Abstract
The present study examined full-flavor cigarette use among women of reproductive age to assess whether use is associated with greater nicotine dependence and smoking during pregnancy. We used data from the National Survey on Drug Use and Health (2005–2014). Consecutive years were combined to assure sufficient numbers of pregnant women. We examined whether use of full-flavor cigarettes was associated with greater odds of nicotine dependence using the Fagerstrom Test for Nicotine Dependence and Nicotine Dependence Syndrome Scale (NDSS), controlling for other smoking characteristics. We next compared prevalence of smoking and use of full-flavor versus lower-yield cigarettes among non-pregnant versus pregnant women and across trimesters. Lastly, we examined whether pregnancy was associated with greater odds of using full-flavor cigarettes after controlling for potential confounders. Use of full-flavor cigarettes was associated with greater adjusted odds of nicotine dependence compared to lower yields among non-pregnant (Fagerstrom: 2.50, 95% CI: 2.32,2.70; NDSS: 1.75, 95% CI: 1.62,1.88) and pregnant (Fagerstrom: 1.53, 95% CI: 1.13,2.05; NDSS: 1.53, 95% CI: 1.12,2.10) smokers. As smoking prevalence decreased among pregnant compared to non-pregnant women (14.31 ± 0.55% versus 22.73 ± 0.17%), prevalence of using full-flavor cigarettes increased (54.82 ± 1.63% versus 38.86 ± 0.35%). Similarly, as smoking prevalence decreased from 1st to 3rd trimester (19.65 ± 1.2%, 12.50 ± 0.84%, 11.3 ± 0.83%), prevalence of using full-flavor cigarettes increased (53.12 ± 2.53%, 50.57 + 2.92%, 63.63 ± 3.19%). Overall, pregnancy was associated with 1.43 (95% CI: 1.22, 1.68) greater adjusted odds of full-flavor cigarette use. These results indicate that users of full-flavor cigarettes have greater nicotine-dependence risk and lower likelihood of quitting smoking during pregnancy, relationships with potential for serious adverse maternal-infant health impacts.
Keywords: Cigarette smoking, Prevalence, Full-flavor cigarettes, Nicotine yield, Pregnancy, Women of reproductive age, Vulnerable populations, National Survey on Drug Use and Health
The 2009 Tobacco Control Act gives the U.S. Food and Drug Administration (FDA) regulatory authority over nicotine content levels in tobacco products (Family Smoking Prevention and Tobacco Control Act, 2009). This legislation grants the FDA authority to reduce although not eliminate nicotine levels in cigarettes if doing so protects public health. That authority is important because it creates the opportunity to eventually require that nicotine exposure levels from cigarettes fall below the threshold necessary to produce nicotine dependence, hence making it easier for current smokers to successfully quit if they choose to do so and preventing the development of dependence and chronic smoking among those newly initiated to cigarette smoking (Benowitz and Henningfield, 1994; Donny et al., 2015). This context underscores the importance of expanding scientific knowledge regarding the behavioral and health impacts of using cigarettes that vary in nicotine content and yield.
The present study was conducted to systematically extend two recent reports machine-estimated higher nicotine/tar yield (i.e., regular full-flavor) cigarettes. The first demonstrated that use of full-flavor cigarettes is associated with increased risk of nicotine dependence compared to lower nicotine/tar yield (light) cigarettes in nationally representative samples of adolescent and adult U.S. smokers (Redner et al., 2016). The second demonstrated that use of full-flavor cigarettes is overrepresented in populations that are especially vulnerable to smoking, and associated with increased odds of nicotine dependence within each of these vulnerable populations (Higgins et al., 2016a).
Important to clarify is that commercial higher and lower nicotine/tar yield cigarettes have the same nicotine content. The lower yield cigarettes are engineered through ventilation and other design features to dilute the smoke and reduce nicotine and tar exposures compared to the higher yield cigarettes. There is broad scientific consensus that users of lower yield cigarettes commonly engage in compensatory smoking by blocking the ventilation holes or altering their smoking topography in order to achieve desired nicotine blood levels thereby undermining the goal of reducing health impacts by lowering toxin exposure (Kozlowski et al., 2001). However, less well recognized is that compensatory smoking is typically partial with regard to nicotine exposure, typically about 75% (Scherer and Lee, 2014). The evidence from the studies mentioned above suggest that this average 25% difference in nicotine exposure levels between higher and lower yield cigarettes in nicotine exposure levels may be sufficient to result in differences in nicotine-dependence risk, which is concerning as nicotine dependence is considered to be a major contributor to the emergence and persistence of chronic smoking and difficulties quitting (Shiffman et al., 2004; U.S. Department of Health and Human Services, 1988; U.S. Department of Health and Human Services, 2014).
The purpose of the present study is to examine whether use of these higher yield or full-flavor cigarettes is associated with increased risk of nicotine dependence in pregnant smokers (Higgins et al., 2016a; Redner et al., 2016). Pregnant smokers are highly vulnerable to serious adverse maternal and infant health impacts from smoking (Cnattingius, 2004; Dietz et al., 2010). Of even greater interest is whether use of full-flavor cigarettes is overrepresented among (a) pregnant compared to non-pregnant smokers and (b) women in late compared to early pregnancy suggesting a lower likelihood of quitting among users of full-flavor cigarettes. It is well established that the overall prevalence of smoking decreases among pregnant compared to non-pregnant women as many quit smoking upon learning of a pregnancy (Heil et al., 2014; Solomon and Quinn, 2004; Tong et al., 2013). Hence, if prevalence of using full-flavor cigarettes is greater among pregnant compared to non-pregnant female smokers of reproductive age, it would suggest that women using full-flavor cigarettes may be less likely to quit smoking upon learning of a pregnancy. Similarly, overall smoking prevalence decreases during the course of pregnancy with the lowest prevalence seen in the third trimester (Alshaarawy and Anthony, 2015). If prevalence of using full-flavor cigarettes is greater among smokers who are later compared to earlier in the course of pregnancy, that too would suggest that women using full-flavor cigarettes may be less likely to quit smoking during pregnancy. Use of full-flavor cigarettes is associated with certain characteristics that also predict a lower likelihood of quitting during pregnancy such as lower educational attainment, poverty, and co-morbid other substance use disorders. Thus, we examined whether use of full-flavor cigarettes was overrepresented among pregnant smokers after controlling for these other characteristics as well as cigarettes smoked per day and age of smoking initiation.
1. Method
1.1. Data source
The National Survey on Drug Use and Health (NSDUH) is a nationally representative survey of the U.S. non-institutionalized population aged ≥ 12 years that measures prevalence and correlates of drug use. Detailed descriptions of survey procedures have been provided for each of the survey years (Center for Behavioral Health Statistics and Quality, 2014). We used the most recent ten (2005–2014) years at the time the study analyses were conducted and opted to combine across survey years for purposes of having a sufficient number of pregnant women to compare prevalence of smoking and use of full-flavor versus lower-yield cigarettes among non-pregnant versus pregnant women and by trimester within pregnancy (Substance Abuse and Mental Health Services Administration, 2006, 2007, 2008, 2009, 2010, 2011, 2012, 2013, 2014, 2015). Across each of the survey years, NSDUH recruitment was completed using a multistage area probability sample design in which a predetermined number of participants were randomly recruited by address within each state. Respondents completed computer- and audio-assisted structured interviews. Respondents were selected from the civilian non-institutionalized population, including group homes, shelters, and college dormitories. Individuals on active military duty, in residential drug treatment programs, in jail, or homeless without residence were excluded. The present study included 199,784 females of reproductive age (15–44), including 43,432 current smokers, 1671 of whom were pregnant. Data were weighted during analysis to adjust for the differential probability of both selection and response.
Current smoker status was defined as smoking all or part of a cigarette within the 30 days preceding the interview and at least 100 cigarettes lifetime. Number of cigarettes smoked per day was collected as a categorical variable, ranging from less than one to >35 (7 levels), and age of smoking initiation was a recorded as a continuous variable. Respondents indicated whether they were pregnant (yes/no) and the trimester of their pregnancy. The NSDUH asks current smokers the first item on the Fagerstrom Test for Nicotine Dependence regarding how soon after waking soon they smoke their first cigarette, with those who report smoking within 30 min classified as nicotine dependent. The NSDUH also has smokers complete the Nicotine Dependence Syndrome Scale (NDSS). Use of full-flavor cigarettes has been associated with increased odds of nicotine dependence across both measures of dependence in prior studies (Higgins et al., 2016a; Redner et al., 2016). Both were included in the present study. Educational attainment was defined as less than high school, high school only, some college, or a 4-year college degree or more. Poverty status (living below or at/above the federal poverty line) was defined using poverty thresholds published by the U.S. Census Bureau. The six racial/ethnic categories used in the survey were mutually exclusive. Persons identified as Hispanic might be of any race while persons identified as White, Black, Asian, American Indian/Alaska Native, or Other were all non-Hispanic. The category “Other” included Native Hawaiians or Other Pacific Islanders and individuals endorsing two or more races. Any mental illness was defined as having a mental, behavioral, or emotional disorder in the past 12 months, excluding developmental or substance use disorders. Past year alcohol and illicit drug abuse/dependence diagnoses were also based on DSM-IV criteria.
1.2. Cigarette type
Smokers in the NSDUH were asked to indicate the type of cigarette they usually smoke. More specifically, they were asked: “During the past 30 days, what type of cigarettes did you smoke most often?” Respondents selected one of four options: full-flavor, medium, light, or ultra-light. For purposes of the present project, responses were dichotomized into use of full-flavor versus other (i.e., medium, light, and ultra-light), as has been done previously (Higgins et al., 2016a). Doing so keeps the focus on the cigarette type associated with the greatest risk for nicotine dependence (Redner et al., 2016) and limits the number of independent variables examined in statistical modeling thereby reducing risk of type 1 error.
1.3. Statistical methods
After combining data from 2005 through 2014 and dividing the person-level sample weight by 10, data were limited to women between the ages of 15 and 44 who were current smokers. Sample-adjusted frequencies and 95% confidence intervals (CIs) were generated across all respondents. Variables of interest for examining risk for nicotine dependence were based on prior studies on this topic (Higgins et al., 2016a; Redner et al., 2016). Variable of interest for examining predictors of full-flavor cigarette use were based on previously identified socioeconomic and sociodemographic independent predictors of cigarette smoking generally (Higgins et al., 2016b) and using full-flavor cigarettes specifically (Higgins et al., 2016a), including educational attainment, poverty status, age, sex, race/ethnicity, alcohol abuse/dependence, and illicit drug abuse/dependence. Pregnancy status and trimester of pregnancy were also included as predictors based on the specific purposes of the present study.
Associations of these risk factors with preference for full-flavor versus lower-yield cigarettes were examined. For each risk factor, weighted, univariate logistic regression was used to determine which variables would be included in subsequent multivariable models. Multiple logistic regression was then used to examine whether odds of nicotine dependence was greater among pregnant than non-pregnant women after controlling for cigarettes smoked per day and age of smoking initiation. Multiple logistic regression was also used to analyze preference for full-flavor cigarettes, using all variables from univariate logistic regression that significantly predicted full-flavor preference, while controlling for cigarettes per day and age of smoking initiation. PROC SURVEYLOGISTIC in SAS (SAS Institute, Cary, NC) was used to conduct these analyses. Variances were estimated using Taylor series linearization. Odds ratios (with 95% CIs) were generated. Across all tests, statistical significance was defined as p < 0.05 (2-tailed).
2. Results
2.1. Multiple regression modeling of nicotine dependence
Adjusted odds of nicotine dependence were greater among users of full-flavor compared to lower-yield cigarettes across both measures of nicotine dependence and subgroups of smokers: pregnant smokers (Fagerstrom: 1.53, 95% CI: 1.13, 2.05; NDSS: 1.53, 95% CI: 1.12, 2.10) and non-pregnant smokers (2.50, 95% CI: 2.32, 2.70; NDSS: 1.75, 95% CI: 1.62, 1.88).
2.2. Prevalence of smoking and use of full-flavor cigarettes
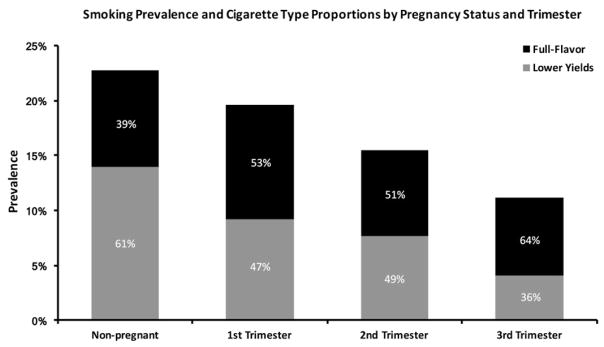
Smoking prevalence was lower among pregnant than non-pregnant women, with 14.31% (95% CI: 13.24, 15.42) and 22.73% (95% CI: 22.38, 23.07) of pregnant and non-pregnant women categorized as current smokers, respectively. By contrast, prevalence of using full-flavor cigarettes was greater among pregnant compared to non-pregnant women, with 54.82% (95% CI: 51.58, 58.05) and 38.86% (38.17, 39.55) of pregnant and non-pregnant categorized as full-flavor cigarette users, respectively (Fig. 1).
Fig. 1.
Bar graph showing prevalence of smoking among non-pregnant and pregnant women of reproductive age (15–44 years). Shown within each bar are the proportions of smokers whose usual brand of cigarette was machine-estimated full-flavor (black) versus a lower yield (gray).
The data source is the National Survey on Drug Use and Health (2005–2014).
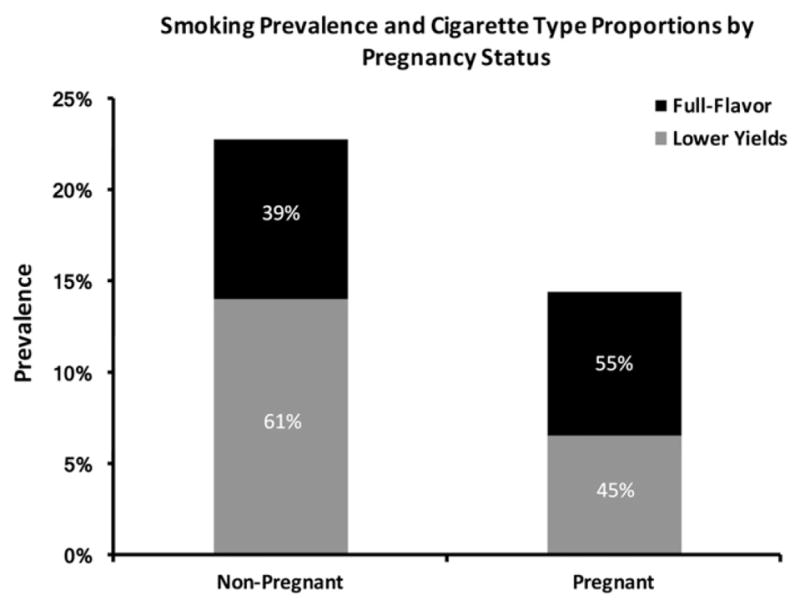
Smoking prevalence also decreased across trimesters, with 19.65% (95% CI: 17.35, 21.95), 12.50% (95% CI: 10.84, 14.17), and 11.13% (95% CI: 9.48, 12.78) of women in their first, second, and third trimesters of pregnancy categorized as smokers, respectively. Prevalence of using full-flavor cigarettes among smokers in the first and second trimesters was 53.12% (95% CI: 48.12, 58.13) and 50.57% (44.78, 56.36), respectively, each well above levels seen among non-pregnant smokers, and increased further to 63.63% (95% CI: 57.31, 69.96) in the third trimester, which was the maximal level observed in the study (Fig. 2).
Fig. 2.
Bar graph showing prevalence of smoking among non-pregnant and pregnant women of reproductive age (15–44 years), with results from the pregnant women displayed by trimester. Shown within each bar are the proportions of smokers whose usual brand of cigarette was machine-estimated full-flavor (black) versus a lower yield (gray).
The data source is the National Survey on Drug Use and Health (2005–2014).
2.3. Multiple logistic regression modeling of full-flavor use
Collapsing across trimesters, pregnant smokers had 1.43 (95% CI: 1.22, 1.68) times greater adjusted odds of using full-flavor cigarettes than non-pregnant smokers (Table 1). Other characteristics associated with greater odds of full-flavor use were younger age, less than a college education, non-Asian race/ethnicity, annual income below the federal poverty level, past year drug abuse or dependence, heavier smoking, and earlier age of smoking initiation. The characteristic examined that was not associated with increased odds of using full-flavor cigarettes was past year alcohol abuse, which predicted lower risk.
Table 1.
Unadjusted and final adjusted multiple logistic regressions with sociodemographic and other characteristics predicting use of full-flavor (high-yield) cigarettes among female smokers of reproductive age (15–44) in the 2005–2014 National Survey on Drug Use and Health (N = 43,432).
| Unadjusted model | Final adjusted model | |||
|---|---|---|---|---|
|
|
|
|||
| OR | CI | AOR | CI | |
| Currently pregnant | 1.90 | (1.67, 2.18) | 1.43 | (1.22, 1.67) |
| Age | ||||
| 15–17 | 2.63 | (2.36, 2.93) | 7.39 | (6.24, 8.75) |
| 18–25 | 1.58 | (1.50, 1.67) | 1.57 | (1.48, 1.66) |
| 26–44 | Ref | Ref | ||
| Education | ||||
| Less than high school | 8.30 | (7.16, 9.62) | 4.45 | (3.80, 5.22) |
| High school graduate | 4.44 | (3.89, 5.06) | 2.91 | (2.55, 3.33) |
| Some college | 2.87 | (2.49, 3.31) | 2.09 | (1.81, 2.42) |
| College graduate | Ref | Ref | ||
| Living in poverty | 2.97 | (2.76, 3.19) | 1.99 | (1.85, 2.15) |
| Race | ||||
| Asian | Ref | Ref | ||
| Black | 10.91 | (7.63, 15.61) | 7.89 | (5.20, 11.97) |
| Latino | 2.25 | (1.62, 3.13) | 1.55 | (1.05, 2.27) |
| Native American | 2.52 | (1.65, 3.83) | 1.32 | (0.80, 2.18) |
| White | 1.68 | (1.21, 2.32) | 1.04 | (0.71, 1.53) |
| Other | 2.43 | (1.68, 3.52) | 1.48 | (0.97, 2.25) |
| Age of first cigarette | 0.97 | (0.96, 0.98) | 0.96 | (0.95, 0.97) |
| Cigarettes per day | ||||
| <1 | 0.62 | (0.53, 0.73) | 0.74 | (0.62, 0.90) |
| 1 | 0.65 | (0.57, 0.74) | 0.75 | (0.66, 0.87) |
| 2 to 5 | Ref | Ref | ||
| 6 to 15 | 1.35 | (1.25, 1.45) | 1.59 | (1.46, 1.74) |
| 16 to 25 | 1.20 | (1.10, 1.31) | 1.63 | (1.49, 1.79) |
| 26 to 35 | 1.27 | (1.04, 1.56) | 1.58 | (1.28, 1.95) |
| >35 | 1.81 | (1.37, 2.39) | 1.80 | (1.32, 2.46) |
| Alcohol abuse or dependence | 0.91 | (0.84, 0.98) | 0.80 | (0.73, 0.87) |
| Drug abuse or dependence | 1.92 | (1.74, 2.12) | 1.60 | (1.41, 1.82) |
Notes. “Other” includes multiracial and Hawaiian/Pacific Islander (due to small sample sizes).
OR= odds ratio, AOR = adjusted odds ratio, CI= confidence interval.
3. Discussion
The present study replicates the results of prior studies demonstrating increased odds of nicotine dependence among users of full-flavor compared to lower yield cigarettes in the general population and socioeconomically disadvantaged and other vulnerable populations of smokers and extends them to pregnant women. The present study also provides evidence that using full-flavor cigarettes is associated with continuing to smoke during pregnancy. That is, the pattern of results observed in the present study where the proportion of women using full-flavor cigarettes increased among pregnant compared to non-pregnant women as the prevalence of smoking decreased in those two groups is consistent with users of the higher yield cigarettes being less likely to quit smoking during pregnancy. Seeing the same pattern where the proportion of women using full-flavor cigarettes increased as prevalence of smoking decreased between those late compared to early in pregnancy further suggests that those using higher estimated yield cigarettes are not quitting during pregnancy at the same rate as those using lower estimated yield brands. The results from the multivariate model indicate that this overrepresentation of full-flavor cigarette use during pregnancy is independent of other socio-demographics, psychiatric characteristics, or smoking characteristics known to be associated with using full-flavor cigarettes (Higgins et al., 2016a) as well as smoking during pregnancy (Kurti et al., 2017)—younger age, lower educational attainment, race/ethnicity, poverty, drug use disorders, heavier smoking, and early smoking initiation.
This pattern of results is also consistent with the possibility that use of full-flavor cigarettes may directly undermine efforts to quit smoking. Use of full-flavor cigarettes is associated with increased risk of nicotine dependence in the present and prior studies, which is a well-established predictor of greater difficulties quitting smoking (Shiffman et al., 2004; U.S. Department of Health and Human Services, 1988; U.S. Department of Health and Human Services, 2014). So there is a plausible mechanism by which use of full-flavor cigarettes could undermine quitting. Alternatively, of course, there is the logical possibility that this association between use of full-flavor cigarettes and pregnancy is attributable to women who use lower estimated yield cigarettes switching to full-flavor cigarettes upon learning of a pregnancy. Although there is nothing in this cross-sectional observational study that can rule out that possibility, we know of no evidence of pregnant women taking steps that might increase nicotine exposure levels upon learning of a pregnancy aside from possibly using nicotine replacement therapy or more recently e-cigarettes in efforts to quit smoking (Chivers et al., 2016). Instead, the literature on cigarette smoking during pregnancy indicates that the majority of women quit or at least reduce their smoking upon learning of a pregnancy while a small minority maintain pre-pregnancy smoking practices (e.g., Heil et al., 2014). So while logically possible, that pathway seems highly unlikely based on current knowledge about smoking during pregnancy. Despite our efforts to control for confounding, there is also the possibility that a third variable(s), such as a lower level of health-related risk aversion, for example, might increase both the likelihood of using full-flavor cigarettes and continuing to smoke during pregnancy. We do not know of any such evidence but again it cannot be ruled out based on the data in this study. We know that risk for being a smoker among women of reproductive age is associated with impulsive decision-making (Chivers et al., 2016) and thus it seems plausible that some such bias in decision-making could potentially increase risk for using higher nicotine-yield cigarettes and being less sensitive to the risks of smoking during pregnancy. Also possible is a combined effect of full-flavor cigarette use directly undermining quitting via greater nicotine dependence and the influence of some third variable. Prospective observational and experimental studies examining cigarette type and likelihood of quitting during pregnancy should be helpful in parsing out some of these possibilities.
In terms of tobacco control and regulatory implications, the present study provides strong evidence from nationally representative samples that use of full-flavor cigarettes is associated with increased odds of nicotine dependence and a lower likelihood of quitting smoking during pregnancy. The literature on use of full-flavor compared to lower estimated yield cigarettes indicates that on average use of the former is associated with approximately 25% greater nicotine exposure (Scherer and Lee, 2014). Considering that nicotine is a well-documented neuro-toxin and contributor to other adverse developmental effects of maternal cigarette smoking (England et al., 2017), there is little question that this association of full-flavor cigarette use and smoking in pregnancy has the potential for serious adverse public health impacts. Efforts to reduce use of full-flavor cigarettes among pregnant women are certainly warranted. Perhaps use of full-flavor cigarettes should be an indicator for providing financial incentives or some other more intensive cessation intervention (Chamberlain et al., 2017; Higgins and Solomon, 2016). At first blush, recommending lower machine-estimated yield cigarettes may appear to represent a viable alternative in terms of being associated with a lower likelihood of dependence and greater likelihood of quitting during pregnancy, but the concern is that should pregnant women who use those products engage in compensatory smoking involving greater puff volume, deeper inhalation, or increased smoking rates, it could increase risk for other serious adverse developmental impacts and pregnancy complications related to increased exposure to carbon monoxide or other toxins. So there is no obviously safer combusted substitute to recommend for pregnant women at this time. However, taking a longer-term view, the present results, in combination with those reported previously on full-flavor cigarette use and greater nicotine-dependence risk, provide additional reasons for FDA to consider lowering the maximal nicotine content of cigarettes. Unlike commercially available light cigarettes, which leave nicotine content unchanged and instead attempt to reduce nicotine yield through filter ventilation, very low nicotine content (VLNC) cigarettes reduce nicotine exposure and dependence levels with minimal compensatory smoking (Benowitz et al., 2012; Donny et al., 2015; Hatsukami et al., 2010). That profile of effects suggests that women of reproductive age using VLNC cigarettes should have lower risk of nicotine dependence and hence greater chance of successfully quitting should they become pregnant. Those who were unable to quit presumably would have lower gestational nicotine exposure levels compared to those using currently available commercial cigarettes. Studies on VNLC cigarettes in pregnant and non-pregnant women of reproductive age will be necessary to determine the accuracy of those projections, but they seem reasonable based on current knowledge. There are already many important and compelling reasons for lowering maximal nicotine content levels in cigarettes to reduce smoking prevalence, tobacco addiction and smoking-related harms more generally. The present results add an important additional rationale to that list.
As noted above, the present study has the limitation of being a cross-sectional, observational survey, which cannot support causal inferences. Additionally, smoking practices in the NSDUH survey are based exclusively on self-report and thus subject to misreporting, which with pregnant women is likely to result in some level of under-reporting the prevalence of smoking due to the stigma associated with smoking during pregnancy. The present study focused exclusively on associations between cigarette type and likelihood of smoking during pregnancy. Certainly other factors in addition to cigarette type predict smoking during pregnancy and that topic is being addressed in other contributions to this special issue (Kurti et al., 2017). Those limitations notwithstanding, we believe the present study provides new knowledge on an important topic that has the potential to inform researchers, clinicians, and policy makers about risks associated with use of full-flavor cigarettes among women of reproductive age.
Acknowledgments
Funding
This project was supported by Tobacco Centers of Regulatory Science award P50DA036114 from the National Institute on Drug Abuse (NIDA) and Food and Drug Administration (FDA), Center of Biomedical Research Excellence award P20GM103644 from the National Institute of General Medical Sciences (NIGMS), and Research award R01HD075669 from the National Institute of Child Health and Human Development (NICHD) and Centers for Disease Control and Prevention (CDC). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIDA, FDA, NIGMS, NICHD, or CDC.
Footnotes
Transparency document
The Transparency document associated with this article can be found, in the online version.
Disclosures
The authors have nothing to declare other than the federal research support acknowledged above.
References
- Alshaarawy O, Anthony JC. Month-wise estimates of tobacco smoking during pregnancy for the United States, 2002–2009. Matern Child Health J. 2015;19(5):1010–1015. doi: 10.1007/s10995-014-1599-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL, Henningfield JE. Establishing a nicotine threshold for addiction: the implications for tobacco regulation. NEJM. 1994;331:123–125. doi: 10.1056/NEJM199407143310212. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Dains KM, Hall SM, Stewart S, Wilson M, Dempsey D, Jacob P., 3rd Smoking behavior and exposure to tobacco toxicants during 6 months of smoking progressively reduced nicotine content cigarettes. Cancer Epidemiol Biomark Prev. 2012;21:761–769. doi: 10.1158/1055-9965.EPI-11-0644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. 2013 national survey on drug use and health public use file codebook. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. [Accessed date: 23 March 2017]. http://www.icpsr.umich.edu/cgi-bin/file?comp=none&study=35509&ds=1&file_id=1166336&path=SAMHDA. [Google Scholar]
- Chamberlain C, O’Mara-Eves A, Porter J, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev. 2017;2:Cd001055. doi: 10.1002/14651858.CD001055.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chivers LL, Hand DJ, Priest JS, Higgins ST. E-cigarette use among women of reproductive age: impulsivity, cigarette smoking status, and other risk factors. Prev Med. 2016;92:126–134. doi: 10.1016/j.ypmed.2016.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cnattingius S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res. 2004;(Suppl 2):S125–40. doi: 10.1080/14622200410001669187. [DOI] [PubMed] [Google Scholar]
- Dietz PM, England LJ, Shapiro-Mendoza CK, et al. Infant morbidity and mortality attributable to prenatal smoking in the U.S. Am J Prev Med. 2010;39(1):45–52. doi: 10.1016/j.amepre.2010.03.009. [DOI] [PubMed] [Google Scholar]
- Donny EC, Denlinger RL, Tidey JW, Koopmeiners JS, Benowitz NL, Vandrey RG, al’Absi M, Carmella SG, Cinciripini PM, Dermody SS, Drobes DJ, Hecht SS, Jensen J, Lane T, Le CT, McClernon FJ, Montoya ID, Murphy SE, Robinson JD, Stitzer ML, Strasser AA, Tindle H, Hatsukami DK. Randomized trial of reduced nicotine standards for cigarettes. NEJM. 2015;373:1340–1349. doi: 10.1056/NEJMsa1502403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- England LJ, Aagaard K, Bloch M, Conway K, Cosgraove K, Grana R, Gould TJ, Hatsukami D, Jensen F, Kandel D, Lanphear B, Leslie F, Pauly JR, Neiderhiser J, Rubinstein M, Slotkin TA, Spindel E, Stroud L, Wakschlag L. Developmental toxicity of nicotine: a transdisciplinary synthesis and implications for emerging tobacco products. Neurosci Biobehav Rev. 2017;72:176–189. doi: 10.1016/j.neubiorev.2016.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [Accessed date: 23 March 2017];Family Smoking Prevention and Tobacco Control Act (H.R. 1256) 2009 https://www.govtrack.us/congress/bills/111/hr1256/text.
- Hatsukami DK, Kotlyar M, Hertsgaard LA, Zhang Y, Carmella SG, Jensen JA, Allen SS, Shields PG, Murphy SE, Stepanov I, Hecht SS. Reduced nicotine content cigarettes: effects on toxicant exposure, dependence, and cessation. Addiction. 2010;105:343–355. doi: 10.1111/j.1360-0443.2009.02780.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heil SH, Herrmann ES, Badger GJ, Solomon IM, Higgins ST. Examining the timing of changes in cigarette smoking upon learning of a pregnancy. Prev Med. 2014;68:58–61. doi: 10.1016/j.ypmed.2014.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Solomon LJ. Some recent developments on financial incentives for cessation among pregnant and newly postpartum women. Curr Addict Rep. 2016;3:9–18. doi: 10.1007/s40429-016-0092-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Kurti AN, Redner R, White TJ, Keith DR, Gaalema DE, Sprague BL, Stanton CA, Roberts ME, Doogan NJ, Priest JS. Co-occurring risk factors for current cigarette smoking in a U.S. nationally representative sample. Prev Med. 2016a;92:110–117. doi: 10.1016/j.ypmed.2016.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Redner R, Priest JS, Bunn JY. Socioeconomic disadvantage and other risk factors for using higher-nicotine/tar-yield (regular full-flavor) cigarettes. Nicotine Tob Res. 2016b Aug 9; doi: 10.1093/ntr/ntw201. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlowski LT, O’Connor RJ, Sweeney CT. Cigarette design. Smoking and Tobacco Control Monograph 13. US Department of Health and Human Services, Public Health Services, National Institutes of Health; Bethesda, MD, USA: 2001. pp. 13–38. [Google Scholar]
- Kurti AN, Redner R, Lopez AA, Keith DR, Villanti AC, Stanton CA, Gaalema DE, Bunn JY, Doogan NJ, Cepeda-Benito A, Roberts ME, Phillips J, Higgins ST. Tobacco and nicotine delivery product use in a national sample of pregnant women. Prev Med. 2017;104:48–54. doi: 10.1016/j.ypmed.2017.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redner R, White TJ, Bunn JY, Higgins ST. Use of high-nicotine/tar-yield (full-flavor) cigarettes and risk for nicotine dependence in nationally representative samples of US smokers. Nicotine Tob Res. 2016;18:1424–1430. doi: 10.1093/ntr/ntv252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer G, Lee PN. Smoking behavior and compensation: a review of the literature and meta-analysis. Regul Toxicol Pharmacol. 2014;70:615–628. doi: 10.1016/j.yrtph.2014.09.008. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Solomon L, Quinn V. Spontaneous quitting: self-initiated smoking cessation in early pregnancy. Nicotine Tob Res. 2004;6(Suppl 2):S203–16. doi: 10.1080/14622200410001669132. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2005 National Survey on Drug Use and Health: Volume 1. Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2006. NSDUH Series H-30, HHS Publication No. (SMA) 06-4194. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2006 National Survey on Drug Use and Health: Volume 1. Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2007. NSDUH Series H-32, HHS Publication No. (SMA) 07-4293. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2007 National Survey on Drug Use and Health: Volume 1. Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2008. NSDUH Series H-34, HHS Publication No. (SMA) 08-4343. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2008 National Survey on Drug Use and Health: Volume 1. Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. NSDUH Series H-36, HHS Publication No. (SMA) 09-4434. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2009 National Survey on Drug Use and Health: Volume 1. Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2010. NSDUH Series H-38A, HHS Publication No. (SMA) 10-4586. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2011. NSDUH Series H-41, HHS Publication No. (SMA) 11-4658. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2011 National Survey on Drug Use and Health: Summary of the National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2012. NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2012 National Survey on Drug Use and Health: Summary of the National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2013 National Survey on Drug Use and Health: Summary of the National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results From the 2014 National Survey on Drug Use and Health: Summary of the National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2015. NSDUH Series H-50, HHS Publication No. (SMA) 15-4927. [Google Scholar]
- Tong VT, Dietz PM, Morrow B, D’Angelo DV, Farr SL, Rockhill KM, et al. Trends in smoking before, during, and after pregnancy—pregnancy risk assessment monitoring system, United States, 40 sites, 2000–2010. MMWR Morb Mortal Wkly Rep. 2013;62:1–19. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—Nicotine Addiction: A Report of the Surgeon General. United States Public Health Service, Office on Smoking and Health; Washington, DC: 1988. [Google Scholar]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health; Atlanta: 2014. [Google Scholar]