Abstract
Urbanization increases risk for depression and other mental disorders. A growing body of research indicates the natural environment confers numerous psychological benefits including alleviation of mental distress. This study examined land cover types and landscape metrics in relation to mental health for 276 U.S. counties within metropolitan areas having a population of 1 million or more. County Health Rankings and Behavioral Risk and Factor Surveillance System (BRFSS) provided a measure of mental health. The 2011 National Land Cover Database (NLCD) provided data on green land cover types, from which seven landscape metrics were generated to characterize landscape patterns. Spearman’s rho correlation and stepwise logistic regression models, respectively, were employed to examine bivariate and multivariate relationships. Models were adjusted for county population and housing density, region, race, and income to account for potential confounding. Overall, individual measures of landscape patterns showed stronger associations with mental health than percent total cover alone. Greater edge contrast was associated with 3.81% lower odds of Frequent Mental Distress (FMD) (Adjusted Odd’s Ratio (AOR) = 0.9619, 95% CI = 0.9371, 0.9860). Shrubland cohesion was associated with greater odds of FMD (AOR = 1.0751, 95% CI = 1.0196, 1.1379). In addition, distance between shrubland cover was associated with greater odds of FMD (AOR = 1.0027, 95% CI = 1.0016, 1.0041). Although effect sizes were small, findings suggest different types of landscape characteristics may have different roles in improving mental health.
Keywords: green land cover, urban forests, urbanization, landscape
1. Introduction
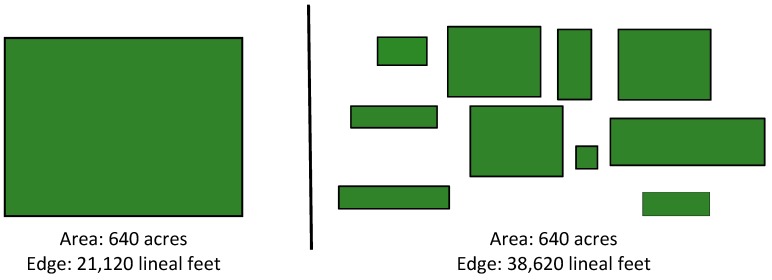
Urban green space has been associated with numerous health benefits. Access to public green space provides opportunities for physical activity, increased social cohesion, and improved psychological well-being [1,2,3,4,5,6]. Therefore, increased urbanization and potential loss of green vegetative cover including trees and open space in cities may hold important implications for human health [7]. Globally, more than half of the population inhabits urban areas. One common health challenge for urban inhabitants is mental distress [3,8]. Environmental exposures in urban built environments produce numerous stressors that adversely associate with mental health [9,10,11]. A meta-analysis of rural-urban differences in psychiatric disorders found that mood and anxiety disorders were more prevalent in urban areas [12]. Frequent mental distress has been linked with several health issues such as coronary heart disease and stroke [13]. Green land cover, even small and fragmented in urban areas [14], provides a range of benefits which can improve mental well-being and other aspects of preventive medicine [15]. For instance, studies correlate the presence of green spaces to fewer symptoms of depression [16], stress [17], and improved measures of well-being [18]. A twin study of effects of access to green space on self-reported depression, stress, and anxiety found significant associations for depression but none for stress and anxiety [19]. A longitudinal study in Britain explored the role of green space on residential happiness and found that people living in cities with more green space reported less mental distress and more well-being [20]. However, most of the studies only utilize total percent cover or greenness (e.g., percent tree cover and Normalized Difference Vegetation Index, respectively) [19,21,22], which mostly show the amount of green land cover and cannot provide information about specific landscape characteristics and their association with health outcomes. For example, as illustrated in Figure 1 (adapted from Adams [23]), forest cover varies in configuration and patterns. Large intact forest patches may exhibit different relationships to health and well-being outcomes than fragmented forest landscapes. Such differences could mean that some environmental attributes may better meet human psychological needs or provide better opportunities for contact with nature. For instance, forest edges have been associated with feelings of security because they fulfill the needs related to open views and enclosure as suggested by prospect refuge theory [24]. More edge density of green land cover may also imply more opportunities for people to realize mental health benefits from contact with nature in general [25], as well as nearby nature, such as street trees and gardens [14]. Moreover, different land cover types as well as landscape patterns may also have different effects on mental health [26]. Given growing interest in sustainable health promotion in cities [27], this study examined relationships between mental health and urban green land cover characteristics for 276 U.S. counties within metropolitan areas having a population of 1 million or more. To summarize, this study addresses the following hypotheses:
Figure 1.
Diagram representing total forest cover, smaller patches, corridors, and increased edges (Adapted from C.E. Adams).
Hypothesis 1.
Specific landscape characteristics are more strongly associated with mental health than amount of green land cover alone.
Hypothesis 2.
Types of green land cover are associated differently with mental health.
2. Methods
2.1. Study Area
U.S. metropolitan statistical areas (MSA) with more than 1 million in population (52 MSAs) were selected and analyzed at the county level (N = 276). The 52 MSA were divided into five regions based on the US Environmental Protection Agency’s ecoregion classification: Northeast (N = 34, including States of Maine, Vermont, New Hemisphere, Connecticut, New York, New Jersey, Massachusetts, Rhode Island, Pennsylvania, Maryland, and Delaware), Southeast (N = 106, including District of Columbia and States of West Virginia, Virginia, Kentucky, North Carolina, Tennessee, South Carolina, Georgia, Alabama, Mississippi, Arkansas, Florida, and Louisiana), Midwest (N = 61, including States of Michigan, Ohio, Indiana, Illinois, Minnesota, Wisconsin, Iowa, Missouri, North Dakoda, South Dakoda, Nebraska, and Kansas), West (N = 35, including States of Montana, Wyoming, Idaho, Colorado, Utah, Nevada, Washington, Oregon, and California), and Southwest (N = 40, including States of Oklahoma, Texas, New Mexico, and Arizona).
2.2. Mental Health
A mental health measure, Frequent Mental Distress, was obtained from County Health Rankings and Roadmaps and was derived from the 2014 U.S. Centers for Disease Control Behavioral Risk and Factor Surveillance System (BRFSS) [28]. Specifically, Frequent Mental Distress (FMD) was defined as percent of county respondents reporting 14 to 30 mentally unhealthy days in the past 30 days using the following question: Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good? (See Moriarty et al. [29] for detailed background on this measure). To classify counties into low and high levels of FMD, the Jenks Natural Breaks classification was employed [30]. This approach classifies observations into groups where the within-group variance is minimal and between-group variance is maximal. Thus, FMD was dichotomized using the break value to reflect low and high prevalence of FMD.
2.3. Land Cover
The 2011 National Land Cover Database (NLCD), a 30-m resolution raster dataset, classifies land cover into eight major types based on Anderson Level I Classification System [31] and provided measures of green land cover types (forest, shrubland, and herbaceous). Forests are areas dominated by trees with a height generally taller than 5 meters, shrubland refers to shrubs generally less than 5 meters in height and young trees at an early successional stage, and herbaceous refers to grassland or low vegetation and typically accounts for more than 75% of the cover [32]. Seven landscape metrics (percent cover, mean patch area, patch density, edge density, edge contrast index, Euclidean distance between patches, and patch cohesion index) were generated for each land cover type at the county level by FRAGSTATS 4.2 (Computer Software Program, University of Massachusetts, Amherst, MA, USA) [33]. Table 1 provides definitions for each of the seven landscape metrics. The selected metrics were chosen to characterize the patterns of green land cover based on existing theory and empirical studies that describe how natural environmental attributes potentially provide opportunities for human contact with nature or meet basic human psychological needs [34,35,36]. For instance, higher percentage of greenspace was found to associate with less stress, depression, and better mental health (percent cover) [37,38,39]. Generally having small parks but close to residential areas, provide more opportunities for urban inhabitants to use (patch size and patch cohesion index) [40]. Distance to small patches of urban greenery, such as greenspaces in urban residential areas, also supports greater frequency usage when compared to other urban greenspaces (e.g., urban parks) (patch size and Euclidean distance between patches) [41]. Likewise, availability of greenspaces increases the likelihood of walking activity (patch density) [42]. Edge features in an environmental setting provide psychological needs for human to both observe and hide (edge density and edge contrast index) [24,36].
Table 1.
Description of landscape metrics.
| Variable | Description |
|---|---|
| Percent Land Cover | The proportional abundance of vegetative cover in the defined area (e.g., county). |
| Patch Area | Mean of the total area of vegetative patches. |
| Patch Density | The number of vegetative patches per 100 hectares. |
| Edge Density | The total length of all vegetative edge segments per hectare. |
| Edge Contrast Index | The total length of segments between vegetative cover and developed area divided by the total perimeter of all the patches. |
| Euclidean Distance | Mean distance to the nearest neighbor patch with the same vegetative type (based on shortest edge-to-edge distance). |
| Patch Cohesion Index | The physical connectedness of vegetative cover. The value increases as the patch type becomes more physically connected. |
2.4. Confounding Variables
Population density, housing density, median household income and race (percentage of non-White racial/ethnic groups) were measured and treated as potential confounding variables in the statistical models [43]. These measures were extracted from the U.S. Census American Community Survey [44]. Because previous research found geographic differences in mental health in the U.S. [29,45], region also served as a potential confounder. The inclusion of region also accounts for differences in landscape biogeographic features in each region.
2.5. Statistical Analysis
Spearman’s rho provided tests of bivariate relationships with the exception of bivariate analysis of region and FMD where one-way Analysis of Variance was used. Stepwise logistic regression was performed to select the most influential landscape variables. Land cover types and landscape metrics of all three types (21 total) were first entered into the model as a pool of candidate variables, and then the set of predictor variables for FMD were finalized by using the Akaike Information Criterion as the selection criterion with bidirectional elimination. A subsequent model provided estimates of effects of the selected landscape metrics on FMD, adjusting for ecoregion and potential confounders. Generalized Variance Inflation Factor (GVIF) values greater than two indicated concerns with multicollinearity. Regression analyses were performed in R Studio 0.98.1103 (RStudio Inc, Boston, MA, USA).
3. Results
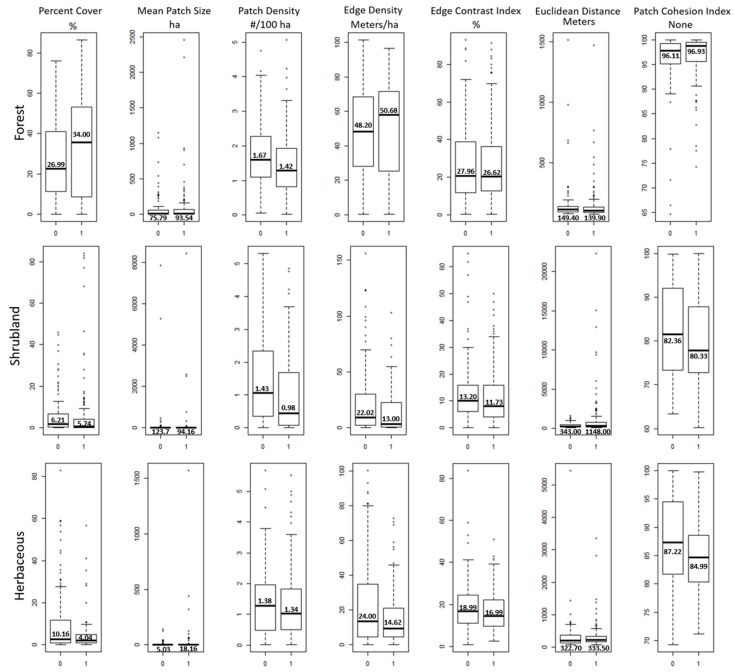
Descriptive statistics for study variables are presented in Table 2. FMD values ranged from 7% to 15% with a mean of 10.76% across the 276 counties. Using the Jenks Natural Breaks approach to dichotomize FMD, the break was identified at 10%. Using this break value as the cut point, 42.75% of counties were classified as low prevalence of FMD. One hundred eighteen counties (24 western, 33 southwestern, 23 midwestern, 16 northeastern, and 22 southeastern) were considered to have low prevalence of FMD. Most of the counties in the southeastern region (84 out of 106) had higher prevalence of FMD. Mean comparisons revealed that the prevalence of higher FMD was significantly greater in the southeast region (Table 3). Mean percent forest cover, edge density, and patch cohesion of forests were greater in counties with the higher prevalence of FMD. Shrubland and herbaceous cover were higher in counties with the low levels of FMD (Figure 2). Mean patch size was larger at the high level of FMD for forest and herbaceous cover but smaller for shrubland cover. Mean patch density and edge contrast index were consistently higher for all types of green land cover at the lower levels of FMD. Mean Euclidean distance between patches of forest and herbaceous cover were similar at both FMD levels but was much greater at the high level of FMD for shrubland cover.
Table 2.
Descriptive statistics for land cover classes, landscape metrics and potential confounding variables a.
| Variables | Mean | SD |
|---|---|---|
| Frequent mental distress | 10.76 | 2.0 |
| Forest | 0.31 | 22.29 |
| Patch area | 8594.68 | 24,802 |
| Patch density | 1.54 | 0.9 |
| Edge density | 49.62 | 26.14 |
| Edge contrast index | 27.19 | 20.78 |
| Euclidean distance | 143.94 | 155.27 |
| Patch cohesion index | 96.58 | 4.98 |
| Shrubland | 5.94 | 13.04 |
| Patch area (ha) | 10,680.60 | 78,921.10 |
| Patch density | 1.18 | 1.22 |
| Edge density | 16.86 | 24.44 |
| Edge contrast index | 12.36 | 11.10 |
| Euclidean distance | 803.69 | 2058.48 |
| Patch cohesion index | 81.2 | 10.25 |
| Herbaceous | 6.66 | 11.95 |
| Patch area (ha) | 1254.51 | 10,091.60 |
| Patch density | 1.36 | 1.14 |
| Edge density | 18.63 | 20.73 |
| Edge contrast index | 17.84 | 10.9 |
| Euclidean distance | 328.89 | 448.87 |
| Patch cohesion index | 85.94 | 7.45 |
| Potential Confounders | ||
| Population density | 402,639 | 823,130 |
| Housing density | 165,658 | 313,323 |
| Median HH income | 57,410 USD | 13,336.70 USD |
| Race (% non-white population) | 27.7 | 19.39 |
a Units of measure for each variable were as follows: Land cover type (%), patch area (ha), patch density (#/100ha), edge density (m/ha), edge contrast index (%), Euclidean distance (m), patch cohesion index (%), population density (#/km2), housing density (#km2).
Table 3.
Mean comparisons of Frequent Mental Distress by region.
| Region | N (Counties) | Mean | SD |
|---|---|---|---|
| Southwest | 40 | 9.5 a | 1.1 |
| West | 35 | 9.8 a | 1.2 |
| Northeast | 34 | 10.5 a,b | 1.2 |
| Midwest | 61 | 10.6 b,c | 1.2 |
| Southeast | 106 | 11.7 d | 1.4 |
ANOVA F = 26.15, df = 4271, p < 0.00001. a,b,c,d Mean values with different superscripts are statistically significant different at p < 0.01 (Scheffe Test).
Figure 2.
Descriptive statistics of FMD (Frequent Mental Distress) level by land cover and landscape metrics (A value of 0 on the X-axis indicates low levels of FMD (≤10%) and 1 indicates high level of FMD rate). Numerals within the plots are mean values).
Among the green land cover types, forest cover was most positively associated with the prevalence of FMD, whereas shrubland and herbaceous types had more negative significant associations with FMD (Table 4). Farther distance between forest patches had the strongest negative association with the prevalence of FMD (rho = −0.18, p < 0.01), whereas closer distance between shrubland patches had the strongest positive association with the prevalence of FMD (rho = 0.19, p < 0.01). Among the confounding variables, median household income (rho = −0.12, p < 0.05) and region (F = 26.15, p < 0.00001) were statistically associated with FMD.
Table 4.
Spearman correlations of frequent mental distress (FMD) with land cover classes, landscape metrics and potential confounding variables.
| Landscape Metric | rho | p-Value |
|---|---|---|
| Forest | 0.18 | 0.003 |
| Patch area | 0.17 | 0.005 |
| Patch density | −0.14 | 0.017 |
| Edge density | 0.11 | 0.059 |
| Edge contrast index | 0.05 | 0.386 |
| Euclidean distance | −0.18 | 0.003 |
| Patch cohesion index | 0.17 | 0.004 |
| Shrubland | −0.16 | 0.007 |
| Patch area | −0.10 | 0.094 |
| Patch density | −0.17 | 0.005 |
| Edge density | −0.17 | 0.004 |
| Edge contrast index | −0.08 | 0.188 |
| Euclidean distance | 0.19 | 0.001 |
| Patch cohesion index | −0.08 | 0.175 |
| Herbaceous | −0.14 | 0.019 |
| Patch area | −0.11 | 0.070 |
| Patch density | −0.03 | 0.670 |
| Edge density | −0.14 | 0.025 |
| Edge contrast index | −0.09 | 0.123 |
| Euclidean distance | 0.11 | 0.067 |
| Patch cohesion index | −0.13 | 0.027 |
| Potential Confounders | ||
| Population density | −0.08 | 0.214 |
| Housing density | −0.07 | 0.251 |
| Median Household Income | −0.12 | 0.042 |
| Race (% non-white population) | −0.14 | 0.016 |
Units of measure were as follows: Land cover type (%), patch area (ha), patch density (#/100ha), edge density (m/ha), edge contrast index (%), Euclidean distance (m), patch cohesion index (%), population density (#/km2), housing density (#km2).
Ten landscape metrics (%forest, %shrubland, %herbaceous, edge contrast index of forest and shrubland, mean patch size of shrubland, Euclidean distance between shrubland patches, patch cohesion index of shrubland, and patch density and edge density of herbaceous) were selected as predictors for the model following stepwise regression. Percent shrubland, edge density of herbaceous cover, and housing density were dropped from model estimation due to GVIF values greater than 2. After adjusting for region and potential confounders, increased forest edge contrast (F_ECON) was associated with 3.81% lower odds high level of FMD (Adjusted Odds Ratio = 0.9619, 95% CI = 0.9371, 0.9860) (Table 5). Shrubland cohesion (more connected shrubland) was associated with greater odds of FMD (AOR = 1.0751, 95% CI = 1.0196, 1.1379). Distance between scrubland cover was also associated with greater odds of FMD (AOR = 1.0027, 95% CI = 1.0016, 1.0041). Although these associations were statistically significant, effect sizes were small.
Table 5.
Logistic regression models of FMD adjusting for region, population and housing density, household income, and race.
| Adjusted Odds Ratio | 95% CI | 95% CI | |||
|---|---|---|---|---|---|
| Lower CI | Lower CI | ||||
| (Intercept) | 0.0016 | ** | 0.0000 | 0.0000 | |
| %Forest | 1.0132 | 0.9917 | 0.9917 | ||
| Forest-Edge contrast index | 0.9619 | ** | 0.9371 | 0.9371 | |
| Shrubland-Patch area | 1.0000 | 1.0000 | 1.0000 | ||
| Shrubland-Edge contrast index | 1.0068 | 0.9595 | 0.9595 | ||
| Shrubland-Euclidean distance | 1.0027 | *** | 1.0016 | 1.0016 | |
| Shrubland-Cohesion index | 1.0751 | ** | 1.0194 | 1.0194 | |
| %Herbaceous | 0.9957 | 0.9347 | 0.9347 | ||
| Herbaceous-Patch density | 1.2880 | 0.8612 | 0.8612 | ||
| Ecoregion | Midwest | Referent | |||
| Northeast | 1.0288 | 0.3255 | 3.2753 | ||
| Southeast | 1.9631 | 0.6698 | 5.8683 | ||
| Southwest | 0.0088 | *** | 0.0009 | 0.0666 | |
| West | 0.0453 | ** | 0.0053 | 0.3155 | |
| Population Density | DL | ||||
| Housing Density | 0.9990 | 0.9965 | 1.0014 | ||
| Median Household Income | 1.0000 | 1.0000 | 1.0000 | ||
| %Non-White | 1.0330 | * | 1.0063 | 1.0623 | |
Pseudo-R2 (McFadden) = 0.365; Significance level: * indicates p <0.05, ** indicates p < 0.01, and *** indicates p < 0.001; DL: deleted from the model due to a GVIF > 2.
4. Discussion
Environmental stressors in urban areas are associated with negative health risks including poor mental health [3,9]. Urban green land cover provides natural scenery and places for restoration from stress and mental fatigue [46,47,48,49]. This study examined the relationships between mental health and characteristics of urban green land cover measured by the amount of green cover (e.g., percent cover) and landscape patterns in 276 counties across the conterminous United States. Confounding factors associated with both urbanization and mental health were also considered. Results showed that longer distance between forest patches, suggestive of more spatially dispersed forests, had the most positive bivariate association with lower prevalence of frequent mental distress (FMD). In multivariable models, forest edge contrast index which indicates more connections between forest and built features was associated with lower mental distress.
Past research demonstrated that access to green space and viewing natural scenery in urban environments are associated with positive emotions, emotional fulfillment, and stress restoration [8,14,46,50]. Even small patches of urban green land cover such as street trees have positive effects on mental health [14]. Surprisingly, more forest cover exhibited a positive relationship with mental distress though it was not significant. Previous research reported a U-shaped dose-response curve for tree density and mental restoration. Jiang et al. reported tree density between 1.7% to 24% contributed to improved stress recovery and the recovery time started to decline when tree density was above 34% [51]. It is possible that there is a threshold for a given amount of landscape characteristics for improving mental health. Findings from the present study also revealed that other characteristics of green land cover (e.g., edge contrast index and patch cohesion index) might aid our understanding of the associations between green land cover and mental health status than percent land cover alone. This can be attributed to the role of edge fragmentation in making green spaces more accessible and supportive of recreational use and physical activity [52]. This study also indicates that different types of green land cover may have different effects on mental health. For example, previous research focused on New York City reported that tree cover was positively associated with reported good or excellent health status but not grass density [53]. Our findings showed that more aggregated shrubland contributed to increased odds of high levels of FMD. These findings suggest that not all the green land cover types have the same effects on health outcomes. Co-benefits associated with different land covers such as temperature and pollution mitigation and scenic views may also be critical for certain health outcomes [54].
Several studies reported that socioeconomic status was associated with mental health [43,55], as well as the process of urbanization [56,57]. Based on the bivariate results, higher median household income was significantly associated with lower mental distress. However, the strength of the land cover-FMD association attenuated slightly after adjusting for income. It is possible that other factors, particularly social engagement, are key mediators in green space-mental health relationships [1,5,58]. Current theorizing suggests that public green space may affect mental health through a number of pathways including social cohesion defined by shared values, norms and social ties in a neighborhood [5,6]. Significant associations between region and FMD were consistent with previous findings related to geographic variation in mental health [29,45].
Several limitations of this study exist. First, the cross-sectional analysis does not permit tests of causal relationships between land cover and mental health [5,59]. Future research should perform longitudinal studies and other appropriate designs to examine causal linkages. Second, the mental health measure relied on self-report and consisted of a single survey item. Third, the analyses relied on 30-m land cover data which compromises accurate land cover classification in densely developed urban areas. Higher resolution land cover data are needed for better identifying small and fragmented (e.g., street trees) green land cover in urban areas. Next, green land cover across the U.S. varies by climatic conditions and geographic features. For example, green land cover in southwestern U.S. counties included in this study are mostly shrubland, whereas in the northwest it is mostly forest. Therefore, greater specification of these regional differences offers opportunities for future research. Further studies should examine green land cover and health using a stratified approach. For example, separate models can be estimated by region or land cover types. Small effect sizes were also observed. In this regard, we acknowledge that mental distress arises from complex interactions of biological, psychosocial, and environmental factors [60]. Additional investigations should clarify pathways that link urban landscape characteristics to mental health. Strengths of the study include use of measures from a widely used and validated surveillance system and objective measures from a national land cover database. Furthermore, the study examined mental health in relation to several landscape metrics in addition to total land cover. With increasing population growth in urban areas and potential threats to green land cover, further research is needed to advance understanding of relationships between urban green land cover and public health. Our study aimed to provide direction for future research by highlighting the importance of studying both land cover classifications and specific landscape metrics in relation to mental health in urban areas.
Acknowledgments
We express appreciation to the National Urban and Community Forestry Advisory Council for funding data collection and US Forest Service Southern Research Station (Agreement 16-JV-11330144-065) for supporting data analysis for this research.
Author Contributions
Wei-Lun Tsai contributed to conceptualization and design of the study, data acquisition, statistical analysis and interpretation, and drafting of the article. Melissa R. McHale contributed to study design, interpretation of results, and critical revisions of the article for intellectual content. Viniece Jennings provided interpretation of the results and critically revised the article for intellectual content. Oriol Marquet contributed to the review of study design, interpretation of results, and critical revisions for intellectual content. J. Aaron Hipp contributed to review of the study design and critically revised the article for intellectual content. Yu-Fai Leung contributed to the design of the study, acquisition of the data, and critical review of the article for intellectual content. Myron F. Floyd contributed to study conceptualization and design, statistical analysis, interpretation of the data, and drafting the article. He is the corresponding author. All authors made substantial contributions to the work reported.
Conflicts of Interest
The authors declare no conflict of interest. Statements in this article are those of the authors and do not necessarily reflect the views of the U.S. federal government.
References
- 1.De Vries S., van Dillen S.M., Groenewegen P.P., Spreeuwenberg P. Streetscape greenery and health: Stress, social cohesion and physical activity as mediators. Soc. Sci. Med. 2013;94:26–33. doi: 10.1016/j.socscimed.2013.06.030. [DOI] [PubMed] [Google Scholar]
- 2.Astell-Burt T., Mitchell R., Hartig T. The association between green space and mental health varies across the lifecourse: A longitudinal study. J. Epidemiol. Community Health. 2014;68:578–583. doi: 10.1136/jech-2013-203767. [DOI] [PubMed] [Google Scholar]
- 3.Bratman G.N., Hamilton J.P., Daily G.C. The impacts of nature experience on human cognitive function and mental health. Ann. N. Y. Acad. Sci. 2012;1249:118–136. doi: 10.1111/j.1749-6632.2011.06400.x. [DOI] [PubMed] [Google Scholar]
- 4.West S.T., Shores K.A., Mudd L.M. Association of available parkland, physical activity, and overweight in America’s largest cities. J. Public Health Manag. Pract. 2012;18:423–430. doi: 10.1097/PHH.0b013e318238ea27. [DOI] [PubMed] [Google Scholar]
- 5.Hartig T., Mitchell R., de Vries S., Frumkin H. Nature and Health. Annu. Rev. Public Health. 2014;35:207–228. doi: 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- 6.Markevych I., Schoierer J., Hartig T., Chudnovsky A., Hystad P., Dzhambov A.M., de Vries S., Triguero-Mas M., Brauer M., Nieuwenhuijsen M.J., et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017;158:301–317. doi: 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- 7.Marsella A.J. Urbanization, mental health, and social deviancy: A review of issues and research. Am. Psychol. 1998;53:624–634. doi: 10.1037/0003-066X.53.6.624. [DOI] [PubMed] [Google Scholar]
- 8.Karjalainen E., Sarjala T., Raitio H. Promoting human health through forests: Overview and major challenges. Environ. Health Prev. Med. 2010;15:1–8. doi: 10.1007/s12199-008-0069-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maantay J., Maroko A. ‘At-risk’ places: Inequities in the distribution of environmental stressors and prescription rates of mental health medications in Glasgow, Scotland. Environ. Res. Lett. 2015;10 doi: 10.1088/1748-9326/10/11/115003. [DOI] [Google Scholar]
- 10.Downey L., Van Willigen M. Environmental stressors: The mental health impacts of living near industrial activity. J. Health Soc. Behav. 2005;46:289–305. doi: 10.1177/002214650504600306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guite H.F., Clark C., Ackrill G. The impact of the physical and urban environment on mental well-being. Public Health. 2006;120:1117–1126. doi: 10.1016/j.puhe.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Peen J., Schoevers R.A., Beekman A.T., Dekker J., Peen The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 13.Liu Y., Croft J.B., Wheaton A.G., Perry G.S., Chapman D.P., Strine T.W., McKnight-Eily L.R., Presley-Cantrell L. Association between perceived insufficient sleep, frequent mental distress, obesity and chronic diseases among US adults, 2009 Behavioral Risk Factor Surveillance System. BMC Public Health. 2013;13:84. doi: 10.1186/1471-2458-13-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor M.S., Wheeler B.W., White M.P., Economou T., Osborne N.J. Research note: Urban street tree density and antidepressant prescription rates—A cross-sectional study in London, UK. Landsc. Urban Plan. 2015;136:174–179. doi: 10.1016/j.landurbplan.2014.12.005. [DOI] [Google Scholar]
- 15.Jennings V.L., Larson C.K., Larson L.R. Ecosystem services and preventive medicine. Am. J. Prev. Med. 2016;50:642–645. doi: 10.1016/j.amepre.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Miles R., Coutts C., Mohamadi A. Neighborhood urban form, social environment, and depression. J. Urban Health. 2012;89:1–18. doi: 10.1007/s11524-011-9621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chawla L., Keena K., Pevec I., Stanley E. Green schoolyards as havens from stress and resources for resilience in childhood and adolescence. Health Place. 2014;28:1–13. doi: 10.1016/j.healthplace.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Larson L.R., Jennings V., Cloutier S.A. Public parks and wellbeing in urban areas of the United States. PLoS ONE. 2016;11:e0153211. doi: 10.1371/journal.pone.0153211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen-Cline H., Turkheimer E., Duncan G.E. Access to green space, physical activity and mental health: A twin study. J. Epidemiol. Community Health. 2015;69:523–529. doi: 10.1136/jech-2014-204667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White M.P., Alcock I., Wheeler B.W., Depledge M.H. Would you be happier living in a greener urban area? A fixed-effects analysis of panel data. Psychol. Sci. 2013;24:920–928. doi: 10.1177/0956797612464659. [DOI] [PubMed] [Google Scholar]
- 21.Beyer K., Kaltenbach A., Szabo A., Bogar S., Nieto F., Malecki K. Exposure to neighborhood green space and mental health: Evidence from the survey of the health of Wisconsin. Int. J. Environ. Res. Public Health. 2014;11:3453–3472. doi: 10.3390/ijerph110303453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gidlow C.J., Smith G., Martinez D., Wilson R., Trinder P., Gražulevičiene R., Nieuwenhuijsen M.J. Research note: Natural environments and prescribing in England. Landsc. Urban Plan. 2016;151:103–108. doi: 10.1016/j.landurbplan.2016.02.002. [DOI] [Google Scholar]
- 23.Adams C.E. Urban Wildlife Management. 3rd ed. CRC Press; Boca Raton, FL, USA: 2016. [Google Scholar]
- 24.Mumcu S., Düzenli T., Özbilen A. Prospect and refuge as the predictors of preferences for seating areas. Sci. Res. Essays. 2010;5:1223–1233. [Google Scholar]
- 25.Roux A.V., Evenson K.R., McGinn A.P., Brown D.G., Moore L., Brines S., Jacobs D.R., Jr. Availability of recreational resources and physical activity in adults. Am. J. Public Health. 2007;97:493–499. doi: 10.2105/AJPH.2006.087734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akpinar A., Barbosa-Leiker C., Brooks K.R. Does green space matter? Exploring relationships between green space type and health indicators. Urban For. Urban Green. 2016;20:407–418. doi: 10.1016/j.ufug.2016.10.013. [DOI] [Google Scholar]
- 27.Hartig T., Kahn P.H. Living in cities, naturally. Science. 2016;352:938–940. doi: 10.1126/science.aaf3759. [DOI] [PubMed] [Google Scholar]
- 28.Roadmaps C.H.R. County Health Rankings & Roadmaps. [(accessed on 1 October 2016)];2016 Available online: http://www.countyhealthrankings.org/explore-health-rankings/what-and-why-we-rank/health-outcomes/morbidity/health-related-quality-of-life/frequent-mental-distress.
- 29.Moriarty D.G., Zack M.M., Holt J.B., Chapman D.P., Safran M.A. Geographic Patterns of Frequent Mental Distress: U.S. Adults, 1993–2001 and 2003–2006. Am. J. Prev. Med. 2009;36:497–505. doi: 10.1016/j.amepre.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 30.Jenks G.F. The data model concept in statistical mapping. Int. Yearb. Cartogr. 1967;7:186–190. [Google Scholar]
- 31.Anderson J.R., Hardy E.E., Roach J.T., Witmer R.E. A Land Use and Land Cover Classification System for Use with Remote Sensor Data. Geological Survey; Washington, DC, USA: 1976. [Google Scholar]
- 32.Homer C.G., Huang C., Yang L., Wylie B.K., Coan M. Development of a 2001 National Land Cover Database for the United States. Photogramm. Eng. Remote Sens. 2004;70:829–840. doi: 10.14358/PERS.70.7.829. [DOI] [Google Scholar]
- 33.McGarigal K., Cushman S.A., Ene E. FRAGSTATS v4: Spatial Pattern Analysis Program for Categorical and Continuous Maps. University of Massachusetts; Amherst, MA, USA: 2012. Computer Software Program. [Google Scholar]
- 34.Cohen D., McKenzie T., Sehgal A., Williamson S., Golinelli D., Lurie N. Contribution of public parks to physical activity. Am. J. Public Health. 2007;97:509–514. doi: 10.2105/AJPH.2005.072447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brownson R.C., Chriqui J.F., Stamatakis K.A. Understanding evidence-based public health policy. Am. J. Public Health. 2009;99:1576–1583. doi: 10.2105/AJPH.2008.156224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ruddell E.J., Hammitt W.E. Prospect refuge theory: A psychological orientation for edge effects in recreation environment. J. Leis. Res. 1987;19:249–260. doi: 10.1080/00222216.1987.11969696. [DOI] [Google Scholar]
- 37.Ward Thompson C., Roe J., Aspinall P., Mitchell R., Clow A., Miller D. More green space is linked to less stress in deprived communities: Evidence from salivary cortisol patterns. Landsc. Urban Plan. 2012;105:221–229. doi: 10.1016/j.landurbplan.2011.12.015. [DOI] [Google Scholar]
- 38.Min K., Kim H., Kim H., Min J. Parks and green areas and the risk for depression and suicidal indicators. Int. Public Health J. 2017;62:647–656. doi: 10.1007/s00038-017-0958-5. [DOI] [PubMed] [Google Scholar]
- 39.Triguero-Mas M., Dadvand P., Cirach M., Martínez D., Medina A., Mompart A., Basagaña X., Gražulevičiene R., Nieuwenhuijsen M.J. Natural outdoor environments and mental and physical health: Relationships and mechanisms. Environ. Int. 2015;77:35–41. doi: 10.1016/j.envint.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 40.Forsyth A., Musacchio L. Designing Small Parks: A Manual Addressing Social and Ecological Concerns. Wiley; Hoboken, NJ, USA: 2005. [Google Scholar]
- 41.Nielsen T., Hansen K. Do green areas affect health? Results from a Danish survey on the use of green areas and health indicators. Health Place. 2007;13:839–850. doi: 10.1016/j.healthplace.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Takano T., Nakamura K., Watanabe M. Urban residential environments and senior citizens’ longevity in megacity areas. The importance of walkable green spaces. J. Epidemiol. Community Health. 2002;56:913–918. doi: 10.1136/jech.56.12.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention Self-reported frequent mental distress among adults-United States, 1993–2001. Morb. Mortal. Wkly. Rep. 2004;53:963–966. [PubMed] [Google Scholar]
- 44.US Census Bureau 2012–2016 American Community Survey 5-Year Estimates. [(accessed on 4 February 2018)]; Available online: https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/2016.
- 45.Current depression among adults—United States, 2006 and 2008. Morb. Mortal. Wkly. Rep. 2010;59:1229–1235. [PubMed] [Google Scholar]
- 46.Grahn P., Stigsdotter U.K. The relation between perceived sensory dimensions of urban green space and stress restoration. Landsc. Urban Plan. 2010;94:264–275. doi: 10.1016/j.landurbplan.2009.10.012. [DOI] [Google Scholar]
- 47.Kaplan S. The urban forest as a source of psychological well-being. In: Bradley G.A., editor. Urban Forest Landscape: Integrating Multidisciplinary Perspectives. University of Washington Press; Seattle, WA, USA: 1995. pp. 101–108. [Google Scholar]
- 48.Ulrich R.S., Simons R.F., Losito B.D., Fiorito E., Miles M.A., Zelson M. Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 1991;11:201–230. doi: 10.1016/S0272-4944(05)80184-7. [DOI] [Google Scholar]
- 49.Nordh H., Hartig T., Hagerhall C.M., Fry G. Components of small urban parks that predict the possibility for restoration. Urban For. Urban Green. 2009;8:225–235. doi: 10.1016/j.ufug.2009.06.003. [DOI] [Google Scholar]
- 50.Van den Berg A.E., Maas J., Verheij R.A., Groenewegen P.P. Green space as a buffer between stressful life events and health. Soc. Sci. Med. 2010;70:1203–1210. doi: 10.1016/j.socscimed.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 51.Jiang B., Chang C.-Y., Sullivan W.C. A dose of nature: Tree cover, stress reduction, and gender differences. Lands. Urban Plan. 2014;132:26–36. doi: 10.1016/j.landurbplan.2014.08.005. [DOI] [Google Scholar]
- 52.Tsai W.-L., Floyd M.F., Leung Y.-F., McHale M.R., Reich B.J. Urban vegetative cover fragmentation in the U.S.: Associations with physical activity and BMI. Am. J. Prev. Med. 2016;50:509–517. doi: 10.1016/j.amepre.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 53.Reid C., Clougherty J., Shmool J., Kubzansky L. Is all urban green space the same? A comparison of the health benefits of trees and grass in New York City. Int. J. Environ. Res. Public Health. 2017;14:1411. doi: 10.3390/ijerph14111411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harlan S.L., Ruddell D.M. Climate change and health in cities: Impacts of heat and air pollution and potential co-benefits from mitigation and adaptation. Curr. Opin. Environ. Sustain. 2011;3:126–134. doi: 10.1016/j.cosust.2011.01.001. [DOI] [Google Scholar]
- 55.Williams D.R., Yan Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J. Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 56.Abdullah S.A., Nakagoshi N. Forest fragmentation and its correlation to human land use change in the state of Selangor, peninsular Malaysia. For. Ecol. Manag. 2007;241:39–48. doi: 10.1016/j.foreco.2006.12.016. [DOI] [Google Scholar]
- 57.Henderson V. The urbanization process and economic growth: The so-what question. J. Econ. Growth. 2003;8:47–71. doi: 10.1023/A:1022860800744. [DOI] [Google Scholar]
- 58.Nieminen T., Martelin T., Koskinen S., Aro H., Alanen E., Hyyppä M.T. Social capital as a determinant of self-rated health and psychological well-being. Int. J. Public Health. 2010;55:531–542. doi: 10.1007/s00038-010-0138-3. [DOI] [PubMed] [Google Scholar]
- 59.Glass T.A., Goodman S.N., Hernán M.A., Samet J.M. Causal inference in public health. Annu. Rev. Public Health. 2013;34:61–75. doi: 10.1146/annurev-publhealth-031811-124606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ahn W.-K., Proctor C.C., Flanagan E.H. Mental Health Clinicians’ Beliefs about the Biological, Psychological, and Environmental Bases of Mental Disorders. Cogn. Sci. 2009;33:147–182. doi: 10.1111/j.1551-6709.2009.01008.x. [DOI] [PMC free article] [PubMed] [Google Scholar]