Abstract
Objective
To analyse the role and meaning of health information in individuals’ experiences with either breast, colorectal or prostate cancer in order to better understand unmet information needs of people with a cancer diagnosis.
Design
This is a secondary analysis of data from a qualitative interview study including narrative interviews and maximum variation sampling. A thematic analysis was conducted, followed by an in-depth analysis based on the principles of grounded theory.
Setting
Interviewees were sought across Germany through self-help organisations, primary care clinics, rehabilitation facilities, physicians and other healthcare professionals to develop cancer modules for the website krankheitserfahrungen.de (illness experiences.de).
Participants
Women with a diagnosis of breast cancer, individuals with a diagnosis of colorectal cancer and men with a diagnosis of prostate cancer.
Results
The meaning and role of information in the illness experiences were clearly associated with gaining control in a seemingly uncontrollable situation in which others —people, the disease— take over. Four categories characterise the ways in which information helped interviewees to regain a sense of control following a diagnosis of cancer: ‘becoming confident in one’s treatment decision’, ‘taking responsibility for one’s situation’, ‘understanding the consequences of the disease and treatment for one’s life’, and ‘dealing with fear’. There was, however, always a fine line between information seeking and becoming overwhelmed by information.
Conclusions
Information needs to be understood as a management tool for handling the disease and its (potential) consequences. Patients’ unmet needs for information might not be easily solved by a simple increase in the amount of information because emotional support and respect for patient autonomy might also play a role. The evaluation of one’s own information behaviour and the information received is closely linked to how the illness unfolds. This makes it challenging to document unmet information needs and satisfaction with information independent of an individual’s illness trajectory over time.
Keywords: information needs, narrative interviews, cancer patients, coping
Strengths and limitations of this study.
Maximum variation in sociodemographic and medical characteristics of interviewees.
Sample size of 127 participants in narrative interviews.
Comprehensive collection of experiences of men and women with cancer.
Data collection methods captured the role and meaning of health information in the experiences of men and women with cancer.
Aim of the interview study was not primarily to identify or understand information needs.
Introduction
Worldwide, breast and colorectal cancer are the most commonly diagnosed cancer types in women, while prostate and colorectal cancer are the most common among men.1 In Germany in 2013, there were 71 640 new diagnoses of breast cancer in women, 59 620 new cases of prostate cancer in men, and 62 410 new cases of colorectal cancer in men and women. Survival rates differ for the different cancer types, with a 5-year relative survival rate of 88% for breast cancer, 93% for prostate cancer and 63% for colorectal cancer.2
In recent years, evidence has been accumulating that shows that patients with cancer have substantial information needs both during and after treatment,3–5 which often remain unmet. These health information needs relate to medical information about the disease and treatments, issues related to psychosocial support and health behaviour information. A survey study in the USA among cancer survivors identified very high rates of unmet information needs regarding side effects, symptoms, tests and treatments,4 while a survey study in Germany found unmet information needs particularly in the field of psychosocial support.3 These studies have also found that half of the surveyed cancer survivors were unsatisfied with the information they had received.
Longitudinal studies on information needs suggest that information needs rise soon after diagnosis and remain high overall,6 7 although the domains in which information is needed may change depending on time since diagnosis.8 In Halbach et al 6 cohort study of newly diagnosed patients with cancer in Germany, participants indicated high unmet information needs regarding side effects and medication, medical examination results, treatment options, social issues, and health promotion. With the exception of social issues, information needs increased during the first 10 weeks after surgery and remained high.
Unmet information needs seem to be associated with lower levels of quality of life.4 Cancer survivors who were satisfied with the information they had received seemed to have a higher health-related quality of life, less anxiety and less depression.9 Indeed, receiving health information influences illness perceptions, with the perceived receipt of more disease-specific information leading to a feeling of being in control and having a better understanding of the illness.10 For an overall positive effect on illness perceptions, being satisfied with the provided information has been shown to be important.
Much effort has been put into developing and distributing medical information that is easily comprehended by patients.11 This has led to a large amount of available cancer information material of varying quality, distributed in the form of leaflets, through mass media and on the internet.12 In Germany, for example, patient guidelines on 11 cancer types, including breast, prostate and colorectal cancer, have been developed.13 These patient guidelines comprise medical recommendations in easy-to-understand language, communicate the risks and benefits of treatments, and aim to guide patients with cancer through their disease journey. In addition, a range of telephone information Hotlines exist for patients with cancer.14
Despite such efforts to provide health information, both older as well as more recent studies on information needs, unmet needs and satisfaction with information indicate that information provision could be further improved. Why, despite the increasing number of carefully crafted patient information resources, do unmet information needs persist?
The literature on information needs provides us with little insight into the meaning of medical and health information in the experiences of indivdiuals with cancer, and the role information plays in patients’ experiences. In order to understand patients’ information needs better, we therefore need to better understand the role of health information in the narratives of men and women with a cancer diagnosis.
Methods
Study design
This article presents the results of a narrative interview study15 that included women with a diagnosis of breast cancer, men and women with a diagnosis of colorectal cancer, and men with a diagnosis of prostate cancer. Narrative interviews aim to capture individuals’ experiences and meaning-making. The interviews were originally collected for the DIPEx (Database of Individual Patients’ Experiences) project Germany, which runs a website (https://www.krankheitserfahrungen.de) that focuses on health and illness experiences.16 All interviews were pseudonymised. The study was funded by the German Federal Ministry of Health (NKP-332–041) and the German foundation Krebsallianz. Only interviewees who gave written consent for the use of their materials for research have been included in the presented analysis.
Data collection
Men and women with a diagnosis of breast, colorectal or prostate cancer were asked to participate in the DIPEx interview study. Maximum variation sampling17 was used to assure a wide range of selected experiences. Selection criteria included time of diagnosis, treatments conducted, and sociodemographic factors such as living with a partner, having children and living in different parts of Germany. Interviewees were sought across Germany through self-help organisations, primary care clinics, clinics for rehabilitation care, oncologists, family doctors and other healthcare professionals.
All authors are experienced qualitative researchers. The interviewers (YA, SA, MS) and the last author (CH) also have additional training in the DIPEx methodology.
The interviews took place at the home of or at a location chosen by the interviewee. The interviews were filmed and/or audio-recorded. They followed a script, with the first question aimed at beginning a narration. This question was identical across all interviews and was phrased as follows: ‘Maybe you can start by talking about how your life was when you first became aware of the signs of cancer and how it went from there. Take your time and talk about how one thing led to another’. The interviewer did not interrupt the resulting stories. This first interview segment lasted between 10 min and 2 hours. After the initial narrative, interviewers had probing questions regarding the story and additional questions regarding experiences with diagnosis, information seeking, consultation, decision-making and living with cancer. The interview guidelines were developed based on an extensive literature review looking at what is important regarding the respective diseases when one aims to capture the experiences. Interviewing continued until no new themes and experiences were captured in the interviews.
Data analysis
The interviews were transcribed verbatim and entered into the software program MAXQDA for management of the data and analysis. First, the interviews were read and themes were identified across the interviews. Then a theme list was created and interview segments were coded accordingly. Theme summaries were written that included the experiences of all text segments coded under each theme.18 For each theme summary quotes from the interview data were selected that illustrated the experiences discussed.
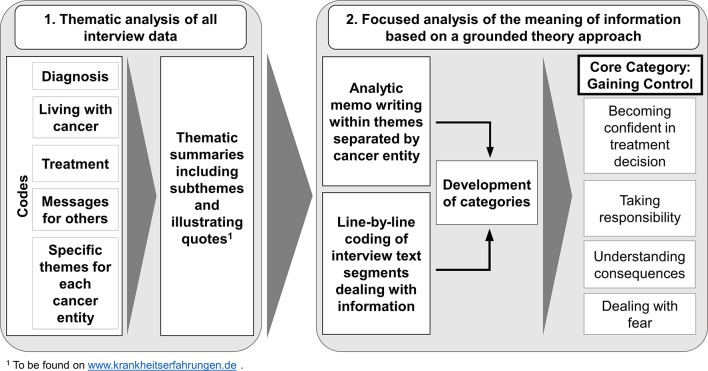
To investigate the meaning of information in the experiences of patients with cancer and those who have had a cancer diagnosis in the past, and to understand the role that information plays in the narratives, we further scrutinised the findings from the thematic analysis of the interviews using an analytical approach derived from grounded theory.19–21 We (CH, SB) read all of the thematic summaries and quotes, as identified by the primary thematic analysis and presented on the website. Then for each of the three cancer entities, analytical memos were written about how information comes into play in the thematic summaries and interview quotes.19 These memos were discussed (CH, SB, MK) and presented to the research team. In addition, quotes that discussed information were scrutinised with line-by-line coding as used in a grounded theory approach,19 with two questions: ‘What is the meaning of this line?’ and ‘What does the statement in this text line stand for?’ This line-by-line coding was done to develop an understanding of the role and meaning of information in the narratives beyond the thematic analysis (figure 1).
Figure 1.
Steps of analysis.
The continued analysis through memo writing and organisation of codes was focused on developing categories that capture the role of information in the narratives. Information played a particular role in the following thematic summaries: for prostate cancer: diagnostic process, living with prostate cancer, education and information seeking, messages; for breast cancer: diagnosis, experience with the healthcare system, information seeking and decision-making, messages; and for colorectal cancer: diagnosis and cause, living with colorectal cancer, information seeking and patient competency, messages.
In order to ensure the quality of the research process and data analysis, the interview guidelines, identified themes and coding trees were compared and discussed within the research group in data meeting sessions. Sampling and theme summaries were discussed in an expert panel that included patients and healthcare providers. Furthermore, the analysis and the data itself were discussed regularly within a qualitative research group at the Institute of Public Health, Charité - Universitätsmedizin Berlin, to ensure agreement on data interpretation and grounding of the analysis in the data. In the following, we present the categories that were identified in order to capture the meaning of information in the interviewees’ experiences.
Results
Sample description
The sample consisted of 127 men and women with either prostate, breast or colorectal cancer (table 1). There was a large variety in terms of age (25–78 years), time since diagnosis (range: 4 weeks–36 years) and type of treatment. Approximately half of our sample was retired at the time of their cancer diagnosis.
Table 1.
Participant characteristics
| Breast cancer (n=43) | Prostate cancer (n=42) | Colorectal cancer (n=42) | |
| Gender | |||
| Women | 43 | 0 | 22 |
| Men | 0 | 42 | 20 |
| Age at diagnosis: range (years) | 25–71 | 47–74 | 25–78 |
| Age categories | |||
| 20–39 | 12 | 0 | 3 |
| 40–49 | 18 | 1 | 5 |
| 50–59 | 10 | 10 | 9 |
| 60–65 | 0 | 19 | 9 |
| >65 | 3 | 12 | 16 |
| Years since diagnosis | |||
| <5 years | 24 | 16 | 20 |
| 5–10 years | 7 | 19 | 12 |
| >10 years | 12 | 7 | 9 |
| Genetic predisposition without a cancer diagnosis | 0 | NA | 1 |
| Working status at diagnosis | |||
| Working | 33 | 19 | 13 |
| Retired | 10 | 23 | 29 |
| Recurrence/metastasis | 12 | 14 | 17 |
| Type of treatment received | |||
| Surgery/mastectomy | 26 | 27 | 40 |
| Chemotherapy | 30 | 5 | 29 |
| Radiation | 31 | 19 | 19 |
| Hormone therapy | 29 | 18 | 0 |
| Antibody therapy | 8 | Unknown | 0 |
| Active surveillance/no treatment | 0 | 3 | 2 |
| Stoma (including return transfer) | 0 | 0 | 26 |
NA, not available.
Role of information in illness narratives
The role that information played in the interviewees’ narratives was mostly about handling the situation of being a patient with cancer and about gaining control in a seemingly uncontrollable situation. Thus information needs to be understood in terms of the special circumstances that patients with cancer are in: a potentially life-threatening situation in which it is assumed that treatment decisions may be decisive in terms of living or dying. Importantly, information helped the interviewees to regain control over their situation and gave them the means to make decisions with which they felt comfortable. On the other hand, when some control and certainty had been regained, information was no longer sought and was sometimes explicitly avoided so as not to challenge this carefully crafted certainty which is under constant threat.
Information had to fulfil special requirements to address the needs of the interviewees. The majority of interviewees mentioned that more than one source of information was necessary ‘to get a complete picture’. Interviewees expressed their desire for trustworthy and reliable information from experts, mostly their physicians, and mentioned a reduction in confidence when they thought that economic interests might guide physicians. Whereas some interviewees talked about their satisfaction with the information they received from their physician, others explicitly looked for additional information from medical studies and meta-analyses.
When talking about information, interviewees acknowledged the importance of encouraging and/or optimistic information for dealing with the disease. A few interviewees, mainly men with a diagnosis of prostate cancer, found the information provided by the physician to be lacking in objectivity and relied on other sources, such as the internet, for information they considered reliable. There was, furthermore, always a fine line between information seeking and becoming overwhelmed by information.
For the interviewed men and women, we identified the following four categories that characterise the ways in which information may help people to regain a sense of control following a diagnosis of cancer: ‘becoming confident in one’s treatment decision’, ‘taking responsibility for one’s situation’, ‘understanding the consequences of the disease and treatment for one’s life’, and ‘dealing with fear’. These four main categories, as identified in the interviews, are presented below. Interview quotes that are representative of the types of quotes found for each particular category can be found in table 2.
Table 2.
Characteristic quotations from the narratives illustrating the four categories of dealing with cancer through information
| Ways of dealing with cancer through information (categories) | Characteristic quotations for the four categories |
| Becoming confident in one’s treatment decision | “And so, okay, then I said: ‘Ok, but I would like to discuss it again with my family doctor’. He said: ‘Of course, obviously’. So I went to my family doctor and discussed it with him. He said: ‘Mr. Weber [pseudomyzed name], I cannot say that you should do this and this. But-’. Essentially I had already decided what I wanted to do, but my family doctor also said that in his opinion this implant would be good. And he also had a patient who’s had it for a long time and was completely satisfied with it. So I said: ‘Ok, I’ll do it.’” (Male, aged 72 years, prostate cancer) “On the topic of wanting a baby, I finally also found some reports of women who said: ‘Yes, I dropped it prematurely [a medication recommended by her physician] and got pregnant’. And these are the things that gave me courage. Because doctors can tell you a whole lot, but ultimately it’s the experiences that count.” (Female, aged 34 years, breast cancer) “Or you hear things left and right, where you think: Well, what to do? Or just the information from the first doctor, who said: ‘Take both breasts off. Do otherwise, and you’re doing it wrong’. The next one says: ‘Hmm, let’s try this’. So now I just go with my gut feeling: ‘I trust him, so that’s alright.’” (Female, aged 54 years, breast cancer) |
| Taking responsibility for one’s situation | “The more you inform yourself and the more you know about the connections, the more qualified you will be for your medical consultants. I have been able to ask quite different questions. I have also been able to discuss things much better with doctors. So I got other answers again. In retrospect, it even happened that I was asked by a physician who was not directly involved, but when talking about my illness: ‘Tell me, are you in the field?’ Whereupon the only answer that came to mind was: ‘No, [but] I have become a professional patient in the meantime’. And you become qualified as a patient, but I think that is also important. It’s up to you. And you have to know everything about it. And you cannot learn enough yourself.” (Male, aged 68 years, colorectal cancer) “So they [the patients] cannot of course develop or suggest the therapy, but they make the decision: ‘I’ll do this therapy because I’ve grappled with it and decided it will help me on the way to recovery’. This is a decision every patient should make for themselves. I am convinced that this therapy will have much more effect when I have decided for it myself. Because of the psychological factor, everyone knows, there are enough studies on placebo effects and so on. This decision, if I can answer clearly for myself with ‘Yes, that’s what I want to do now’, this is incredibly important. And I believe that physicians could also relieve themselves a bit if they would involve the patients more in the decision, and that is simply the right way in terms of how our society is developing.” (Female, aged 51 years, breast cancer) “Well, I got up in the morning two days before the surgery, got dressed and said: ‘I’m going. I’m going to look for someone who has an artificial bowel exit. If you cannot get me that, then I’ll look for myself’. (…) At that moment I said: ‘If so [going for the surgery], then I have to know this. I have to see someone who is living with that thing’. (…) And I was totally amazed how it went. In any case, to get to the point, after this conversation [with a woman with a stoma] it was clear to me: I can deal with it.” (Male, aged 64 years, colorectal cancer) |
| Understanding the consequences of the disease and treatment for one’s life | “And therefore, according to an estimation of the probability, a urologist may say: ‘You don’t have to worry, nothing will happen in the next seven years’. So why chemo, why OP? If the end of life is already settled in this area, then one should live in peace. But if you want to live longer, then you have to, this sounds terribly dramatic, choose life-sustaining measures, and this is what I have done. (…) And the crucial question was: ‘You are now 60 years old, how old do you want to live to?’ And when I said: ‘Yes, my parents are both over 80’, the only conclusion was: ‘Your life expectancy of 20 years, counted from today, leaves the recommendation that you should be operated on’, because it is almost impossible that this cancer will remain so long within the organ. And I would really like to be 80. Therefore I have been operated on.” (Male, aged 66 years, prostate cancer) “But I know that he said: ‘Ninety-nine percent certainty colorectal cancer. And you have two quite uncomfortable years ahead of you’. In retrospect, somebody I told this to, he said: ‘For God’s sake, how can you assault someone like that?’ I must say, in retrospect, I was very grateful to him.” (Female, aged 62 years, colorectal cancer) “Well, now I’m just thinking of course about the debate: Should I be operated on or not? What plays a role, one thing is my strong desire: I simply want to stay healthy and stay intact. And of course, the fear of the side effects of an operation, so the fear of changing or losing my sexuality. I did not really feel the worry of becoming incontinent, somehow I had the feeling that I’m this young, my body will manage. A surgeon had also made it relatively clear that the chances are really quite good. (…).” (Male, aged 48 years, prostate cancer) |
| Dealing with fear | “When the fear comes, there is really no advice one can give. So at that time that book [about a lady who had breast cancer and whom the doctors had given up on] was improbably helpful, she really gave me courage. At first I thought: Is it good to read such a thing? However, it was very good, because she fought like a lion. And that was very good.” (Female, aged 48 years, breast cancer) “No, I did not want to [do Internet research], for the simple reason: In order not to make myself crazy. Because others might describe this or that and have this or that. From my personal experience – I know myself, when I learn about things that others have, then it could happen that I will project it onto myself and perhaps I do not have it at all. And that’s why I did not do that. Protected myself. That was a protection. (…).” (Female, aged 51 years, breast cancer) “So, my prostate cancer education actually only came in the years after. This is really strange, now that you ask. I do not know why I did not ask before. Maybe even from cowardice. That could also be. Maybe I did not really want to know.” (Male, aged 77 years, prostate cancer) “[I searched] On the Internet. But now, in hindsight, I really have to say, there are really quite a few websites that I would not recommend. There really is sometimes, or with some things I have indeed already said: Man, what is written here is in the first place just not medically sound. This will give many patients really a lot of fear. And then I said at some point: No, I’ll let it go. I’ll not look anymore.” (Female, aged 44 years, colorectal cancer) |
Becoming confident in one’s treatment decision
Interviewees had the feeling that mistakes regarding treatment decisions can be avoided, and that in order to avoid mistakes information is needed. The importance of up-to-date information, with the internet as the best source of the most current data, was emphasised by some interviewees. Furthermore, they expressed a need for information that would allow them to evaluate the experience and quality of physicians and healthcare services. Some interviewees also wanted to be reassured about their decision and went for a second opinion, either to another specialist or to a physician they knew, such as their family physician. For others, the assurance of friends and family members regarding the decision about treatment venue was important. The confirmation of others was important to gain or maintain confidence in one’s treatment trajectory.
The interviews demonstrate the difficulties faced by those who held beliefs or treatment preferences that differed from those of their physicians. None of the interviewees felt themselves to be in a situation in which they could simply oppose their healthcare provider. Rather, in such a situation they continued to seek information for healthcare providers that supported their intentions and gave them a sense of authorisation to do what they perceived to be good for them. In general, the cancer trajectory was characterised by phases in which treatment decision-making was ongoing, something that interviewees described as ‘situations of uncertainty’, while phases in which decisions had been made gave orientation and a sense of acceptance. Indeed, some interviewees voiced their strategy of avoiding information or not seeking information from complementary medicine approaches once a treatment decision had been made, as this could potentially lead to a re-emergence of uncertainty.
Finally, in the course of the illness trajectory, for some a sense of and trust in being ‘guided’ by their (lived) bodies emerged, which then replaced the information-seeking behaviour. Interviewees used terms such as ‘gut feeling’ when voicing such sensations of trust and confidence.
Taking responsibility for one’s situation
Information had the function of preparing interviewees for their communications with physicians, other healthcare providers and institutions such as health insurance companies. Whereas some interviewees thought that an informed patient had a better chance of staying healthy, others expressed the need to support their physicians due to their own limitations in knowing what is best. Furthermore, interviewees believed that one can only make decisions if one is knowledgeable in the medical matters at hand. Finally, since the decisions made would influence the trajectory of the cancer journey profoundly, they wanted to be part of it. Thus taking responsibility was an important way of overcoming the feeling of having lost control.
Being an informed patient, according to the interviewees, was therefore a means of taking responsibility for their situation. This also gave them back a sense of control over what was happening to them.
Understanding the consequences of the disease and treatment for one’s life
For the interviewees, information was also a very important means of gauging their situation and understanding the longer term consequences. They were eager to receive information that would help them to assess the meaning of the disease and treatment for their own journey and fate, and to estimate the impact of the disease on their personal lives. Even though some information was perceived as shocking and discouraging by the interviewees, it nevertheless helped them to assess the potential impact.
Furthermore, interviewees mentioned that while superficial and misleading information might be encouraging in the short term, it limited their understanding of how life would be when dealing with the consequences of treatment. Interviewees thus mentioned how hearing about the experiences of others was sometimes necessary to gain a comprehensive picture of the disease’s impact on individuals’ life experiences.
Dealing with fear
Information can be a double-edged sword: although it might give hope, it can also be discouraging. This risk was something that interviewees discussed in their stories. Thus most interviewees had experienced times in which they had sought out information, as well as times when they had tried to avoid receiving more information. If information is important in terms of gaining control over the situation, handling one’s emotions is a crucial aspect of this. Managing and controlling emotions when confronted with a potentially life-threatening disease was mostly done by the interviewees with the help of information. This made it important to be selective in terms of the type of information one reads or listens to. What was selected was closely related to where in the illness trajectory they were positioned at the time and what types of feelings they had at that particular moment. Information could help the interviewees deal with fear because it was uplifting and gave them hope in relation to their own situation, although other information could increase their worries and fears.
Interviewees thus always engaged in a selection of information, although what type of information was considered good or bad for a particular interviewee was entirely dependent on the individual and the particular moment of the disease trajectory that they were in. Some feared information in general at the beginning following their diagnosis, while others tried to gather as much information as possible. Sometimes the interviewees only knew in hindsight that they would have preferred not to have known about or read particular information, and only became more selective with time. The interviewees’ illness experiences therefore also talk about how it is a learning process to know what type of information exists and what may or may not be helpful for the individual.
Discussion and conclusion
Discussion
The meaning and role of information in the narratives of men and women with a diagnosis of either breast, colorectal or prostate cancer were clearly associated with gaining control in a seemingly uncontrollable situation. Information was helpful in terms of strengthening the treatment decision, both when it was congruent to the physician’s suggestions and when it diverged. However, information was not only meaningful for decision-making, but also in terms of learning how to handle the disease and knowing what consequences may arise from the potentially life-threatening diagnosis and the ensuing treatments.
Information in the narratives was about managing the emotions that accompanied the disease and its potential consequences. All types of information—medical, experiential or regarding psychosocial support—could take on such a role in the narratives; what information was better suited to help a person gain control was often dependent on the stage of the disease, the particular situation and the type of person. The need to be selective about what information to hear and trust also presented a means of managing emotion and gaining control.
A diagnosis of cancer represents a life-threatening event that brings individuals into a confusing and uncertain situation that might trigger a rollercoaster of emotions and feelings, including anxiety, fear, hope, helplessness, courage and despair.22 23 Individuals talk about profound shock and fear when faced with a cancer diagnosis.22 24 Many patients associate cancer with death.24 The difficulty in accepting the diagnosis is associated with feelings of anger, a sense of unfairness, stigma and a complete loss of hope.25 In a previous study, Holmberg26 has shown that a breast cancer diagnosis results in an experience of shock and trauma, followed by a situation of existential uncertainty. Fear becomes a part of a woman’s life, and biomedical practices such as regular follow-up care help to control the fear.22 Patients have concerns about death, the unpredictable nature of cancer, and later in their illness trajectory about cancer recurrence.27
In such a situation, information is an essential part of the illness experience as a means of handling the situation. The uncertainty inherent in both a cancer diagnosis and in deciding on treatments means that information is very important, as it allows patients to gain a sense of control and closure about the decisions to be made. The important role of information remains even beyond initial treatment decisions as it is a constant management tool that can be used to gauge and assess the situation in a continued state of uncertainty that may remain for a long time. For this reason, it may well be that in hindsight, once the illness trajectory has advanced, former information provision is seen more critically and other information becomes important.
From the perspective of the narratives of men and women with a diagnosis of cancer, seeking out and finding information is not so much a cognitive activity of intellectual understanding, but is rather a means of coping with the disease and reducing stress.28–30 Information is never a simple or neutral means whereby a patient’s role within healthcare provider–patient interactions is altered,31 32 but is a crucial coping strategy, although one that nevertheless always has a Janus face33 34: information appears as a means of managing emotions, although it can increase or decrease fear according to a number of factors. Given this contingency, the type of information accessed needs to be carefully selected. However, only over the course of the illness trajectory does it become clearer what information would have been good to have at a given point, and what information patients may have been better off without. Thus it is not surprising that information provision may be judged differently in hindsight.
Treatment decision-making is a crucial juncture for patients with cancer, as their decisions will influence their future path. As such, it is not surprising that patients need to become comfortable with their treatment trajectory, regardless of who makes the decision, since in the end they will have to face the consequences of this decision. Active information seeking was most often talked about during phases of the illness when decisions had to be made or bodily symptoms surfaced. Germeni and Schulz33 have suggested that a number of personal and contextual characteristics should be taken into account when evaluating patients’ desires for information and their behaviours in terms of seeking or avoiding information. They highlight how information seeking may complement the physician–patient relationship as a means of becoming comfortable with what is going on.
Indeed, as our results show, information seeking or avoidance behaviours need to be understood in the context of the general situation that patients with cancer are in, and can be seen as a way of gaining control and managing emotions in a seemingly difficult-to-control situation. In line with Lambert et al,35 36 one could argue that the narratives speak about how information is used to self-regulate feelings of uncertainty and control. Similarly, information needs and information-seeking behaviour change over the course of the disease trajectory. Having to make a decision about treatment options is a trigger for information-seeking behaviour.33 36 37 Indeed, as the narratives of our study participants show, in instances in which patients did not feel comfortable following a physician’s suggestions, information seeking became important to help re-enforce patients’ opposing position. In the rare cases where this was not enough, a new physician was sought.
Our paper has several limitations that should be considered when interpreting the results. For this study, we relied on secondary analysis of qualitative data drawn from interviews that focused on the experiences of men and women diagnosed with breast, colorectal or prostate cancer in order to understand the role of information in the experiences of patients with cancer. The original data collection and sampling were, however, focused on capturing as many facets as possible of possible illness experiences of those diagnosed with cancer, and were not geared specifically towards information needs. A study with a particular focus on information needs would have chosen more specific sampling categories accordingly.
For example, information needs may vary by age cohort. Thus in contrast to the study’s sampling strategy, which tried to be as diverse as possible, one might have selected more interviewees in the younger and older age groups in order to investigate possible age effects in terms of the role and meaning of information. Such strategies would have allowed for patterns to emerge regarding how and what type of information is important in different stages of the illness trajectory, and could have allowed for a more nuanced analysis in this respect.
Following the primary thematic analysis in which information had been identified as important, we added a further analysis based on a grounded theory approach to capture the meaning of information. If the interviews had originally been analysed solely on the basis of a grounded theory approach, which is much more open, the derived theoretical understanding might not have developed a core category such as gaining control, and it might have not been information-focused. However, since information has generally been established as important for the health-related quality of life of patients with cancer, it seems safe to say that the meaning of information in terms of gaining control and managing emotions presents an important and valid finding.
Conclusion
Information was never a simple, neutral fact in the interviewees’ narratives, something that was cognitively used to make treatment decisions. Rather, information was crucial as a means of gaining a sense of control in a seemingly uncontrollable situation. Information seeking and avoidance were both means of feeling or becoming comfortable with the chosen treatment trajectory. One could argue that information gathering and/or avoidance should be seen as a means for a patient to strengthen his or her relationship with the physician or the treatment trajectory. Ideally, both belong together. Since information provision is closely tied to treatment decision-making, the patient–physician relationship and coping with the disease, the unmet need for (some) information might not be easily solved by a simple increase in the amount of information provided. Other factors, such as emotional support3 and respect for patient autonomy, might also play a role. The psychosocial care of patients with cancer has improved in the last decades38 and might partially help to close this gap. However, information is closely linked to patients’ relationships with their physicians, and thus delegation of information provision to other care professionals may not always be appropriate. Finally, the evaluation of one’s own information behaviour and the information received change over time and are closely linked to how the illness unfolds. This makes it challenging to document unmet information needs and satisfaction with information independent of the individual illness trajectory.
Practical implications
Based on our findings, we suggest that the role of information, be it medical or otherwise, in the illness experiences of patients with cancer needs to be seen in terms of a coping tool, which influences a patient’s understanding of the disease and a means for managing emotions. Information must be understood as intrinsically entangled in the patient’s cancer trajectory and in his or her interactions with healthcare providers, especially physicians. Methods for developing and evaluating health information tools for patients with cancer and survivors should therefore include domains other than knowledge provision, such as emotional management and gaining control through reassurance, and/or developing an independent stance as a patient.
Supplementary Material
Acknowledgments
We thank all those who agreed to participate in the interviews and who supported us in finding study participants, in particular ‘Bundesverband Prostatakrebsselbsthilfe e.V.’, the Department for Psycho-Oncology of Charité - Universitätsmedizin Berlin, ‘Frauenselbsthilfe nach Krebs e.V.’, ‘Deutsche ILCO e.V.’ and ‘Stiftung Männergesundheit’. We are grateful to the foundation ‘Krebsallianz’, which made the above-presented analyses of the interviews possible. We also acknowledge support from the German Research Foundation (DFG) and the Open Access Publication Fund of Charité - Universtiätsmedizin Berlin to make this article available open access.
Footnotes
Contributors: CH and JM-N developed and conducted the DIPEx oncology study on which the data analysis of this paper is based. CH planned the secondary analysis study. SB and MK analysed the data and wrote the first manuscript. CH and SB interpreted the study results. YA, SA and MS undertook the thematic analysis for the website. All authors discussed and edited the final manuscript.
Funding: Data collection, the thematic analysis of the narratives and their presentation on krankheitserfahrungen.de was funded by the German Federal Ministry of Health (NKP-332-041). The secondary analyses presented in this article were funded by the German foundation Krebsallianz. Open Access publication fees were provided by the German Research Foundation (DFG) and the Open Access Publication Fund of the Charité - Universitätsmedizin Berlin.
Competing interests: None declared.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Ethics approval: DIPEx oncology was approved by the University of Freiburg Ethics Committee (EA/247/12) and was reported to the Charité - Universitätsmedizin Berlin Ethics Committee (EA4/053/12).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Due to data protection restrictions, additional data are not available.
References
- 1.Centers for disease control and prevention. Global cancer statistics. 2012. https://www.cdc.gov/cancer/international/statistics.htm (accessed Mar 2016).
- 2.Robert Koch-Institut. [Cancer in Germany 2016] Zentrum für Krebsregisterdaten im Robert Koch-Instiitut; Berlin, 2016. [Google Scholar]
- 3.Faller H, Koch U, Brähler E, et al. . Satisfaction with information and unmet information needs in men and women with cancer. J Cancer Surviv 2016;10:62–70. 10.1007/s11764-015-0451-1 [DOI] [PubMed] [Google Scholar]
- 4.Kent EE, Arora NK, Rowland JH, et al. . Health information needs and health-related quality of life in a diverse population of long-term cancer survivors. Patient Educ Couns 2012;89:345–52. 10.1016/j.pec.2012.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rood JA, Eeltink CM, van Zuuren FJ, et al. . Perceived need for information of patients with haematological malignancies: a literature review. J Clin Nurs 2015;24:353–69. 10.1111/jocn.12630 [DOI] [PubMed] [Google Scholar]
- 6.Halbach SM, Ernstmann N, Kowalski C, et al. . Unmet information needs and limited health literacy in newly diagnosed breast cancer patients over the course of cancer treatment. Patient Educ Couns 2016;99:1511–8. 10.1016/j.pec.2016.06.028 [DOI] [PubMed] [Google Scholar]
- 7.Matsuyama RK, Kuhn LA, Molisani A, et al. . Cancer patients' information needs the first nine months after diagnosis. Patient Educ Couns 2013;90:96–102. 10.1016/j.pec.2012.09.009 [DOI] [PubMed] [Google Scholar]
- 8.Rutten LJ, Arora NK, Bakos AD, et al. . Information needs and sources of information among cancer patients: a systematic review of research (1980-2003). Patient Educ Couns 2005;57:250–61. 10.1016/j.pec.2004.06.006 [DOI] [PubMed] [Google Scholar]
- 9.Husson O, Mols F, van de Poll-Franse LV. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review. Ann Oncol 2011;22:761–72. 10.1093/annonc/mdq413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Husson O, Thong MS, Mols F, et al. . Illness perceptions in cancer survivors: what is the role of information provision? Psychooncology 2013;22:490–8. 10.1002/pon.3042 [DOI] [PubMed] [Google Scholar]
- 11.Arbeitsgruppe G. [Good practice guidelines for health information]. Z Evid Fortbild Qual Gesundhwes 2016;110-111:85–92. 10.1016/j.zefq.2015.11.005 [DOI] [PubMed] [Google Scholar]
- 12.Viswanath K. Science and society: the communications revolution and cancer control. Nat Rev Cancer 2005;5:828–35. 10.1038/nrc1718 [DOI] [PubMed] [Google Scholar]
- 13.Schaefer C, Zowalla R, Wiesner M, et al. . [Patient guidelines in oncology: objectives, procedures and first experiences with this format]. Z Evid Fortbild Qual Gesundhwes 2015;109:445–51. 10.1016/j.zefq.2015.09.013 [DOI] [PubMed] [Google Scholar]
- 14.Heimer A, Henkel M. [Population’s needs of cancer information: analysis of the information behaviour of people seeking advice. Representative survey commissioned by the Cancer Information Service of the German Cancer Research Centre]. Heidelberg: Akademische Verlagsgesellschaft, 2012. (accessed 10 Mar 2017). [Google Scholar]
- 15.Ziebland S, Hunt K. Using secondary analysis of qualitative data of patient experiences of health care to inform health services research and policy. J Health Serv Res Policy 2014;19:177–82. 10.1177/1355819614524187 [DOI] [PubMed] [Google Scholar]
- 16.Engler J, Adami S, Adam Y, et al. . Using others' experiences. Cancer patients' expectations and navigation of a website providing narratives on prostate, breast and colorectal cancer. Patient Educ Couns 2016;99:1325–32. 10.1016/j.pec.2016.03.015 [DOI] [PubMed] [Google Scholar]
- 17.Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J Adv Nurs 1997;26:623–30. 10.1046/j.1365-2648.1997.t01-25-00999.x [DOI] [PubMed] [Google Scholar]
- 18.Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405–14. 10.1111/j.1365-2929.2006.02467.x [DOI] [PubMed] [Google Scholar]
- 19.Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. CA: SAGE Publications, Inc, 2006. [Google Scholar]
- 20.Gunn CM, Bokhour B, Parker VA, et al. . Exploring explanatory models of risk in breast cancer risk counseling discussions: NSABP/NRG oncology decision-making project 1. Cancer Nurs 2017. 10.1097/NCC.0000000000000517 [Epub ahead of print 28 Jun 2018]. 10.1097/NCC.0000000000000517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strauss A. Qualitative analysis for social scientists. New York: NY: Cambridge University Press, 1987. [Google Scholar]
- 22.Holmberg C. No one sees the fear: becoming diseased before becoming ill--being diagnosed with breast cancer. Cancer Nurs 2014;37:175–83. 10.1097/NCC.0b013e318281395e [DOI] [PubMed] [Google Scholar]
- 23.McCaughan E, McKenna H. Never-ending making sense: towards a substantive theory of the information-seeking behaviour of newly diagnosed cancer patients. J Clin Nurs 2007;16:2096–104. 10.1111/j.1365-2702.2006.01817.x [DOI] [PubMed] [Google Scholar]
- 24.Nanton V, Docherty A, Meystre C, et al. . Finding a pathway: information and uncertainty along the prostate cancer patient journey. Br J Health Psychol 2009;14(Pt 3):437–58. 10.1348/135910708X342890 [DOI] [PubMed] [Google Scholar]
- 25.Chen PY, Chang HC. The coping process of patients with cancer. Eur J Oncol Nurs 2012;16:10–16. 10.1016/j.ejon.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 26.Holmberg C, Brustkrebs D. Eine ethnografische Studie über Krankheit und Krankheitserleben [Diagnosis Breastcancer. An ethnographic study on disease and illness experience]. Frankfurt/New York: Campus-Verlag, 2005. [Google Scholar]
- 27.Kvale EA, Meneses K, Demark-Wahnefried W, et al. . Formative research in the development of a care transition intervention in breast cancer survivors. Eur J Oncol Nurs 2015;19:329–35. 10.1016/j.ejon.2015.01.010 [DOI] [PubMed] [Google Scholar]
- 28.Gonzalez P, Nuñez A, Wang-Letzkus M, et al. . Coping with breast cancer: Reflections from Chinese American, Korean American, and Mexican American women. Health Psychol 2016;35:19–28. 10.1037/hea0000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rains SA, Tukachinsky R. Information seeking in uncertainty management theory: exposure to information about medical uncertainty and information-processing orientation as predictors of uncertainty management success. J Health Commun 2015;20:1275–86. 10.1080/10810730.2015.1018641 [DOI] [PubMed] [Google Scholar]
- 30.van der Molen B. Relating information-needs to the cancer experience. 1. Jenny’s story: a cancer narrative. Eur J Cancer Care 2000;9:41–7. 10.1046/j.1365-2354.2000.00191.x [DOI] [PubMed] [Google Scholar]
- 31.Kvåle K, Bondevik M. What is important for patient centred care? A qualitative study about the perceptions of patients with cancer. Scand J Caring Sci 2008;22:582–9. 10.1111/j.1471-6712.2007.00579.x [DOI] [PubMed] [Google Scholar]
- 32.Shay LA, Lafata JE. Understanding patient perceptions of shared decision making. Patient Educ Couns 2014;96:295–301. 10.1016/j.pec.2014.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Germeni E, Schulz PJ. Information seeking and avoidance throughout the cancer patient journey: two sides of the same coin? A synthesis of qualitative studies. Psychooncology 2014;23:1373–81. 10.1002/pon.3575 [DOI] [PubMed] [Google Scholar]
- 34.Leydon GM, Boulton M, Moynihan C, et al. . Cancer patients' information needs and information seeking behaviour: in depth interview study. BMJ 2000;320:909–13. 10.1136/bmj.320.7239.909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lambert SD, Loiselle CG, Macdonald ME. An in-depth exploration of information-seeking behavior among individuals with cancer: part 2: understanding patterns of information disinterest and avoidance. Cancer Nurs 2009;32:26–36. 10.1097/01.NCC.0000343373.01646.91 [DOI] [PubMed] [Google Scholar]
- 36.Lambert SD, Loiselle CG, Macdonald ME. An in-depth exploration of information-seeking behavior among individuals with cancer: part 1: understanding differential patterns of active information seeking. Cancer Nurs 2009;32:11–23. quiz 24-5. doi 10.1097/01.NCC.0000343372.24517.bd [DOI] [PubMed] [Google Scholar]
- 37.Loiselle CG, Lambert SD, Cooke A. The searching, processing, and sharing of breast cancer information by women diagnosed with the illness. Can J Nurs Res 2006;38:82–104. [PubMed] [Google Scholar]
- 38.Kuhnt S, Mehnert A, Giesler JM, et al. . [The development of quality standards for the psychosocial outpatient care of cancer patients - results of a delphi survey]. Gesundheitswesen 2016. 10.1055/s-0042-100732 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.