Abstract
Background
The purpose of this study is to investigate the effects of administration order when a sedative drug (midazolam) and an opioid analgesic drug (fentanyl) is applied for moderate intravenous (IV) sedation in dentistry.
Methods
A retrospective chart review was conducted in one dental clinic during its transition from a midazolam-first to a fentanyl-first protocol for dental procedures requiring moderate IV sedation. Physiological parameters, drug administration times, patient recovery times, drug dosages, and patient recall and satisfaction were investigated for differences.
Results
A total of 76 charts (40 midazolam-first and 36 fentanyl-first administrations), were used in the analysis. Administering midazolam first resulted in an average 4.38 min (52%) decrease in administration times (P < 0.001), and a decrease in procedural recollection immediately following the procedure (P = 0.03), and 24 to 48 hours later (P = 0.009). Administering fentanyl first required an average of 2.43 mg (29%) less midazolam (P < 0.001). No significant differences were found for change in vital signs, minimum oxygen saturation levels, recovery times, and patient satisfaction (P > 0.05). Oxygen saturation levels did not drop below 90% for either group; however, 5 cases in the fentanyl-first group fell to between 90% and 92%, compared with 0 cases in the midazolam-first group.
Conclusions
The administration order of fentanyl and midazolam may have different effects on patients and the sedation procedure. Findings from this study should be used to facilitate discussion among dental practitioners and to guide additional research investigating this topic.
Keywords: Conscious Sedation, Fentanyl, Midazolam, Moderate Sedation
INTRODUCTION
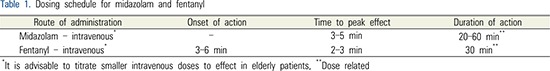
Moderate (conscious) sedation is a common pharmacological approach to managing psychological anxiety and physical pain associated with dental procedures including surgery. While maintaining patient responsiveness to verbal and tactile stimuli [1], safety of conducting moderate sedation in dental clinic is well documented with infrequent complications [1,2]. Preferred drug choices for administering moderate intravenous (IV) sedation are midazolam (benzodiazepine sedative) and fentanyl (opioid analgesic) because their safety and efficacy have been well established [3,4,5,6,7,8]. Other drug options for moderate IV sedation exist, but are beyond the scope of this article.
The Alberta Dental Association and College regulates and provides provincial practice standards for use of moderate sedation in dentistry [9]. Regulations provide strict rules for the environment, support personnel, and monitoring of airway patency, vitals, and oxyhemoglobin saturation (SpO2). However, the administration order of the sedative/opioid two-drug moderate sedation is not prescribed. In most of North America, the administration order―whether the sedative or the opioid should be administered first―is determined at the discretion of the dentist based on clinician preference and/or assessment of the patient's individual need [3,10]. For example, if a patient suffers from moderate to high anxiety and reduced anxiety, or recall of the procedure is the patients' expectation, a sedative-first approach may be preferred. Whereas if pain is the patient's main concern, then opioid-first administration may be the better option [10]. Teaching practices across North America prepare trainees to administer midazolam first, followed by fentanyl. As such, the administration order of midazolam first is likely guided by educational practice.
While logical arguments for prescription based on patient need exists, there is limited research or compelling evidence regarding how to prescribe sedative/analgesic administration order in dental sedation. One randomized control trial found no significant effects of fentanyl and midazolam order administration on patient pain, changes in vital signs, or satisfaction [3]. However, this study held drug dosages constant, whereas in general practice, drugs are typically titrated to effect (i.e., patient comfortable and appropriately responsive), with dosages varying depending on patient characteristics (e.g., anxiety) and procedural stimuli (e.g., complexity of the dental procedure). There is evidence, however, that opioid-first administration yields a substantial reduction in the amount of sedative needed to achieve similar degrees of moderate sedation due to a pharmacodynamic interaction [6,11,12]. A pharmacodynamic interaction occurs when the use of a combination of drugs results in a change in the clinical effect from that which would occur if either drug was used on its own. One study specifically demonstrated a 36% reduction in the amount of midazolam needed to titrate to a suitable end-point for oral surgery when the patient was pretreated with 0.1 mg/70 kg of fentanyl [6]. With the potential in reducing sedative dosage, jurisdictions, such as the United Kingdom, specify opioid-first administration for use in dental procedures [13]. Opioids are known to exert less profound effects on cardiovascular stability compared with sedatives [11]. More research is needed to determine whether the opioid-first technique is appropriate for administration of moderate IV sedation in dentistry.
Aware of the potential pharmacological benefits of opioid-first techniques, a dental clinic in Alberta, Canada, began to adopt a protocol for fentanyl-first administration. Clinical observations when fentanyl was used first included an apparent decrease in discomfort with injection of the local anesthetic (i.e., patients exhibited less response, such as wincing, during needle insertions). This finding was attributed to the fact that by administering the opioid sooner, it reached peak effect before the procedure started. Eventually, this clinic decided to formally switch their protocol from midazolam first to fentanyl first. During the transition period from midazolam-first to fentanyl-first administrations, several dental procedures were performed. The purpose of the present study was to contribute to the evidence base of outcomes for sedative/opioid administration order in moderate IV sedation for dental procedures in a dental clinic environment, where charts and sedation records from this transition period were collected for analysis. Specifically, our study was designed to determine order effects on: patient safety and physiological parameters (i.e., blood oxygen saturation levels [SPO2], end-tidal carbon dioxide [EtCO2], blood pressure, heart and respiration rates); drug administration times and patient recovery times; total drug dosages; and patient recall and satisfaction.
METHODS
Ethics approval for this study was obtained from the University of Alberta Research Ethics Office (Edmonton, Alberta; Pro00061742). A retrospective chart review was conducted in a general dentistry clinic in Alberta that altered administration order of midazolam and fentanyl for procedures requiring moderate IV sedation over a period of nine months. Patients were assigned to each administration order at random with no effort made to equalize or balance the treatments between midazolam first or opioid first. Anonymized chart data and sedation records from 80 patients who underwent moderate IV sedation during this period were collected for data extraction, coding, and analysis. A patient satisfaction questionnaire was also included in the analysis, completed before discharge, and again 24 to 48 hours after procedural sedation.
1. Sedation Procedures
Standards from the Alberta Dental Association and College are followed for all procedures [9]. Three personnel are present at each treatment: the dentist (IV sedation permit holder), a certified dental assistant, and a dedicated sedation assistant for continuous monitoring of patient well-being. All team members are certified in Health-Care Provider Basic Life Support, and able to assist in case of a sedation emergency. The dentist is further trained in advanced cardiac life support and emergency airway management. All patients receive 2 L/min of oxygen via nasal cannula. Patient monitoring (before, during, and after the procedure) involves clinical observations and physiological electronic monitoring to ensure adequate patient responsiveness, airway patency, ventilation, oxygenation, and circulation, with measurements recorded at 5 min intervals. Standard physiological monitoring devices used include: pulse oximeter, EtCO2, non-invasive blood pressure, and standard 3-lead electrocardiogram. The full protocol used at the clinic is presented in Appendix 1.
Based on the safe sedation practice guideline for selecting the order of drug administration [14], the change in order of the sedation from midazolam first to fentanyl first does not alter the aims or endpoints of moderate sedation or its measurement. The principle of titrating drug/drugs to optimal effect is critical to safely achieving a recognized sedation end-point, thereby avoiding inadvertent under- or over-sedation [15]. The use of fixed doses or boluses is unacceptable.
1.1. Fentanyl-first protocol
Fentanyl (5 mcg/ml saline solution) is administered at a rate of 1 ml/min to a suitable endpoint of 25–50 mcg. Total administration dosage depends on the length and complexity of the procedure (e.g., for non-surgical procedures 25 mcg is typically administered, while for impacted wisdom teeth 50 mcg is typically administered), patient characteristics (such as, but not limited to, age, body mass index [BMI], American Society of Anesthesiologists [ASA] status, and underlying health concerns or current medications), and practitioner experience. A 2 min wait time is used to assess patient's respiration, ventilation, and oxygenation (i.e., SpO2 levels) before midazolam administration. Midazolam (1 mg/ml saline solution) is titrated in 1 ml/min increments until the patient is visibly relaxed but responsive (maximum 10 mg).
1.2. Midazolam-first protocol
Midazolam (1 mg/ml saline solution) is titrated in 1 ml/min increments until the patient is visibly relaxed but responsive (maximum midazolam 10 mg). Fentanyl (5 mcg/ml saline solution) is administered at a rate of 1 ml/min to a suitable endpoint of 25–50 mcg (see above). The patient is continuously assessed, and SpO2 levels monitored. Once a suitable endpoint is achieved (patient relaxed but responsive), local anesthesia is administered and the procedure may commence.
The provision of safe sedation in the present study was to sustain throughout the sedation and recovery period the patient's ability to maintain consciousness/responsiveness and control of physiological parameters. This assessment is measured using the Ramsay Sedation Scale [16,17], with moderate sedation level defined as a score: 3–4; and by measurement of surrogates of over-sedation (SpO2 ≤ 90% or the need for an airway opening maneuver).
2. Data Extraction and Coding
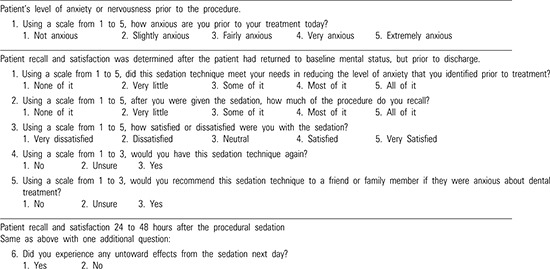
Demographic information extracted included age, sex, smoking status, BMI, and ASA physical status classification [18]. All blood SpO2 and EtCO2 levels were extracted. Pre- and post-procedure systolic and diastolic blood pressure (SBP, DBP), respiration, and heart rate were collected and the differences calculated (i.e., change in vital signs). Administration times were recorded as the time between the first IV drug administration and the administration of local anesthesia (start of the clinical procedure). Recovery times were determined as the time from procedure end to patient discharge. Safe discharge was determined using criteria from a modified discharge scale described by Aldrete [19]. The total dosages of each drug administered were also recorded. Patient anxiety, procedure recollection, and satisfaction were captured through Likert scale questionnaire items (Appendix 2).
3. Data Analysis
Analysis was conducted using STATA Release 14 (StataCorp, College Station, TX, USA) [20]. Data were screened before analysis for statistical outliers. Cases with outliers and potential entry errors were reviewed to determine whether single data points or entire cases should be removed from the analysis. To remove potential bias associated with covariates in the secondary data, propensity scores were determined to control for the effects of demographic differences between the two groups [17]. Due to the small sample size, rather than using a matched pairs approach (which would cause further sample attrition) these propensity scores were used as a single summary covariate in linear and ordinal regression analyses, so that the outcomes described demonstrate only the relative effects of administration order. Statistical significance was set at P < 0.05.
RESULTS
Seventy-six of 80 charts were included in the final analysis, with 40 cases involving midazolam first and 36 involving fentanyl first. The charts removed from analysis were missing key demographic information that would allow for a propensity score to be calculated. Within the included charts there were also 9 single data points reflecting statistical outliers, data entry mistakes, or missing data for certain outcome measures; therefore, these cases were not included in the respective analyses requiring these variables. In addition, 6 charts did not include a satisfaction questionnaire, and 13 additional cases were missing the 24- to 48-hour satisfaction questionnaire responses. These charts were not included in the analyses related to satisfaction.
1. Demographics
Demographic information for the midazolam-first and fentanyl-first groups are summarized in Tables 1 and 2. Before propensity score analysis, the groups significantly differed in age (t[74] = 2.38; P = 0.02); smoking status (χ2[1] = 4.99; P = 0.03 [n = 76]); and ASA status (χ2[1] = 6.46; P = 0.01 [n = 76]). After determining and controlling for propensity scores, the two groups were statistically equivalent for potential covariates.
Table 1. Demographic information (continuous variables).
| Variable | Without covariate adjustment | Adjusted according to propensity score | ||||
|---|---|---|---|---|---|---|
| Midazolam first | Fentanyl first | T-test | Midazolam first | Fentanyl first | Multiple linear regression | |
| Age (yr) | 39.33 ± 17.54 | 30.22 ± 15.66 | t(74) = 2.38; P = 0.02* | 35.09 ± 14.15 | 34.92 ± 14.22 | β = −0.16; P = 0.96 |
| Weight (kg) | 74.51 ± 16.61 | 72.83 ± 16.61 | t(74) = 0.41; P = 0.68 | 73.73 ± 18.84 | 73.70 ± 18.93 | β = −0.03; P = 1.00 |
| Body mass index | 25.70 ± 5.17 | 24.34 ± 4.23 | t(74) = 1.24; P = 0.22 | 25.07 ± 4.76 | 25.04 ± 4.78 | β = −0.02; P = 0.98 |
Data presented as mean ± SD unless otherwise indicated.
*Statistically significant at P < .05
Table 2. Demographic information (categorical variables).
| Variable | Midazolam first | Fentanyl first | χ2 test | Logistic regression† controlling for propensity scores |
|---|---|---|---|---|
| Sex | 15 M, 25 F | 14 M, 22 F | χ2 (1, n =76) = .02; P = 0.9 | β = −0.00; P = 1.00 |
| Smoking status | 27 Non-smokers | 32 Non-smokers | χ2 (1, n = 76) = 4.99; P = 0.03* | β = −0.10; P = 0.91 |
| 13 smokers | 3 smokers | |||
| ASA status | 24 Class I | 31 Class I | χ2 (1, n = 76) = 6.46; P = 0.01* | β = 0.08; P = 0.93 |
| 16 Class II | 5 Class II |
*Statistically significant at P < 0.05.
†First listed variable coded 0, second coded 1. ASA, American Society of Anesthesiologists.
2. Patient Safety and Physiological Parameters
Changes in vital signs, and average SpO2 and EtCO2 levels according to administration group, are shown in Table 3. After controlling for covariates, none of these physiological parameters significantly differed between the midazolam-first and fentanyl-first groups (P > 0.05). For patient safety, verbal contact with the patients was maintained throughout the sedation period (Ramsay score −3), oxygenation desaturation (below 90%) was not observed, and no airway intervention was monitored. Specific to the minimum SpO2 levels experienced by the patients, there were no statistically significant differences; however, there was a potential clinically significant difference, namely, the fentanyl-first group had five (14%) cases in which SpO2 levels dropped below 92%, compared with zero in the midazolam-first group. SpO2 levels never dropped below 90% in either group.
Table 3. Patient safety and physiological parameters.
| Physiological parameter | Midazolam first | Fentanyl first | Multiple linear regression adjusted for propensity scores* |
|---|---|---|---|
| Average SpO2 (%) | 98.15 ± 1.78 | 98.12 ± 1.58 | β = −0.70; P = 0.07 |
| Minimum SpO2 (%) | 96.30 ± 2.20 | 95.11 ± 2.70 | β = −1.12; P = 0.08 |
| Average EtCO2 (mmHg) | 32.71 ± 4.67 | 34.95 ± 4.79 | β = 1.56; P = 0.19 |
| Change in SBP (mmHg) | −7.80 ± 11.98 | −4.71 ± 11.45 | β = 1.17; P = 0.70 |
| Change in DBP (mmHg) | −8.68 ± 8.21 | −8.17 ± 17.46 | β = −0.68; P = 0.84 |
| Change in heart rate (beats/min) | −0.93 ± 9.86 | −1.08 ± 12.56 | β = −0.09; P = 0.97 |
| Change in respiration (breaths/min) | −0.50 ± 3.27 | −2.16 ± 4.02 | β = −1.63; P = 0.09 |
Data presented as mean ± SD unless otherwise indicated. *Statistically significant at P < 0.05. DBP, diastolic blood pressure; EtCO2, end-tidal carbon dioxide SBP, systolic blood pressure; SpO2, oxygen saturation
3. Administration and Recovery Times
There was no significant difference in average procedure length according to administration order (P > 0.05) (Table 4), meaning that the procedures administered between both order groups were statistically comparable. With the use of the propensity score to control for potential confounders, a significant difference was found between the midazolam-first and fentanyl-first groups for drug administration times (β = 4.38, t[71] = 9.63; P < 0.001). On average, when midazolam was administered first, procedures started 4.38 min earlier. The percent change indicated a 51% decrease in average administration times. No significant difference was detected for recovery times (P > 0.05).
Table 4. Administration and recovery times.
| Midazolam first | Fentanyl first | Multiple linear regression adjusted for propensity scores | |
|---|---|---|---|
| Administration (min) | 5.05 ± 1.50 | 9.37 ± 2.00 | β = 4.38; P < 0.001* |
| Procedure (min) | 40.33 ± 29.28 | 31.94 ± 18.86 | β = −5.31; P = 0.40 |
| Recovery (min) | 10.54 ± 3.37 | 10.75 ± 3.42 | β = 0.11; P = 0.90 |
Data presented as mean ±SD unless otherwise indicated. *Statistically significant at P < 0.05.
4. Drug Dosages
Controlling for covariates, there was a significant difference in the amount of midazolam administered (Table 5). When fentanyl was administered first, the total midazolam dosage was, on average, 2.43 mg less than when midazolam was administered first (β = −2.43, t[70] = −5.12; P < 0.001). The percent change indicated a 29% decrease in average midazolam dosages. There was no significant difference in total fentanyl dosage (P > 0.05).
Table 5. Drug dosages.
| Drug | Midazolam first | Fentanyl first | Multiple linear regression adjusting for propensity scores |
|---|---|---|---|
| Total midazolam dosage (mg) | 8.24 ± 1.71 | 6.07 ± 1.99 | β = −2.43; P < 0.001* |
| Total fentanyl dosage (mcg) | 32 ± 10.97 | 36.81 ± 9.12 | β = 1.88; P = 0.44 |
Data presented as mean ±SD unless otherwise indicated. *Statistically significant at P < 0.05
5. Patient Satisfaction
Ordinal logistic regression revealed significant differences in response to the recollection item on the satisfaction questionnaires. On average, the odds of greater procedural recollection before discharge was 3.13 times higher with the administration of fentanyl first (OR = 3.13; z[68] = 2.24; P = 0.03). This tendency continued for the 24- to 48-hour questionnaire, with 4.18 times odds of increased recollection (OR = 4.18; z[55] = 2.61; P = 0.009). There were no significant differences in other satisfaction items (P > 0.05).
DISCUSSION
The purpose of this study was to elaborate on the effects of sedative/analgesic administration order when applied in a private practice dental office setting. This study revealed a 29% reduction in midazolam dosage when low-dose fentanyl opioid was administered first, further demonstrating a significant pharmacodynamic interaction that should be taken into consideration when prescribing drug order for moderate IV sedation in dentistry [6,13]. Opioids are often described as having less profound effects on cardiovascular stability than sedative/hypnotic agents [11]. Therefore, use of a fentanyl-first protocol may be indicated to reduce overall midazolam dosage requirements, while still maintaining adequate patient sedation and operator satisfaction, and without increasing the amount of fentanyl required. Alternatively, this study showed that midazolam-first administrations appeared to result in fewer cases of SpO2 below 92%, and took less time to administer. Admittedly, at least 2 of the 4 min in increased procedure length can be accounted for by the difference in the administration protocol; however, if similar protocols were to be used clinically for fentanyl-first procedures, then this is still an important difference to consider. These latter findings suggest there may be circumstances when midazolamfirst administrations may be preferred, but require further substantiation from additional research.
Findings of the present study also included a significant increase in patient recollection when fentanyl was administered first. Because the fentanyl-first procedures required less midazolam, it follows logically that recollection may increase. Some practitioners may worry that increased recollection would result in greater patient dissatisfaction of the sedation procedure; however, recollection differences did not appear to have any significant impact on the measures of satisfaction in this study. It could be argued that increased recollection (without decreased satisfaction) is actually a benefit, because it means the patient maintained more control to achieve the same level of comfort and pain management. Consideration of recollection effects may be indicated when making patient-centered procedural decisions.
The retrospective design of this study leads to many inherent limitations. Although propensity scores were used to improve the level of statistical control over several known covariates, the lack of control in the assignment of patient groups created issues that may have confounded the results. The comparability of procedures between the groups was demonstrated, with no significant difference found in procedure time; however, it is difficult to determine whether other confounding variables may have influenced the results. Despite using statistical covariates, holding drug dosages constant was also not possible across patients, reflecting individual variations in patient needs and practitioner experience. The issue of not holding dosage constant at initial outset and overall, while limiting the comparability of the administration order, better reflects the actual practice of sedation within a typical dental clinic. The data collection relied on the record-keeping diligence of secondary sources, and missing/improbable data could not be followed up. Furthermore, the time recorded for each procedure, as analyzed in this study, was only accurate to the minute, as recorded by the assistant. Finally, the use of only a single dental clinic in data gathering also limits generalizability. Despite these limitations, however, the information provided in this preliminary study can be used to stimulate discussion and additional research on a topic that has largely been ignored in the literature. This project's findings can be used to guide development of more rigorous prospective studies. Dental practitioners are also encouraged to think more holistically about their administration(s) of moderate IV sedation, and to consider the effects drug order may have on the patient and procedure, instead of relying on a single mechanical routine.
In conclusion, this study demonstrated the characteristics of midazolam and fentanyl when each was administered first for moderate IV sedation in a dental clinic. When fentanyl was administered before midazolam, there was a significant reduction in sedative/hypnotic dosages. However, when midazolam was administered first, there may have been a reduction in administration time and procedural recollection by the patient. From these findings, practitioners may want to consider midazolam-first sedation when patients are experiencing high anxiety or high gag reflex, while the use of fentanyl-first sedation may be recommended when a strong stimulus or painful procedures are required. Moreover, when a lighter level of sedation is desired to provide comfort, a lower-dose fentanyl administration first may enable a (pharmacodynamic) reduction in the amount of midazolam required compared with a midazolam-only sedation. These findings can be used to guide additional research investigating this topic.
Appendix 1
Intravenous (IV) Sedation Protocols - IV Drug Administration for Moderate (Conscious) Sedation in Dentistry
Midazolam-First Administration – Titration to Effect (Moderate Sedation)
Midazolam and Fentanyl sedation protocol
Start sedation with midazolam
1. Draw 10 mg midazolam up to 10 ml with saline (1 mg/ml solution).
2. Administer 1–2 mg initially IV then 1 mg at 1 min intervals until the patient is suitably relaxed, and at sedation end-point of moderate sedation.
Start analgesia with fentanyl
3. Draw 50 mcg fentanyl up to 10 ml with saline (5 mcg/ml solution).
4. Administer 1 ml/min to a suitable end-point of 25–50 mcg. Level of fentanyl is based on procedure stimulus – practitioner judgement. For more complex procedures or surgery (e.g., surgical extraction - impacted wisdom teeth removal or extractions requiring bone removal and/or tooth sectioning), the full 50 mcg is generally administered, less complex cases (e.g., restorations, root canal therapy, crown and bridge treatment, dental cleanings, patients with a high gag reflex that required sedation and routine periodontal treatment) generally require 25 mcg or less.
5. Continuously assess the patient and monitor SpO2 levels.
6. Once the patient seems more relaxed, and at a suitable sedation end-point, then commence with local anesthetic administration.
Start anesthesia with local anesthetic administration
1. Wait for local anesthetic to take effect and then proceed with dental procedure
TITRATION OF SEDATION DURING PROCEDURE
1. IV sedation is generally adequate for procedures of 30–45 min. duration
2. If the procedure extends beyond this time frame and the sedation becomes inadequate then maintenance or supplemental titration may be required.
Wait 2 min. after administering supplemental midazolam before administering either midazolam or fentanyl.
Wait 2 min. after administering supplemental fentanyl before administering either fentanyl or midazolam.
Titrate in 1.0 ml increments.
IF THE PATIENT COMPLAINS OF1
Pain: assess the local anesthesia and re-administer
Discomfort: increase the fentanyl for analgesia
Awareness: increase the midazolam for sedation
REASONS TO STOP SEDATION OR SUPPORT PATIENT
Patient does not respond to loud voice or shaking
SpO2 < 90%
Patient needs airway support
Patient becomes unstable
If the patient becomes unresponsive and has entered a deeper level of sedation or general anesthesia then assess, support and observe the patient. Consideration must be given to administer antagonist or reversal agents: naloxone to reverse fentanyl, or flumazenil to reverse midazolam.
Fentanyl-First Administration – Titration to Effect (Moderate Sedation)
Fentanyl and Midazolam sedation protocol
Start analgesia with fentanyl
1. Draw 50 mcg fentanyl up to 10 ml with saline, (5 mcg/ml solution).
2. Administer 1 ml/min to a suitable end-point of 25–50 mcg. Level of fentanyl is based on procedure stimulus – practitioner judgement. For more complex procedures or surgery (e.g., surgical extraction - impacted wisdom teeth removal or extractions requiring bone removal and/or tooth sectioning), the full 50 mcg is generally administered, less complex cases (e.g., restorations, root canal therapy, crown and bridge treatment, dental cleanings, patients with a high gag reflex that required sedation and routine periodontal treatment) generally require 25 mcg or less. In fentanyl first administration, patients often mention they feel something, however there is not a definitive endpoint like is seen with midazolam administration.
3. Wait 2 min. after administering last increment of fentanyl before administering midazolam - continuously assess the patient and monitor SpO2 levels.
Start sedation with midazolam
4. Draw 10 mg midazolam up to 10 ml with saline, (1 mg/ml solution).
5. Administer 1–2 mg initially IV then 1 mg at 1-min. intervals until the patient is suitably relaxed, and at sedation end-point of moderate sedation.
6. Once the patient seems more relaxed, and at a suitable sedation end-point, then commence with local anesthetic administration.
Start anesthesia with local anesthetic administration
1. Wait for local anesthetic to take effect and then proceed with dental procedure.
TITRATION OF SEDATION DURING PROCEDURE
1. IV sedation is generally adequate for procedures of 30–45 min. duration.
2. If the procedure extends beyond this time frame and the sedation becomes inadequate then maintenance or supplemental titration may be required.
Wait 2 min. after administering supplemental midazolam before administering either midazolam or fentanyl.
Wait 2 min. after administering supplemental fentanyl before administering either fentanyl or midazolam.
Titrate in 1.0 ml increments.
IF THE PATIENT COMPLAINS OF1
Pain - assess the local anesthesia and re-administer
Discomfort – increase the fentanyl for analgesia
Awareness – increase the midazolam for sedation
REASONS TO STOP SEDATION OR SUPPORT PATIENT
Patient does not respond to loud voice or shaking
SpO2 < 90%
Patient needs airway support
Patient becomes unstable
If the patient becomes unresponsive and has entered a deeper level of sedation or general anesthesia then assess, support and observe the patient. Consideration must be given to administer antagonist or reversal agents: naloxone to reverse fentanyl, or flumazenil to reverse midazolam.
Appendix 2
Patient Recall and Satisfaction Questionnaire
The sedationist/operator will be blinded to individual answers to this questionnaire.
Footnotes
CONFLICT OF INTEREST AND SOURCES OF FUNDING: The authors state explicitly that there are no conflicts of interest in connection with this article.
References
- 1.American Society of Anesthesiologists. Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/Analgesia 2014. [Available from: http://www.asahq.org/]
- 2.Inverso G, Dodson TB, Gonzalez ML, Chuang SK. Complications of moderate sedation versus deep sedation/general anesthesia for adolescent patients undergoing third molar extraction. J Oral Maxillofac Surg. 2016;74:474–479. doi: 10.1016/j.joms.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Khader R, Oreadi D, Finkelman M, Jarmoc M, Chaudhary S, Schumann R, et al. A prospective randomized controlled trial of two different sedation sequences for third molar removal in adults. J Oral Maxillofac Surg. 2015;73:224–231. doi: 10.1016/j.joms.2014.08.033. [DOI] [PubMed] [Google Scholar]
- 4.Dionne RA, Gift HC. Drugs used for parenteral sedation in dental practice. Anesth Prog. 1988;35:199–205. [PMC free article] [PubMed] [Google Scholar]
- 5.Ong CK, Seymour RA, Tan JM. Sedation with midazolam leads to reduced pain after dental surgery. Anesth Analg. 2004;98:1289–1293. doi: 10.1213/01.ane.0000111107.18755.cc. [DOI] [PubMed] [Google Scholar]
- 6.Moore PA, Finder RL, Jackson DL. Multidrug intravenous sedation: determinants of the sedative dose of midazolam. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:5–10. doi: 10.1016/s1079-2104(97)90285-7. [DOI] [PubMed] [Google Scholar]
- 7.Kelly A, Higgins P, Cunningham A, Hollingsworth J. Fentanyl Midazolam combination for endoscopy sedation is safe and effective. Gastroenterology. 1998;114:A22. [Google Scholar]
- 8.Mamula P, Markowitz JE, Neiswender K, Zimmerman A, Wood S, Garofolo M, et al. Safety of intravenous midazolam and fentanyl for pediatric GI endoscopy: prospective study of 1578 endoscopies. Gastrointest Endosc. 2007;65:203–210. doi: 10.1016/j.gie.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 9.The Alberta Dental Association and College. Standards for the use of sedation in non-hospital dental practice. Alberta: 2011. [Google Scholar]
- 10.Weaver JM. The narcotic or the benzodiazepine-which should be given first for IV conscious sedation? Anesth Prog. 2001;48:123–124. [PMC free article] [PubMed] [Google Scholar]
- 11.Absalon A, Struys M. An overview of TCI and TIVA. 2nd ed. Academia Press; 2007. pp. 27–48. [Google Scholar]
- 12.Stander M, Wallis L. Procedural sedation in the emergency centre. S Afr Med J. 2011;101:195–201. doi: 10.7196/samj.4418. [DOI] [PubMed] [Google Scholar]
- 13.The Dental Faculties of the Royal Colleges of Surgeons and the Royal College of Anaesthetists. Standards for conscious sedation in the provision of dental care. UK: 2015. [Google Scholar]
- 14.Academy of Medical Royal Colleges. Safe Sedation Practice for Healthcare Procedures: Standards and Guidance. 2013. [Google Scholar]
- 15.Edwards JA, Kinsella J, Shaw A, Evans S, Anderson KJ. Sedation for oocyte retrieval using target controlled infusion of propofol and incremental alfentanil delivered by non-anaesthetists. Anaesthesia. 2010;65:453–461. doi: 10.1111/j.1365-2044.2010.06264.x. [DOI] [PubMed] [Google Scholar]
- 16.Ramsay MA, Savege TM, Simpson BRJ, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–659. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Dishoeck AM, van der Hooft T, Simoons ML, van der Ent M, Scholte op Reimer WJ. Reliable assessment of sedation level in routine clinical practice by adding an instruction to the Ramsay Scale. Eur J Cardiovasc Nurs. 2009;8:125–128. doi: 10.1016/j.ejcnurse.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Mittal N, Goyal A, Jain K, Gauba K. Pediatric dental sedation research: Where do we stand today? J Clin Pediatr Dent. 2015;39:284–291. doi: 10.17796/1053-4628-39.3.284. [DOI] [PubMed] [Google Scholar]
- 19.Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995;7:89–91. doi: 10.1016/0952-8180(94)00001-k. [DOI] [PubMed] [Google Scholar]
- 20.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]


