Abstract
KwaZulu-Natal, South Africa, is the epicenter of an epidemic of drug-resistant tuberculosis (DR-TB) and human immunodeficiency virus (HIV) co-infection, characterized by low rates of medication adherence and retention in care. Social workers may have a unique role to play in improving DR-TB-HIV outcomes. We designed, implemented and evaluated a model-based pilot training course on patient-centered care, treatment literacy in DR-TB and HIV coinfection, patient support group facilitation, and self-care. Ten social workers participated in a 1-day training course. Post-training questionnaire scores showed significant overall gains (P = 0.003). A brief training intervention may be a useful and feasible way to engage social workers in patient-centered care for DR-TB and HIV coinfection.
Keywords: drug-resistant TB-HIV, patient-centred care, social worker, medication adherence
Abstract
Le KwaZulu-Natal, en Afrique du Sud, est l'épicentre d'une épidémie de coïnfection par la tuberculose pharmacorésistante (TB-DR) et le virus de l'immunodéficience humaine caractérisée par des taux faibles d'adhérence aux médicaments et de rétention en soins. Les travailleurs sociaux pourraient avoir un rôle unique dans l'amélioration des résultats de la coïnfection TB-DR et VIH. Nous avons conçu, mis en œuvre et évalué une formation pilote basée sur un modèle de soins centré sur le patient, de connaissance du traitement de la coïnfection TB-DR et VIH, de facilitation des groupes de soutien aux patients et de soins auto-administrés. Dix travailleurs sociaux ont participé à une formation d'un jour. Les scores des questionnaires après la formation ont montré des gains d'ensemble significatifs (P = 0,003). Une brève intervention de formation pourrait être une façon utile et faisable d'engager les travailleurs sociaux dans la prise en charge centrée sur le patient coïnfecté par la TB-DR et le VIH.
Abstract
KwaZulu-Natal, en Suráfrica, es el epicentro de una epidemia de coinfección por el virus de la inmunodeficiencia humana (VIH) y la tuberculosis farmacorresistente (TB-DR), que se caracteriza por bajas tasas de cumplimiento terapéutico y una deficiente retención en la atención. Los trabajadores sociales pueden cumplir una función muy útil en el mejoramiento de los desenlaces clínicos de estos casos. En el presente artículo se describe el diseño, la ejecución y la evaluación de un curso experimental de capacitación a partir de un modelo, sobre la atención centrada en el paciente, la divulgación terapéutica relacionada con la coinfección por el VIH y la TB-DR, la facilitación en grupos de apoyo de pacientes y la autoasistencia. Diez trabajadores sociales participaron en un curso de capacitación de un día de duración. La puntuación de los cuestionarios posteriores a la capacitación reveló progresos notables en general (P = 0,003). Una intervención breve de capacitación puede representar un medio útil y viable para fomentar la participación de los trabajadores sociales en la atención centrada en el paciente de los casos de coinfección por el VIH y la TB-DR.
KwaZulu-Natal, South Africa, is the epicenter of an epidemic of drug-resistant tuberculosis (DR-TB) and human immunodeficiency virus (HIV) co-infection in South Africa.1 This epidemic is characterized by nosocomial and community spread, amplification of anti-tuberculosis drug resistance over time, and low rates of medication adherence and retention in care.2
Poor outcomes among patients with DR-TB and HIV coinfection are driven in part by harsh treatment demands and psychosocial issues.3 Patient-centered care that incorporates counseling and support is increasingly being recognized as an approach to improve outcomes.4–6 Social workers, who are often staff at hospitals and clinics that treat DR-TB patients, may be an overlooked resource.
In South Africa, social workers must have a 4-year bachelors' degree in social work (BSW) and be registered with the South African Council for Social Service Professions.7 South African public sector social workers are primarily community-based and employed by the Department of Social Development; however, the Department of Health (DoH) employs social workers in hospitals and clinics, including those offering specialized TB services. Hospital social workers assess patient psychosocial issues, including mental health, substance abuse, food insecurity, housing needs, family issues and poverty. They assist with applications for social grants, such as disability, pensions, and child support. They also counsel and educate patients prior to ‘pass-outs’ (temporary visits home) or discharge, focusing on how patients will manage their health issues once they leave the hospital. If social issues are determined to be a factor in patient care, especially in non-adherence to treatment, patients are often referred to hospital social workers by medical staff.
The objective of this pilot training workshop was to strengthen social worker skills to motivate patients' active engagement in the care of DR-TB and HIV coinfection, improve understanding of DR-TB treatment, and identify barriers and challenges to patients' sustained engagement in treatment. The workshop adapted an information, motivation, behavioral skills model,8 and used a range of methods to promote active participation, including role play, break-out sessions for small group discussions, and brainstorming. Social workers employed by the KwaZulu-Natal DoH in the eThekwini metropolitan municipality and who were working with DR-TB patients were invited to participate.
The 1-day training curriculum was delivered by social work facilitators, one US-based and one South African, with research and practice experience with DR-TB and HIV. Training was delivered in English and isiZulu, allowing social workers to engage in role play and brainstorming in the languages primarily used with their patients. Curriculum topics included patient-centered care, barriers to treatment success and the role of social work (1.5 h); treatment literacy for DR-TB medications (1.5 h); support group skill-building (2 h); and resources and referrals, advocacy, self-care, and infection control (1.5 h).
A standardized pre- and post-training questionnaire was administered to evaluate the social workers' knowledge, attitudes, and intended practices following training. The post-training questionnaire was re-administered at a follow-up meeting 6 months later. The pre- and post-training responses were compared using paired samples t-test (Statistical Package for the Social Sciences, v 24; IBM Corp, Armonk, NY, USA). Qualitative data, derived from facilitator notes, were analyzed using standard qualitative methods.
The ethics committees at the University of KwaZulu-Natal approved the study protocol (UKZN Biomedical Research Ethics Committee, BF005/09). Written informed consent was obtained from all participants.
ASPECT OF INTEREST
Ten of 12 eligible KwaZulu-Natal DoH social workers attended the training. The majority of the trainees were female (8/10), and were employed in a centralized TB hospital (4/10), decentralized TB treatment hospital (4/10), or TB clinic (2/10).
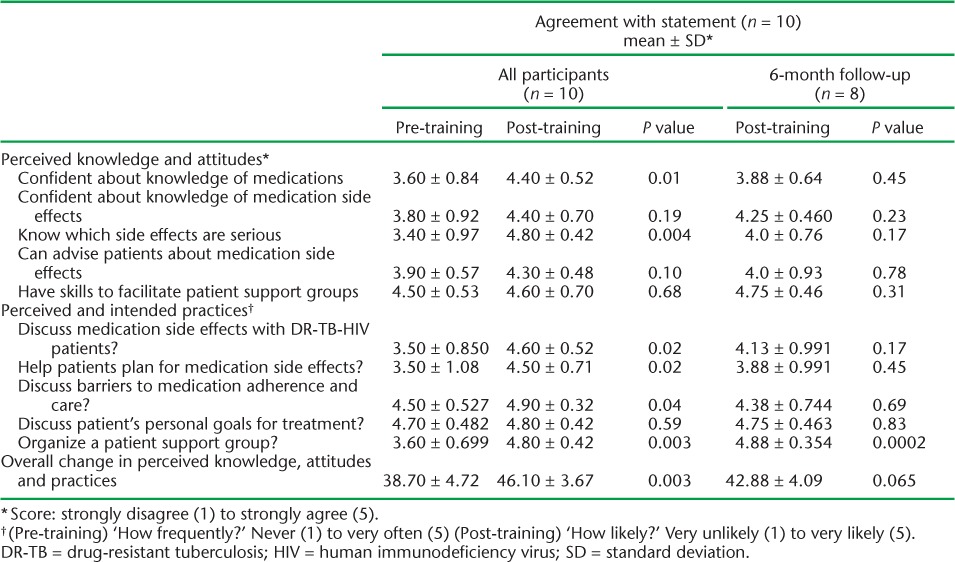
Following the training course, participants showed significant improvement in the post-test survey scores, particularly with regard to treatment literacy and intention to discuss treatment literacy topics with patients and to conduct patient support groups. However, gains in treatment literacy had deteriorated at the 6-month post-training test (Table 1).
TABLE 1.
Pre- and post-training comparison of social workers' knowledge, attitudes and intended practices related to treatment literacy and patient support groups for patients with DR-TB and HIV coinfection
During the group discussions, social workers identified barriers to medication adherence and retention in care in the health care system, individual patient situations, and patient motivation (Table 2). Health care system barriers included structural impediments to adherence (e.g., drug stock-outs, staff and bed shortages); policy impediments (e.g., poorly functioning DOTS system and lack of adequate rewards); and social impediments (e.g., disrespectful treatment of patients and language barriers).
TABLE 2.
Social worker perspectives on barriers to medication adherence and retention in care for DR-TB and HIV co-infected patients in KwaZulu-Natal, South Africa
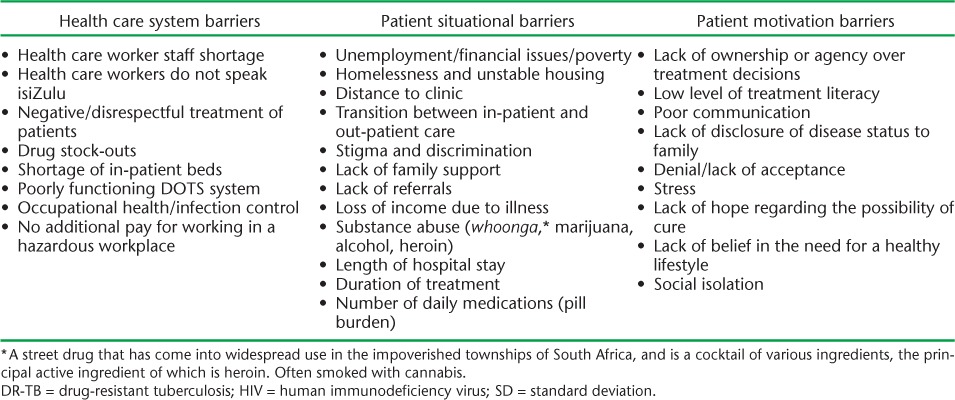
Patient situational barriers identified by social workers included factors intrinsic to treatment for DR-TB and HIV coinfection (e.g., long hospital stay and treatment course, pill burden, loss of income), material hardship (e.g., poverty and homelessness), and psychosocial problems (e.g., lack of family support, substance abuse, depression). Stigma and discrimination were described as being interrelated with other situational barriers.
Social workers identified a web of factors, including denial, social isolation, lack of hope, and poor communication, which contributed to patients' motivation to take an active role in their treatment, although paternalism in the health care system was also identified as hindering patients' active engagement. Low levels of treatment literacy and lack of disclosure to family were also seen as impediments to patient motivation to adhere to difficult treatment, and remain in care over the long course of treatment (Table 2).
DISCUSSION
This brief, focused training course significantly improved the perceived knowledge, attitudes and intended practices of social workers around the treatment of DR-TB and HIV in South Africa, although the weak 6-month retest results suggest a need for follow-up activities to consolidate any training gains.
Despite their vast experience working with DR-TB and HIV co-infected patients, most participants lacked the confidence to comfortably discuss topics related to patients' TB care and treatment. As social workers discuss patients concerns and challenges and, unlike most doctors, most often communicate in the patient's first language (typically isiZulu), this gap in treatment literacy suggests a need for training/materials specifically designed for social workers. Treatment literacy advocacy campaigns among HIV/AIDS (acquired immune-deficiency syndrome) activists serve as an excellent model,9 although the complexity of the DR-TB medications and their variability based on individual resistance patterns is a challenge.
Training social workers to assist in care and treatment for DR-TB and HIV coinfection may have important public health implications. Newly introduced medications to treat DR-TB in South Africa, including bedaquiline and linezolid, show promising results.10 However, this advance underscores the need to find new, effective ways to support patients as well as protect the medicines against community-acquired resistance.
CONCLUSION
While limited by the small sample size and design, our evaluation of this brief, targeted training course for social workers suggests that it may be an efficient, effective, and potentially cost-effective component of a patient-centered approach.
Acknowledgments
This training was supported by Grant number U2G GH001142, funded by the US Centers for Disease Control and Prevention (CDC; Atlanta, GA, USA). Its contents are solely the responsibility of the presenter(s) and does not necessarily represent the official views of the US CDC or the US Department of Health and Human Services. This research (MO, NP, AD, KA) was supported in part by National Institutes of Health-US President's Emergency Plan for AIDS Relief (Grant number R01AI124413).
Footnotes
Conflicts of interest: none declared.
References
- 1. Abdool Karim S S, Churchyard G J, Karim Q A, Lawn S D.. HIV infection and tuberculosis in South Africa: an urgent need to escalate the public health response. Lancet 2009; 374: 921– 933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. O'Donnell M R, Padayatchi N, Kvasnovsky C, Werner L, Master I, Horsburgh C R.. Treatment outcomes for extensively drug-resistant tuberculosis and HIV co-infection. Emerg Infect Dis 2013; 19: 416– 424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Daftary A, Padayatchi N, O'Donnell M R.. Preferential adherence to antiretroviral therapy over tuberculosis treatment: a qualitative study of drug-resistant TB/HIV co-infected patients in South Africa. Glob Public Health 2014; 9: 1107– 1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O'Donnell M R, Daftary A, Frick M, . et al. Re-inventing adherence: toward a patient-centered model of care for drug-resistant tuberculosis and HIV. Int J Tuberc Lung Dis 2016; 20: 430– 434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Acha J, Sweetland A, Guerra D, Chalco K, Castillo H, Palacios E.. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health 2007; 2: 404– 417. [DOI] [PubMed] [Google Scholar]
- 6. Mohr E K, Hughes J, Snyman L, . et al. Patient support interventions to improve adherence to drug-resistant tuberculosis treatment: a counselling tool-kit. S Afr Med J 2015; 105: 631. [DOI] [PubMed] [Google Scholar]
- 7. South African Council of Social Service Professions. . Education, training and development. Pretoria, South Africa: SACSSP, 2018. https://www.sacssp.co.za/Professionals/Education Accessed January 2018. [Google Scholar]
- 8. Fisher J D, Fisher W A, Amico K R, Harman J J.. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. J Health Psychol 2006; 25: 462– 473. [DOI] [PubMed] [Google Scholar]
- 9. Achmat Z, Simcock J.. Combining prevention, treatment and care: lessons from South Africa. AIDS 2007; 21 Suppl 4: S11– S20. [DOI] [PubMed] [Google Scholar]
- 10. Médecins Sans Frontières. . DR-TB drugs under the microscope: sources and prices for drug-resistant tuberculosis medicines. 4th ed MSF Access Campaign Paris, France: MSF, 2016. http://www.hst.org.za/publications/NonHST%20Publications/TB_report_4ed_UnderMicroscope_ENG_2016.pdf#search=Search%2E%2E%2Edrug%20resistant%20TB Accessed January 2018. [Google Scholar]


