with risk for depression in children across all ages (i.e., 0 to 18 years) and reported no group differences in rates of depression in those who reported elevated PCS compared to those who did not. On the contrary, Tham et al29 found pain to be associated with significantly higher self-reported depressive symptoms among adolescents (ages 14 to 17 years) with TBI, regardless of severity (i.e., no group differences between mild, moderate, and severe TBI). Only one study examined structural brain changes associated with TBI and their relationship to risk of depression. Specifically, Max et al30 reported lesions in the left inferior frontal gyrus, right frontal lobe white matter, left temporal pole, and left parietal regions to be predictive of depression in children, ages 5 to 14 years, with complicated mild (i.e., neuroimaging findings) to severe TBI. In sum, injury-related factors, such as pain and brain lesions, may be related to an increased risk of depression and/or depressive symptoms in adolescents or in cases of more severe injury (i.e., presence of neuroimaging findings). However, the literature is unclear whether this relationship exists for children of all ages and for TBI of all severities.
Non-injury factors associated with depression following TBI
Pre-injury and non-injury factors were considered in several studies as possible predictors of risk for depression following TBI. Peterson et al24 did not find that a greater number of previous mild TBIs increases the risk for clinical depression. However, one study found age at injury to be predictive of depression. Specifically, Max and colleagues30 reported the incidence of depression to be significantly greater in children who sustained a TBI when 12 years of age or older (18.2% prevalence), compared to those who sustained their injury before 9 years of age (3.5% prevalence). Similar findings were reported by Chrisman et al26 who reported a 1.5-fold increased risk for depression in children aged 15–17 years compared to those aged 12–14 years, even after controlling for previous mild TBI. In children aged 5–14 years, pre-injury family and adaptive functioning, as well as non-injury factors, such as gender, race, and socioeconomic status (SES), were not found to be significantly predictive of the presence of depression among children with mild, moderate, or severe TBI.30 On the contrary, Kirkwood et al31 reported an association between SES and self-reported depressive symptoms among 6 to 12 year-old children with TBI and OI. Specifically, they reported higher SES to be related to fewer depressive symptoms, regardless of injury. They also reported a moderating effect of SES, wherein the presence of depressive symptoms in the severe TBI group relative to the comparison group was more pronounced among children from low SES homes. Additionally, Max et al30 found that a family history of anxiety disorders, but not depressive disorders, was predictive of post-injury depression in children with TBI. In summary, the literature suggests that pre-injury factors may be related to the presence of depression following TBI, but that current environmental factors, such as SES, may be a stronger predictor of depressive symptoms, although their contribution to depressive disorder is unclear.
Effect of depression on other outcomes following TBI
Four studied examined the role of depressive symptoms in predicting other outcomes following TBI. Tham et al25 provided support for the role of self-reported depressive symptoms as a significant predictor of poorer sleep quality among adolescents with mild TBI. Additionally, increased self-reported symptoms of depression were found to be a significant predictor of persistent pain among adolescents with mild, moderate, or severe TBI at 3 months post-injury and poorer health-related quality of life at 36 months post-injury29. Furthermore, O’Connor et al27 found that, among adolescents, increased self-reported depressive ratings 3 months post-injury were associated with poorer school functioning at 12 and 24 months post-injury. Finally, Kirkwood et al31 did not find a significant relationship between self-reported depressive symptoms and intelligence scores at 6 and 12 months post-injury in children aged 6 to 12 years. Taken together, the evidence suggests that depressive symptoms following TBI may place a child at a greater risk for poorer functional outcomes.
Depression as a primary or secondary outcome following TBI
A key goal of this review was to elucidate whether depression is a primary or secondary outcome following TBI in children. That is, do depression/depressive symptoms arise due to changes in the brain related to the TBI itself, or as a result of changes in a child’s experiences post-injury that may make them more prone to depressive symptoms (e.g., missing school, removal from sports teams, decreased interaction with peers)? Several studies included in the review addressed this question, but results were mixed. One approach to determining whether depression is a primary outcome due to brain changes as a result of injury is to compare depressive symptoms in children with differing levels of TBI severity. Max et al30 found no significant differences in injury severity between those with and without depression. A similarly finding was reported by O’Connor et al27, who reported no group differences in rates of depression among children with mild and moderate/severe TBI. In another study, raised intracranial pressure (ICP), a marker of injury severity, was shown to be unrelated to rates of depression among children with severe TBI several years post-injury (M = 3.9; Slawik et al32). Calvert et al33 reported a significant correlation between scores on a measure of head injury severity and level of self-reported depressive symptoms shortly after injury, although the correlation was not significant at 3- and 6-month follow-up assessments. Furthermore, Mather et al34 found no significant differences in self-reported depressive symptom ratings between children with and without mild TBI when assessed shortly after involvement in a traffic accident, suggesting that the role of a traumatic event may be more predictive of depressive symptoms than TBI. Although Max et al30 found structural changes in the brain to be associated with depressive symptoms, it is difficult to know whether the structural differences were related to the injury itself, were pre-existing, or were related to non-injury factors. Thus, the existing research tends to suggest that depression is a secondary rather than primary outcome of TBI.
Discussion
The current scoping review sought to examine the state of the literature regarding depression and/or depressive symptoms in pediatric TBI. The quality of the studies included varied in terms of design (i.e., cross-sectional, longitudinal), sample size, comparison group, and measurement of depression. Overall, the relative dearth of research in this area reflects significant gaps in our understanding of depression after childhood TBI, although several key issues were elucidated by the existing research.
First, depressive symptoms do appear to be more common in children with TBI than in the general healthy or non-head injured population (e.g., Peterson et al24; Tham et al25). The question of whether depression as a clinical diagnosis (i.e., major depressive disorder; MDD) is more common, however, was not answered by this review, mainly because of inconsistencies in the definition of depression (i.e., symptoms vs. disorder). Few studies defined depression in terms of the DSM-5 definition of MDD (see APA10) or used structured psychiatric interviews to make a formal diagnosis. Given that symptoms of depression are so varied, studies of individual symptoms of depression can result in substantial variability in research results, hampering inferences regarding prevalence. Thus, although children with a history of TBI may be more likely to report increased depressive symptoms, we cannot conclude whether they are at a greater risk for a clinical diagnosis of MDD. Consequently, our findings should be taken to describe the risk of depressive symptoms associated with pediatric TBI, and not necessarily clinical depression. Additionally, little consensus exists regarding the risk for depression in the short-term (e.g., within the first year post-TBI) versus long-term (e.g., 5 years post-TBI). Future studies should therefore aim to examine the prevalence of MDD diagnoses in children following TBI by employing prospective, longitudinal designs using structured interviews at different times post-injury.
Secondly, several injury and non-injury factors were identified that contribute to the risk for depression or depressive symptoms following childhood TBI. Injury-related factors, such as presence of pain29 or brain lesions,30 were found to be associated with an increased risk for depressive symptoms, although relevant findings were limited to two studies and were contradicted by a third (i.e., Smyth et al28). Although older age at injury appears to be a risk factor for depression after TBI, other non-injury factors, such as SES and family history of psychiatric disorders, are less well understood in terms of their relationship to depression. Whether children from low SES environments or with a family history of psychiatric disorders who develop depression after TBI would have done so absent the TBI remains uncertain. Perhaps sustaining a TBI pushes them over the threshold between prodromal symptoms and clinical diagnosis. More research is needed to better understand both the injury and non-injury related factors associated with increased risk for depression after TBI, as well as their interactions with age and the mechanisms behind these relationships.
A third issue this review addressed was the relationship of depression to TBI as a primary versus secondary outcome. If depression were a primary outcome, then the level of depressive symptoms should be worse among those with more severe TBI (i.e., more brain damage); however, the available research does not support a strong relationship in this regard. Depression might be a primary outcome following TBI in the early stages post injury (as reported by Calvert et al33), but the long-term associations remain unclear. Whether the risk for depression is due to interruptions of neural circuits18 or hormonal changes,19 as suggested in adult populations, or whether it is secondary to changes in the child’s experiences or perceptions thereof, represents an area requiring further research. Studies that examined the relationship of depression to other outcomes of TBI (e.g., quality of life29; school functioning27) indicated that depression is predictive of other outcomes, but the causal direction of these relationships was not addressed. Mostly likely, the effects are bidirectional. Furthermore, factors such as age at injury and the family environment may interact with injury severity to predict depression. Nonetheless, taken together, the existing literature suggests that depression is largely a secondary outcome of childhood TBI, though further research is needed before any definitive conclusion can be drawn.
Several methodological limitations of the extant literature were highlighted by this review. One is the relative lack of attention to the effects of age on both symptoms of depression and the effects of TBI. Older age at injury was found to be predictive of greater risk for depression30. However, symptoms as well as etiology of depression likely differ between younger and older children.35,36 Therefore, age at injury should be examined as a moderator of risk factors related to depression and depressive symptoms in TBI. Furthermore, children under the age of 8 years are scarcely represented in the existing literature; thus this population would benefit from future study. Another limitation involves the measures used to assess depression. These measures are not specifically normed on TBI populations; thus, the problem of overlap between TBI-related and depressive symptoms becomes a significant methodological challenge. Future studies would benefit from factoring out symptoms that may be related to TBI to better understand depression-specific symptomatology (e.g., persistent low mood, feelings of worthlessness) in TBI.
In summary, this scoping review provides insights into the status of existing research regarding depression and/or depressive symptoms in pediatric TBI. The results suggest that children who sustain a TBI are at an increased risk for depressive symptoms, and that several injury and non-injury factors may predict this risk. However, literature in this area is scarce, and several unanswered questions remain regarding the risk factors associated with depression, as well as the mechanisms behind these relationships. Furthermore, the quality of the existing studies is varied, and the use of combined multi-informant (e.g., parent and child ratings) and multimodal assessments (e.g., self-report and structured interview) to better inform findings is limited. More research is thus required to better understand these associations, particularly given the high prevalence of depressive symptoms associated with TBI in children, as well as the risk of suicidality associated with childhood depression in the general population.37 Directing research towards untangling the complexities of this issue can help guide treatments with the goal of producing better functional outcomes for children who sustain a TBI.
Acknowledgments
Source of Funding: The first author received funding from Alberta Innovates – Health Solutions in the form of a graduate studentship. No direct sources of funding supported this article.
Footnotes
Conflicts of Interest: The authors do not disclose any conflicts of interest including financial, consultant, institutional, and other relationships that might lead to bias or conflict of interest.
References
- 1.Langlois JA, Rutland-Brown W, Thomans KE. The incidence of traumatic brain injury among children in the United States: Differences by race. J Head Trauma Rehabil. 2005;20(3):229–238. doi: 10.1097/00001199-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002–2006. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]
- 3.Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–548. doi: 10.1097/00001199-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Ewing-Cobbs L, Prasad MR, Kramer L, et al. Late intellectual and academic outcomes following traumatic brain injury sustained during early childhood. J Neurosurg. 2006;105(4 Suppl):287–296. doi: 10.3171/ped.2006.105.4.287. (2006) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeates KO, Swift E, Taylor HG, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10(3):412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems after pediatric traumatic brain injury: Prevalence, predictors, and correlates. J Pediatr Psychol. 2003;28(4):251–263. doi: 10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- 7.Brown G, Chadwick O, Shaffer D, Rutter M, Traub M. A prospective study of children with head injuries: III. Psychiatric sequelae. Psychol Med. 1981;11(1):63–78. doi: 10.1017/s0033291700053289. [DOI] [PubMed] [Google Scholar]
- 8.Max JE, Smith WL, Jr, Sato Y, et al. Traumatic brain injury in children and adolescents: Psychiatric disorders in the first three months. J Am Acad Child Adolesc Psychiatry. 1997;36(1):94–102. doi: 10.1097/00004583-199701000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Bockting CL, Hollon SD, Jarrett RB, Kuyken W, Dobson K. A lifetime approach to major depressive disorder: The contributions of psychological interventions in preventing relapse and recurrence. Clin Psychol Rev. 2005;41:16–26. doi: 10.1016/j.cpr.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] National Center for Injury Prevention and Control, CDC; [Accessed January 8, 2017]. http://www.cdc.gov/injury/wisqars/index.html. Published 2011, 2013. Updated December 22, 2016. [Google Scholar]
- 12.Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major depression in the National Comorbidity Survey – Adolescent Supplement: Prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37–44.e2. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pettit JW, Lewinsohn PM, Roberts RE, Seeley JR, Monteith L. The long-term course of depression: Development of an empirical index and identification of early adult outcomes. Psychol Med. 2009;39(3):403–412. doi: 10.1017/S0033291708003851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Leary D, Costello F, Gormley N, Webb M. Remission onset and relapse in depression: An 18-month prospective study of course for 100 first admission patients. J Affect Disord. 2000;57(1–3):159–171. doi: 10.1016/S0165-0327(99)00086-5. [DOI] [PubMed] [Google Scholar]
- 15.Chen J-K, Johnston KM, Petrides M, Ptito A. Neural substrates of symptoms of depression following concussion in male athletes with persisting post-concussion symptoms. Arch Gen Psychiatry. 2008;65(1):81–89. doi: 10.1001/archgenpsychiatry.2007.8. [DOI] [PubMed] [Google Scholar]
- 16.Jorge R, Robinson RG. Mood disorders following traumatic brain injury. Int Rev Psychiatry. 2003;17:311–324. doi: 10.1080/09540260310001606700. [DOI] [PubMed] [Google Scholar]
- 17.Trenchard SO, Rust S, Bunton P. A systematic review of psychosocial outcomes within 2 years of paediatric traumatic brain injury in a school-aged population. Brain Injury. 2013;27(11):1217–1237. doi: 10.3109/02699052.2013.812240. [DOI] [PubMed] [Google Scholar]
- 18.Emery CA, Barlow KM, Max JE, Villaviencencio-Requis A, Gnanakumar V, Robertson HL, Schneider K, Yeates KO. A systematic review of psychiatric, psychological, and behavioural outcomes following mild traumatic brain injury in children and adolescents. The Canadian Journal of Psychiatry. 2016;61(5):259–269. doi: 10.1177/0706743716643741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor HG, Yeates KO, Wade SL, Stancin T, Minich N. A prospective study of long- and short-term outcomes after traumatic brain injury in children: Behaviour and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.) Washington, DC: APA; 2000. [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th ed.) Washington, DC: APA; 2013. [Google Scholar]
- 22.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 23.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 24.Peterson RL, Connery AK, Baker DA, Kirkwood MW. Preinjury emotional-behavioral functioning of children with lingering problems after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2015;27(4):280–286. doi: 10.1176/appi.neuropsych.14120373. [DOI] [PubMed] [Google Scholar]
- 25.Tham SW, Fales J, Palermo TM. Subjective and objective assessment of sleep in adolescents with mild traumatic brain injury. J Neurotrauma. 2015;32:847–852. doi: 10.1089/neu.2014.3559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chrisman SPD, Richardson LP. Prevalence of diagnosed depression in adolescents with history of concussion. J Adolesc Health. 2013;54:582–586. doi: 10.1016/j.jadohealth.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Connor SS, Zatzick DF, Wang J, et al. Association between posttraumatic stress, depression, and functional impairments in adolescents 24 months after traumatic brain injury. J Trauma Stress. 2012;25:264–271. doi: 10.1002/jts.21704. (2012) [DOI] [PubMed] [Google Scholar]
- 28.Smyth K, Sandhu SS, Crawford S, Dewey D, Parboosingh J, Barlow KM. The role of serotonin receptor alleles and environmental stressors in the development of post-concussive symptoms after pediatric mild traumatic brain injury. Dev Med Child Neurol. 2013;56:73–77. doi: 10.1111/dmcn.12263. [DOI] [PubMed] [Google Scholar]
- 29.Tham SW, Palermo TM, Wang J, et al. Persistent pain in adolescents following traumatic brain injury. J Pain. 2013;14(10):1242–1249. doi: 10.1016/j.jpain.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Max JE, Keatley E, Wilde EA, et al. Depression in children and adolescents in the first 6 months after traumatic brain injury. Int J Dev Neurosci. 2012;30:239–245. doi: 10.1016/j.ijdevneu.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirkwood M, Janusz J, Yeates KO, et al. Prevalence and correlates of depressive symptoms following traumatic brain injuries in children. Child Neuropsychol. 2000;6(3):195–208. doi: 10.1076/chin.6.3.195.3157. [DOI] [PubMed] [Google Scholar]
- 32.Slawik H, Salmond CH, Taylor-Tavares JV, Williams GB, Sahakian BJ, Tasker RC. Frontal cerebral vulnerability and executive deficits from raised intracranial pressure in child traumatic brain injury. J Neurotrauma. 2009;26:1891–1903. doi: 10.1089/neu.2009.0942. [DOI] [PubMed] [Google Scholar]
- 33.Calvert S, Miller HE, Curran A, et al. The King’s Outcome Scale for Childhood Head Injury and injury severity and outcome measures in children with traumatic brain injury. Dev Med Child Neurol. 2008;50:426–431. doi: 10.1111/j.1469-8749.2008.02061. [DOI] [PubMed] [Google Scholar]
- 34.Mather FJ, Tate RL, Hannan TJ. Post-traumatic stress disorder in children following road traffic accidents: a comparison of those with and without mild traumatic brain injury. Brain Inj. 2003;17(12):1077–1087. doi: 10.1080/0269905031000114045. [DOI] [PubMed] [Google Scholar]
- 35.Scourfield J, Rice F, Thapar A, Harold GT, Martin N, McGuffin P. Depressive symptoms in children and adolescents: Changing aetiological influences with development. Journal of Child Psychology and Psychiatry. 2003;44(7):968–976. doi: 10.1111/1469-7610.00181. [DOI] [PubMed] [Google Scholar]
- 36.Duggal S, Carlson E, Sroufe L, Edeland B. Depressive symptomatology in childhood and adolescence. Development and Psychopathology. 2001;13(1):143–164. doi: 10.1017/s0954579401001109. [DOI] [PubMed] [Google Scholar]
- 37.Rao U, Weissman MM, Martin JA, Hammond RW. Childhood depression and risk of suicide: A preliminary report of a longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(1):21–27. doi: 10.1097/00004583-199301000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Keightley ML, Singh SR, Chen J-K, et al. A functional magnetic resonance imaging study of working memory in youth after sports-related concussion: Is it still working? J Neurotrama. 2014;31:437–451. doi: 10.1089/neu.2013.3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wade SL, Walz NC, Carey JC, Williams KM. Preliminary efficacy of a web-based family problem-solving treatment program for adolescents with traumatic brain injury. J Head Trauma Rehabil. 2008;23:369–377. doi: 10.1097/01.HTR.0000341432.67251.48. [DOI] [PubMed] [Google Scholar]
- 40.Wade SL, Wolfe CR, Brown TM, Pestian JP. Can a web-based family problem-solving intervention work for children with traumatic brain injury? Rehabil Psychol. 2005;50:337–345. doi: 10.1037/0090-5550.50.4.337. [DOI] [Google Scholar]


