Abstract
Background:
The options to perform total knee arthroplasty (TKA) with retained hardware in femur are mainly – removal of hardware, use of extramedullary guide, or computer-assisted surgery. Patient-specific blocks (PSBs) have been introduced with many potential advantages, but their use in retained hardware has not been adequately explored. The purpose of the present study was to outline and assess the usefulness of the PSBs in performing TKA in patients with retained femoral hardware. Materials and
Materials and Methods:
Nine patients with retained femoral hardware underwent TKA using PSBs. All the surgeries were performed by the same surgeon using same implants. Nine cases (7 males and 2 females) out of total of 120 primary TKA had retained hardware. The average age of the patients was 60.55 years. The retained hardware were 6 patients with nails, 2 with plates and one patient had screws. Out of the nine cases, only one patient needed removal of a screw which was hindering placement of pin for the PSB.
Results:
All the patients had significant improvement in their Knee Society Score (KSS) which improved from 47.0 to postoperative KSS of 86.77 (P < 0.00). The mechanical axis was significantly improved (P < 0.03) after surgery. No patient required blood transfusion and the average tourniquet time was 41 min.
Conclusion:
TKA using PSBs is useful and can be used in patients with retained hardware with good functional and radiological outcome.
Keywords: Arthroplasty, knee, patient-specific blocks, prostheses and implants, replacement
MeSH terms: Arthroplasty, knee, replacement, knee prosthesis, implants
Introduction
Total knee arthroplasty (TKA) has been accepted worldwide for functional improvement in patients suffering from osteoarthritis. The recent focus has been for achieving implant longevity and it has been believed that achieving good alignment is crucial for long term implant survival and patient satisfaction. Intra-medullary (IM) guides are routinely used as intraoperative guides for achieving correct alignment. In this quest of achieving accurate alignment, first, computer-assisted surgery (CAS) was introduced to help in achieving accurate alignment using the femoral head center, knee, and ankle as a guide.1 Subsequently, the patient-specific blocks (PSBs) were introduced, which have been reported to cause less soft tissue damage, less postoperative pain and rapid functional recovery compared to conventional TKA.2 Alignment of the knee can be restored by using PSB and CAS without using the IM rod.3,4 All these advantages of PSB have been under scrutiny, with a number of publications either in favor or against.3,5,6,7,8,9 Out of the potential advantages, one unequivocal use with the PSBs could be their use in TKAs with retained hardware.
The problems in patients with retained hardware are multi-factorial. The femoral medullary canal is obstructed by retained implants; there may be canal sclerosis and obliteration from callus along with extraarticular deformity from the previous fracture.10 Due to these reasons, IM rods cannot be used in these cases.11,12 Hardware removal is usually advised either before TKA or at the same sitting, but this increases the risk of intraoperative fracture and other complications resulting in a poorer outcome.13 An extra-medullary (EM) guide or free-hand cutting can be tried in these cases, but results are usually inferior compared to conventional IM guide.14
The use of CAS with retained hardware has been studied and published, but the use of PSB has not been discussed in detail. Thienpont et al. discussed the use of PSB in extraarticular deformity in ten patients but had only a single case with retained hardware in their series.10 We report a retrospective study of nine cases of computerized tomogram (CT) based PSB-TKA in patients with knee arthritis and retained hardware in the ipsilateral femur, where a single type of PSB (PrePlan™, Stryker™) was used in all the cases. Our hypothesis was that PSB helps in attaining mechanical limb alignment in patients with retained hardware.
Materials and Methods
120 primary TKA using CT-based PSB were operated between April 2012 and January 2014, out of which nine knees had retained ipsilateral femoral hardware. All these nine cases had advanced osteoarthrosis (OA) of the knees (Ahlback's Grade IV). These patients gave informed consent for their TKA using PSB. A preoperative CT scan of the lower limb (hip-knee-ankle (HKA) was done in all patients. There was no interference with the imaging due to the hardware in the present study.
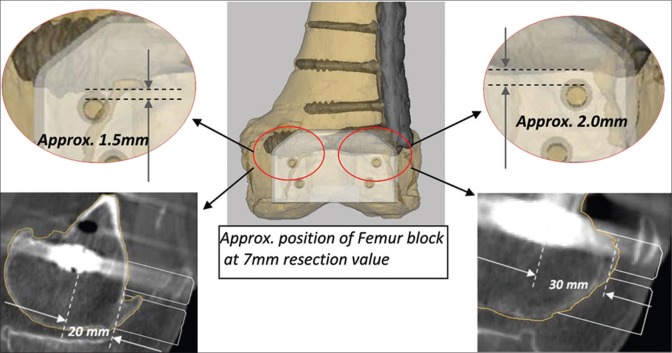
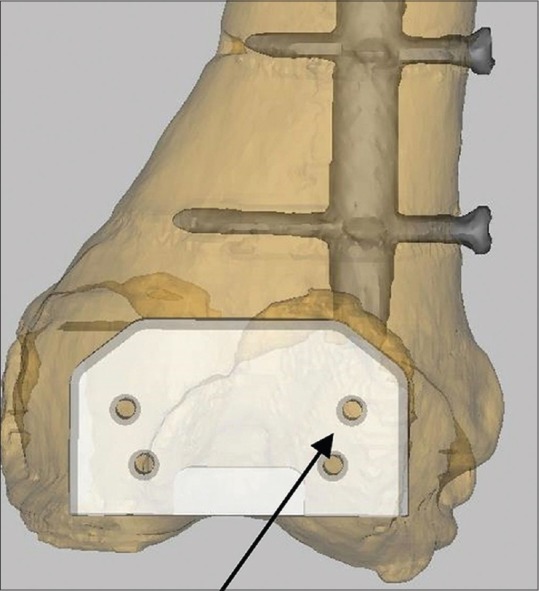
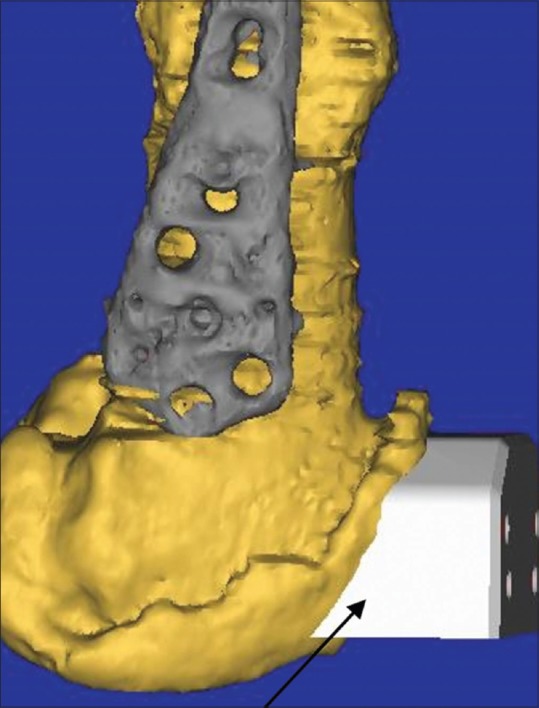
After segmenting the obtained data, three-dimensional models of femoral as well as tibial components were created to determine their optimal size, position, and alignment. An image of the patient's knee with the proposed bony resections completed could be viewed preoperatively online by the surgeon [Figure 1]. The position of the pins to be used to secure the PSB was preoperatively visualized virtually, and hence, any interference from the previous hardware was also checked [Figure 2].
Figure 1.
A three-dimensional computer reconstructed image of distal femur with retained inter-locking nail. A patient-specific block has been superimposed on the femur. Arrow depicts site of pin insertion for femur patient-specific block
Figure 2.
A patient-specific block super imposing on femur with retained dynamic condylar screw. The images in upper inset depict the distance of the lag screw from the site for pin insertion of patient-specific block and any possible interference. Lower inset images depict 20 mm and 30 mm thickness from anterior cortex of the femur on medial and lateral side respectively
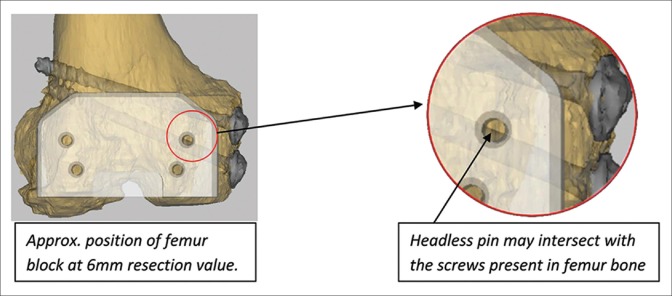
After approval by the surgeon, rapid prototyping technology was used to fabricate disposable, custom cutting guides (PrePlan™, Stryker™). All the surgeries were performed using posterior stabilized implants (Scorpio, Stryker™). Anterior midline approach (modified Insall's approach) was used for exposure of all the knees.15 After exposing the distal femur and proximal tibia, PSB were used for proximal tibial and distal femoral cuts without requiring the opening of the medullary canal [Figure 3]. During the surgery, these PSB fitted well on the patient's native anatomy and could be used to determine accurate pin positioning for the use of standard resection instruments. The cuts were re-checked using EM guides in all the cases, and the surgeon proceeded with the cuts given by PSB in all the cases. In one case which had two retained screws, one screw, which was preoperatively found to be hindering the insertion of the pin for the PSB, needed removal [Figure 4]. Conventional cutting blocks were used after the proximal tibial and distal femoral cuts. Remaining steps of the surgery were completed as in a conventional TKA.
Figure 3.
A three-dimensional computer reconstructed lateral view of distal femur with distal femoral locking plate in situ. Arrow depicts block sitting well on anterior femur with no interference with the screws and plate
Figure 4.
One retained screw in this femur seems to be overlapping with the hole for patient-specific block pin (inset, arrow) and needed removal during surgery
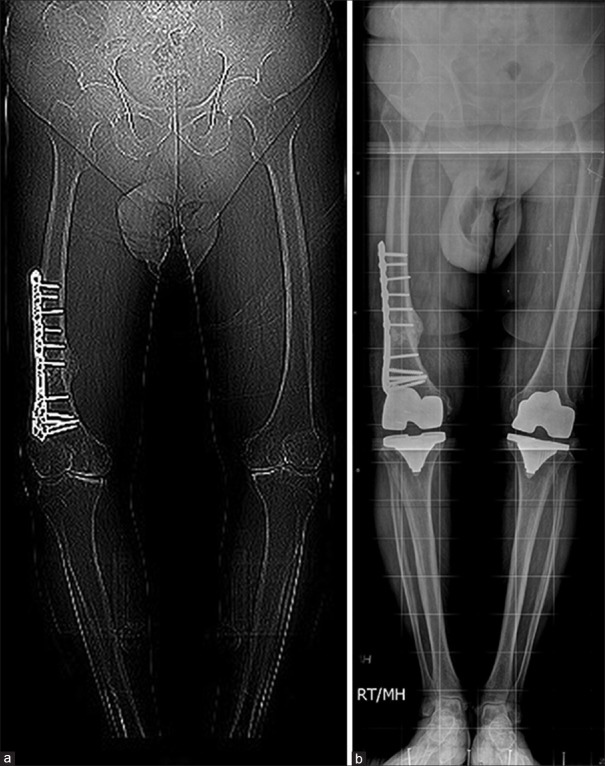
Postoperative care and physical therapy were performed as per the standard protocol of TKA of our institution. All the patients were made to walk on the 2nd postoperative day with the help of walking frame. After each patient was discharged from the hospital, postoperative followup was done at 2, 6, and 12 weeks. The preoperative CT scanograms were compared with the postoperative full-length radiographs for this retrospective study [Figure 5a and b]. Other pre- and postoperative clinical were also reviewed retrospectively for this study.
Figure 5.
(a) Preoperative hip-knee-ankle computerized tomogram of a patient with retained plate showing the united fracture and bilateral varus deformity of the knees. (b) Postoperative hip-knee-ankle radiograph of the same patient showing restoration of the mechanical axis
Statistical analysis
The preoperative and postoperative data such as Knee Society Score (KSS), HKA mechanical axis (MA) were checked for statistical significance using Student's t-test and the values were considered statistically significant for the value of P < 0.05. All the analyses were performed using SPSS version 16 software (SPSS Inc., Chicago, IL, USA).
Results
A total of nine patients (seven men and two women) with an average age of 60.55 years (range 51–71 years) were studied in this series. All patients had suffered an extra-articular ipsilateral femoral fracture in the past and underwent open/closed reduction and internal fixation either by nail or plate and had retained hardware. Six patients had IM nails, and two had plates and one had screws in femur. The patients had all underwent single surgery for the fixation of femoral fracture prior to the planned TKA. The average distance from the distal side of the implant to the intercondylar notch was 5.43 cm. The average tourniquet time was 41 min (range 34–47 min). None of the patients needed blood transfusion, even though they were complex primary TKAs. None of the patients needed the use of special implants like wedges or stems in the present series. On clinical examination, improvement in the range of motion was noted postoperatively. The KSS, including the knee-specific score and function score, also significantly improved after surgery [Table 1].
Table 1.
Results of total knee arthroplasty with retained hardware, using patient-specific blocks
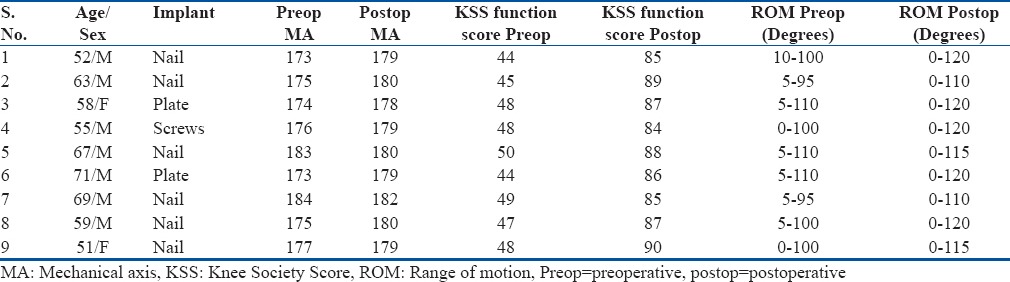
As compared to preoperative mean KSS of 47.0, the postoperative KSS improved to 86.77 (P < 0.00). Neither postoperative infections nor any complications occurred after surgery using PSB. The comparison between the pre- and post-operative radiographs was done; the results are shown in Table 1. There was good restoration of the MA in all the cases when the pre- and the post-operative radiographs were compared, with a mean HKA of 179.55 (range 178–182). The difference of preoperative versus postoperative MA on HKA was also found to be statistically significant (P < 0.03). The average followup of these patients was 12.5 months (range 6–22 months).
Discussion
The patient-specific instruments (blocks) are being used in TKA to improve the surgical accuracy and minimize the surgical error. There are various other potential advantages of the PSB like decreased surgical time, decreased blood loss, increased OR efficiency, theoretically decreased risk of fat embolism and improved function results.3,5,6,7 Various studies have shown that when compared to conventional TKA, PSB could provide more accurate restoration of MA, better coronal and sagittal plane implant position, less bleeding, and less intraoperative time.3,5,6,16 Moreover, fat embolism has been reported in TKA due to increased pulmonary pressures due to canal invasion.7
TKA after femoral fracture with retained hardware using IM alignment system would require implant removal. The implant removal done before TKA has the disadvantages of increased duration of surgery, increased blood loss, increased risk of infection and intraoperative fracture due to stress risers from implant removal.17 Some surgeons have even reported using prophylactic IM nail after distal femoral plate removal and before TKA to bypass the stress risers.17 Apart from the issue of implant removal, there are issues of canal obliteration and extraarticular deformity in these cases. The two stage procedure which involves removal of hardware in the first stage and TKA in the second stage has certain disadvantages. The surgery for implant removal involves increased exposure to anesthesia, blood loss, and delayed final surgery of TKA. Moreover, there is always a chance of an indolent low-grade infection getting activated after the implant removal, which may otherwise remain hidden underneath the implant previously. An old implant may also pose difficulty in removal and increase tissue and bone damage which may further delay the future joint replacement surgery. Hardware removal may also be associated with the development of stress risers in the bone, which may lead to a potential peri-prosthetic fracture. The presence of a stress riser may also necessitate the use of complex implants which may be associated with delayed recovery and longer rehabilitation protocol.1
The possible definite indication of using PSB is in performing TKA with retained hardware.10 Another option for TKA with retained hardware could be with CAS.18 Tigani et al. reported good results using CAS for conventional TKA in patients of extraarticular deformity (n = 9) and retained hardware (n = 5).19 The studies which have been carried out using CAS in retained hardware have mentioned the advantages of this procedure.18,19,20 As compared to the previously published studies, the results of this study are comparable with satisfactory outcomes. However, CAS-TKA may be associated with delayed functional recovery, if additional quadriceps dissection has been done for putting the femoral reference pin.21 Furthermore, use of CAS is associated with longer surgical time, it is technically more demanding, involves a long learning curve and universal nonavailability, due to costly instrumentation of CAS.8
PSBs, on the other hand, have been consistently shown to achieve postoperative mechanical alignment. The other advantages cited are decreased operative time, decreased blood loss, and increased OR efficiency among others.16 Although these advantages are under debate, the use of PSB in extraarticular deformity is universally accepted with their use in retained hardware been reported rarely.10 The potential advantages of using PSB is the avoidance of implant removal, the ability to see the fitting of blocks preoperatively and also to see the flexion and extension gaps preoperatively and hence planning the surgery before the incision is made.
PSB are made after calculation of the MA (using the femoral head, knee and ankle centers) from preoperative imaging modality, and it helps the surgeon in restoring MA and implanting the prosthesis accurately without relying on IM rod or distorted anatomical landmarks. PSB can be manufactured on the basis of the patient's anatomy, and this depends on image acquisition which can be done preoperatively using magnetic resonance imaging (MRI) or CT. There are proponents of the use of both imaging modalities where the most common cited advantage of MRI-based PSB is decreased radiation hazard. We believe, that CT-based PSB have several advantages over MRI-based PSB as CT scanning is quick, easily available and gives better anatomical details of the bones, whereas MRI is associated with increased scan time, claustrophobia, more expense and most importantly inability to use it with retained implants, in situ pacemakers, and with contralateral existing TKA. Furthermore, the reduced cost of CT versus MRI makes it more favorable to use in manufacturing the PSB. In this study also, there was no interference in image capture using CT scans for PSB manufacturing. In fact, it is one of the advantages of using CT-based PSB as compared to the MRI-based PSBs. There may be varied levels of interference in image capture in MRI due to the metallic hardware, especially if the implant is not titanium. However, such interference is not common when CT scan is used for image capture.
In our series of nine patients, one required implant removal. The jigs fitted well in all patients and did not need a shift to the conventional technique in any patient. None of the patients needed blood transfusion. In comparison to an earlier study,10 all the surgeries were performed using the same PSB system (Preplan™). This helped in decreasing block and technology related variability between the patients.
Main drawbacks with PSB are the time lag between image acquisition and preparation of the blocks which can extend up to 3 weeks and the added cost associated with the manufacturing of the block. In our scenario, we have been able to decrease the cost of the manufacturing to approximately $400 and the period for manufacturing of the block has been decreased to 1 week.16 Moreover, a postoperative CT scan performed in these patients would have added to a better comparison of preoperative and postoperative alignment. A postoperative CT scan was, however, not included in the study protocol due to increased radiation exposure to the patients and ethical consideration. Another drawback of the study is the small sample size. This could be due to the incidence of patients with retained hardware undergoing TKA with retained femoral hardware being small. Manzotti et al., in a series of 789 knee replacements done over 9 years were able to find a subset of only 16 patients with retained hardware undergoing TKA.1 Hence, a sample size of nine patients undergoing TKA with retained hardware and using a newer technology like PSB is significant. This can act as a pilot for future studies using PSBs.
In our experience, in cases of retained femoral implants, one of the important factors to calculate preoperatively is the distance of the distal-most implant from the joint line. This is necessary as the distal tip of the implant usually comes close to the intercondylar notch. A distance of at least 12–17 mm of femoral bone is necessary for the central box cut of the posterior stabilized prosthesis. PSB provide a simple and accurate solution to the complex problem without increasing the morbidity and surgical time in these TKA.
There are some limitations of the study. First, it was a retrospective study. Furthermore, the sample size of the study is small. Since PSB are a relatively new technology and the cases with retained hardware are rare, it would need more time for the series of such patients to increase. The earlier mentioned use of PSB in retained hardware was restricted to a single case in ten cases of extraarticular deformity by Thienpont et al.10 Furthermore, our followup period is small.
Conclusion
With only one of the patients needing hardware removal in the current series, almost all the patients were saved the morbidity of implant removal. We suggest that PSBs should be considered as a viable option in patients with retained femoral hardware. With the advantage of pre-operative planning, the necessity of hardware removal may be obviated in most cases. The use of PSBs for performing TKA in retained femoral hardware was associated with significantly improved knee scores and no added morbidity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Manzotti A, Chemello C, Pullen C, Cerveri P, Confalonieri N. Computer-assisted total knee arthroplasty after prior femoral fracture without hardware removal. Orthopedics. 2012;35(10 Suppl):34–9. doi: 10.3928/01477447-20120919-55. [DOI] [PubMed] [Google Scholar]
- 2.Boonen B, Schotanus MG, Kort NP. Preliminary experience with the patient-specific templating total knee arthroplasty. Acta Orthop. 2012;83:387–93. doi: 10.3109/17453674.2012.711700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV., Jr Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Confalonieri N, Manzotti A, Pullen C, Rangone V. Computer-assisted technique versus intramedullary and extramedullary alignment systems in total knee replacement: A radiological comparison. Acta Orthop Belg. 2005;71:703–9. [PubMed] [Google Scholar]
- 5.Daniilidis K, Tibesku CO. Frontal plane alignment after total knee arthroplasty using patient-specific instruments. Int Orthop. 2013;37:45–50. doi: 10.1007/s00264-012-1732-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koch PP, Müller D, Pisan M, Fucentese SF. Radiographic accuracy in TKA with a CT-based patient-specific cutting block technique. Knee Surg Sports Traumatol Arthrosc. 2013;21:2200–5. doi: 10.1007/s00167-013-2625-6. [DOI] [PubMed] [Google Scholar]
- 7.Thienpont E, Bellemans J, Delport H, Van Overschelde P, Stuyts B, Brabants K, et al. Patient-specific instruments: industry's innovation with a surgeon's interest. Knee Surg Sports Traumatol Arthrosc. 2013;21:2227–33. doi: 10.1007/s00167-013-2626-5. [DOI] [PubMed] [Google Scholar]
- 8.Hoffart HE, Langenstein E, Vasak N. A prospective study comparing the functional outcome of computer-assisted and conventional total knee replacement. J Bone Joint Surg Br. 2012;94:194–9. doi: 10.1302/0301-620X.94B2.27454. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton WG, Parks NL, Saxena A. Patient-specific instrumentation does not shorten surgical time: A prospective, randomized trial. J Arthroplasty. 2013;28(8 Suppl):96–100. doi: 10.1016/j.arth.2013.04.049. [DOI] [PubMed] [Google Scholar]
- 10.Thienpont E, Paternostre F, Pietsch M, Hafez M, Howell S. Total knee arthroplasty with patient-specific instruments improves function and restores limb alignment in patients with extra-articular deformity. Knee. 2013;20:407–11. doi: 10.1016/j.knee.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Kim KK, Heo YM, Won YY, Lee WS. Navigation-assisted total knee arthroplasty for the knee retaining femoral intramedullary nail, and distal femoral plate and screws. Clin Orthop Surg. 2011;3:77–80. doi: 10.4055/cios.2011.3.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klein GR, Austin MS, Smith EB, Hozack WJ. Total knee arthroplasty using computer-assisted navigation in patients with deformities of the femur and tibia. J Arthroplasty. 2006;21:284–8. doi: 10.1016/j.arth.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Backstein D, Safir O, Gross A. Periprosthetic fractures of the knee. J Arthroplasty. 2007;22:45–9. doi: 10.1016/j.arth.2006.12.054. [DOI] [PubMed] [Google Scholar]
- 14.Engh GA, Petersen TL. Comparative experience with intramedullary and extramedullary alignment in total knee arthroplasty. J Arthroplasty. 1990;5:1–8. doi: 10.1016/s0883-5403(06)80002-1. [DOI] [PubMed] [Google Scholar]
- 15.Vaishya R, Singh AP, Vaish A. Outcome of subvastus approach in elderly nonobese patients undergoing bilateral simultaneous total knee arthroplasty: A randomized controlled study. Indian J Orthop. 2013;47:430–1. doi: 10.4103/0019-5413.114948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaishya R, Vijay V, Vaish A. Letter to the editor: Patient-specific instrumentation does not shorten surgical time: A prospective, randomized trial. J Arthroplasty. 2014;29:1508. doi: 10.1016/j.arth.2014.01.027. [DOI] [PubMed] [Google Scholar]
- 17.Ries MD. Prophylactic intramedullary femoral rodding during total knee arthroplasty with simultaneous femoral plate removal. J Arthroplasty. 1998;13:718–21. doi: 10.1016/s0883-5403(98)80019-3. [DOI] [PubMed] [Google Scholar]
- 18.Lin SY, Chen CH, Huang PJ, Fu YC, Huang HT. Computer-navigated minimally invasive total knee arthroplasty for patients with retained implants in the femur. Kaohsiung J Med Sci. 2014;30:415–21. doi: 10.1016/j.kjms.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Tigani D, Masetti G, Sabbioni G, Ben Ayad R, Filanti M, Fosco M. Computer-assisted surgery as indication of choice: Total knee arthroplasty in case of retained hardware or extra-articular deformity. Int Orthop. 2012;36:1379–85. doi: 10.1007/s00264-011-1476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hernandez-Vaquero D, Suarez-Vazquez A, Iglesias-Fernandez S. Computer-assisted navigation in total knee arthroplasty without femoral hardware removal. Acta Chir Orthop Traumatol Cech. 2012;79:331–24. [PubMed] [Google Scholar]
- 21.Bae DK, Song SJ. Computer assisted navigation in knee arthroplasty. Clin Orthop Surg. 2011;3:259–67. doi: 10.4055/cios.2011.3.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]