Abstract
Background:
This clinical trial investigated the effectiveness of two remineralizing creams on regression of white spot lesions (WSLs) after orthodontic therapy.
Materials and Methods:
The study included patients with WSLs on their upper anterior teeth who recently completed orthodontic treatment at the Department of Orthodontics of Mashhad Dental School and two private offices. The participants were randomly assigned into three groups by treatment: (1) a 12-week regimen of a cream containing casein phosphopeptide-amorphous calcium phosphate and fluoride (MI Paste Plus); (2) a 12-week regimen of a cream containing hydroxyapatite and fluoride (Remin Pro); and (3) usual home care (control). Thirty-nine patients participated and three withdrew. The main outcomes including area, mineral content, and color of WSLs were measured at enrolment and 4, 8, and 12 weeks later, respectively. Blinding was applied for outcome assessment only. The data were analyzed by analysis of variance and repeated measures analysis at the statistical significance of P < 0.05.
Results:
Over a 3-month period, the application of both MI Paste Plus and Remin Pro caused significantly greater reduction in area and significantly higher increase in mineral content of WSLs compared to the control group (P < 0.05). The appearance of WSLs improved significantly in both experimental groups (P < 0.05), but not in the control group. No side effect was observed throughout the experiment.
Conclusion:
The application of either MI Paste Plus or Remin Pro was effective in reducing the area, increasing the mineral content and improving the appearance of demineralized enamel, indicating that these products could be recommended for managing postorthodontic WSLs.
Key Words: Hydroxyapatite, orthodontic treatment, remineralization, white spot
INTRODUCTION
White spot lesions (WSLs) are defined as clinically opaque, white areas caused by the loss of minerals below the outermost enamel layer.[1] The prevalence of WSLs has been reported from 5% to 97% in orthodontically treated participants,[1] and the labial surfaces of maxillary incisors are most commonly affected.[2] The presence of fixed orthodontic appliances increases the accumulation of food and bacterial plaque and promotes successive changes in the mineral and optical properties of subsurface enamel, leading to creation of demineralized areas, which are the precursors to caries formation.[3,4,5]
In recent years, calcium phosphate-based remineralization products have shown promising results for noninvasive management of early caries lesions.[6,7,8,9] It has been demonstrated that the application of products containing casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) could lead to a suppression of demineralization and enhancement of remineralization or most likely, a combination of both could occur.[10,11] Previous studies indicated reduced demineralization around orthodontic brackets in vitro,[12,13] and visual regression of WSLs following topical application of agents containing CPP–ACP complexes in vivo.[2,14] It is believed that the combined application of CPP-ACP with fluoride provides a synergistic effect on enamel remineralization.[15,16,17,18,19] Tooth Mousse Plus (MI Paste Plus; GC Corporation, Tokyo, Japan) is a commercial product that combines CPP-ACP and 900 ppm fluoride (CPP-ACPF), assuming to provide more therapeutic effects than Tooth Mousse (MI Paste), which contains CPP-ACP alone.
Recently, a remineralizing water-based cream containing hydroxyapatite, fluoride and xylitol (Remin Pro, VOCO GmbH, Cuxhaven, Germany) has been introduced. It has been claimed that hydroxyapatite fills eroded enamel, fluoride seals dentinal tubules and xylitol acts as an antibacterial agent. This product has been assumed to be suitable for management of dentinal hypersensitivity, prevention of enamel demineralization and promoting remineralization of enamel subsurface lesions.[20] To the authors' knowledge, no clinical trial investigated the efficacy of Remin Pro in regression of postorthodontic WSLs.
The quantitative caries detection could be accomplished by fluorescent methods.[21] Recently, a new fluorescent camera (VistaCam iX; Dürr Dental, Bietigheim-Bissingen, Germany) was introduced for caries detection.[22] It has been demonstrated that this fluorescent camera provides reliable results similar to that of DIAGNOdent.[22] In addition, this device has an interchangeable head which enables the clinician to take intraoral images.[23]
There are few studies regarding the effect of calcium phosphate- and hydroxyapatite-based agents on remineralization and optical appearance of WSLs following orthodontic therapy. The results of a recent systematic review suggest that there is a tendency toward a benefit for the use of Tooth Mousse (MI Paste) over brushing with a fluoride toothpaste for regression of WSLs in orthodontic patients but the quality of evidence is limited.[24] Therefore, this study was conducted to assess the efficacy of MI Paste Plus and Remin Pro on area, mineral content and color of postorthodontic WSLs.
MATERIALS AND METHODS
The study protocol was reviewed and approved by the ethics committee of Mashhad University of Medical Science (910368). This was a parallel-group, randomized, controlled trial with a 1:1:1 allocation ratio. At the beginning of the study, the investigators asked the faculty colleagues and two orthodontists in private offices to refer patients who recently finished orthodontic therapy and had WSLs on their upper anterior teeth, to the principal investigator. All referred patients were consecutively assessed by the principal investigator to confirm their accordance with the inclusion criteria of the study and those who did not meet the criteria were excluded. Eligible patients were recruited if they met the following criteria:
Completion of fixed appliance therapy within the past 2 weeks
Presence of at least two WSLs on the labial surfaces of six maxillary anterior teeth that were not present before orthodontic therapy (as confirmed in pretreatment photographs)
Age range between 13 and 23 years.
The complete removal of residual composite was assessed clinically. The exclusion criteria were as follows:
Unwillingness to be randomly assigned to 1 of the 3 treatment groups
Presence of abnormal oral, medical, or mental condition (including any milk-related allergies or any medical condition involving kidneys or salivary glands)
Presence of dentin caries or enamel hypoplasia on maxillary anterior teeth
Presence of periodontal pockets around maxillary anterior teeth.
The objectives of the study were explained clearly and informed consent document was obtained from the patients or their parents (if the patient was under 18 years old) before the study commencement.
Interventions
The participants were randomly assigned to one of the three groups and received different treatment regimens. The randomization was performed by a computer-generated table of random numbers using NCSS software (NCSS, Kaysville, UT, USA). The details of the allocated groups were recorded on cards contained in sequentially numbered, opaque, sealed envelopes. These cards were prepared by an independent person who was not involved in the study protocol. Once the participant underwent the baseline assessments by the principal investigator and his/her accordance with the inclusion criteria was confirmed, the allocation assignment was revealed by opening the envelope by this independent person.
An alginate impression was taken from the upper arch of the patients in groups 1 and 2 (experimental groups). Then, vacuum formed retainers were made for the patients in the experimental groups using 1-mm clear sheets.
The participants in group 1 were instructed to apply a remineralizing cream containing CPP-ACPF (MI Paste Plus; GC Corporation, Tokyo, Japan). The cream was inserted within the clear retainer over each of the upper anterior teeth at an approximate height of one-fourth of the central incisor. The patients were asked to use the clear retainer containing MI Paste Plus for 30 min after brushing and not to eat or drink within 1 h later. This procedure was repeated nightly for 12 weeks. A telephone call was made every week to reinforce the patients for using the cream.
The patients in group 2 were instructed to apply a cream containing fluoridated hydroxyapatite (Remin Pro, VOCO GmbH, Cuxhaven, Germany) under the same conditions as described in group 1.
The participants in group 3 underwent no treatment intervention and served as the control group.
All groups received usual home care advice and 2 pockets of fluoridated toothpaste (Crest Cavity Protection, 1100 ppm F as NaF). The participants were instructed to brush twice daily using a soft-texture toothbrush and not to use any supplementary fluoridated products. The supply of remineralizing creams and oral hygiene recommendations were accomplished by an operator who was not involved in the baseline and follow-up assessments.
Outcomes
The patients were evaluated at the start of the treatment (T1) and intervals of 4 (T2), 8 (T3) and 12 (T4) weeks later. The main outcome was any difference in the area, mineral content, and color of WSLs. All measurements were taken in a light-controlled environment by an experienced operator who had been trained to do the measurements before the study commencement and was blinded to the group assignment.
For patient assessment, the anterior maxillary teeth were cleaned with pumice slurry and a rubber prophy cup, and then a lip retractor was inserted to hold the soft tissue away. A series of three intraoral photographs were then taken (one photograph from the labial surfaces of central and lateral incisors and two photographs from the labial surfaces of the right and left canines) using VistaCam iX (Dürr Dental, Bietigheim-Bissingen, Germany). The photographs were taken as the patient's head was positioned horizontally and the lens of the device was 8 cm away from the labial surfaces of the teeth. To calculate the area of WSLs, the intraoral photographs were transported to a microstructure image processing software (MIP4Student software; Nahamin Pardazan Asia Co, Iran).[25,26] Each photograph was calibrated by inserting the mesiodistal width of the imaged tooth into the software. The borders of WSLs were specified manually, and their areas were calculated by the software. Nine sets of photographs were selected, and the areas of WSLs were measured again 1 week later to determine intraexaminer reliability.
To measure the mineral content of WSLs, the labial surfaces of the selected teeth were assessed by VistaCam iX using a special head for taking fluorescent images according to the manufacturer's instructions. The protective cover of the head was in contact with the labial surfaces of the teeth during imaging. This disposable protective cover was recommended by the manufacturer to avoid cross-contamination. The image of each surface was recorded by special software (DBSWIN Imaging Software; Durr Dental). This software creates images of 720 × 576 pixels. The fluorescent images are quantified from green (approximately 510 nm wavelength) to red (approximately 680 nm wavelength) and a numerical value from 0 to 3 is assigned to each image corresponding to the lesion severity. According to the manufacturer, the values in the range of 0–1.0 indicate healthy tooth enamel, whereas those in the range of 1.0–1.5 are representative for early-stage enamel caries. For each WSL, the highest value in the range of 1.0–1.5 was recorded, corresponding to the lowest amount of mineral content.
The Vita Easyshade spectrophotometer (Vita Zahnfabrik, Bad Säckingen, Germany) was employed for color assessment of WSLs. The device was calibrated before each appointment using a white table supplied by the manufacturer. Tooth color was measured by holding the probe tip at a right angle to the surface and the values were reported according to the CIELAB (Commission Internationale de l'Eclairage L* a* and b*) color space system. In this system, the “L” axis represents the degree of lightness, whereas the “a” and “b” values indicate positions on red/green (+a = red, −a = green) and yellow/blue (+b = yellow, −b = blue) axis, respectively. For each tooth, the color assessment was performed at the central area of WSL and also on healthy tooth structure. To minimize measurement errors, the assessments were repeated three times, and the mean values of three consecutive measurements were recorded for each area. The color assessment was repeated in the same conditions at the follow-up appointments. The color difference between WSL and sound tooth surface was calculated using the following formula:
The outcome assessor was kept blinded to the treatment groups. However, blinding of either patient or supplier was not possible because the participants used commercial products.
Statistical analysis
The six upper anterior teeth of each patient were evaluated by one investigator and the area, mineral content and color of WSLs were measured in teeth presenting demineralization. The mean values of variables were then calculated for each participant and considered in the statistical analysis. Therefore, the units for statistical analysis in this study were patients (n = 12).
The normal distribution of the data was confirmed by the Kolmogrov–Smirnov test. Between-group differences in age and number of teeth presenting WSLs were assessed by analysis of variance (ANOVA) and the difference in sex of the participants among the groups was analyzed by the Chi-square test. A repeated measures analysis was run to determine any significant differences in the area, mineral content and color change variables between the different evaluation times in each group. The change between T1 and T4 values for each variable was calculated, and between-group differences in area, mineral content and color of WSLs were analyzed by ANOVA followed by post hoc Tukey test for pairwise comparisons. The statistical calculation was performed using SPSS software (SPSS 16.0, Chicago, IL, USA) and the level of significance was determined at P < 0.05.
RESULTS
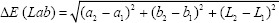
Thirty-nine patients were randomized in a 1:1:1 ratio to either of MI Paste Plus, Remin-Pro or control groups. Three participants withdrew the trial, therefore, a total of 36 participants (20 girls, 16 boys; mean age, 16 ± 3 years) underwent the interventions and had complete records for statistical analysis [Figure 1]. Patient recruitment started in November 2012 and ended in January 2014. At baseline, information regarding age, sex, and number of teeth affected by WSLs was collected. The three groups were well matched in all characteristics at enrollment [Table 1].
Figure 1.

CONSORT flow diagram showing patient flow during the trial.
Table 1.
Comparison of baseline characteristics in the study groups
Using the 9 sets of repeated measurements, the correlation coefficient for detecting the area of WSLs was 0.94, indicating excellent reliability.
Comparison of area, mineral content, and color of white spot lesions between the different evaluation times in each group
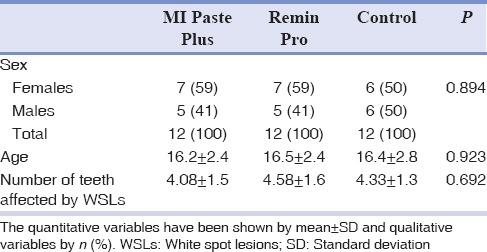
The repeated measures analysis revealed that the area of WSLs decreased significantly between T1 and T2 in all the study groups (P< 0.05) [Figure 2]. However, between T2-T3 and T3-T4 time points, a significant reduction in the area of WSLs occurred in MI Paste Plus and Remin Pro groups (P< 0.05), whereas the control group revealed no significant improvement in this aspect (P > 0.05) [Figure 2].
Figure 2.
A line chart indicating the area of white spot lesions (mm2) at different evaluation times in the study groups. Significant reductions were found between T1–T2 in all groups (P < 0.05), and between T2–T3, and T3–T4 in both MI Paste Plus and Remin Pro groups (P < 0.001).
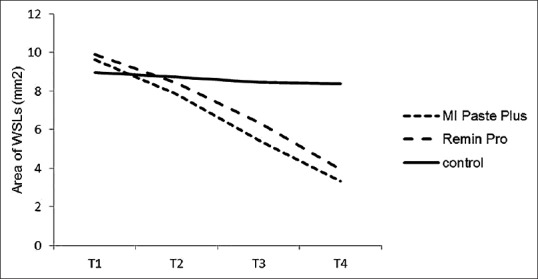
A significant increase in the mineral content of WSLs occurred between T1-T2, T2-T3 and T3-T4 time points in the two experimental groups (P< 0.05) [Figure 3]. The control group experienced a slight but significant increase in mineral content of WSLs between T1-T2 and T3-T4 time points (P = 0.001 and P = 0.014, respectively), but the increase between T2-T3 was not statistically significant (P > 0.05) [Figure 3]. It should be noted that the mineral content of WSLs in MI Paste Plus and Remin Pro groups increased approximately 16% and 22%, respectively, between the baseline and final measurements. This increase was 5% in the control group.
Figure 3.
A line chart indicating the mineral content of white spot lesions at different evaluation times in the study groups. Significant increase in mineral content of the teeth were found between T1–T2, T2–T3 and T3–T4 for the experimental groups (P < 0.05) and between T1–T2 and T3–T4 in the control group (P < 0.05).
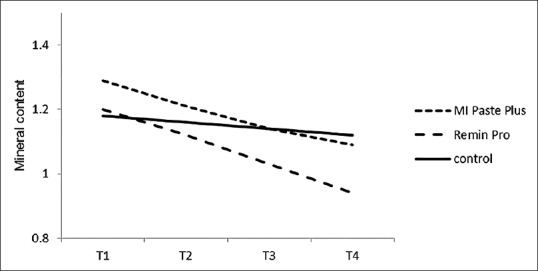
The repeated measures analysis exhibited that the two experimental groups experienced significant reduction in the color difference between sound and demineralized parts of enamel throughout the experiment (P< 0.05), whereas the improvement in the control group was not statistically significant (P > 0.05) [Figure 4].
Figure 4.
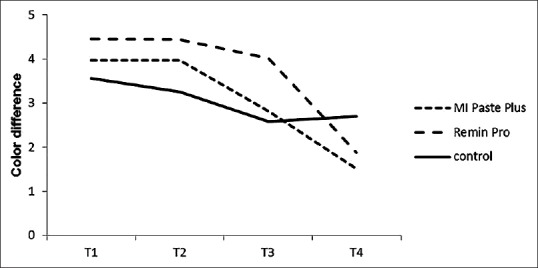
A line chart indicating the color difference (ΔE) between sound tooth surface and white spot lesions at different evaluation times in the study groups. Significant reductions n the color difference between sound and demineralized enamel were found between T1–T2, T2–T3 and T3–T4 in both experimental groups (P < 0.05) but not in the control group (P > 0.05).
Comparison of T1–T4 differences in area, mineral content and color of white spot lesions between the study groups
Tables 2 and 3 present the mean values and standard deviations regarding the area and mineral content of WSLs at different evaluation times, and the changes in these variables between baseline (T1) and end of the experiment (T4) for the three groups. Table 4 indicates descriptive results regarding the color difference between sound tooth surfaces and WSLs at different treatment stages and the change in this variable between T1 and T4 time points for the study groups. ANOVA revealed statistically significant differences for T1-T4 improvement in area (P< 0.001), mineral content (P< 0.001), and color (P = 0.009) of WSLs between the study groups. All groups showed reduction in area of WSLs throughout the experiment, but the degree of reduction was significantly greater in Remin Pro and MI Paste Plus groups, as compared to the control group [P < 0.05; Table 2]. Pairwise comparison by Tukey test also revealed that both experimental groups exhibited significantly greater increase in mineral content of WSLs as compared to the control group [P < 0.05; Table 3]. Comparison of the alteration in values between baseline and end of the experiment revealed that both experimental groups experienced significantly greater reduction in the color difference between sound and demineralized enamel, as compared to the control group [P < 0.05; Table 4].
Table 2.
The mean and standard deviation regarding the area of white spot lesions (mm2) at follow up appointments and the difference between T1 and T4 values in the study groups

Table 3.
The mean and standard deviation regarding the mineral content of white spot lesions at follow up appointments and the difference between T1 and T4 values in the study groups
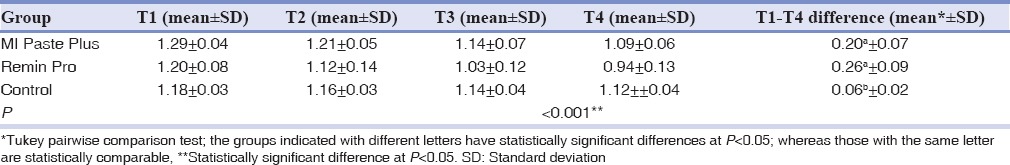
Table 4.
The mean and standard deviation regarding the color difference (ΔE) between sound tooth surface and white spot lesions at follow up appointments and the difference between T1 and T4 values in the study groups

No harm was observed over the period of the experiment.
DISCUSSION
This study investigated the effectiveness of two remineralizing agents, MI Paste Plus and Remin Pro, against usual home care for treatment of postorthodontic WSLs. The study was contemplated during a 12-week period because in most cases, a rapid reduction in the size of WSLs occurs during the first 12 weeks following appliance removal.[27] It has been demonstrated that fluorescent-based systems are suitable for visual detection of caries lesions.[28,29] In this study, VistaCam iX was employed to capture fluorescent images. A previous study indicated that this fluorescent camera provides high reproducibility and good performance for caries detection at various stages of the disease process.[30] In addition, the portability and fair cost of the device makes it easily applied in the clinical situation. In contrast to some previous studies [1,2,11] that scored areas of WSLs in photographs; the present investigation took advantage from MIP4Student software for quantitative assessment of demineralized areas of enamel. Because of the esthetic problem of WSLs, the color change was another variable that was measured in the present investigation. Tooth color can be determined by 2 means: visual and instrumental assessments. It is believed that instrumental methods are more accurate and more reproducible compared with human visual shade assessments.[31] Therefore, in the present study, a spectrophotometer was employed for color assessment. Under clinical conditions, if the color difference exceeds 3.3 units, it would be perceptible by human eyes, indicating color mismatching.[32]
In the present study, a significant reduction in the area of WSLs occurred in the MI Paste Plus (65%) and Remin Pro (60%) groups during the course of the study, whereas in the control group there was no significant improvement in the area of WSLs between T2-T3 and T3-T4 time points (7% reduction over the study period). This outcome indicates that MI Paste Plus and Remin Pro have remineralizing effects on enamel caries and can effectively reduce the extent of WSLs in a 3-month treatment period. It is believed that MI Paste Plus can maintain a state of supersaturation of calcium and phosphate over the enamel surface. In addition, the fluoride content in MI Paste Plus has a synergistic effect with CPP-ACP, increasing its remineralizing potential.[17,18] The Remin Pro product contains fluoride as well as calcium and phosphate in the form of hydroxyapatite, with the capability to fill superficial enamel lesions. The little improvement observed in the extent of WSLs in the control group can be attributed to the natural remineralization phenomenon that results in partial reversal of what is an early caries lesion.[27]
In this study, the mineral content of MI Paste Plus and Remin Pro groups increased approximately 16% and 22%, respectively throughout the experiment. In comparison, the increase in mineral content of the control group was only 5%. When the alteration in mineral content between baseline and end of the experiment was compared between groups, it was revealed that both MI paste Plus and Remin Pro groups had significantly greater increase in mineral content of WSLs than that of the control group, indicating the remineralizing capability of these products. The increase in mineral content of WSLs was slightly greater in Remin Pro than MI paste Plus group, possibly due to the more efficient delivery of calcium and phosphate ions by hydroxyapatite.
The two experimental groups (MI Paste Plus and Remin Pro) showed significant improvement in the color of WSLs during the study, whereas the controls experienced only a small insignificant regression. This finding can be attributed to the effectiveness of MI Paste Plus and Remin Pro in remineralizing WSLs. When mineral is lost from the enamel, it becomes more porous; so the light is scattered and the result is the clinical appearance of white spot lesions.[33] It is expected that remineralizing treatments help to prevent light scattering by filling the porous areas and in this way, improve the appearance of the tooth surface. The lower amount of mineral content in the control group, however, leads to greater light scattering and consequently more color difference between sound tooth surface and WSLs.
Some authors believe that concentrated fluoride agents should not be used for the treatment of demineralized enamel immediately after appliance removal because they cause fluoride precipitation in surface-softened enamel with less effect on subsurface lesions, and thus, the optical appearance of demineralized enamel would not be improved.[1,34,35] The findings of this study, however, indicate that the natural improvement in mineral content and appearance of WSLs is negligible following appliance removal, whereas both remineralizing creams were effective in enhancing mineral properties and reducing the color difference between healthy and demineralized parts of enamel. Therefore, it is suggested that the clinicians recommend the patients with extensive WSLs to use these remineralizing agents after appliance removal to decrease complications and promote the esthetic outcome of orthodontic therapy. Since the participants of this study were recruited from several dental centers and they were randomly assigned to the study groups, the results may have good generalizability to other groups of orthodontic patients.
The outcomes of this study agree with the results of some clinical trials.[2,3,14,36] Robertson et al.[3] found that the use of MI Paste Plus prevented the development of new WSLs during orthodontic treatment and reduced the number of WSLs already present, whereas the placebo paste had no significant effect on prevention and treatment of caries lesions. Another clinical trial showed that a remineralizing paste containing CPP-ACP significantly enhanced regression of WSLs compared with a placebo cream over a 12-week period.[2] In contrast to the results of this study, some randomized clinical trials reported no beneficial effects of using products containing casein phosphopeptide-amorphous calcium phosphate for the treatment of WSLs.[1,11,37] This difference may be related to the use of fluoride-free CPP-ACP or to the shorter intervention periods in those studies [1,12] compared to the 3-month application in the present investigation. Another factor that could affect the results is the volume of the remineralizing agent used and its close contact with the demineralized tooth surface. In contrast to some previous studies that recommended a pea-sized amount or 1 g of CPP-ACP applied by a finger or brush,[1,11] in this study, the patients were instructed to use the remineralizing paste as much as one-fourth of the central incisor height within a clear retainer. This retainer provided close proximity between the cream and the demineralized tooth surface for 30 min, which was longer than that used in other investigations.[1,3,11] Further studies with greater sample size and longer follow-ups are warranted to compare the effectiveness of MI Paste Plus and Remin Pro with topical fluoride application in regression of WSLs.
A limitation of the current study was the lack of blinding for the patients and the supplier because industrial products were used. However, the outcome evaluator was kept blinded, so the risk of biases should be considered low. Another limitation of the study was its small sample size. This was related to the difficulty in finding patients who met the inclusion criteria and agreed to participate in the trial. However, it should be noted that most patients in this investigation had multiple teeth with WSLs; therefore, the number of teeth examined was much higher than 12 (the number of patients).
CONCLUSION
Under the conditions used in this 12-week clinical trial:
The application of MI Paste Plus and Remin Pro caused a significant decrease in the area of WSLs, which was significantly greater than that of the control group
The mineral content of WSLs enhanced in all groups throughout the experiment, but the degree of enhancement was significantly greater in MI Paste Plus and Remin Pro groups than the control group
A significantly greater improvement in the appearance of WSLs occurred following the use of MI Paste Plus and Remin Pro products as compared to the patients receiving usual home care.
The prescription of either MI Paste Plus or Remin Pro can be recommended after orthodontic therapy to increase mineral properties and enhance dental esthetics in participants with extensive WSLs.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
Acknowledgments
The authors would like to thank the vice chancellor for research of Mashhad University of Medical Sciences for the financial support of this project. The results presented in this work have been taken from a postgraduate student thesis (thesis number 529).
REFERENCES
- 1.Huang GJ, Roloff-Chiang B, Mills BE, Shalchi S, Spiekerman C, Korpak AM, et al. Effectiveness of MI paste plus and previDent fluoride varnish for treatment of white spot lesions: A randomized controlled trial. Am J Orthod Dentofacial Orthop. 2013;143:31–41. doi: 10.1016/j.ajodo.2012.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bailey DL, Adams GG, Tsao CE, Hyslop A, Escobar K, Manton DJ, et al. Regression of post-orthodontic lesions by a remineralizing cream. J Dent Res. 2009;88:1148–53. doi: 10.1177/0022034509347168. [DOI] [PubMed] [Google Scholar]
- 3.Robertson MA, Kau CH, English JD, Lee RP, Powers J, Nguyen JT, et al. MI paste plus to prevent demineralization in orthodontic patients: A prospective randomized controlled trial. Am J Orthod Dentofacial Orthop. 2011;140:660–8. doi: 10.1016/j.ajodo.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 4.Höchli D, Hersberger-Zurfluh M, Papageorgiou SN, Eliades T. Interventions for orthodontically induced white spot lesions: A systematic review and meta-analysis. Eur J Orthod. 2017;39:122–33. doi: 10.1093/ejo/cjw065. [DOI] [PubMed] [Google Scholar]
- 5.Ahrari F, Poosti M, Motahari P. Enamel resistance to demineralization following Er: YAG laser etching for bonding orthodontic brackets. Dent Res J (Isfahan) 2012;9:472–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, et al. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2008;87:344–8. doi: 10.1177/154405910808700420. [DOI] [PubMed] [Google Scholar]
- 7.Reynolds EC. Calcium phosphate-based remineralization systems: Scientific evidence? Aust Dent J. 2008;53:268–73. doi: 10.1111/j.1834-7819.2008.00061.x. [DOI] [PubMed] [Google Scholar]
- 8.Heravi F, Ahrari F, Mahdavi M, Basafa S. Comparative evaluation of the effect of Er: YAG laser and low level laser irradiation combined with CPP-ACPF cream on treatment of enamel caries. J Clin Exp Dent. 2014;6:e121–6. doi: 10.4317/jced.51309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azarpazhooh A, Limeback H. Clinical efficacy of casein derivatives: A systematic review of the literature. J Am Dent Assoc. 2008;139:915–24. doi: 10.14219/jada.archive.2008.0278. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds EC. Casein phosphopeptide-amorphous calcium phosphate: The scientific evidence. Adv Dent Res. 2009;21:25–9. doi: 10.1177/0895937409335619. [DOI] [PubMed] [Google Scholar]
- 11.Bröchner A, Christensen C, Kristensen B, Tranæus S, Karlsson L, Sonnesen L, et al. Treatment of post-orthodontic white spot lesions with casein phosphopeptide-stabilised amorphous calcium phosphate. Clin Oral Investig. 2011;15:369–73. doi: 10.1007/s00784-010-0401-2. [DOI] [PubMed] [Google Scholar]
- 12.Sudjalim TR, Woods MG, Manton DJ, Reynolds EC. Prevention of demineralization around orthodontic brackets in vitro. Am J Orthod Dentofacial Orthop. 2007;131:705.e1–9. doi: 10.1016/j.ajodo.2006.09.043. [DOI] [PubMed] [Google Scholar]
- 13.Yap J, Walsh LJ, Naser-Ud Din S, Ngo H, Manton DJ. Evaluation of a novel approach in the prevention of white spot lesions around orthodontic brackets. Aust Dent J. 2014;59:70–80. doi: 10.1111/adj.12142. [DOI] [PubMed] [Google Scholar]
- 14.Andersson A, Sköld-Larsson K, Hallgren A, Petersson LG, Twetman S. Effect of a dental cream containing amorphous cream phosphate complexes on white spot lesion regression assessed by laser fluorescence. Oral Health Prev Dent. 2007;5:229–33. [PubMed] [Google Scholar]
- 15.Elsayad I, Sakr A, Badr Y. Combining casein phosphopeptide-amorphous calcium phosphate with fluoride: Synergistic remineralization potential of artificially demineralized enamel or not? J Biomed Opt. 2009;14:044039. doi: 10.1117/1.3210780. [DOI] [PubMed] [Google Scholar]
- 16.Kumar V, Itthagarun A, King N. The effect of casein phosphopeptide-amorphous calcium phosphate on remineralization of artificial caries-like lesions: An in vitro study. Aust Dent J. 2008;53:34–40. doi: 10.1111/j.1834-7819.2007.00006.x. [DOI] [PubMed] [Google Scholar]
- 17.Cochrane NJ, Saranathan S, Cai F, Cross KJ, Reynolds EC. Enamel subsurface lesion remineralisation with casein phosphopeptide stabilised solutions of calcium, phosphate and fluoride. Caries Res. 2008;42:88–97. doi: 10.1159/000113161. [DOI] [PubMed] [Google Scholar]
- 18.Srinivasan N, Kavitha M, Loganathan S. Comparison of the remineralization potential of CPP-ACP and CPP-ACP with 900ppm fluoride on eroded human enamel: An in situ study. Arch Oral Biol. 2010;55:541–4. doi: 10.1016/j.archoralbio.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Wu G, Liu X, Hou Y. Analysis of the effect of CPP-ACP tooth mousse on enamel remineralization by circularly polarized images. Angle Orthod. 2010;80:933–8. doi: 10.2319/110509-624.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamath U, Sheth H, Mullur D, Soubhagya M. The effect of Remin Pro(R) on bleached enamel hardness: An in-vitro study. Indian J Dent Res. 2013;24:690–3. doi: 10.4103/0970-9290.127612. [DOI] [PubMed] [Google Scholar]
- 21.Thoms M. Detection of intraoral lesions using a fluorescence camera. Proc SPIE. 2006;6137:613705. [Google Scholar]
- 22.De Benedetto MS, Morais CC, Novaes TF, de Almeida Rodrigues J, Braga MM, Mendes FM, et al. Comparing the reliability of a new fluorescence camera with conventional laser fluorescence devices in detecting caries lesions in occlusal and smooth surfaces of primary teeth. Lasers Med Sci. 2011;26:157–62. doi: 10.1007/s10103-010-0757-1. [DOI] [PubMed] [Google Scholar]
- 23. [Last accessed on 2014 Oct 30]. Available from: http://www.duerrdental.com/en/products/imaging/vistacam-intraoral-camera-systems/vistacam-ix/A .
- 24.Raphael S, Blinkhorn A. Is there a place for tooth mousse in the prevention and treatment of early dental caries. A systematic review? BMC Oral Health. 2015;15:113. doi: 10.1186/s12903-015-0095-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahrari F, Basafa M, Fekrazad R, Mokarram M, Akbari M. The efficacy of Er, Cr:YSGG laser in reconditioning of metallic orthodontic brackets. Photomed Laser Surg. 2012;30:41–6. doi: 10.1089/pho.2011.3088. [DOI] [PubMed] [Google Scholar]
- 26.Ahrari F, Fekrazad R, Kalhori KA, Ramtin M. Reconditioning of ceramic orthodontic brackets with an Er, Cr:YSGG laser. Lasers Med Sci. 2013;28:223–8. doi: 10.1007/s10103-012-1093-4. [DOI] [PubMed] [Google Scholar]
- 27.Willmot D. White spot lesions after orthodontic treatment. Semin Orthod. 2008;14:209–19. [Google Scholar]
- 28.Rodrigues JA, Hug I, Neuhaus KW, Lussi A. Light-emitting diode and laser fluorescence-based devices in detecting occlusal caries. J Biomed Opt. 2011;16:107003. doi: 10.1117/1.3631796. [DOI] [PubMed] [Google Scholar]
- 29.Akbari M, Ahrari F, Jafari M. A comparative evaluation of DIAGNOdent and caries detector dye in detection of residual caries in prepared cavities. J Contemp Dent Pract. 2012;13:515–20. doi: 10.5005/jp-journals-10024-1178. [DOI] [PubMed] [Google Scholar]
- 30.Jablonski-Momeni A, Liebegall F, Stoll R, Heinzel-Gutenbrunner M, Pieper K. Performance of a new fluorescence camera for detection of occlusal caries in vitro. Lasers Med Sci. 2013;28:101–9. doi: 10.1007/s10103-012-1080-9. [DOI] [PubMed] [Google Scholar]
- 31.Eslami N, Ahrari F, Rajabi O, Zamani R. The staining effect of different mouthwashes containing nanoparticles on dental enamel. J Clin Exp Dent. 2015;7:e457–61. doi: 10.4317/jced.52199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Powers JM, Sakaguchi RL. Craig's Restorative Dental Materials. 12th ed. St Louis: Mosby; 2006. p. p. 30. [Google Scholar]
- 33.Benson P. Evaluation of white spot lesions on teeth with orthodontic brackets. Semin Orthod. 2008;14:200–8. [Google Scholar]
- 34.García-Godoy F, Hicks MJ. Maintaining the integrity of the enamel surface: The role of dental biofilm, saliva and preventive agents in enamel demineralization and remineralization. J Am Dent Assoc. 2008;139(Suppl 2):25S–34S. doi: 10.14219/jada.archive.2008.0352. [DOI] [PubMed] [Google Scholar]
- 35.Poosti M, Ahrari F, Moosavi H, Najjaran H. The effect of fractional CO2 laser irradiation on remineralization of enamel white spot lesions. Lasers Med Sci. 2014;29:1349–55. doi: 10.1007/s10103-013-1290-9. [DOI] [PubMed] [Google Scholar]
- 36.Ebrahimi M, Mehrabkhani M, Ahrari F, Parisay I, Jahantigh M. The effects of three remineralizing agents on regression of white spot lesions in children: A two-week, single-blind, randomized clinical trial. J Clin Exp Dent. 2017;9:e641–8. doi: 10.4317/jced.53582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beerens MW, van der Veen MH, van Beek H, ten Cate JM. Effects of casein phosphopeptide amorphous calcium fluoride phosphate paste on white spot lesions and dental plaque after orthodontic treatment: A 3-month follow-up. Eur J Oral Sci. 2010;118:610–7. doi: 10.1111/j.1600-0722.2010.00780.x. [DOI] [PubMed] [Google Scholar]


