Abstract
Background:
First-time lateral patellar dislocation is a common orthopaedic injury. The purposes of this study were to (1) evaluate the incidence of first-time lateral patellar dislocation in a geographically-determined population, (2) report trends over time in the incidence of dislocation, and (3) describe the rate of surgical treatment.
Hypothesis:
The rate of patellar dislocation is highest among adolescent patients.
Study Design:
Cohort study.
Level of Evidence:
Level 3.
Methods:
The study population included 609 individuals identified through a multidisciplinary geographic cohort county database who were diagnosed with first-episode lateral patellar dislocation between 1990 and 2010. The complete medical records were reviewed to confirm the diagnosis and to evaluate details of injury and treatment. Age- and sex-specific incidence rates were calculated and adjusted to the 2010 US population. Poisson regression analyses were performed to examine incidence trends by age, sex, and calendar period.
Results:
The overall age- and sex-adjusted annual incidence of patellar dislocation was 23.2 (95% CI, 21.2-24.9) per 100,000 person-years. The annual incidence was similar between male and female patients and highest among adolescents aged 14 to 18 years (147.7/100,000 person-years). The mean age at dislocation was 21.4 ± 9.9 years, and 331 patients (54.4%) were female. During the study period, there was a significant decline in the incidence of patellar dislocation among men aged 19 to 25 years (P = 0.002) and girls aged 14 to 18 years (P = 0.025). Eighty patients received surgical treatment during the study period, including 66 patients (10.8%) for recurrent instability and 14 patients (2.3%) for acute osteochondral injury.
Conclusion:
With an annual incidence of 23.2 per 100,000 person-years, lateral patellar dislocation is a frequently encountered orthopaedic injury. The incidence of dislocation among adolescent patients in this cohort is higher than previously reported. Despite a decrease in the annual incidence of dislocation in adolescent girls, the overall incidence of patellar dislocation remained relatively constant over a 21-year observation period.
Clinical Relevance:
This study demonstrates that the incidence of patellar dislocation in adolescents is greater than previously reported.
Keywords: patellar dislocation, instability, recurrence, incidence
First-time patellar dislocation is a relatively common cause of traumatic knee hemarthrosis observed in orthopaedic clinics.21 Most episodes of instability result from a noncontact, flexion-rotation injury to the knee resulting in a lateral dislocation of the patella across the lateral femoral condyle.11 This injury often results in concomitant disruption of medial soft tissue restraints and articular cartilage injury.24,25
Previous studies have estimated the incidence of patellar dislocation to be between 2 and 74 per 100,000 people.1,6,10,15,18,26 However, many of these studies have either focused on select patient groups or relied only on administrative data without verification of diagnosis.8,14,19,26 For example, 1 investigation reported an incidence of 77 per 100,000 people using a cohort of Finnish male military personnel.19 An additional study reported a lower incidence of 2 per 100,000 people using a national administrative database of patients who presented to the emergency room.26 A recent investigation using similar methodology showed that the incidence of patellar dislocation varies based on sport and activity level.14 While these studies help describe the incidence of patellar instability, they may not accurately reflect the injury burden in the general population.
Therefore, the purpose of this study was to (1) evaluate the incidence of first-time lateral patellar dislocation in a geographically determined population (Olmsted County, Minnesota), (2) report trends in the incidence of dislocation, and (3) describe the rate of surgical treatment. The primary hypothesis tested was that the greatest incidence of patellar instability and subsequent surgical intervention would occur in adolescent patients.
Methods
This study was conducted after approval from the institutional review board at the supporting institutions (15-009310 and 077-OMC-15). The Rochester Epidemiology Project (REP) was used to identify patients with first-episode lateral patellar dislocation. As previously described, the REP is a medical record database providing access to the complete medical records (all medical encounters) for all residents of Olmsted County, Minnesota, and has been shown previously to be generalizable for epidemiologic studies.17,20 The information in the REP is derived from physician-determined diagnostic codes and includes comprehensive diagnostic and procedural information from all medical centers in Olmsted County in 1 database. The database captures any medical diagnosis for each resident of Olmsted County regardless of the facility in which the diagnosis was made.
Subjects who were residents of Olmsted County and sustained a lateral patellar dislocation were identified by searching the International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code consistent with patellar dislocation between January 1, 1990 and December 31, 2010. The ICD-9 code was used to identify a cohort of potential patients (n = 1442), and the medical record of each subject was reviewed manually to confirm the diagnosis, laterality of injury, and evaluate details of treatment. All clinical notes, radiographic images, and operative notes related to the injury were manually reviewed in detail. Knee radiographs at the time of injury were reviewed by a senior orthopaedic resident for evidence of patella alta (Caton Deschamps),22 osteochondral injury,7 and trochlear dysplasia (Dejour classification).4,5 Similarly, if a patient received magnetic resonance imaging (MRI) or a computed tomography scan after injury, the images were read by a musculoskeletal-trained radiologist and verified by a senior orthopaedic resident to evaluate for the presence of osteochondral injury involving the patella or lateral femoral condyle. Osteochondral injury was defined as a displaced articular osteochondral fragment (from either the patella or lateral femoral condyle) associated with a corresponding donor area.
Patients were included if they had a first-episode, complete, lateral patellar dislocation within the study period. A complete dislocation was defined as requiring a manual reduction (by the patient or physician) of a dislocated patella or a convincing history of a complete dislocation followed by spontaneous reduction. Convincing history of dislocation included obvious visual deformity on the lateral aspect of the knee that was sustained for a period of time followed by spontaneous (or manually reduced) disappearance of the deformity associated with a mechanical or audible sensation. Subjects were excluded if they experienced a subluxation of the patella (without frank dislocation), experienced a first patellar dislocation prior to 1990 with recurrence during study period (ie, not a true first-time dislocation during the study period), had associated fractures of the femur or tibia (not including osteochondral injury), or experienced a tibiofemoral dislocation. Patients were also followed to determine the rate of surgical intervention, including osteochondral fragment removal, medial soft tissue advancement, lateral release, medial patellofemoral ligament reconstruction, tibial tubercle osteotomy, or trochleoplasty. The decision for surgical treatment was made by the treating physician. However, patients were treated surgically for recurrent patellar instability or symptomatic loose bodies. After review, 609 patients with new-onset lateral patellar dislocation were included in the study.
Statistical Analysis
Age- and sex-specific rates of patellar dislocation were calculated by using the number of first-time lateral patellar dislocations (incident cases) as the numerator and population estimates based on decennial census counts as the denominator, with linear interpolation between census years. Only patients who were residents of Olmsted County at the time of patellar dislocation and who fulfilled the study criteria were included in the incidence calculations. Overall incidence rates were age- and sex-adjusted to the 2010 white population of the United States. Ninety-five percent CIs for the incidence rates were constructed using the assumption that the number of incident cases per year followed a Poisson distribution. Incidence trends were examined using Poisson regression models, with smoothing splines for age and calendar year. Similarly, for each patellar dislocation incident, the rate of surgical intervention was determined.
Results
The final study cohort consisted of 609 patients with first-episode lateral patellar dislocation, with a mean follow-up of 12.3 ± 6.5 years. The mean patient age was 21.4 ± 9.9 years, and 331 patients (54.4%) were female. One hundred five patients (17.2%) had evidence of trochlear dysplasia (type A, 82; type B, 19; type C, 2; type D, 2), and 92 patients (15.1%) had radiographic evidence of patella alta. Review of radiographs and MRI images identified osteochondral injury in 101 patients (16.7%). One hundred eighty-three patients (30.0%) experienced recurrent lateral patellar dislocation during the study period. Trochlear dysplasia (hazard ratio, 18.5; 95% CI, 9.7-37.2) and patella alta (hazard ratio, 8.8; 95% CI, 4.2-19.2) were associated with recurrent patellar dislocation.
The overall age- and sex-adjusted annual incidence of patellar dislocation was 23.2 (95% CI, 21.2-24.9) per 100,000 person-years (Table 1 and Figure 1). The annual incidence was similar between men (21.7; 95% CI, 18.5-23.5) and women (24.7; 95% CI, 22.3-27.7) per 100,000 person-years. However, among patients 13 years or younger, girls had a significantly higher incidence of patellar dislocation than boys (17.5 vs 9.6, P = 0.01). Age- and sex-specific annual incidence was greatest between 14 and 18 years for both girls (150.3) and boys (145.3).
Table 1.
Incidence of patellar dislocation by age and sex
| Incident Cases, No. |
Incidence Rate (per 100,000 person-years) |
||||||
|---|---|---|---|---|---|---|---|
| Age, y | Female | Male | Total | Female | Male | Total | P Valuea |
| ≤13 | 47 | 27 | 74 | 17.5 | 9.6 | 13.5 | 0.01 |
| 14-18 | 134 | 136 | 270 | 150.3 | 145.3 | 147.7 | 0.9 |
| 19-25 | 64 | 58 | 122 | 54.9 | 52.4 | 53.6 | 0.7 |
| 26-35 | 44 | 33 | 77 | 20.7 | 15.7 | 18.2 | 0.4 |
| 36-45 | 24 | 16 | 40 | 11.7 | 7.9 | 9.8 | 0.3 |
| ≥46 | 18 | 8 | 26 | 4.0 | 2.1 | 3.1 | 0.1 |
| Total | 331 | 278 | 609 | 24.7 | 21.7 | 23.2 | 0.3 |
P value determined using Poisson regression model to evaluate for the association between sex and incidence rate.
Figure 1.
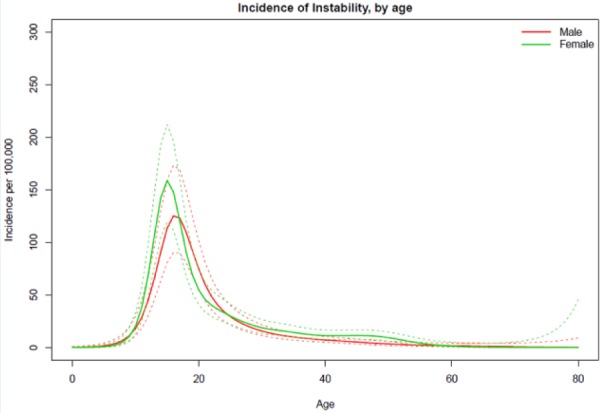
Incidence of patellar dislocation by age.
There was a significant decline in the incidence of patellar dislocation among men aged 19 to 25 years (Table 2 and Figure 2). In the 19- to 25-year age group, incidence declined from 76.6 per 100,000 person-years from 1990 to 1994 to 26.9 per 100,000 person-years from 2005 to 2010. However, the overall incidence in men remained relatively unchanged during the study period. Likewise, there was a significant decrease in the incidence of dislocation among girls aged 14 to 18 years. In this age group, the incidence decreased from 200.7 per 100,000 person-years from 1900 to 1994 to 131.5 per 100,000 person-years from 2005 to 2010. Despite this, the overall incidence of patellar instability in female patients remained unchanged.
Table 2.
Trends in patellar dislocation, 1990 to 2010
| 1990-1994 |
1995-1999 |
2000-2004 |
2005-2010 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Age, y | No. | Incidence Rate | No. | Incidence Rate | No. | Incidence Rate | No. | Incidence Rate | P Value |
| Male | |||||||||
| ≤13 | 6 | 9.6 | 8 | 12.3 | 6 | 8.9 | 7 | 8.1 | 0.316 |
| 14-18 | 27 | 145.8 | 29 | 130.8 | 42 | 173.3 | 38 | 132.6 | 0.749 |
| 19-25 | 19 | 76.6 | 12 | 46.6 | 18 | 67.3 | 9 | 26.9 | 0.002 |
| 26-35 | 6 | 11.6 | 5 | 10.4 | 11 | 23.1 | 11 | 17.6 | 0.139 |
| 36-45 | 3 | 7.2 | 5 | 10.1 | 3 | 5.7 | 5 | 8.7 | 0.775 |
| ≥46 | 0 | 0 | 3 | 3.7 | 2 | 2.1 | 3 | 2.1 | 0.659 |
| Total | 61 | 22.8 | 62 | 21.2 | 82 | 16 | 73 | 17.9 | 0.183 |
| Female | |||||||||
| ≤13 | 10 | 16.8 | 10 | 16.2 | 14 | 21.7 | 13 | 15.8 | 0.991 |
| 14-18 | 36 | 200.7 | 30 | 142.7 | 32 | 140.1 | 36 | 131.5 | 0.025 |
| 19-25 | 12 | 44.4 | 16 | 60 | 21 | 76.9 | 15 | 42.1 | 0.608 |
| 26-35 | 9 | 17 | 7 | 14.4 | 15 | 31.4 | 13 | 20.6 | 0.402 |
| 36-45 | 4 | 9.3 | 6 | 11.9 | 12 | 22.6 | 2 | 3.5 | 0.977 |
| ≥46 | 1 | 1.2 | 4 | 4.2 | 10 | 9 | 3 | 1.9 | 0.922 |
| Total | 72 | 25.5 | 73 | 24.1 | 104 | 31.9 | 82 | 19.2 | 0.176 |
Figure 2.
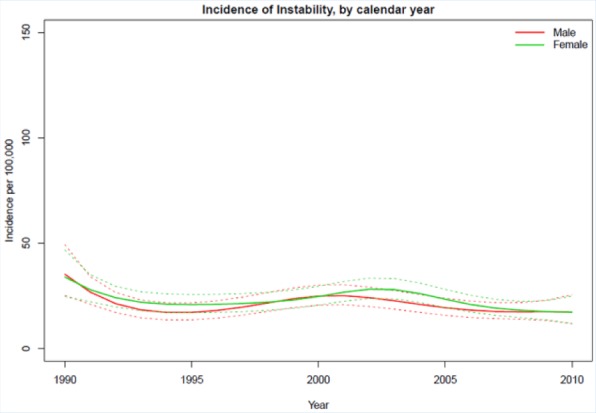
Incidence of patellar dislocation by year.
During follow-up, 66 patients (10.8%) received surgical treatment for recurrent patellar instability, and 14 patients (2.3%) had acute surgical removal of an osteochondral fragment (Table 3). The overall mean time from initial dislocation to surgery was 3.2 years, and the rate of surgery was highest among patients 13 years and younger. The rate of patella-stabilizing surgeries remained consistent during the study period (13.1% from 1990 to 1994 to 9.7% from 2005 to 2010).
Table 3.
Rate of surgical treatment after lateral patellar dislocation
| Age, y | Incident Cases |
Surgeries, n (%) | ||
|---|---|---|---|---|
| Female | Male | Total | ||
| ≤13 | 47 | 27 | 74 | 13 (17.6) |
| 14-18 | 134 | 136 | 270 | 40 (14.8) |
| 19-25 | 64 | 58 | 122 | 18 (14.7) |
| 26-35 | 44 | 33 | 77 | 5 (6.4) |
| 36-45 | 24 | 16 | 40 | 3 (7.5) |
| ≥46 | 18 | 8 | 26 | 1 (3.8) |
| Total | 331 | 278 | 609 | 80 (13.1) |
Discussion
The overall incidence of patellar dislocation in this study was lower than previous estimates from select patient cohorts.8,15,19 For example, 2 retrospective series of military personnel reported the incidence of patellar dislocation to be between 69 and 77 per 100,000 people.8,19 The lower incidence in our study may reflect an overall lower activity level in the general population compared with select military or athletic cohorts, which has been shown to affect the risk for patellar dislocation.14 In contrast, this study demonstrates a significantly greater incidence of patellar dislocation among adolescents than previous estimates.1,15,18,26 For example, 1 prospective study reported a patellar dislocation incidence of 43 per 100,000 people among children 16 years or younger.15 An additional health care database study reported an incidence of patellar dislocation of 31 per 100,000 people among adolescents 10 to 19 years of age.26 Therefore, this study demonstrates that the risk of patellar dislocation among adolescents is greater than previously described. While the reason for adolescent predominance is unknown, rapid skeletal growth, changes in q-angle with growth, or ligamentous laxity may contribute to the high rate of instability.2 The greater incidence may also reflect a higher activity level and risk exposure in the adolescent population.
The incidence of patellar dislocation remained relatively consistent over the study period. However, there was a significant decrease in the incidence of dislocation among female patients 14 to 18 years and male patients 19 to 25 years of age during the study period. The reduction in dislocations among adolescent girls was unexpected since several studies have reported the high incidence of patellar instability in this group.6,8,15 The reasons for the decrease in patellar dislocations in these age groups is unclear. Additionally, the rate of patella-stabilizing procedures was highest in patients 25 years or younger. Surgical stabilization has been recommended for recurrent patellar instability.3,16,21,23 A retrospective series of 210 patients showed a high rate of recurrent dislocation and subsequent patella-stabilizing surgery in patients 18 years or younger.13 Additional studies have shown that recurrent patellar dislocation occurs more frequently in young patients9,12 and may in part explain the higher rate of patella-stabilizing surgery among young patients in this cohort, although longer follow-up may be needed to confirm this observation. In addition, this geographic cohort demonstrates that the majority of patients with lateral patellar dislocation have only a single episode, and few will require surgical treatment. The lower rate of surgery in this cohort compared with previous investigations9,12 may also reflect a relatively lower incidence of structural abnormalities (eg, trochlear dysplasia, patella alta) in the general population compared with cohorts of patients with recurrent instability.
Despite the population-based design, this study has a number of potential limitations. The incidence estimates reflect only clinically diagnosed patellar dislocations and do not include individuals who did not seek medical care or who were misdiagnosed. Additionally, any patient who moved permanently outside Olmsted County was lost to follow-up. Patient activity level could not consistently be recorded, which may have influenced the risk of patellar dislocation and subsequent surgery. Additionally, the trends in specific surgical procedures (lateral release) could not be evaluated over time due to a relatively low number of surgical cases combined with recognizing that many patients received more than 1 type of treatment in the same surgical procedure (combined medical reconstruction and lateral release). Likewise, radiographs were not available for every patient, which limited analysis of radiographic factors for patellar recurrence.
Conclusion
With an annual incidence of 23.2 per 100,000 person-years, lateral patellar dislocation is a frequently encountered orthopaedic injury. The incidence of dislocation among adolescent patients in this cohort is much higher than previously reported. Despite a decrease in the annual incidence of dislocation in adolescent girls, the overall incidence of patellar dislocation remained relatively constant over a 21-year observation period.
Acknowledgments
The authors would like to thank Tyson Christensen for his contribution to this article.
Footnotes
The following author(s) declared potential conflicts of interest: Michael J. Stuart, MD, is a paid consultant for and receives royalties from Arthrex and receives research support from Stryker. Aaron J. Krych, MD, is a paid consultant for Arthrex and receives research support from Arthritis Foundation and Histogenics.
This study was made possible by the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under award number R01AG034676. The findings and conclusions of this report are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
References
- 1. Atkin D, Fithian D, Marangi K, Stone M, Dobson B, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000:28:472-479. [DOI] [PubMed] [Google Scholar]
- 2. Beasley L, Vidal A. Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr. 2004;16:29-36. [DOI] [PubMed] [Google Scholar]
- 3. Boden B, Pearsall A, Garrett W, Feagin J. Patellofemoral instability: evaluations and management. J Am Acad Orthop Surg. 1997;5:47-57. [DOI] [PubMed] [Google Scholar]
- 4. Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:45-54. [PubMed] [Google Scholar]
- 5. Dejour H, Walch G, Nove-Josserand L, Guler C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26. [DOI] [PubMed] [Google Scholar]
- 6. Fithian D, Paxton E, Stone M, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114-1121. [DOI] [PubMed] [Google Scholar]
- 7. Hass J, Collins M, Stuart M. The “sliver sign”: a specific radiographic sign of acute lateral patellar dislocation. Skeletal Radiol. 2012:41:595-601. [DOI] [PubMed] [Google Scholar]
- 8. Hsaio M, Owens B, Burks R, Sturdivant R, Cameron K. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38:1997-2004. [DOI] [PubMed] [Google Scholar]
- 9. Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation [published online October 21, 2015]. J Pediatr Orthop. doi: 10.1097/BPO.0000000000000674. [DOI] [PubMed] [Google Scholar]
- 10. Khormaee S, Kramer D, Yen Y, Heyworth B. Evaluation and management of patellar instability in pediatric and adolescent athletes. Sports Health. 2015;7:115-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kramer D, Pace J. Acute traumatic and sports-related osteochondral injury of the pediatric knee. Orthop Clin N Am. 2012;43:227-236. [DOI] [PubMed] [Google Scholar]
- 12. Lewallen L, McIntosh A, Dahm D. First-time patellofemoral dislocation: risk factors for recurrent instability. J Knee Surg. 2015;28:303-309. [DOI] [PubMed] [Google Scholar]
- 13. Lewallen L, Mcintosh A, Dahm D. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41:575-581. [DOI] [PubMed] [Google Scholar]
- 14. Mitchell J, Magnussen R, Collins C, et al. Epidemiology of patellofemoral instability injuries among high school athletes in the United States. Am J Sports Med. 2015;43:1676-1682. [DOI] [PubMed] [Google Scholar]
- 15. Nietosvarra Y, Aalto K, Kallio P. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513-515. [DOI] [PubMed] [Google Scholar]
- 16. Petri M, Liodakis E, Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled trial. Arch Orthop Trauma Surg. 2013;133:209-213. [DOI] [PubMed] [Google Scholar]
- 17. Sanders TL, Kremers HM, Bryan AJ, Kremers WK, Stuart MJ, Krych AJ. Procedural intervention for arthrofibrosis after ACL reconstruction: trends over two decades. Knee Surg Sports Traumatol Arthrosc. 2017;25:532-537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schneider D, Grawe B, Magnussen R, et al. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med. 2016;44:2993-3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sillanpaa P, Matilla V, Visuri T, Maenpaa H, Pihlajamaki H. Patellofemoral osteoarthritis in patients with operative treatment for patellar dislocation: a magnetic resonance-based analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:230-235. [DOI] [PubMed] [Google Scholar]
- 20. St Sauver J, Grossardt B, Leibson C, Yawn B, Melton L, Rocca W. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stefancin J, Parker R. First-time traumatic patellar dislocation. Clin Orthop Relat Res. 2007,455:93-101. [DOI] [PubMed] [Google Scholar]
- 22. Thevenin-Lemoine C, Ferrand M, Courvoisier A, Damsin J, Ducou le, Pointe H, Vialle R. Is the Caton-Deschamps index a valuable ratio to investigate patellar height in children? J Bone Joint Surg Am. 2011;93:e35. [DOI] [PubMed] [Google Scholar]
- 23. Vavken P, Wimmer M, Camathias C, Quidde J, Valderrabano V, Pagenstert G. Treating patella instability in skeletally immature patients. Arthroscopy. 2013;29:1410-1422. [DOI] [PubMed] [Google Scholar]
- 24. Virolainen H, Visuri T, Kuusela T. Acute dislocation of the patella: MR findings. Radiology. 1993;189:243-246. [DOI] [PubMed] [Google Scholar]
- 25. Vollnberg B, Koehlitz T, Jung T, et al. Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation. Eur Radiol. 2012;22:2347-2356. [DOI] [PubMed] [Google Scholar]
- 26. Waterman B, Belmont P, Owens B. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25:51-57. [DOI] [PubMed] [Google Scholar]


