Abstract
Objectives
To investigate factors associated with the need for assistance in basic and instrumental activities of daily living in Norwegian elderly.
Design
Prospective cohort study.
Setting
The Nord-Trøndelag Health Study (HUNT), a large population-based health survey in Norway.
Participants
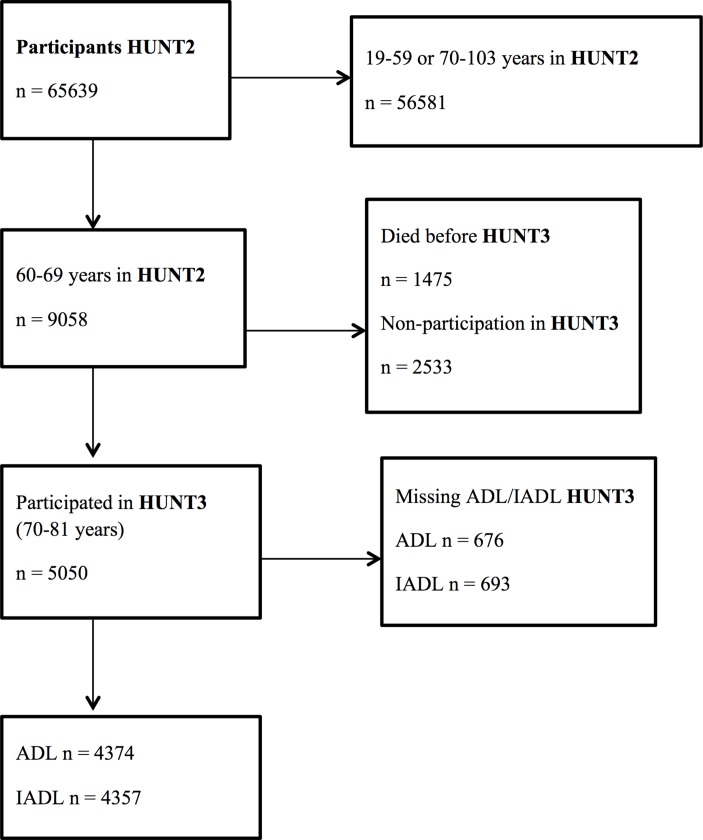
5050 individuals aged 60–69 years old at baseline in HUNT2 (1995–1997) who also participated in HUNT3 (2006–2008) were included in the study. 676/693 individuals were excluded in the analyses due to missing outcomes.
Outcomes
Needing assistance in one or more basic or instrumental activities of daily living reported in HUNT3.
Results
In adjusted multinomial logistic regression analyses, poor self-rated health and depression were the strongest risk factors for needing assistance in one or more basic activities of daily living in HUNT3, with ORs of 2.13 (1.35 to 3.38) and 1.58 (0.91 to 2.73). Poor self-rated health and poor life satisfaction were the strongest risk factors for needing assistance in one or more instrumental activities of daily living in HUNT3, with ORs of 2.30 (1.93 to 2.74) and 2.29 (1.86 to 2.81), respectively. Excessive sitting time, short or prolonged sleeping time, and physical inactivity seemed to be the most important lifestyle risk factors for basic/instrumental activities of daily living (ADL/IADL) disability. The studied factors were, in general, greater risk factors for mortality during follow-up than for ADL/IADL disability. Smoking was the strongest risk factor for mortality during follow-up and non-participation in HUNT3. Smoking and low social participation were the strongest risk factors for non-participation in HUNT3.
Conclusions
Subjective health perception, life satisfaction and depression were the strongest risk factors for needing assistance in one or more basic/instrumental activities of daily living later in life. These factors could be possible targets for prevention purposes.
Keywords: epidemiology, public health, social medicine
Strengths and limitations of this study.
The Nord-Trøndelag Health Study (HUNT) is a large cohort study comprising the whole county of Nord-Trøndelag, Norway, and including a large selection of variables.
Based on emerging risk factors for morbidity and mortality in society, this study incorporates sleep duration and sitting time as risk factors for function in activities of daily living.
This study did not have information on function in activities of daily living at baseline, but the robustness of the results was evaluated through a sensitivity analysis including those with good self-rated health and good life satisfaction at baseline.
The risk factors for disability in daily life activities also increase the risk for non-participation in HUNT3 or mortality during follow-up from HUNT2 to HUNT3; therefore, the competing outcomes were evaluated in a multinomial logistic regression analysis.
Introduction
Most countries are experiencing population ageing, and it is estimated that in 2030 two billion people will be over 60 years old (22% of the world’s population).1 Norway can expect over 1.3 million people over 70 years old and a doubling of the dependency ratio (the ratio of the dependent part of the workforce over the productive part) in 2060.2 The need for healthcare and long-term care increases with age,1 and a quarter of the disease burden occurs among people over 60 years.3 Evidence is equivocal whether there is a compression or expansion of morbidity among the elderly, but increasing prevalence of chronic diseases seems to be a pattern.4 An ageing population is likely to cause increased strain on healthcare systems and increase public expenditures. Thus, it is of interest to maintain good health and high functioning into old age, both for the elderly themselves and for the society as a whole.
Activities of daily living (ADL) is an index used to measure functional capacity.5 It can be divided into basic or personal ADL (ADL) and instrumental ADL (IADL). ADL concerns the abilities necessary for basic functioning, whereas IADL includes functions necessary for living in a community. ADL and IADL disabilities increase with age,4 and in Europe ADL disability has decreased over time,4 6–11 whereas the results for IADL are ambiguous.4 9 12 Women have been found to exhibit higher risk of developing functional disabilities than men,4 6 13–15 but regardless of more ADL disabilities women seem to live longer than men.14 ADL disability and functional decline predict morbidity and mortality,16 as well as nursing home admission and poor outcomes after hospital discharge.17–19 Once disabled, few persons over 85 years regain independent ADL function.20
Meta-analyses and systematic reviews have identified risk factors for functional decline, such as physical inactivity,21–24 depression23 25 and poor self-rated health.23 26 Smoking,23 27 28 alcohol consumption23 27 29–31 and low social participation23 28 32–35 have also been found to be factors for functional decline and ADL and IADL disability, whereas few studies have investigated anxiety in relation to functional decline.23 Further, few studies have investigated the association between quality of life and the need for assistance in ADLs. One Swedish study found that low health-related quality of life was associated with more problems with IADL.36 In addition to the factors mentioned, we wanted to study the association between the new emerging risk factors sleeping time and sitting time and ADL/IADL disability in an elderly Norwegian population. These are known risk factors for mortality and morbidity37–43 and are also likely to be associated with disability, since disability is part of the continuum of population health change from risk factors, diseases, loss of function, disability and mortality.44
The aim of this study was to investigate risk factors for needing assistance in basic and instrumental ADLs among Norwegian elderly by using the Nord-Trøndelag Health Study (HUNT).
Methods
Study population
This study uses data from the HUNT Study. The HUNT Study is a regional health study that has been carried out three times: in 1984–1986, 1995–1997 and 2006–2008. The county of Nord-Trøndelag consists of rural areas and six small towns, but lacks large cities. The average income, prevalence of higher education and prevalence of current smokers are a little lower than in Norway overall.45–47 The population is stable (little inmigration and outmigration) and homogeneous,48 and it is considered to be fairly representative of Norway.46 All inhabitants in the county of Nord-Trøndelag over 20 years of age were invited to participate in the adult part of the HUNT Study. The participants completed questionnaires, undertook various clinical examinations and provided blood samples. The participation rate was 69.5% in HUNT2 and 54.1% in HUNT3.48 Every participant signed a written consent to participate. Details about the HUNT Study are extensively described elsewhere.46 48
The study group selected for this study included participants aged 60–69 years in HUNT2 (1995–1997) who also had completed HUNT3 in 2006–2008 (n=5050). Unfortunately we did not have any information on ADL/IADL status at baseline (in the 60–69 years age group) because questions about ADLs and IADLs in the HUNT Study were only given to participants aged 70 years and older. Choosing an older age group at baseline would have yielded fewer participants and increased the healthy survivor bias. Therefore we selected the 60–69 years age group as baseline in the multinomial logistic regression despite the limitation of not having information on ADL/IADL status at baseline. Those missing information on ADL/IADL at HUNT3 were excluded from the analysis. A flow diagram illustrating the selection of participants is shown in figure 1.
Figure 1.
Flow diagram showing the selection of participants. ADL, activities of daily living; HUNT, Nord-Trøndelag Health Study; IADL, instrumental ADL.
Variables
The wording of all questions and answer categories, as well as further details on the handling of the variables, are presented in online supplementary material 1. The outcomes were defined as needing assistance of another person in one or more ADLs in HUNT3, non-participation in HUNT3, or mortality during follow-up between HUNT2 and HUNT3. Non-participation in HUNT3 was defined as individuals aged 60–69 years old in 1995–1997 participating in HUNT2 but not in HUNT3. The HUNT Study is regularly updated with administrative national records containing information on participant status (died, emigrated, alive), from which we obtained information on mortality.
bmjopen-2017-018942supp001.pdf (112.1KB, pdf)
The independent variables in HUNT2 included lifestyle risk factors, psychological and subjective health perceptions. The lifestyle risk factors were defined as follows: being a daily smoker, participating only a few times a year or never in social activities, sitting 8 hours or more daily, sleeping 6 hours or less or 10 hours or more, less than 3 hours of light physical activity and no hard physical activity a week, and scoring 2 or more (out of 4) on the Cut down, Annoyed, Guilty and Eye opener (CAGE) questionnaire for problematic drinking behaviour.49 The Hospital Anxiety and Depression Scale (HADS) was used to measure anxiety and depression, which consists of a separate score for anxiety and depression. The score was dichotomised, where a score of 8 or more (out of 21) was defined as a case of anxiety or depression.50
Confounders (HUNT2) were constitutional factors such as age, gender, education, marital status and chronic illness. Age was entered as a continous variable, gender had two categories (men and women), education was defined as primary (0–10 years), secondary (11–13 years) or tertiary education (higher education), and marital status was defined as being married or not, whereas chronic illness was self-reported (yes or no).
Statistical calculations
Using multinomial logistic regression models, we investigated the association between lifestyle risk factors (smoking, alcohol, physical inactivity, sitting time, sleep and social participation), depression, anxiety, self-rated health and life satisfaction and the need for assistance from another person in ADLs or IADLs. The average follow-up time between HUNT2 and HUNT3 was 11 years. Separate multinomial logistic regression models were run for each independent variable to investigate the association with ADL and IADL disabilities. Using multinomial regression models allowed the simultaneous examination of competing outcomes mortality during follow-up and non-participation in HUNT3. Those missing information on ADL/IADL at HUNT3 were excluded from the analysis. The analyses were controlled for potential confounders including the constitutional factors age, gender, education, marital status and chronic illness.
Since baseline information on ADL and IADL disability was not available at baseline in the 60–69 years age group (only available for participants over 70 years old), we did a sensitivity analysis to evaluate the robustness of the results by including those answering having good self-rated health and good life satisfaction at baseline. We report Odds Ratios (OR) with 95% confidence intervals (CI). Statistical significance was set at 0.05 (5%). Analyses were carried out in Stata V.14.
Results
Baseline characteristics for participants aged 60–69 years in HUNT2 (1995–1997) who also participated in HUNT3 (2006–2008) are shown in table 1. Valid percentages are shown for the variables and below the response rate (total). Of the 5050 participants, 45.8% were men and 54.2% were women. There were fewer with tertiary education (10.6%) compared with secondary (46.4%) and primary (42.9%). Low social participation (47.2%) and being physically inactive (44.5%) were the most prevalent independent variables, whereas problematic alcohol behaviour (4.8%) was the least prevalent. More participants reported needing assistance from another person in any of the IADLs (19.9%) than in ADLs (2.4%). A total of 20.3% needed assistance in any of the ADL/IADLs. The highest assistance need was reported for doing heavier housework (13.1%), doing the laundry (8.2%) and taking the bus (7.2). There was 0.8%–31.0% missing on the independent variables, most on the questions about problematic alcohol behaviour comprising CAGE. There was 13% missing on the ADL and IADL variables in HUNT3. These cases were excluded from the analysis.
Table 1.
Baseline characteristics of individuals aged 60–69 years old in 1995–1997 participating in the HUNT Study, HUNT2 (1995–1997) and HUNT3 (2006–2008), n=5050
| Independent variables (HUNT2) | n (%) | Adjustment variables (HUNT2) | n (%) | Outcome variables (HUNT3) | n (%) |
| Anxiety | Gender | ADL disability | |||
| HADS-A≤7 | 3471 (88.0) | Women | 2738 (54.2) | Walk | 43 (1.0) |
| HADS-A≥8 | 472 (12.0) | Men | 2312 (45.8) | Toilet | 32 (0.7) |
| Total | 3943 (78.1) | Total | 5050 (100.0) | Wash yourself | 50 (1.2) |
| Depression | Education | Bath/shower | 82 (1.9) | ||
| HADS-D≤7 | 3996 (88.2) | Primary | 2166 (43.0) | Dress | 40 (0.9) |
| HADS-D≥8 | 534 (11.8) | Secondary | 2343 (46.5) | Go to bed and get up | 34 (0.8) |
| Total | 4530 (89.7) | Tertiary | 533 (10.6) | Eat | 22 (0.5) |
| Self-rated health | Total | 5042 (99.8) | No ADL | 4270 (97.6) | |
| Good | 3145 (62.8) | Marital status | Any ADL | 104 (2.4) | |
| Poor | 1864 (37.2) | Married | 4021 (79.8) | Average ADL | 0.02 |
| Total | 5009 (99.2) | Unmarried | 1021 (20.2) | Total | 4374 (86.6) |
| Life satisfaction | Total | 5042 (99.8) | IADL disability | ||
| Good | 4253 (85.8) | Chronic illness | Prepare warm meals | 141 (3.3) | |
| Poor | 702 (14.2) | No | 2378 (50.0) | Do light housework | 76 (1.8) |
| Total | 4955 (98.1) | Yes | 2381 (50.0) | Do heavier housework | 564 (13.1) |
| Daily smoker | Total | 4759 (94.2) | Do the laundry | 347 (8.2) | |
| No | 3997 (80.1) | Pay bills | 168 (3.9) | ||
| Yes | 992 (19.9) | Take the medicines | 56 (1.3) | ||
| Total | 4989 (98.8) | Go out | 69 (1.6) | ||
| Alcohol | Do the shopping | 142 (3.3) | |||
| CAGE≤1 | 3315 (95.2) | Take the bus | 301 (7.2) | ||
| CAGE≥2 | 167 (4.8) | No IADL | 3488 (80.1) | ||
| Total | 3482 (69.0) | Any IADL | 869 (19.9) | ||
| Sleep duration | Average IADL | 0.20 | |||
| 7–9 hours | 3669 (83.0) | Total | 4357 (86.3) | ||
| ≤6/≥10 | 749 (17.0) | ADL/IADL disability | |||
| Total | 4418 (87.5) | No ADL/IADL | 3501 (79.7) | ||
| Sitting time | Any ADL/IADL | 891 (20.3) | |||
| ≤7 hours | 2974 (73.4) | Average ADL/IADL | 0.20 | ||
| ≥8 hours | 1078 (26.6) | Total | 4392 (87.0) | ||
| Total | 4052 (80.2) | ||||
| Social participation | Mortality during follow-up | 1475 | |||
| Participates | 2341 (52.8) | Non-participation in HUNT3 | 2533 | ||
| Seldom, never | 2094 (47.2) | ||||
| Total | 4435 (87.8) | ||||
| Physical activity | |||||
| Active | 2403 (55.5) | ||||
| Inactive | 1928 (44.5) | ||||
| Total | 4331 (85.8) |
ADL, activities of daily living; CAGE, Cut down, Annoyed, Guilty, Eye opener (questionnaire for problematic alcohol behaviour); HADS-A, Hospital Anxiety and Depression Scale-Anxiety; HADS-D, Hospital Anxiety and Depression Scale-Depression; HUNT, Nord-Trøndelag Health Study; IADL, instrumental activities of daily living.
The association between lifestyle risk factors, self-rated health, life satisfaction, anxiety and depression, and the need for assistance in ADLs, mortality during follow-up and non-participation in HUNT3 11 years later is shown in table 2. We report ORs from adjusted multinomial logistic regression analyses. Unadjusted analyses are included in online supplementary material 2. The adjusted analyses show that poor self-rated health and depression were the strongest risk factors for needing assistance in one or more ADLs in HUNT3 (OR=2.13 and 1.58). Short or prolonged sleeping time, smoking and physical inactivity were the most important lifestyle risk factors for needing assistance in ADL (OR=1.50, 1.43 and 1.42). All risk factors except poor self-rated health and short or prolonged sleeping time were stronger risk factors for mortality during follow-up than for being ADL disabled in HUNT3. Smoking was the most important risk factor for mortality during follow-up and non-participation in HUNT3 (OR=2.66 and 2.12). Being a daily smoker and low social participation were the strongest risk factors for non-participation in HUNT3 compared with ADL disability.
Table 2.
ORs from multinomial logistic regression analyses showing the association between lifestyle risk behaviours, self-rated health, life satisfaction, anxiety and depression in participants aged 69–69 years in HUNT2 (1995–1997, baseline) and the need for assistance in basic activities of daily living, mortality during follow-up and non-participation in HUNT3 (2006–2008, main and competing outcomes)
| ADL independent | ADL disability | Mortality during follow-up | Non-participation in HUNT3 | |||||||
| n | n | OR* | 95% CI | n | OR* | 95% CI | n | OR* | 95% CI | |
| Self-rated health | ||||||||||
| Good | 2571 | 40 | 1.00 | Ref | 608 | 1.00 | Ref | 1271 | 1.00 | Ref |
| Poor | 1422 | 55 | 2.13 | (1.35 to 3.38) | 711 | 1.84 | (1.59 to 2.13) | 1014 | 1.23 | (1.09 to 1.38) |
| Total | 7692 | |||||||||
| Depression | ||||||||||
| HADS-D≤7 | 3256 | 71 | 1.00 | Ref | 893 | 1.00 | Ref | 1655 | 1.00 | Ref |
| HADS-D≥8 | 424 | 17 | 1.58 | (0.91 to 2.73) | 218 | 1.62 | (1.34 to 1.96) | 321 | 1.32 | (1.12 to 1.55) |
| Total | 6855 | |||||||||
| Sleep duration | ||||||||||
| 7–9 hours | 3020 | 66 | 1.00 | Ref | 801 | 1.00 | Ref | 1395 | 1.00 | Ref |
| ≤6/≥10 hours | 589 | 22 | 1.50 | (0.91 to 2.46) | 246 | 1.32 | (1.11 to 1.57) | 353 | 1.10 | (0.94 to 1.28) |
| Total | 6492 | |||||||||
| Physical activity | ||||||||||
| Active | 1999 | 39 | 1.00 | Ref | 522 | 1.00 | Ref | 901 | 1.00 | Ref |
| Inactive | 1547 | 43 | 1.42 | (0.91 to 2.23) | 553 | 1.44 | (1.25 to 1.67) | 920 | 1.26 | (1.12 to 1.42) |
| Total | 6524 | |||||||||
| Life satisfaction | ||||||||||
| Good | 3449 | 76 | 1.00 | Ref | 1013 | 1.00 | Ref | 1827 | 1.00 | Ref |
| Poor | 524 | 19 | 1.43 | (0.84 to 2.42) | 277 | 1.67 | (1.40 to 1.98) | 420 | 1.42 | (1.22 to 1.64) |
| Total | 7605 | |||||||||
| Daily smoker | ||||||||||
| No | 3222 | 70 | 1.00 | Ref | 771 | 1.00 | Ref | 1453 | 1.00 | Ref |
| Yes | 760 | 25 | 1.43 | (0.89 to 2.28) | 515 | 2.66 | (2.31 to 3.07) | 764 | 2.12 | (1.88 to 2.39) |
| Total | 7580 | |||||||||
| Sitting time | ||||||||||
| ≤7 hours | 2431 | 56 | 1.00 | Ref | 619 | 1.00 | Ref | 1112 | 1.00 | Ref |
| ≥8 hours | 901 | 25 | 1.23 | (0.76 to 2.01) | 319 | 1.47 | (1.25 to 1.73) | 424 | 1.15 | (1.00 to 1.33) |
| Total | 5887 | |||||||||
| Anxiety | ||||||||||
| HADS-A≤7 | 2889 | 65 | 1.00 | Ref | 776 | 1.00 | Ref | 1341 | 1.00 | Ref |
| HADS-A≥8 | 370 | 10 | 1.10 | (0.55 to 2.21) | 148 | 1.50 | (1.20 to 1.88) | 245 | 1.30 | (1.09 to 1.57) |
| Total | 5844 | |||||||||
| Alcohol | ||||||||||
| CAGE≤1 | 2730 | 66 | 1.00 | Ref | 740 | 1.00 | Ref | 1211 | 1.00 | Ref |
| CAGE≥2 | 132 | 4 | 1.08 | (0.38 to 3.04) | 75 | 1.76 | (1.28 to 2.40) | 73 | 1.30 | (0.96 to 1.76) |
| Total | 5031 | |||||||||
| Social participation | ||||||||||
| Participates | 1939 | 44 | 1.00 | Ref | 413 | 1.00 | Ref | 687 | 1.00 | Ref |
| Seldom, never | 1694 | 43 | 0.94 | (0.60 to 1.46) | 642 | 1.50 | (1.29 to 1.74) | 1063 | 1.62 | (1.44 to 1.84) |
| Total | 6525 | |||||||||
n varies from 5031 to 7692 in the various analyses due to different amounts of missing on the independent variables.
*Adjusted for gender, education, age, marital status and chronic illness.
ADL, activities of daily living; CAGE, Cut down, Annoyed, Guilty, Eye opener (questionnaire for problematic alcohol behaviour); HADS-A, Hospital Anxiety and Depression Scale-Anxiety; HADS-D, Hospital Anxiety and Depression Scale-Depression; HUNT, Nord-Trøndelag Health Study; ref, reference category.
bmjopen-2017-018942supp002.pdf (84.7KB, pdf)
The association between lifestyle risk factors, self-rated health, life satisfaction, anxiety and depression, and the need for assistance in IADLs, mortality during follow-up and non-participation in HUNT3 11 years later is shown in table 3. We report ORs from adjusted multinomial logistic regression analyses. Unadjusted analyses are included in online supplementary material 2. In the adjusted analyses poor self-rated health, poor life satisfaction and depression were the strongest risk factors for needing assistance in one or more IADLs in HUNT3 (OR=2.30, 2.29 and 1.79, respectively). Physical inactivity and excessive sitting time were the most important lifestyle risk factors for needing assistance in IADL (OR=1.61 and 1.40). Smoking was the most important risk factor for mortality during follow-up and non-participation in HUNT3 (OR=2.73 and 2.17). Poor self-rated health and poor life satisfaction were also strong risk factors for mortality during follow-up (OR=2.21 and 2.11). Being a smoker and low social participation were the strongest risk factors for non-participation in HUNT3 compared with IADL disability.
Table 3.
ORs from multinomial logistic regression showing the association between lifestyle risk behaviours, self-rated health, life satisfaction, anxiety and depression in participants aged 69–69 years in HUNT2 (1995–1997, baseline) and the need for assistance in instrumental activities of daily living, mortality during follow-up and non-participation in HUNT3 (2006–2008, main and competing outcomes)
| IADL independent | IADL disability | Mortality during follow-up | Non-participation in HUNT3 | |||||||
| n | n | OR* | 95% CI | n | OR* | 95% CI | n | OR* | 95% CI | |
| Self-rated health | ||||||||||
| Good | 2230 | 371 | 1.00 | Ref | 608 | 1.00 | Ref | 1271 | 1.00 | Ref |
| Poor | 1019 | 451 | 2.30 | (1.93 to 2.74) | 711 | 2.21 | (1.90 to 2.58) | 1014 | 1.46 | (1.29 to 1.66) |
| Total | 7675 | |||||||||
| Depression | ||||||||||
| HADS-D≤7 | 2700 | 616 | 1.00 | Ref | 893 | 1.00 | Ref | 1655 | 1.00 | Ref |
| HADS-D≥8 | 297 | 141 | 1.79 | (1.43 to 2.24) | 218 | 1.90 | (1.55 to 2.32) | 321 | 1.53 | (1.28 to 1.82) |
| Total | 6841 | |||||||||
| Sleep duration | ||||||||||
| 7–9 hours | 2498 | 575 | 1.00 | Ref | 801 | 1.00 | Ref | 1395 | 1.00 | Ref |
| ≤6/≥10 hours | 447 | 162 | 1.36 | (1.11 to 1.68) | 246 | 1.42 | (1.18 to 1.70) | 353 | 1.17 | (1.00 to 1.38) |
| Total | 6477 | |||||||||
| Physical activity | ||||||||||
| Active | 1696 | 334 | 1.00 | Ref | 522 | 1.00 | Ref | 901 | 1.00 | Ref |
| Inactive | 1214 | 371 | 1.61 | (1.36 to 1.91) | 553 | 1.60 | (1.38 to 1.86) | 920 | 1.38 | (1.22 to 1.57) |
| Total | 6511 | |||||||||
| Life satisfaction | ||||||||||
| Good | 2886 | 626 | 1.00 | Ref | 1013 | 1.00 | Ref | 1827 | 1.00 | Ref |
| Poor | 351 | 188 | 2.29 | (1.86 to 2.81) | 277 | 2.11 | (1.75 to 2.54) | 420 | 1.77 | (1.51 to 2.08) |
| Total | 7588 | |||||||||
| Daily smoker | ||||||||||
| No | 2635 | 645 | 1.00 | Ref | 771 | 1.00 | Ref | 1453 | 1.00 | Ref |
| Yes | 605 | 175 | 1.15 | (0.95 to 1.39) | 515 | 2.73 | (2.35 to 3.17) | 764 | 2.17 | (1.91 to 2.47) |
| Total | 7563 | |||||||||
| Sitting time | ||||||||||
| ≤7 hours | 2009 | 466 | 1.00 | Ref | 619 | 1.00 | Ref | 1112 | 1.00 | Ref |
| ≥8 hours | 708 | 215 | 1.40 | (1.16 to 1.69) | 319 | 1.59 | (1.34 to 1.89) | 424 | 1.24 | (1.07 to 1.44) |
| Total | 5871 | |||||||||
| Anxiety | ||||||||||
| HADS-A≤7 | 2384 | 558 | 1.00 | Ref | 776 | 1.00 | Ref | 1341 | 1.00 | Ref |
| HADS-A≥8 | 278 | 99 | 1.43 | (1.11 to 1.86) | 148 | 1.65 | (1.31 to 2.08) | 245 | 1.43 | (1.17 to 1.73) |
| Total | 5829 | |||||||||
| Alcohol | ||||||||||
| CAGE≤1 | 2248 | 530 | 1.00 | Ref | 740 | 1.00 | Ref | 1211 | 1.00 | Ref |
| CAGE≥2 | 106 | 30 | 1.04 | (0.68 to 1.59) | 75 | 1.76 | (1.27 to 2.44) | 73 | 1.30 | (0.94 to 1.79) |
| Total | 5013 | |||||||||
| Social participation | ||||||||||
| Participates | 1600 | 374 | 1.00 | Ref | 413 | 1.00 | Ref | 687 | 1.00 | Ref |
| Seldom, never | 1368 | 362 | 1.01 | (0.85 to 1.20) | 642 | 1.50 | (1.29 to 1.76) | 1063 | 1.63 | (1.43 to 1.85) |
| Total | 6509 | |||||||||
n varies from 5013 to 7675 in the various analyses due to different amounts of missing on the independent variables.
*Adjusted for gender, education, age, marital status and chronic illness.
CAGE, Cut down, Annoyed, Guilty, Eye opener (questionnaire for problematic alcohol behaviour) HADS-A, Hospital Anxiety and Depression Scale-Anxiety; HADS-D, Hospital Anxiety and Depression Scale-Depression; HUNT, Nord-Trøndelag Health Study, IADL, instrumental activities of daily living; ref, reference category.
Sensitivity analysis
The sensitivity analysis including a healthy cohort at baseline (selecting those with good self-rated health and good life satisfaction at baseline) showed that the ORs for mortality during follow-up and non-response in HUNT3 was lower than in the original analyses (online supplementary material 3). All factors except physical inactivity showed stronger associations with ADL function in HUNT3. Physical inactivity had considerably lower OR for ADL in the sensitivity analysis (OR=0.97 (0.45 to 2.06)), compared with the original analysis (OR=1.42 (0.91 to 2.23)). All factors showed weaker associations with IADL disability in the sensitivity analysis.
bmjopen-2017-018942supp003.pdf (95.8KB, pdf)
Discussion
In this study we found that poor self-rated health, poor life satisfaction and depression were the strongest risk factors for needing assistance in one or more ADL/IADL. Additionally, we showed that the emerging risk factors short or prolonged sleeping time and excessive sitting time also increased the risk for ADL and IADL disability. Problematic alcohol behaviour and low social participation were not associated with ADL and IADL disability. The studied factors were, in general, greater risk factors for mortality during follow-up than for ADL/IADL disability. Daily smokers had greater risk for mortality during follow-up or not participating in HUNT3 compared with ADL/IADL disability, while low social participation was an additional risk factor for non-participation in HUNT3.
The main limitations of this study are the lack of ADL/IADL information at baseline, healthy survivor and participant bias and generalisability. We performed a sensitivity analysis to determine the robustness of the results given the lack of ADL/IADL status at baseline by including only those who answered having good self-rated health and good life satisfaction at baseline. The lower ORs for mortality during follow-up and non-response in HUNT3 in the sensitivity analysis could indicate a reduction in non-response bias. There were stronger associations between all factors and ADL function in HUNT3, except for physical inactivity, suggesting a general underestimation of the associations in the original analyses. The precision of the effect estimates was poor, but nevertheless the results from the sensitivity analysis indicated that the strength of the association between physical inactivity and ADL disability reported in the results might be exaggerated. Associations between all factors and IADL disability were weaker in the sensitivity analysis, suggesting that the associations could be weaker than indicated in the main analysis. However, physical inactivity, sleeping and sitting time remained the most important lifestyle risk factors. Lastly, assessing sleep through the hours lying down could be misleading, and the lack of a standardised assessment of sleep disorders and quality of life is a limitation. Anyhow, the results that short or prolonged sleeping time was an important risk factor for ADL and IADL disability could be instrumental for future studies on sleep disorders and ADL/IADL disability.
The healthy participant and survivor bias was evaluated through the use of multinomial logistic regression models to evaluate the competing outcomes mortality during follow-up and non-participation in HUNT3. Non-participants in the HUNT3 Study have been found to have lower socioeconomic status, higher mortality, and higher prevalence of smoking and problematic alcohol behaviours.51 We found that the studied risk factors were, in general, stronger risk factors for mortality during follow-up compared with ADL and IADL disability, and that smoking and low social participation were the strongest risk factors for non-participation in HUNT3. The results may therefore represent the healthier part of the population. There were few elderly reporting needing assistance in ADLs compared with IADLs. Abilities to perform the basic ADLs such as walking and eating are fundamental for independent living, and may also be determinants for participating in the HUNT Study. The results from this study could be generalised to populations comparable with the Norwegian setting with low mortality and a high number of elderly. Further, it is limited to community-dwelling elderly since institutionalised elderly are not included in the HUNT Study.
Our results confirmed previous findings that poor self-rated health,23 26 depression,23 25 52 53 physical inactivity21–24 and smoking23 27 28 were risk factors for functional decline and ADL/IADL disabilities. Few studies have investigated the association between anxiety, life satisfaction, sitting time and sleeping time and ADL/IADL disability—we found an association between all factors and ADL and IADL disability. In contrast to previous studies where problematic alcohol behaviour23 27 29–31 has been found to influence functional disability, we found no such associations. It has further been found a U-shaped relationship between abstainers, moderate drinkers and heavy drinkers, and functional status.27 We used the CAGE questionnaire and therefore only investigated one end of the scale by looking at problematic alcohol behaviour. Focusing on problem drinkers would bias the results towards finding an association with functional disability. However, including abstainers in non-drinkers could have cancelled out the effects and explain why we did not find any association between problematic alcohol behaviour and ADL and IADL disability. Further, a small number of participants reporting problematic alcohol behaviour (4.8%) resulted in large uncertainties associated with the effect estimates.
Social participation has also been found to be associated with functional disability,23 28 32–35 in contrast to our results. The measurement of social participation varies between studies,33 34 which could be an explanation for the contrast between our findings and previous research. Further, it must be noted that heterogeneity in methods and measurements of functional decline hampers the comparability between studies.54 The association between risk factors and IADLs has been found to vary with the age group studied,55 and what constitutes risk factors can be different for the ‘young old’ and ‘old old’.24
The strong associations between self-rated health, life satisfaction and depression and the need for assistance in one or more ADLs point out the importance of subjective perceptions and coping as important factors for future ADL/IADL function. Further, excessive sitting time, short or prolonged sleeping time and physical inactivity seemed to be the most important lifestyle risk factors for ADL/IADL disability. This highlights sleep duration and sitting time as emerging risk factors. However, it must be noted that the causality and interrelationship between the studied variables have not been properly established. Life satisfaction is associated with depression56 and self-rated health, and it seems to be different for men and women.57 There could also be different risk factors for each individual activity of daily living.58 Investigating separate ADL and IADL functions is beyond the scope of this paper, but differentiation between basic and instrumental ADLs in the HUNT material has been found useful since they seem to be associated with different variables.59
The results from this study show that subjective perceptions such as self-rated health, life satisfaction and depression were the most important risk factors for ADL/IADL disability. This highlights possible targets for prevention purposes available for policy makers. Clinicians could also focus on the same factors in their meetings with elderly patients to prevent future ADL/IADL decline. Short or prolonged sleep duration and excessive sitting time showed high associations with ADL/IADL disability in this study, but further research is needed to determine the relationship between these emerging risk factors and elderly’s function in ADLs and IADLs.
Supplementary Material
Acknowledgments
The Nord-Trøndelag Health Study (the HUNT Study) is a collaboration between the HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, NTNU), the Nord-Trøndelag County Council, the Central Norway Health Authority and the Norwegian Institute of Public Health.
Footnotes
Contributors: All authors (SHS, ERS and SK) contributed substantially to the conceptualisation and design of the study. SHS performed the statistical analysis under supervision of ERS and SK, and all authors contributed to the interpretation of the data. SHS wrote the first draft of the article, and ERS and SK revised it critically for important intellectual content. All authors have read and approved the final version of the manuscript to be published.
Funding: This study was funded by the Norwegian Research Council and the Faculty of Medicine and Health Sciences at the Norwegian University of Science and Technology (NTNU) through the Student Research Programme at NTNU, and by the Norwegian Medical Students’ Association (NMSA).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The Regional Committee for Medical Research Ethics in Norway approved the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Bloom DE, Chatterji S, Kowal P, et al. Macroeconomic implications of population ageing and selected policy responses. Lancet 2015;385:649–57. 10.1016/S0140-6736(14)61464-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Syse A, Pham DQ, Keilman N. Befolkningsframskrivninger 2016-2100: Dødelighet og levealder [Population projections 2106-2100: Mortality and life expectancy (Norwegian)]. Økonomiske analyser 2016;3. [Google Scholar]
- 3.Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet 2015;385:549–62. 10.1016/S0140-6736(14)61347-7 [DOI] [PubMed] [Google Scholar]
- 4.Chatterji S, Byles J, Cutler D, et al. Health, functioning, and disability in older adults—present status and future implications. Lancet 2015;385:563–75. 10.1016/S0140-6736(14)61462-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noelker LS, Browdie R. Sidney Katz, MD: a new paradigm for chronic illness and long-term care. Gerontologist 2014;54:13–20. 10.1093/geront/gnt086 [DOI] [PubMed] [Google Scholar]
- 6.Moe JO, Hagen TP. Trends and variation in mild disability and functional limitations among older adults in Norway, 1986–2008. Eur J Ageing 2011;8:49–61. 10.1007/s10433-011-0179-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christensen K, Thinggaard M, Oksuzyan A, et al. Physical and cognitive functioning of people older than 90 years: a comparison of two Danish cohorts born 10 years apart. Lancet 2013;382:1507–13. 10.1016/S0140-6736(13)60777-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engberg H, Christensen K, Andersen-Ranberg K, et al. Improving activities of daily living in danish centenarians--but only in women: a comparative study of two birth cohorts born in 1895 and 1905. J Gerontol A Biol Sci Med Sci 2008;63:1186–92. 10.1093/gerona/63.11.1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Falk H, Johansson L, Östling S, et al. Functional disability and ability 75-year-olds: a comparison of two Swedish cohorts born 30 years apart. Age Ageing 2014;43:636–41. 10.1093/ageing/afu018 [DOI] [PubMed] [Google Scholar]
- 10.Bravell ME, Berg S, Malmberg B. Health, functional capacity, formal care, and survival in the oldest old: a longitudinal study. Arch Gerontol Geriatr 2008;46:1–14. 10.1016/j.archger.2007.02.003 [DOI] [PubMed] [Google Scholar]
- 11.Sulander T, Martelin T, Sainio P, et al. Trends and educational disparities in functional capacity among people aged 65–84 years. Int J Epidemiol 2006;35:1255–61. 10.1093/ije/dyl183 [DOI] [PubMed] [Google Scholar]
- 12.Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA 2002;288:3137–46. 10.1001/jama.288.24.3137 [DOI] [PubMed] [Google Scholar]
- 13.Sjölund BM, Wimo A, Engström M, et al. Incidence of ADL Disability in Older Persons, Physical Activities as a Protective Factor and the Need for Informal and Formal Care--Results from the SNAC-N Project. PLoS One 2015;10:e0138901 10.1371/journal.pone.0138901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sjölund BM, Wimo A, Qiu C, et al. Time trends in prevalence of activities of daily living (ADL) disability and survival: comparing two populations (aged 78+ years) living in a rural area in Sweden. Arch Gerontol Geriatr 2014;58:370–5. 10.1016/j.archger.2013.12.004 [DOI] [PubMed] [Google Scholar]
- 15.Nybo H, Gaist D, Jeune B, et al. Functional Status and Self-Rated Health in 2,262 Nonagenarians: The Danish 1905 Cohort Survey. J Am Geriatr Soc 2001;49:601–9. 10.1046/j.1532-5415.2001.49121.x [DOI] [PubMed] [Google Scholar]
- 16.Millán-Calenti JC, Tubío J, Pita-Fernández S, et al. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr 2010;50:306–10. 10.1016/j.archger.2009.04.017 [DOI] [PubMed] [Google Scholar]
- 17.Gaugler JE, Duval S, Anderson KA, et al. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr 2007;7:13 10.1186/1471-2318-7-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly. A systematic review. Age Ageing 2010;39:31–8. 10.1093/ageing/afp202 [DOI] [PubMed] [Google Scholar]
- 19.Preyde M, Brassard K. Evidence-based risk factors for adverse health outcomes in older patients after discharge home and assessment tools: a systematic review. J Evid Based Soc Work 2011;8:445–68. 10.1080/15433714.2011.542330 [DOI] [PubMed] [Google Scholar]
- 20.Gill TM, Robison JT, Tinetti ME. Predictors of recovery in activities of daily living among disabled older persons living in the community. J Gen Intern Med 1997;12:757–62. 10.1046/j.1525-1497.1997.07161.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tak E, Kuiper R, Chorus A, et al. Prevention of onset and progression of basic ADL disability by physical activity in community dwelling older adults: A meta-analysis. Ageing Res Rev 2013;12:329–38. 10.1016/j.arr.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 22.Vermeulen J, Neyens JCL, van Rossum E, et al. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr 2011;11:33 10.1186/1471-2318-11-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stuck AE, Walthert JM, Nikolaus T, et al. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med 1999;48:445–69. 10.1016/S0277-9536(98)00370-0 [DOI] [PubMed] [Google Scholar]
- 24.van der Vorst A, Zijlstra GAR, Witte ND, et al. Limitations in activities of daily living in community-dwelling people aged 75 and over: a systematic literature review of risk and protective factors. PLoS One 2016;11:e0165127 10.1371/journal.pone.0165127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoogerduijn JG, Schuurmans MJ, Duijnstee MSH, et al. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs 2007;16:46–57. 10.1111/j.1365-2702.2006.01579.x [DOI] [PubMed] [Google Scholar]
- 26.Tas U, Verhagen AP, Bierma-Zeinstra SM, et al. Prognostic factors of disability in older people: a systematic review. Br J Gen Pract 2007;57:319–23. [PMC free article] [PubMed] [Google Scholar]
- 27.Sulander T, Martelin T, Rahkonen O, et al. Associations of functional ability with health-related behavior and body mass index among the elderly. Arch Gerontol Geriatr 2005;40:185–99. 10.1016/j.archger.2004.08.003 [DOI] [PubMed] [Google Scholar]
- 28.d’Orsi E, Xavier AJ, Steptoe A, et al. Socioeconomic and lifestyle factors related to instrumental activity of daily living dynamics: results from the English Longitudinal Study of Ageing. J Am Geriatr Soc 2014;62:1630–9. 10.1111/jgs.12990 [DOI] [PubMed] [Google Scholar]
- 29.León-Muñoz LM, Guallar-Castillón P, García-Esquinas E, et al. Alcohol drinking patterns and risk of functional limitations in two cohorts of older adults. Clin Nutr 2017;36:831–8. 10.1016/j.clnu.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 30.Karlamangla AS, Sarkisian CA, Kado DM, et al. Light to moderate alcohol consumption and disability: variable benefits by health status. Am J Epidemiol 2009;169:96–104. 10.1093/aje/kwn294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin JC, Guerrieri JG, Moore AA. Drinking patterns and the development of functional limitations in older adults: longitudinal analyses of the health and retirement survey. J Aging Health 2011;23:806–21. 10.1177/0898264310397541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haga H, Shibata H, Ueno M, et al. Factors contributing to longitudinal changes in activities of daily living (ADL): The Koganei study. J Cross Cult Gerontol 1991;6:91–9. 10.1007/BF00117113 [DOI] [PubMed] [Google Scholar]
- 33.Avlund K, Lund R, Holstein BE, et al. The impact of structural and functional characteristics of social relations as determinants of functional decline. J Gerontol B Psychol Sci Soc Sci 2004;59:S44–S51. 10.1093/geronb/59.1.S44 [DOI] [PubMed] [Google Scholar]
- 34.Tomioka K, Kurumatani N, Hosoi H. Association between social participation and 3-year change in instrumental activities of daily living in community-dwelling elderly adults. J Am Geriatr Soc 2017;65:107–13. 10.1111/jgs.14447 [DOI] [PubMed] [Google Scholar]
- 35.Tomioka K, Kurumatani N, Hosoi H. Association between social participation and instrumental activities of daily living among community-dwelling older adults. J Epidemiol 2016;26:553–61. 10.2188/jea.JE20150253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andersson LB, Marcusson J, Wressle E. Health-related quality of life and activities of daily living in 85-year-olds in Sweden. Health Soc Care Community 2014;22:368–74. 10.1111/hsc.12088 [DOI] [PubMed] [Google Scholar]
- 37.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 2009;18:148–58. 10.1111/j.1365-2869.2008.00732.x [DOI] [PubMed] [Google Scholar]
- 38.Cappuccio FP, D’Elia L, Strazzullo P, et al. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 2010;33:585–92. 10.1093/sleep/33.5.585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cappuccio FP, Cooper D, D’Elia L, et al. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 2011;32:1484–92. 10.1093/eurheartj/ehr007 [DOI] [PubMed] [Google Scholar]
- 40.Alvarez GG, Ayas NT. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs 2004;19:56–9. 10.1111/j.0889-7204.2004.02422.x [DOI] [PubMed] [Google Scholar]
- 41.Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One 2013;8:e80000 10.1371/journal.pone.0080000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 2015;162:123–32. 10.7326/M14-1651 [DOI] [PubMed] [Google Scholar]
- 43.Dunstan DW, Howard B, Healy GN, et al. Too much sitting--a health hazard. Diabetes Res Clin Pract 2012;97:368–76. 10.1016/j.diabres.2012.05.020 [DOI] [PubMed] [Google Scholar]
- 44.Crimmins EM. Trends in the health of the elderly. Annu Rev Public Health 2004;25:79–98. 10.1146/annurev.publhealth.25.102802.124401 [DOI] [PubMed] [Google Scholar]
- 45.Statistics Norway. Highest level of education in Oslo. 2017. https://www.ssb.no/en/utdanning/artikler-og-publikasjoner/highest-level-of-education-in-oslo (accessed 23 Oct 2017).
- 46.Holmen J, Midthjell K, Ø K, et al. The Nord-Trøndelag Health Study 1995–97 (HUNT 2). Norsk Epidemiologi 2003;13:19–32. [Google Scholar]
- 47.Statistics Norway. Smoking habits, 2015. 2016. https://www.ssb.no/helse/statistikker/royk/aar/2016-01-14 (accessed 23 Oct 2017).
- 48.Krokstad S, Langhammer A, Hveem K, et al. Cohort Profile: the HUNT Study, Norway. Int J Epidemiol 2013;42:968–77. 10.1093/ije/dys095 [DOI] [PubMed] [Google Scholar]
- 49.Skogen JC, Overland S, Knudsen AK, et al. Concurrent validity of the CAGE questionnaire. The Nord-Trøndelag Health Study. Addict Behav 2011;36:302–7. 10.1016/j.addbeh.2010.11.010 [DOI] [PubMed] [Google Scholar]
- 50.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77. [DOI] [PubMed] [Google Scholar]
- 51.Langhammer A, Krokstad S, Romundstad P, et al. The HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol 2012;12:143 10.1186/1471-2288-12-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kivinen P, Sulkava R, Halonen P, et al. Self-reported and performance-based functional status and associated factors among elderly men: the Finnish cohorts of the Seven Countries Study. J Clin Epidemiol 1998;51:1243–52. [DOI] [PubMed] [Google Scholar]
- 53.Taş Ümit, Verhagen AP, Bierma-Zeinstra SMA, et al. Incidence and risk factors of disability in the elderly: The Rotterdam Study. Prev Med 2007;44:272–8. 10.1016/j.ypmed.2006.11.007 [DOI] [PubMed] [Google Scholar]
- 54.Buurman BM, van Munster BC, Korevaar JC, et al. Variability in measuring (instrumental) activities of daily living functioning and functional decline in hospitalized older medical patients: a systematic review. J Clin Epidemiol 2011;64:619–27. 10.1016/j.jclinepi.2010.07.005 [DOI] [PubMed] [Google Scholar]
- 55.Tomioka K, Kurumatani N, Hosoi H. Age and gender differences in the association between social participation and instrumental activities of daily living among community-dwelling elderly. BMC Geriatr 2017;17:99 10.1186/s12877-017-0491-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sivertsen H, Bjørkløf GH, Engedal K, et al. Depression and quality of life in older persons: a review. Dement Geriatr Cogn Disord 2015;40:311–39. 10.1159/000437299 [DOI] [PubMed] [Google Scholar]
- 57.Berg AI, Hassing LB, McClearn GE, et al. What matters for life satisfaction in the oldest-old? Aging Ment Health 2006;10:257–64. 10.1080/13607860500409435 [DOI] [PubMed] [Google Scholar]
- 58.Furner SE, Rudberg MA, Cassel CK. Medical conditions differentially affect the development of IADL disability: implications for medical care and research. Gerontologist 1995;35:444–50. 10.1093/geront/35.4.444 [DOI] [PubMed] [Google Scholar]
- 59.Grov EK, Fosså SD, Dahl AA. Activity of daily living problems in older cancer survivors: a population-based controlled study. Health Soc Care Community 2010;18:396–406. 10.1111/j.1365-2524.2010.00912.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018942supp001.pdf (112.1KB, pdf)
bmjopen-2017-018942supp002.pdf (84.7KB, pdf)
bmjopen-2017-018942supp003.pdf (95.8KB, pdf)