Abstract
Proximal humerus fractures constitute a significant percentage of fragility fractures. The growing use of locking plate has helped treat this problem, but at the same time has brought about complications. Past systematic reviews have documented these complications, however a large number of recent studies have been published since, reporting their own complication rates with different techniques. This study reviews the current complications associated with locking plate of proximal humerus fractures as well as methods to reduce them. A systematic review, following the PRISMA guidelines, was conducted in November 2013 and repeated in March 2015, using PubMed, Scopus, and Cochrane databases, to evaluate locking plate fixation (and complications) of traumatic proximal humerus fractures. Inclusion criteria included adults (>18 years), minimum of 12-month postoperative followup, articles within the last 5 years, and studies with >10 participants. Exclusion criteria included pathologic fractures, cadaveric studies, and nonhuman subjects. Eligible studies were graded using a quality scoring system. Articles with a minimum of 7/10 score were included and assessed regarding their level of evidence per the Journal of Bone and Joint Surgery and Centre for Evidence-Based Medicine guidelines. The initial query identified 51,206 articles from multiple databases. These records were thoroughly screened and resulted in 57 articles, consisting of seven Level 1, three Level 2, 10 Level 3, and 37 Level 4 studies, totaling 3422 proximal humerus fractures treated with locking plates. Intraarticular screw penetration was the most reported complication (9.5%), followed by varus collapse (6.8%), subacromial impingement (5.0%), avascular necrosis (4.6%), adhesive capsulitis (4.0%), nonunion (1.5%), and deep infection (1.4%). Reoperation occurred at a rate of 13.8%. Collapse at the fracture site contributed to a majority of the implant-related complications, which in turn were the main reasons for reoperation. The authors of these studies discussed different techniques that could be used to address these issues. Expanding use of locking plate in the proximal humerus fractures leads to improvements and advancements in surgical technique. Further research is necessary to outline indications to decrease complications, further.
Keywords: Fracture, proximal humerus, locking plate, complications
MeSH terms: Bone plates, humeral fractures, proximal, surgical complications
Introduction
Proximal humerus fractures represent a steadily growing problem within the health-care system. Proximal humerus fractures are the third-most common type of fragility fracture, accounting for nearly 6% of all adult fractures.1,2 In addition, as the world's population has aged, the incidence of this fracture type has increased as well.3 Surgical intervention for this fracture type is around 20%, due to the increase in complications as patients age.3,4 Surgical fixation with locking plates is the most common type of intervention for displaced proximal humerus fractures, though other options exist, such as closed reduction with percutaneous pinning, hemiarthroplasty, proximal humeral nailing, and reverse total shoulder arthroplasty.4,5
Locking plate represents a relatively new technology that theoretically supports fixation in the setting of osteoporotic bone.6 Its biomechanical properties made it promising in the setting of proximal humerus fractures, where purchase in the humeral head is difficult to obtain, due to large variations in bone density and strength.7 Understandably, complications were highly variable as locking plates first began to be used in the proximal humerus fractures. The first systematic review in this setting noted the importance of medial calcar support and the need for more attention to technical aspects of the procedure.8 Sproul et al. performed another review with a focus on length of followup, to more accurately capture the time frame necessary for the development of avascular necrosis (AVN) of the humeral head. The study confirmed factors for screw cutout and had similar rates of complications.9
Since the publication of these two reviews, there has been an increase in the literature, regarding locking plate fixation for proximal humerus fractures. In addition, studies have attempted to curtail the complication rates mentioned earlier with augmentation strategies such as fibular strut allograft, autograft, cancellous chips, suture fixation of the rotator cuff, and defined technical steps, regarding plate and screw placement. Recent years have shown an increase in the indications for the use of locking plates, as well as reverse total shoulder arthroplasty versus hemiarthroplasty in the setting of proximal humerus fractures.10,11 Given the relative infancy of locking plate fixation at the time of prior systematic reviews, and the small number of studies included within each review, a more recent systematic review of the literature is warranted. This study examines the current literature to evaluate complications experienced with locking plate in light of changes to operative technique as familiarity with this implant has increased.
Materials and Methods
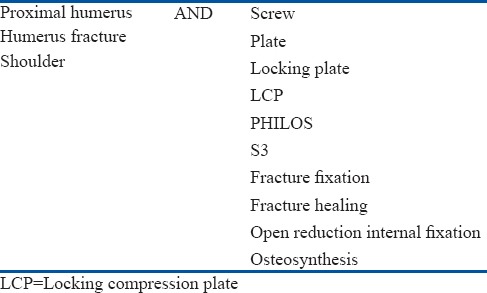
Following preregistration with PROSPERO (CRD42015019038), a comprehensive search of the literature was performed in November 2013 and repeated in February 2015, to capture recent publications, utilizing the PubMed, Cochrane, and Scopus databases.12 Database queries were performed using modifiers, limiting results to publications in the English language of the past 10 years, in studies involving human subjects. Search terms were intentionally broad to identify all relevant articles [Table 1].
Table 1.
Search terms used in the PubMed, Cochrane, and Scopus databases
The study design was conducted strictly in accordance with the PRISMA guidelines.12 The results were subsequently filtered for duplicates, and titles and abstracts were manually screened for relevance and potential adherence to our inclusion criteria. To be included, eligible studies must have been conducted in the past 5 years (modifier in initial query was 10 years to ensure broadness of search), involving 10 or more subjects, adults aged 18 years or older, and a minimum average followup of 12 months. International studies with the English translation were included. Studies involving pathologic fractures, nonhuman subjects (in vitro studies), and cadavers were excluded. Publications with overlapping or duplicate patient populations were excluded.
Next, articles were assigned a quality score using a previously published quality scoring system, which was also used by Sproul et al.9,13 The scoring system took into account the quality of the study design, as well as the quality of its information. Two reviewers scored the articles and only studies with a minimum score of 7/10 were included. Disagreements were resolved by consensus. Finally, the studies were graded in accordance with the Journal of Bone and Joint Surgery and Centre for Evidence-Based Medicine guidelines, to universally assess the level of evidence of each study. Statistics were performed by authors with training in biostatistics. Complication rates were analyzed in a simple manner, first divided by the total number of fractures treated and followed by stratification by level of evidence. There were no comparative analyses performed due to the heterogeneity of each study.
Results
The initial query conducted through the PubMed, Scopus, and Cochrane databases identified 51,206 citations. After removing duplicates and articles with irrelevant titles and abstracts, a total of 191 full-text articles were assessed for eligibility. From these 191 articles, 57 articles were included to be a part of this systematic review. The results of screening and application of inclusion/exclusion criteria are outlined in Figure 1.14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70
Figure 1.
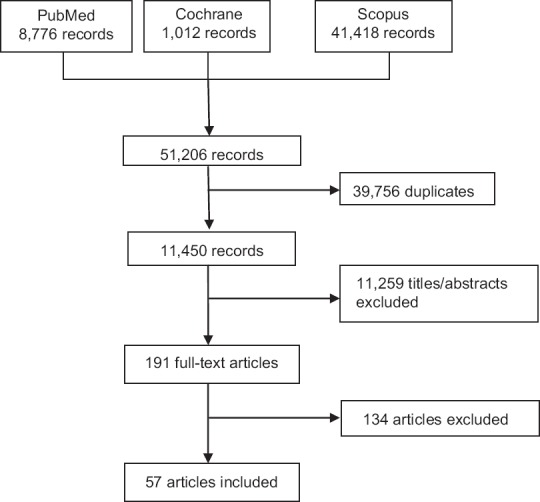
Flowchart showing selection of studies
There were seven Level 1, three Level 2, 10 Level 3, and 37 Level 4 studies. Level 1 and 2 studies included control groups in regard to surgical approaches, nonoperative treatment, various treatment modalities, or deferring operative techniques. Some Level 3 studies had a basis for comparison when evaluating different surgical approaches or operative techniques. Finally, Level 4 studies were case series without a basis for comparison. Some of these series investigated techniques such as strut allografts, suture fixation, bone grafting, and minimally invasive surgery.
There were a total of 3422 proximal humerus fractures that were treated with locking plate. Certain studies failed to mention or report the presence or absence of complications that were specifically being investigated. If this occurred, the study was not included in the complication's analysis. The most common complication was intraarticular screw penetration (9.5%), followed by varus collapse (6.8%), subacromial impingement (5.0%), AVN (4.6%), adhesive capsulitis (4.0%), nonunion (1.5%), and deep infection (1.4%). Reoperation occurred at a rate of 13.8%. Tables 2-9 display these rates of complications broken down by levels of evidence.
Table 2.
Rate of intraarticular screw penetration
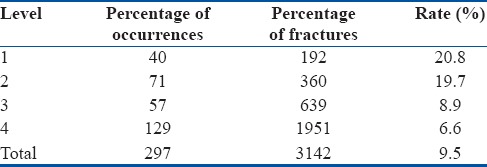
Table 9.
Rate of reoperation
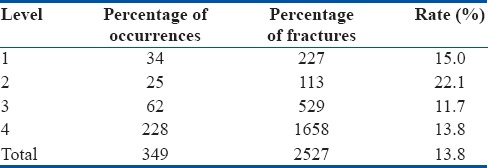
Table 3.
Rate of varus collapse
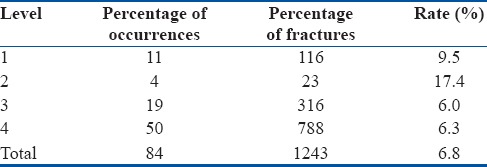
Table 4.
Rate of subacromial impingement
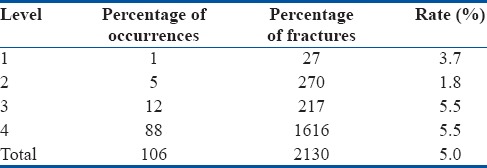
Table 5.
Rate of avascular necrosis
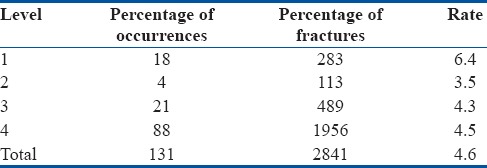
Table 6.
Rate of adhesive capsulitis
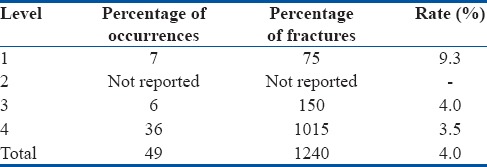
Table 7.
Rate of nonunion
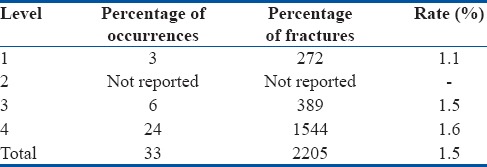
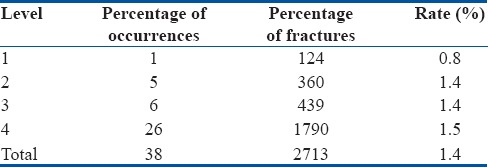
Table 8.
Rate of deep infection
Discussion
Intraarticular screw penetration (9.5%)
Intraarticular screw penetration through the humeral head has been noted as a problematic complication and may lead to additional surgery to revise or remove the screw(s). Two different screw penetrations have been discussed: primary and secondary. Primary screw penetration refers to the intraoperative placement of screws into the glenohumeral joint. Secondary screw penetration refers to the screws that have violated the articular surface as a result of collapse of the humeral head due to varus collapse, AVN, or failure of fixation. Reports from the earlier literature show the prevalence of this complication to range from 0% to 23%.71 Sproul et al. demonstrated this complication to be at a rate of 7.5%.9
Level 1
Fjalestad et al. reported that the majority of these complications occurred in patients with Orthopaedic Trauma Association (OTA) Type C fractures, with evidence of AVN.27 Another study noted that attempts to obtain maximal purchase into the humeral head led to higher rates of primary screw penetrations. The authors adjusted their surgical technique by placing screws 2 mm–3 mm away from the subchondral bone, as was done in another level 1 study.48,70 In comparing different plates, Voigt et al. found that polyaxial locking screws with blunted ends could be advantageous if screw penetration were to occur.65
Level 2
Buecking et al. observed that complications pertaining to the humeral head were higher in their deltoid-splitting approach group, while complications pertaining to the humeral shaft were higher in their deltopectoral approach group.19 Konrad et al. reported screw penetration, not varus collapse or loosening, as the most common complication with locking plate in their large multicenter study of 270 patients.34
Level 3
In a study comparing locking plate fixation with calcium phosphate cement augmentation versus cancellous bone chips versus no augmentation, Egol et al. demonstrated a significant decrease in intraarticular screw penetration with calcium phosphate cement augmentation. In addition, there was no association between the number of screws in the humeral head and screw penetration. However, age was associated with screw penetration as elderly patients sustained this complication more frequently.26
Level 4
Little et al. described five incidences of asymptomatic screw penetration in their series evaluating 72 cases, for which endosteal augmentation was used. The authors believed that this intramedullary graft decreased the working length of the locking screws.38 Ricchetti et al. reported no cases of screw penetration in their series of 54 fractures followed for 13 months. The authors described using screws 5 mm–10 mm away from the subchondral bone to decrease the risk of screw perforation both primarily and secondarily, should collapse occur. This technique has also been reported in a review article by Ricchetti et al.52,71 Spross et al. noted that, by placing screws 4 mm–5 mm away from the subchondral bone, complications regarding intraarticular screw penetration decreased significantly. They also advocated the use of fluoroscopy in three planes in an attempt to avoid missing primary screw penetrations.62
Varus collapse (6.8%)
Varus collapse represents one of the more important complications in the setting of locking plate in proximal humerus fractures. Varus collapse is responsible for secondary subacromial impingement and screw penetration into the articular surface of the glenohumeral joint. Sproul et al. reported this as the most common complication in their review, at a rate of 16.3%.9 The authors recommended that special attention should be paid to the medial column, which has led some surgeons to place inferomedial support screws, cement, or graft in hopes of lowering this complication rate.
Level 1
In comparing polyaxial versus monoaxial locking screws, Voigt et al. noted an increase in the rate of varus deformity in the group treated with monoaxial screws. The authors felt that polyaxial screws gave more options for screw placement inferomedially.65 Zhang et al. postulated that inferomedially placed support screws would resist varus stress to the humeral head, therefore maintaining neck shaft angle in three- and four-part fractures.69
Level 2
Evaluating a new carbon fiber–reinforced-polyetheretherketone (CFR-PEEK) locking plate, Schliemann et al. showed a lower rate of varus deformity in comparison to the control titanium locking plate. They believed that this was due to CFR-PEEK being less rigid and having a similar elastic modulus to bone.58
Level 3
Lin et al. reported low rates of varus collapse in both their minimally invasive and deltopectoral approach groups. However, they attributed a slightly higher rate within the minimally invasive group due to a false sense of security with progression through weight-bearing exercises because of faster wound healing and smaller scars.37
Level 4
Ricchetti et al. discussed additional contouring of the locking plate as a method to reduce the incidence of varus malunion as it aids in obtaining an anatomic neck–shaft angle. In addition, they placed bone graft for complicated three- and four-part fractures.52 Kim et al. performed a study using autologous iliac bone impaction graft with locking plate of four-part fractures and reported 0 incidences of varus collapse in 21 cases over a 27.5-month followup period. The authors believed that their meticulous attention to restoring the medial calcar, obtaining sufficient screw purchase in the inferomedial aspect of the humeral head, and suturing the rotator cuff to the plate led to such positive results.32 Badman et al. reported on 81 proximal humerus fractures, a majority of which were three-part fractures. The authors focused on supplemental suture fixation of the rotator cuff in the five cases of varus collapse and also used structural allograft in the setting of severe osteopenia.16
Subacromial impingement (5.0%)
Subacromial impingement can be the result of poor intraoperative plate positioning or the sequelae of humeral head collapse. Impingement is frequently symptomatic and may require plate removal. Sproul et al. reported this complication at a rate of 4.8%.9 Increased attention to plate placement and preventing varus collapse are the methods surgeons are using to decrease this complication.
Level 1
Only one study mentioned a case of subacromial impingement. Olerud et al. reported one patient in their treatment group of 27 cases with three-part fractures, who subsequently required plate removal. The authors recommended averting humeral head collapse to prevent this complication.48
Level 2
Konrad et al. attributed their cases of impingement to placing the plate too superiorly, leading to five cases in their study population of 270.34
Level 3
Lin et al. attributed their cases of impingement to varus collapse, while Jung et al. attributed their one case to intraoperative error.31,37 Jung et al. described their operative positioning of the plate following reduction as caudal to the superior end of the greater tuberosity and lateral to the bicipital groove.31 Bachelier et al. instead specified plate position 1 cm caudal to the superior aspect of the greater tuberosity.15
Level 4
Sahu reported no case of impingement, taking the shoulder through a range of motion arc before closure of the wound to detect any symptoms of impingement.55 Osterhoff et al. described the majority of their 10 cases of impingement to be strongly associated with medial calcar comminution.49 Ricchetti et al. positioned the locking plate 5 mm–10 mm lateral to the bicipital groove and 15 mm–20 mm caudal to the tip of the greater tuberosity. Two patients in their series of 54 cases had postoperative subacromial impingement symptoms.52 Finally, Aggarwal et al. described provisionally fixing the plate with K-wires and placing the shoulder through a range of motion arc under fluoroscopy. This technique resulted in five cases of impingement in their series of 47.14
Avascular necrosis (4.4%)
AVN has been a historic concern with proximal humerus fractures. Sproul et al. reported this rate to affect 10.8% of patients.9 This has even led to studies attempting to discover predictors of necrosis, following a proximal humerus fracture. Hertel et al. determined that the most relevant factors included integrity of the medial hinge, length of the dorsomedial metaphyseal extension, and different fracture types.72 Furthermore, growing indications for reverse total shoulder arthroplasty and recent favorable studies in comparison to hemiarthroplasty may have artificially decreased the rate of AVN currently being reported.73 In addition, AVN may present later in followup and inadequate lengths of followup would, in turn, under report this complication. Recent studies have attempted to use deltoid-splitting or minimally invasive approaches with the belief that less soft tissue disruption in proximity to the humeral head would preserve its blood supply. Finally, there is growing belief that asymptomatic cases of AVN can potentially over-report this serious complication.
Level 1
Comparing the minimally invasive approach to the deltopectoral approach, Liu et al. reported one case of AVN in the latter group and zero in the former. The authors believed that the minimally invasive approach decreased soft tissue stripping and preserved the blood supply around the proximal humerus.39 Zhang et al. reported only one case of AVN in their study that focused on medial support screws using a deltopectoral approach. In their opinion, preventing medial collapse also aided in preventing AVN.69 Interestingly, the findings from Fjalestad et al. showed that nonoperatively treated patients had a higher rate of AVN than those in the operative group. All patients had displaced three- and four-part fractures.27
Level 2
Buecking et al. reported no case of AVN and no difference between deltoid-splitting and deltopectoral approaches. Followup, however, was only for 1 year.19 Schliemann et al. reported a lower incidence of AVN in patients treated with their CFR-PEEK implant compared to conventional locking plate. Their followup was for a minimum of 2 years.58
Level 3
Martetschlager et al. reported higher rates of AVN in patients treated with a deltopectoral approach compared to a minimally invasive deltoid-splitting approach. With a mean followup of nearly 4 years, AVN was diagnosed in six of 33 patients in the deltopectoral approach group and one of 37 patients in the deltoid-splitting approach group.41 Wu et al. reported similar findings over a mean followup of 2.5 years in comparing a minimally invasive approach to a deltopectoral approach.67
Level 4
Using a minimally invasive plating technique and a mean followup of nearly 3 years, Chen et al. reported only one case of AVN in their series of 64 cases.21 Little et al. reported low rates of AVN as well by using a deltoid splitting approach and a medial strut allograft.38 On the other hand, Spross et al. reported 20 cases of AVN in their large case series of 294 followed for 1 year. The patients were treated using a deltopectoral approach. The authors determined, however, that fracture type influenced whether AVN occurred or not, with fracture dislocations having the highest rate.62
Reoperations (13.8%)
Reoperations are a very important measure of how successful the index operation was and also highlight the most significant complications. Reoperations also highlight possible improvements in surgical decision-making or technique to avoid certain complications. Even in regard to AVN, more meticulous soft tissue management, attempts at minimally invasive techniques, and consideration of arthroplasty as primary surgery have led to a decrease in reoperation. It is also important to make a distinction between “planned” versus “unplanned” operations as many patients do request to have hardware removed. Hardware removal has been associated with a very low complication rate and high patient satisfaction as indicated in a recent case series.74 This should be differentiated from the need to undergo an arthroplasty procedure due to failed primary open reduction and internal fixation (ORIF).
Level 1
Cai et al. reoperated on three of 12 patients following locking plate. The patients originally had four-part fractures and reoperations were during the 2nd year of followup. Plates were removed for fixation failure and revision internal fixation for nonunion.20 Zhu et al. performed five screw revisions due to primary screw penetration.70 Voigt et al. attributed the majority of reoperations in their study due to secondary displacement of the greater tuberosity.65
Level 2
Buecking et al. reported a large number of reoperations: three screw revisions, 18 plate removals, four revision ORIF, and seven arthroplasties in their study population of 90.19 Seventeen of the plate removals were at the request of the patient and the rest were due to screw perforation, implant loosening, or infection. Schliemann et al. performed seven plate removals with arthrolysis in two of those cases.58
Level 3
Kralinger et al. reported mechanical failure as a strong predictor of reoperation in their study consisting of majority three- and four-part fractures. Two revision arthroplasties, six capsular releases, six revisions of internal fixation, 14 plate removals, and one hematoma evacuation were performed.35 Sanders et al. discussed screw revisions and plate removals secondary to intraarticular screw penetration and impingement, respectively, as a major reason for their 50% reoperation rate.56
Level 4
Ockert et al. noted an unplanned reoperation rate of 14% and a planned reoperation rate (due to impingement, patient request, or range of motion deficit) of 40% in its series of 43 patients followed for 10 years.46 Kim et al. reported 2 implant removals for cultural reasons in their case series of 21 four-part fractures followed for 27.5 months.32 Finally, Schliemann et al. reported impingement and screw penetration as the primary reason their revision rate was close to 30%.57
The data presented in this systematic review not only support data from past reviews but also present potential solutions proposed by investigators, in the hopes of decreasing the complication rate associated with locking plate of proximal humerus fractures. Recent reviews have emphasized the importance of AVN and fracture dislocation patterns negatively impacting outcome. Complex, intraarticular fracture patterns have high complication rates when treated with locking plate. Brorson et al. also noted that the methodological quality of studies is lacking.75 Tepass et al. noted that three- and four-part fractures actually had better outcomes when treated with head preserving surgery compared to a hemiarthroplasty and that there were an increase in the number of complications as the fracture complexity increased.76 Finally, in a review specifically looking at referrals for complications, Jost et al. discussed the importance of making the primary surgery the definitive surgery. A majority of the patients received arthroplasty as a revision surgery, secondary to complications from locking plate. In these patients, primary reduction was not achieved, indicating that the more complex fracture patterns may not necessarily be amenable to locking plate.77
None of the articles presented in this review were in the most recent comprehensive systematic review, as Sproul et al. completed their literature search in 2009. In addition, none of the articles from the previous systematic reviews are in this review as we only included the most recent articles. We repeated our queries to capture the most recent literature and data, noting that there were quite a few articles we would not have been able to include. More experience with locking plate in treating proximal humerus fractures and the application of newer techniques has definitely adjusted complication rates. Moreover, the complication rates may not have been entirely accurate in the previous reviews as they were analyzing a smaller number of total cases. Thus, one of the aims of this review was to encompass as many recent articles without sacrificing quality, which we accomplished by including only high scoring articles into this study.
It is also worthwhile to discuss the fact that there is a large amount of literature describing nonoperative treatment of proximal humerus fractures. Concerning the number of complications as well as costs associated with surgical treatment, there have also been studies comparing operative versus nonoperative treatment of these fractures. Handoll et al. found in their Proximal Fracture of the Humerus: Evaluation by Randomization trial that surgical treatment does not result in improved outcomes in most patients and that it is not cost effective.78 This lends support to the argument that every fracture should be treated on a case-by-case basis. The osteoporotic nature of some of these fractures leaves it incredibly difficult to treat, and though locking plate has been promising in theory, not every plate is the same and cannot replicate force distributions of the proximal humerus. The most used plate seemed to be the Synthes PHILOS plate; however, not every article in our review reported which plate they used. The design of the plate cannot prevent varus collapse and subsequent cutout of the screws. Biomechanical studies have shown this and the importance of a medial buttress to prevent those complications.79
There are a number of limitations to this review. First, minimum followup was set to 12 months, which may have underestimated the incidence and prevalence of AVN. Not every article commented on every complication analyzed in this report. This could have led to either under-reporting or over reporting of results. Next, the heterogeneity of the articles, whether it was based on level of evidence, type of fracture, approach, or specific technique used, could not be fully accounted for. In addition, we did not perform a metaanalysis of the complication rate. Our aim was to provide a broad overview of complications with proposed methods to decrease complication rate. A meta-analysis was not our goal as we cannot equally compare each study, such as comparing a three part fracture with a four-part fracture. An attempt was made to highlight the most important conclusions from each article. Finally, giving more weight to articles with higher levels of evidence may have skewed the results as well.
Conclusion
The points of consideration from this review, in regard to the major complications associated with locking plate in proximal humerus fractures, are as follows:
Screw penetration
Greater care with fluoroscopy, use of at least two perpendicular planes to confirm screw is not within the glenohumeral joint. Placement of screws that are too short of subchondral bone should be avoided.
Varus collapse
Ensure the medial column is intact (medial hinge). Consideration of the use of strut allograft, bone graft, suture augmentation, and plate contouring. Consider placement of inferomedial support screws.
Subacromial impingement
Ensure the plate does not sit too proximally, AVN, Consider fracture type to stratify risk of AVN, Careful soft-tissue dissection, Consider minimally invasive techniques.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–7. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma. 2015;29:e242–4. doi: 10.1097/BOT.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 3.Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, et al. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98:715–9. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Launonen AP, Lepola V, Saranko A, Flinkkilä T, Laitinen M, Mattila VM, et al. Epidemiology of proximal humerus fractures. Arch Osteoporos. 2015;10:209. doi: 10.1007/s11657-015-0209-4. [DOI] [PubMed] [Google Scholar]
- 5.Handoll HH, Ollivere BJ, Rollins KE. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2012;12:CD000434. doi: 10.1002/14651858.CD000434.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488–93. doi: 10.1097/00005131-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Frich LH, Jensen NC. Bone properties of the humeral head and resistance to screw cutout. Int J Shoulder Surg. 2014;8:21–6. doi: 10.4103/0973-6042.131851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: A systematic review. J Shoulder Elbow Surg. 2009;18:837–44. doi: 10.1016/j.jse.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42:408–13. doi: 10.1016/j.injury.2010.11.058. [DOI] [PubMed] [Google Scholar]
- 10.Jobin CM, Galdi B, Anakwenze OA, Ahmad CS, Levine WN. Reverse shoulder arthroplasty for the management of proximal humerus fractures. J Am Acad Orthop Surg. 2015;23:190–201. doi: 10.5435/JAAOS-D-13-00190. [DOI] [PubMed] [Google Scholar]
- 11.Badman BL, Mighell M. Fixed-angle locked plating of two-, three-, and four-part proximal humerus fractures. J Am Acad Orthop Surg. 2008;16:294–302. doi: 10.5435/00124635-200805000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Harris JD, Quatman CE, Manring MM, Siston RA, Flanigan DC. How to write a systematic review. Am J Sports Med. 2014;42:2761–8. doi: 10.1177/0363546513497567. [DOI] [PubMed] [Google Scholar]
- 13.Papadokostakis G, Papakostidis C, Dimitriou R, Giannoudis PV. The role and efficacy of retrograding nailing for the treatment of diaphyseal and distal femoral fractures: A systematic review of the literature. Injury. 2005;36:813–22. doi: 10.1016/j.injury.2004.11.029. [DOI] [PubMed] [Google Scholar]
- 14.Aggarwal S, Bali K, Dhillon MS, Kumar V, Mootha AK. Displaced proximal humeral fractures: An Indian experience with locking plates. J Orthop Surg Res. 2010;5:60. doi: 10.1186/1749-799X-5-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bachelier F, Pizanis A, Schwitalla J, Pohlemann T, Kohn D, Wirbel R, et al. Treatment for displaced proximal humerus fractures: Comparison of interlocking plate fixation versus minimal invasive techniques. Eur J Orthop Surg Traumatol. 2014;24:707–14. doi: 10.1007/s00590-013-1235-9. [DOI] [PubMed] [Google Scholar]
- 16.Badman B, Frankle M, Keating C, Henderson L, Brooks J, Mighell M, et al. Results of proximal humeral locked plating with supplemental suture fixation of rotator cuff. J Shoulder Elbow Surg. 2011;20:616–24. doi: 10.1016/j.jse.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 17.Barco R, Barrientos I, Encinas C, Antuña SA. Minimally invasive poly-axial screw plating for three-part fractures of the proximal humerus. Injury. 2012;43(Suppl 2):S7–11. doi: 10.1016/S0020-1383(13)70173-6. [DOI] [PubMed] [Google Scholar]
- 18.Barlow JD, Sanchez-Sotelo J, Torchia M. Proximal humerus fractures in the elderly can be reliably fixed with a “hybrid” locked-plating technique. Clin Orthop Relat Res. 2011;469:3281–91. doi: 10.1007/s11999-011-1894-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures? Clin Orthop Relat Res. 2014;472:1576–85. doi: 10.1007/s11999-013-3415-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cai M, Tao K, Yang C, Li S. Internal fixation versus shoulder hemiarthroplasty for displaced 4-part proximal humeral fractures in elderly patients. Orthopedics. 2012;35:e1340–6. doi: 10.3928/01477447-20120822-19. [DOI] [PubMed] [Google Scholar]
- 21.Chen Y, Zhang K, Qiang M, Li H, Dai H. Computer-assisted preoperative planning for proximal humeral fractures by minimally invasive plate osteosynthesis. Chin Med J (Engl) 2014;127:3278–85. [PubMed] [Google Scholar]
- 22.Chowdary U, Prasad H, Subramanyam PK. Outcome of locking compression plating for proximal humeral fractures: A prospective study. J Orthop Surg (Hong Kong) 2014;22:4–8. doi: 10.1177/230949901402200104. [DOI] [PubMed] [Google Scholar]
- 23.Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg. 2010;19:489–94. doi: 10.1016/j.jse.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 24.de Kruijf M, Vroemen JP, de Leur K, van der Voort EA, Vos DI, Van der Laan L, et al. Proximal fractures of the humerus in patients older than 75 years of age: Should we consider operative treatment? J Orthop Traumatol. 2014;15:111–5. doi: 10.1007/s10195-013-0273-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duralde XA, Leddy LR. The results of ORIF of displaced unstable proximal humeral fractures using a locking plate. J Shoulder Elbow Surg. 2010;19:480–8. doi: 10.1016/j.jse.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 26.Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD, et al. Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2012;21:741–8. doi: 10.1016/j.jse.2011.09.017. [DOI] [PubMed] [Google Scholar]
- 27.Fjalestad T, Hole MØ, Hovden IA, Blücher J, Strømsøe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: A randomized controlled trial. J Orthop Trauma. 2012;26:98–106. doi: 10.1097/BOT.0b013e31821c2e15. [DOI] [PubMed] [Google Scholar]
- 28.Gaheer RS, Hawkins A. Fixation of 3- and 4-part proximal humerus fractures using the PHILOS plate: Mid-term results. Orthopedics. 2010;33:671. doi: 10.3928/01477447-20100722-11. [DOI] [PubMed] [Google Scholar]
- 29.Gavaskar AS, Chowdary N, Abraham S. Complex proximal humerus fractures treated with locked plating utilizing an extended deltoid split approach with a shoulder strap incision. J Orthop Trauma. 2013;27:73–6. doi: 10.1097/BOT.0b013e31825cf545. [DOI] [PubMed] [Google Scholar]
- 30.Hirschmann MT, Fallegger B, Amsler F, Regazzoni P, Gross T. Clinical longer-term results after internal fixation of proximal humerus fractures with a locking compression plate (PHILOS) J Orthop Trauma. 2011;25:286–93. doi: 10.1097/BOT.0b013e3181f2b20e. [DOI] [PubMed] [Google Scholar]
- 31.Jung WB, Moon ES, Kim SK, Kovacevic D, Kim MS. Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate? BMC Musculoskelet Disord. 2013;14:102. doi: 10.1186/1471-2474-14-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim SH, Lee YH, Chung SW, Shin SH, Jang WY, Gong HS, et al. Outcomes for four-part proximal humerus fractures treated with a locking compression plate and an autologous iliac bone impaction graft. Injury. 2012;43:1724–31. doi: 10.1016/j.injury.2012.06.029. [DOI] [PubMed] [Google Scholar]
- 33.Königshausen M, Kübler L, Godry H, Citak M, Schildhauer TA, Seybold D, et al. Clinical outcome and complications using a polyaxial locking plate in the treatment of displaced proximal humerus fractures. A reliable system? Injury. 2012;43:223–31. doi: 10.1016/j.injury.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 34.Konrad G, Hirschmüller A, Audige L, Lambert S, Hertel R, Südkamp NP, et al. Comparison of two different locking plates for two-, three- and four-part proximal humeral fractures – Results of an international multicentre study. Int Orthop. 2012;36:1051–8. doi: 10.1007/s00264-011-1410-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kralinger F, Blauth M, Goldhahn J, Käch K, Voigt C, Platz A, et al. The influence of local bone density on the outcome of one hundred and fifty proximal humeral fractures treated with a locking plate. J Bone Joint Surg Am. 2014;96:1026–32. doi: 10.2106/JBJS.M.00028. [DOI] [PubMed] [Google Scholar]
- 36.Kumar C, Gupta AK, Nath R, Ahmad J. Open reduction and locking plate fixation of displaced proximal humerus fractures. Indian J Orthop. 2013;47:156–60. doi: 10.4103/0019-5413.108903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin T, Xiao B, Ma X, Fu D, Yang S. Minimally invasive plate osteosynthesis with a locking compression plate is superior to open reduction and internal fixation in the management of the proximal humerus fractures. BMC Musculoskelet Disord. 2014;15:206. doi: 10.1186/1471-2474-15-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Little MT, Berkes MB, Schottel PC, Lazaro LE, LaMont LE, Pardee NC, et al. The impact of preoperative coronal plane deformity on proximal humerus fixation with endosteal augmentation. J Orthop Trauma. 2014;28:338–47. doi: 10.1097/BOT.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 39.Liu K, Liu PC, Liu R, Wu X. Advantage of minimally invasive lateral approach relative to conventional deltopectoral approach for treatment of proximal humerus fractures. Med Sci Monit. 2015;21:496–504. doi: 10.12659/MSM.893323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu ZZ, Zhang GM, Ge T. Use of a proximal humeral internal locking system enhanced by injectable graft for minimally invasive treatment of osteoporotic proximal humeral fractures in elderly patients. Orthop Surg. 2011;3:253–8. doi: 10.1111/j.1757-7861.2011.00150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martetschläger F, Siebenlist S, Weier M, Sandmann G, Ahrens P, Braun K, et al. Plating of proximal humeral fractures. Orthopedics. 2012;35:e1606–12. doi: 10.3928/01477447-20121023-17. [DOI] [PubMed] [Google Scholar]
- 42.Matassi F, Angeloni R, Carulli C, Civinini R, Di Bella L, Redl B, et al. Locking plate and fibular allograft augmentation in unstable fractures of proximal humerus. Injury. 2012;43:1939–42. doi: 10.1016/j.injury.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 43.Matejcić A, Vidović D, Ivica M, Durdević D, Tomljenović M, Bekavac-Beslin M, et al. Internal fixation with locking plate of 3- and 4-part proximal humeral fractures in elderly patients: Complications and functional outcome. Acta Clin Croat. 2013;52:17–22. [PubMed] [Google Scholar]
- 44.Miyazaki AN, Estelles JR, Fregoneze M, Santos PD, da Silva LA, do Val Sella G, et al. Evaluation of the complications of surgical treatment of fractures of the proximal extremity of the humerus using a locking plate. Rev Bras Ortop. 2012;47:568–74. doi: 10.1016/S2255-4971(15)30005-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Norouzi M, Naderi MN, Komasi MH, Sharifzadeh SR, Shahrezaei M, Eajazi A, et al. Clinical results of using the proximal humeral internal locking system plate for internal fixation of displaced proximal humeral fractures. Am J Orthop (Belle Mead NJ) 2012;41:E64–8. [PubMed] [Google Scholar]
- 46.Ockert B, Siebenbürger G, Kettler M, Braunstein V, Mutschler W. Long term functional outcomes (median 10 years) after locked plating for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2014;23:1223–31. doi: 10.1016/j.jse.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 47.Olerud P, Ahrengart L, Soderqvist A, Saving J, Tidermark J. Quality of life and functional outcome after a 2-part proximal humeral fracture: A prospective cohort study on 50 patients treated with a locking plate. J Shoulder Elbow Surg. 2010;19:814–22. doi: 10.1016/j.jse.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 48.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: A randomized controlled trial. J Shoulder Elbow Surg. 2011;20:747–55. doi: 10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 49.Osterhoff G, Hoch A, Wanner GA, Simmen HP, Werner CM. Calcar comminution as prognostic factor of clinical outcome after locking plate fixation of proximal humeral fractures. Injury. 2012;43:1651–6. doi: 10.1016/j.injury.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 50.Pak P, Eng K, Page RS. Fixed-angle locking proximal humerus plate: An evaluation of functional results and implant-related outcomes. ANZ J Surg. 2013;83:878–82. doi: 10.1111/ans.12370. [DOI] [PubMed] [Google Scholar]
- 51.Parmaksizoǧlu AS, Sökücü S, Ozkaya U, Kabukçuoǧlu Y, Gül M. Locking plate fixation of three- and four-part proximal humeral fractures. Acta Orthop Traumatol Turc. 2010;44:97–104. doi: 10.3944/AOTT.2010.2275. [DOI] [PubMed] [Google Scholar]
- 52.Ricchetti ET, Warrender WJ, Abboud JA. Use of locking plates in the treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2010;19:66–75. doi: 10.1016/j.jse.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 53.Robinson CM, Wylie JR, Ray AG, Dempster NJ, Olabi B, Seah KT, et al. Proximal humeral fractures with a severe varus deformity treated by fixation with a locking plate. J Bone Joint Surg Br. 2010;92:672–8. doi: 10.1302/0301-620X.92B5.22849. [DOI] [PubMed] [Google Scholar]
- 54.Röderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2010;24:400–6. doi: 10.1097/BOT.0b013e3181ccafb3. [DOI] [PubMed] [Google Scholar]
- 55.Sahu RJ. Minimally invasive percutaneous plate osteosynthesis for the treatment of proximal humerus fractures in osteoporotic patients with Philos plate. Bangladesh J Med Sci. 2013;12:140–5. [Google Scholar]
- 56.Sanders RJ, Thissen LG, Teepen JC, van Kampen A, Jaarsma RL. Locking plate versus nonsurgical treatment for proximal humeral fractures: Better midterm outcome with nonsurgical treatment. J Shoulder Elbow Surg. 2011;20:1118–24. doi: 10.1016/j.jse.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 57.Schliemann B, Siemoneit J, Theisen C, Kosters C, Weimann A, Raschke MJ. Complex fractures of the proximal humerus in the elderly-outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96:s3–11. doi: 10.1007/s12306-012-0181-8. [DOI] [PubMed] [Google Scholar]
- 58.Schliemann B, Hartensuer R, Koch T, Theisen C, Raschke MJ, Kösters C, et al. Treatment of proximal humerus fractures with a CFR-PEEK plate: 2-year results of a prospective study and comparison to fixation with a conventional locking plate. J Shoulder Elbow Surg. 2015;24:1282–8. doi: 10.1016/j.jse.2014.12.028. [DOI] [PubMed] [Google Scholar]
- 59.Schulte LM, Matteini LE, Neviaser RJ. Proximal periarticular locking plates in proximal humeral fractures: Functional outcomes. J Shoulder Elbow Surg. 2011;20:1234–40. doi: 10.1016/j.jse.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 60.Sharma V, Balvinder S, Khare S. Management of proximal humeral fractures with proximal humerus locking plate – A prospective study. J Orthop Trauma Rehabil. 2014;18:89–93. [Google Scholar]
- 61.Sohn HS, Shin SJ. Minimally invasive plate osteosynthesis for proximal humeral fractures: Clinical and radiologic outcomes according to fracture type. J Shoulder Elbow Surg. 2014;23:1334–40. doi: 10.1016/j.jse.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 62.Spross C, Platz A, Rufibach K, Lattmann T, Forberger J, Dietrich M, et al. The PHILOS plate for proximal humeral fractures – Risk factors for complications at one year. J Trauma Acute Care Surg. 2012;72:783–92. doi: 10.1097/TA.0b013e31822c1b5b. [DOI] [PubMed] [Google Scholar]
- 63.Trepat AD, Popescu D, Fernandez-Valencia JA, Cune J, Rios M, Prat S. Comparative study between locking plates versus proximal humeral nail for the treatment of 2-part proximal humeral fractures. Eur J Orthop Surg Traumatol. 2012;22:373–9. [Google Scholar]
- 64.Verdano MA, Lunini E, Pellegrini A, Corsini T, Marenghi P, Ceccarelli F, et al. Can the osteosynthesis with locking plates be a better treatment for unstable fractures of the proximal humerus? Musculoskelet Surg. 2014;98:27–33. doi: 10.1007/s12306-013-0267-y. [DOI] [PubMed] [Google Scholar]
- 65.Voigt C, Geisler A, Hepp P, Schulz AP, Lill H. Are polyaxially locked screws advantageous in the plate osteosynthesis of proximal humeral fractures in the elderly? A prospective randomized clinical observational study. J Orthop Trauma. 2011;25:596–602. doi: 10.1097/BOT.0b013e318206eb46. [DOI] [PubMed] [Google Scholar]
- 66.Wild JR, DeMers A, French R, Shipps MR, Bergin PF, Musapatika D, et al. Functional outcomes for surgically treated 3- and 4-part proximal humerus fractures. Orthopedics. 2011;34:e629–33. doi: 10.3928/01477447-20110826-14. [DOI] [PubMed] [Google Scholar]
- 67.Wu CH, Ma CH, Yeh JJ, Yen CY, Yu SW, Tu YK, et al. Locked plating for proximal humeral fractures: Differences between the deltopectoral and deltoid-splitting approaches. J Trauma. 2011;71:1364–70. doi: 10.1097/TA.0b013e31820d165d. [DOI] [PubMed] [Google Scholar]
- 68.Yang H, Li Z, Zhou F, Wang D, Zhong B. A prospective clinical study of proximal humerus fractures treated with a locking proximal humerus plate. J Orthop Trauma. 2011;25:11–7. doi: 10.1097/BOT.0b013e3181d2d04c. [DOI] [PubMed] [Google Scholar]
- 69.Zhang L, Zheng J, Wang W, Lin G, Huang Y, Zheng J, et al. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: A prospective randomized study. Int Orthop. 2011;35:1655–61. doi: 10.1007/s00264-011-1227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhu Y, Lu Y, Shen J, Zhang J, Jiang C. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: A prospective randomized trial with a minimum of three years of followup. J Bone Joint Surg Am. 2011;93:159–68. doi: 10.2106/JBJS.J.00155. [DOI] [PubMed] [Google Scholar]
- 71.Ricchetti ET, DeMola PM, Roman D, Abboud JA. The use of precontoured humeral locking plates in the management of displaced proximal humerus fracture. J Am Acad Orthop Surg. 2009;17:582–90. doi: 10.5435/00124635-200909000-00005. [DOI] [PubMed] [Google Scholar]
- 72.Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427–33. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 73.Wang J, Zhu Y, Zhang F, Chen W, Tian Y, Zhang Y, et al. Meta-analysis suggests that reverse shoulder arthroplasty in proximal humerus fractures is a better option than hemiarthroplasty in the elderly. Int Orthop. 2016;40:531–9. doi: 10.1007/s00264-015-2811-x. [DOI] [PubMed] [Google Scholar]
- 74.Kirchhoff C, Braunstein V, Kirchhoff S, Sprecher CM, Ockert B, Fischer F, et al. Outcome analysis following removal of locking plate fixation of the proximal humerus. BMC Musculoskelet Disord. 2008;9:138. doi: 10.1186/1471-2474-9-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brorson S, Rasmussen JV, Frich LH, Olsen BS, Hróbjartsson A. Benefits and harms of locking plate osteosynthesis in intraarticular (OTA type C) fractures of the proximal humerus: A systematic review. Injury. 2012;43:999–1005. doi: 10.1016/j.injury.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 76.Tepass A, Rolauffs B, Weise K, Bahrs SD, Dietz K, Bahrs C, et al. Complication rates and outcomes stratified by treatment modalities in proximal humeral fractures: A systematic literature review from 1970-2009. Patient Saf Surg. 2013;7:34. doi: 10.1186/1754-9493-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: Analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22:542–9. doi: 10.1016/j.jse.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 78.Handoll H, Brealey S, Rangan A, Keding A, Corbacho B, Jefferson L, et al. The proFHER (PROximal fracture of the humerus: Evaluation by randomisation) trial – A pragmatic multicentre randomised controlled trial evaluating the clinical effectiveness and cost-effectiveness of surgical compared with non-surgical treatment for proximal fracture of the humerus in adults. Health Technol Assess. 2015;19:1–280. doi: 10.3310/hta19240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bae JH, Oh JK, Chon CS, Oh CW, Hwang JH, Yoon YC, et al. The biomechanical performance of locking plate fixation with intramedullary fibular strut graft augmentation in the treatment of unstable fractures of the proximal humerus. J Bone Joint Surg Br. 2011;93:937–41. doi: 10.1302/0301-620X.93B7.26125. [DOI] [PubMed] [Google Scholar]


