Abstract
Autism spectrum disorders (ASD) and obsessive-compulsive disorder (OCD) are highly comorbid, precipitating an urgent need to identify evidence-based practices that might be used to address this comorbidity exclusively. The aim of this study was to conduct a review of intervention research and clinical reports to examine the use of cognitive behavioral therapy (CBT) with individuals who have comorbid ASD and OCD. Based on the pre-determined review inclusion criteria, 11 studies were included in the review: three randomized control trials (RCT), one case controlled study, two single subject experimental designs, and five case studies. These studies offer promising data on the use of CBT interventions for individuals with ASD and comorbid OCD as well as for individuals with OCD and comorbid ASD when standard CBT protocol is enhanced with modifications such as parental involvement, increased use of visuals, personalized treatment metaphors, self-monitoring, positive reinforcement, and use of clear language and instructions. Limitations and implications for future research and practice are discussed.
Keywords: Cognitive behavioral therapy, Obsessive-compulsive disorder, Autism spectrum disorders, Modifications, Comorbidity, Evidence-based practices
Autism spectrum disorders (ASD) are a continuum of neurodevelopmental disorders characterized by impairments in reciprocal social interaction and communication as well as restrictive, repetitive patterns of behavior and interests (DSM-V, American Psychiatric Association [APA] 2013). In 2014, the Autism and Developmental Disabilities Monitoring Network reported that about one in 68 children in the United States (US) was diagnosed with ASD (ADDM Principal Investigators 2010).
Individuals with ASD are at an increased risk of presenting with comorbid psychopathology (Joshi et al. 2013; Matson and Nebel-Schwalm 2007; Tsakanikos et al. 2006) with researchers finding that 72% - 80% of children with ASD meet criteria for a comorbid psychiatric disorder. Obsessive-compulsive disorder (OCD) was reported to occur as a comorbid condition with autism in 37% of the population (Joshi et al. 2010; White et al. 2009a, b). According to DSM-IV (American Psychiatric Association 2000), OCD was one of the nine major types of anxiety disorders; however, it is classified as a separate disorder according to DSM-V (American Psychiatric Association 2013). OCD is a chronic condition characterized by repeated intrusive thoughts and compulsive acts that are ego-dystonic (i.e., not pleasurable, distressing and resisted) (American Psychiatric Association 2013) while the repetitive patterns of behavior endemic to ASD are thought to be ego-syntonic (i.e., pleasurable, not distressing and not resisted). This prognostic criterion is critical to preclude diagnostic overshadowing since when left ignored, obsessive-compulsive behaviors (OCBs) might be confused with autism-related repetitive and restricted behaviors and remain untreated. Whilst OCD traits are prevalent in ASD, ASD traits in OCD are recognized significantly more often. Meier et al. (2015) found that individuals with a primary diagnosis of ASD had a 2-fold higher risk of comorbid of OCD, whereas individuals with a primary diagnosis of OCD displayed a nearly 4-fold higher risk of a subsequent diagnosis of ASD.
The comorbid condition of OCD can be a challenging issue for individuals with ASD. Thus, the identification of effective treatment approaches to address OCD for individuals with autism is a critical need. The first line of treatment for OCD in the general population is the use of cognitive behavioral therapy (CBT) (McGuire et al. 2015). Since OCD affects individuals with ASD in the same way it affects the general population, CBT has been shown to help this specific population as well in reducing their OCBs. Prior research has focused on the treatment options for individuals with ASD and OCD separately or for individuals with ASD and other comorbid disorders, including but not limited to OCD (Lang et al. 2010; Neil and Sturmey 2014). This review conceptually had a more concentrated focus and evaluated the research that has used CBT in the treatment of individuals who have both ASD and OCD only.
Cognitive Behavioral Therapy
CBT with exposure and response prevention (ERP) is the best-established psychological treatment for typically developing people with OCD (Ponniah et al. 2013). Although outcome studies of ERP proved to be very successful for reducing OCD symptoms (Foa et al. 2005; McGuire et al. 2015; Simpson et al. 2008), the prominence of cognitive biases, dysfunctional beliefs, and erroneous thinking in the disorder motivated the inclusion of the cognitive component in the treatment regimen of OCD, namely cognitive therapy (CT) (Freeston and Ladouceur 1999). In its current form, there are generally five components to CBT: (1) psychoeducation, (2) fear hierarchy development, (3) exposure/response prevention, (4) cognitive strategies, and (5) generalization/relapse prevention (Piacentini and Langley 2004; March et al. 2001).
With the recognition of the high comorbidity of anxiety with ASD, the use of CBT with individuals with ASD has become increasingly prominent (White et al. 2010). However, due to the unique challenges and multifaceted needs of individuals on the autism spectrum, standard CBT programs require individualized modifications (Scattone and Mong 2013). There are several studies that have demonstrated that a personalized variant of CBT can result in successful outcomes when treating anxiety symptoms within the ASD population (Reaven and Hepburn 2003; Reaven et al. 2009, 2012; Sofronoff et al. 2005; Storch et al. 2013, 2015; White et al. 2009a, b; Wood et al. 2009, 2015). In these studies, primary modifications included increased structure in the sessions, visual aids and cues, and considerable parent involvement (i.e., parents as coaches in intervention delivery). Modifications made in the process, content, and structure of standard CBT address social and communication difficulties, cognitive rigidity, alexithymia (i.e., difficulties with describing and labeling emotions), and difficulties in generalization faced by individuals with ASD (Bird and Cook 2013; Dahlgren et al. 2003; Happé and Frith 2006).
Given the elevated prevalence of OCD in the ASD population (Joshi et al. 2010; White et al. 2009a, b) and the frequency of autistic symptoms in pediatric OCD (Meier et al. 2015), there is a need for identifying evidence-based practices for this dual psychopathology. There is an established research base supporting the effectiveness of CBT for alleviating anxiety symptoms in individuals with ASD and considerable work has been done addressing the treatment needs of individuals with ASD with varying clinical presentations (Dawson et al. 2010; Kasari 2002). To the best of the authors' knowledge, there has been no review to date focusing on the effectiveness of CBT for individuals diagnosed with ASD and OCD exclusively. This review aimed to (1) identify research studies that document the use of CBT to treat OCD in individuals with ASD; (2) identify the treatment components and the modifications that were used to support the engagement of individuals with ASD in the treatment protocol; and (3) discuss research and clinical practice implications arising from the literature.
Method
We identified studies by detailed searches of the following electronic databases: ERIC, ProQuest, PsychINFO, PsycARTICLES, and Google Scholar. We also searched the electronic database of the University of South Florida (USF) Library to identify any overlooked studies relevant for review. Search terms for all databases included at minimum one identifier for ASD (e.g., autism, autistic, Asperger, pervasive developmental disorder (PDD), one identifier for OCD (e.g., obsessions and compulsions, obsessive-compulsive disorder), and one identifier for evidence-based practices (e.g., CBT, exposure response prevention) in the title and/or full text of the article. We used a combination of search terms including: cognitive behav*- autism*- Asperger* - obsessive-compul* - pervasive develop* - cbt for ocd and asd* –cbt for comorbid asd*.
After we screened titles and abstracts for eligibility, we included the treatment studies if they were published in peer-reviewed English language journals after 1/1/2000 to keep track of the most recent and updated evidence-based practices. The other criteria included: (1) participants had a diagnosis of ASD (or autistic disorder, Asperger disorder, or pervasive developmental disorder falling under the ASD criteria according to the publication of DSM-V) and comorbidity of OCD or vice versa, (2) the treatment used was any modality of CBT (e.g., individual, group-based, family-centered therapy, and Function-based CBT), (3) the authors evaluate the effectiveness of CBT components (both cognitive and/or behavioral) for people with ASD and OCD, (4) the results reported on at least one validated and standardized outcome measure of core features of OCD. No limits were applied to the age of participants or severity of the diagnosis (i.e., both low- and high-functioning autism and mild to severe OCD are included). All quantitative research manuscripts were eligible to be included, regardless of research design (i.e., single subject, case study, or group).
Studies were excluded if they met the following criteria: (1) the primary intervention was not CBT (e.g., psychopharmacological treatment, anger-management etc.), (2) methodology employed was qualitative or a meta-analysis, (3) CBT interventions delivered to people with ASD and other comorbidities than OCD (e.g., anxiety disorder, attention deficit hyperactivity disorder (ADHD) and vice versa, or (4) CBT interventions delivered exclusively to people with ASD or exclusively to people with OCD.
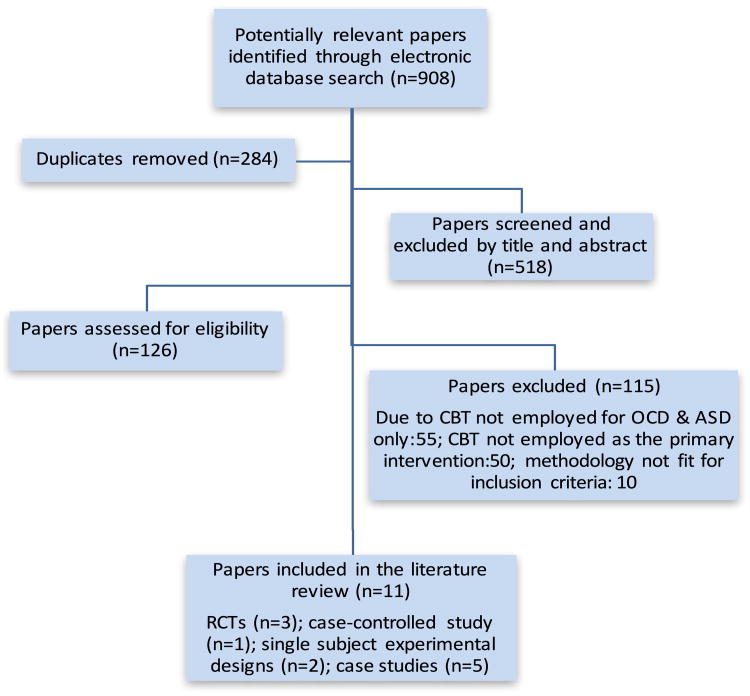
The initial search of the electronic databases yielded 908 potentially eligible articles that met the search terms; we removed 284 duplicates at this stage. As a result of an initial screen of the titles and abstracts, we excluded 518 papers due to not meeting any of the inclusion criteria. To enhance rigor, the second author screened 10% (52 papers) of all titles and abstracts for eligibility, resulting in agreement in all cases. Out of the remaining 106 studies, we excluded 55 papers because CBT was not employed for OCD and ASD comorbidity exclusively (it was employed either for typically developing people with OCD, or for people with ASD or anxiety, or for people with OCD and other disorders than ASD (e.g., social phobia, depression, sleep problems etc.). From the rest, we excluded 30 papers because CBT was not employed as the primary intervention and the effects of CBT could not be isolated, and 10 papers because the methodology employed did not fit for the inclusion criteria (see Fig. 1 for research review results).
Fig. 1. Research Review Results.
One study that met the inclusion criteria was in press. Thus, a total of eleven studies were included in the review: three randomized control trials (RCTs), one case controlled study, two single subject experimental designs, and five case studies. We also closely examined the reference lists of these eleven papers; no new studies were found for inclusion.
Results
A total of eleven studies met the criteria for inclusion in this review (Elliott and Fitzsimons 2014; Farrell et al. 2016; Lehmkuhl et al. 2008; Murray et al. 2015; Nadeau et al. 2013; Neil et al. 2017; Reaven and Hepburn 2003; Russell et al. 2013; Vause et al. 2014, 2015; Wolters et al. 2016). Table 1 summarizes the studies in terms of participant characteristics, nature of the intervention, and treatment outcomes.
Table 1. Overview of studies.
| Study | Method | Sample (n, core and comorbid diagnosis) | Intervention | Results |
|---|---|---|---|---|
| Elliott and Fitzsimons (2014) U.K. | Case study | 1 male: 7 years old ASD OCD |
Number of sessions: 10 Session duration: not specified Techniques: Traditional elements of CBT with modifications |
Authors describe reduction in symptoms |
| Farrell et al. (2016) Australia | Case study | 1 male: 16 years old, Caucasian Australian OCD ASD, ADHD |
Number of sessions: 6 (3 intensive CBT and 3 maintenance sessions) Session duration: not specified Techniques: Family psycho-education, intensive ERP |
Reductions in severity scores of all checklists *Not diagnosed with OCD at 3 month follow-up |
| Lehmkuhl et al. (2008) U.S. | Case study | 1 male: 12 years old ASD OCD |
Number of sessions: 10 Session duration: 50 min. Techniques: Traditional elements of CBT with modifications for ASD |
Reductions in OCD symptoms, CY-BOCS score decreased from 18 (moderately se vere) to 3 (within normal limits) and CYIS score from 40 to 3 at pre/post treatments *Parent report of treatment effect maintenance at 3 month post-treatment |
| Murray et al. (2015) U.K. | Case-controlled study CBT for OCD + ASD (n = 22) vs OCD + NoASD (n = 22) |
44 individuals (ages not specified) OCD + ASD mean age: 15 OCD + NoASD mean age: 15 OCD ASD |
Number of sessions: 14 (no significant change between the two groups, OCD + ASD and OCD + NoASD) Session duration: 1 h Techniques: Psycho-education, graded EPR, Relapse prevention |
Smaller decrease in symptoms in OCD + ASD than in OCD + NoASD (38.31% vs 48.20%) and lower remission rates at post-treatment (9% vs 46%) |
| Nadeau et al. (2013) U.S. | Case study | 1 male: 9 years old, Caucasian ASD OCD, social phobia and specific phobia |
Number of sessions: 16 Session duration: 35–70 min. Techniques: affective education, coping skill development, identification and generation of rewards, OCD hierarchy & EPR |
Reductions in OCD symptoms & decreases in all checklist scores from clinical significance to within normal limits, CY-BOCS score decreased from 27 (severe) to 0* *Treatment gains sustained at 4 month follow-up |
| Neil et al. (2017) Canada | Multiple baseline across behaviors | 1 male: 11 years old ASD OCBs |
Number of sessions: 9 Session duration: 2 h. Techniques: Psycho-education, cognitive-behavioral skills training, and exposure and response prevention coupled with functional behavioral as sessment and intervention |
Decreases of OCBs to zero levels in all checklists and high consumer satisfaction *Treatment gains maintained at 6, 12, and 20 month follow-up |
| Reaven and Hepburn (2003) U.S. | Case study | 1 female: 7 years old Asperger syndrome OCD |
Number of sessions: 14 Session duration: not specified Techniques: Traditional elements of CBT with modifications (establishing a neurobehavioral framework, mapping OCD symptoms, establishing a hierarchy, ERP), and intervening with other behaviors on the hierarchy) |
65% decrease in OCD symptoms |
| Russell et al. (2013) U.K. | RCT CBT for OCD (n = 20) vs Anxiety Management (AM) (n = 20) |
46 adolescents & adults (aged 14–65 years) CBT mean age: 28.6 AM mean age: 25.2 ASD, OCD |
Number of sessions: Mean CBT: 17.4 Mean AM: 14.4 Session duration: 1 h Techniques: emotional literacy, exposure-based tasks, cognitive restructuring |
Statistically significant reductions in OCD symptoms in both (CBT and AM) condition; no significant difference between groups (45% and 20% treatment responders in CBT and AM, respectively) *Treatment gains sustained over 12 month follow-up |
| Vause et al. (2014) Canada | Multiple baseline across behaviors and participants | 1 male: 10 years old 1 female: 8 years old ASD OCD |
Number of sessions: 15 for male, 11 for female Session duration: 90 min. For male, 60–90 min. For female Techniques: psychoeducation/mapping, cognitive training, (graded) exposure and response prevention (ERP), and relapse prevention (with adaptations for ASD) |
Reductions in OCD symptoms in both cases, CY-BOCS score decreased from 25 (severe) to 14.5 (mild) for male and from 29 (severe) to 9.5 (subclinical) for female Reduction in target behavior to near zero levels after FBAI, CT, ERP plus Positive Reinforcement was implemented in addition to psychoeducation and mapping |
| Vause et al. (2015) Canada | RCT Function based- CBT (Fb-CBT) for OCD (n = 7) vs Treatment as usual (TAU) (n = 7) |
14 children (8–12 years) Fb-CBT mean age: 9.32 TAU mean age: 10.17 High-functioning ASD OCD |
Number of sessions: Fb-CBT: 9 TAU:0 Session duration: 2 h Techniques: Psycho-education/Mapping, Functional behavior assessment and intervention, cognitive & behavioral strategies, ERP & positive reinforcement, parent training |
All between-group and within-group com parisons revealed medium to large effect sizes, significantly greater reduction be tween pre- and post-treatment in OCD symptoms in Fb-CBT vs TAU *No significant changes in gains at 5 month follow-up |
| Wolters et al. (2016) The Netherlands | RCT Waitlist (n = 24) vs Randomized to CBT (n = 19) vs Not-randomized to CBT (n = 17) |
58 children (8–18 years) Waitlist mean age: 13 Randomized to CBT mean age: 11.9 Not-randomized to CBT mean age: 13.6 Severe OCD ASD |
Number of sessions: pre- andmid-CBT: 8 sessions, post-CBT: 16 sessions Session duration: 45–60 min. Techniques: psycho-education, mapping OCD, ERP, cognitive interventions and relapse prevention |
Neither baseline severity nor autistic symptoms were predictive of treatment effect, significant differences between waitlist and CBT conditions in terms of symptom reduction *No significant changes in 1 year follow-up |
Participants
A total of 170 participants received CBT treatment across the eleven studies. The case study reports included 1–2 children who ranged in ages from 7 to 16 (Elliott and Fitzsimons 2014; Reaven and Hepburn 2003; Farrell et al. 2016). Out of the 44 participants in the case-controlled study by Murray et al. (2015), 22 were described as youth with ASD with a mean age of 15 years. In the randomized trial conducted by Russell et al. (2013), the participants included adults in addition to adolescents, ranging from 14 to 65 years of age. Of the 170 participants, 110 participants were male (65%) and 60 were female (35%). Out of the five case studies, only Reaven and Hepburn (2003) included a female participant and out of the two single-subject experimental designs, one of them (Vause et al. 2014) included both a male and a female participant.
The onset of OCD was not mentioned across studies, except in the case-controlled study (Murray et al. 2015), where it was specified as a mean age of 10 years for both experimental and control group and in a case study (Farrell et al. 2016), where it was given as three years prior to the introduction of the treatment (diagnosed at the age of 13 and treated at the age of 16). Similarly, the age of ASD diagnosis was not given across studies, except in a case study (Lehmkuhl et al. 2008), where it was specified as 2. Except the RCT study by Vause et al. (2015), the studies stated that a trained clinician verified the ASD diagnoses, completing a structured diagnostic instrument with participants, namely the Autism Diagnostic Observation Schedule (ADOS) (Lord et al. 1999), Autism Diagnostic Interview- Revised (ADI-R) (Lord et al. 1994) or both.
Of the 170 participants, 103 (65%) were diagnosed with OCD, 66 (39%) with ASD, and 1 (0.58%) with Asperger syndrome. Only 39 (23%) of 170 participants were provided with a specific ASD diagnosis; 10 (26%) were diagnosed with high-functioning autism, 22 (56%) with Asperger syndrome, and 7 (18%) with PDD-NOS. 109 participants (64%) were reported to have an ASD, but it was not specified which sub-diagnosis they had. In addition to ASD comorbidity, one participant in a case study (Farrell et al. 2016) had ADHD and in addition to OCD comorbidity, one participant in another case study (Nadeau et al. 2013) had social and specific phobia. Although these two case studies did not exclusively involve ASD and OCD, the treatment measures and procedure primarily focused on this dual psychopathology, warranting inclusion in the review. In studies reporting IQ of participants, the IQ ranged from borderline to gifted (Lehmkuhl et al. 2008; Nadeau et al. 2013; Neil et al. 2017; Reaven and Hepburn 2003; Russell et al. 2013; Vause et al. 2014, 2015; Wolters et al. 2016). Other studies described intellectual functioning as Bhaving at least average cognitive abilities “(Farrell et al. 2016), Babove average intelligence” (Elliott and Fitzsimons 2014) and one study failed to report on intellectual functioning (Murray et al. 2015).
CBT Treatment Variables
The sessions of CBT treatment ranged from 6 (Farrell et al. 2016) to 17.4 (mean CBT sessions in Vause et al. 2014) over a period of 9 (Neil et al. 2017) to 21 weeks (Nadeau et al. 2013) while the duration of sessions ranged from 35 min (Nadeau et al. 2013) to 2 h (Neil et al. 2017). With all studies, CBT treatment was implemented mainly in a clinic or a therapist's office. With the purpose of generalization, ERP sessions core to CBT treatment were also implemented in home (e.g., Farrell et al. 2016; Lehmkuhl et al. 2008; Reaven and Hepburn 2003) and school (e.g., Reaven and Hepburn 2003; Lehmkuhl et al. 2008) settings. In the case study by Farrell et al. (2016), in addition to clinic and home, CBT was implemented on a beach and in a park to maximize opportunities for ERP. Clinical psychologists or therapists, who were trained postdoctoral fellow or masters-level students and supervised by licensed providers, implemented the treatment sessions. Out of the eleven studies, seven of them included supervision of the therapists by the supervisor or clinical psychologists, who were trained within cognitive behavioral framework and had extensive experience in treating OCD in young people and adults.
In all studies, a multi-component CBT treatment was implemented. The components of CBT typically involved mapping, cognitive restructuring, fear hierarchy development, ERP, and relapse prevention. Two of the studies also included affective education or emotional literacy (Nadeau et al. 2013; Russell et al. 2013), which addressed identification of emotions based on facial and contextual clues. Although traditional elements of CBT treatment (e.g., March and Mulle 1998) were employed across studies, there were several modifications or enhancements to the standard treatment to address the social, emotional, and cognitive needs of participants with ASD. Table 2 summarizes the modifications that were used.
Table 2. Overview of treatment modifications from the most common to the least.
| Treatment Modifications | Elliott and Fitzsimons (2014) | Farrell et al. (2016) | Lehmkuhl et al. (2008) | Murray et al. (2015) | Nadeau et al. (2013) | Neil et al. (2017) | Reaven and Hepburn (2003) | Russell et al. (2013) | Vause et al. (2014) | Vause et al. (2015) | Wolters et al. (2016) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Parental involvement | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Increased use of visuals | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | N |
| Incorporation of child interests | Y | Y | N | N | Y | Y | Y | Y | Y | N | N |
| Personalized treatment metaphors & coping statements | Y | Y | Y | N | N | Y | Y | N | Y | Y | N |
| Self-monitoring | Y | Y | Y | N | N | Y | Y | Y | Y | N | N |
| Non-verbal and concrete examples | Y | N | N | N | Y | Y | N | N | Y | Y | N |
| Positive reinforcement | N | N | N | N | Y | Y | N | N | Y | Y | N |
| Explicit directions | Y | Y | N | N | Y | N | Y | N | N | N | N |
| Functional Behavioral Assessment & Intervention (FBAI) | N | N | N | N | N | Y | N | N | Y | Y | N |
| Narratives | N | Y | N | N | N | N | Y | N | N | N | N |
Y refers to “Yes, this treatment modification has been used in the referred study.” N refers to “No, this treatment modification has not been used in the referred study.”
Common modifications included parental involvement, visual aids to accommodate the non-verbal and concrete learning styles (e.g., weekly written schedule in Nadeau et al. 2013; Neil et al. 2017), incorporation of child interests, personalized treatment metaphors and coping statements (e.g., “Buzz off OC” in Vause et al. 2014; “Beat OCD and not let him be the boss” in Lehmkuhl et al. 2008), self-monitoring (e.g., behavior monitoring chart in Lehmkuhl et al. 2008; tracking logs in Reaven and Hepburn 2003), non-verbal and concrete examples, positive reinforcement, use of clear language and instructions, functional behavioral assessment, and narratives to increase social understanding. Parents were involved in all studies; some of the studies involved them in all phases of CBT (Farrell et al. 2016; Reaven and Hepburn 2003; Vause et al. 2014) while one of them involved them in a few phases only (e.g., psychoeducation, relapse prevention phases in Murray et al. 2015). Parent training and parent psychoeducation were also components of CBT treatment in two of the studies (Farrell et al. 2016; Vause et al. 2015). Parental involvement was not only clinic-based; parents were also responsible for doing homework in the home setting. These homework assignments were a component of CBT treatment to aid generalization of treatment gains, limit family accommodation (Lehmkuhl et al. 2008), and promote awareness of OCBs (Vause et al. 2015). Homework was an element of CBT treatment across all studies, except in a case study by Reaven and Hepburn (2003) and in the single subject experiment by Neil et al. (2017).
Modifications of CBT were not only contextual but also procedural. Two of the studies (Lehmkuhl et al. 2008; Wolters et al. 2016) started ERP sessions early (in the second or third session) due to the protracted cognitive component that diminished the participant(s)' ability to reflect on specific obsessions. Three studies included the use of functional behavioral assessment to identify the perceived functions of the compulsions and included assessment-based behavior intervention techniques (e.g., applied behavior analysis) and called this new treatment approach Fb-CBT (Neil et al. 2017; Vause et al. 2014, 2015). Fb-CBT included identification of potential functions of behaviors (i.e., social attention, escape from task, tangible, sensory/non-social) and appropriate techniques such as differential reinforcement of alternative behavior (DRA), planned ignoring, redirection (Vause et al. 2014), and positive reinforcement (i.e., verbal praise and tangibles such as tokens, stickers) (Neil et al. 2017; Vause et al. 2015).
Research Design
The literature review yielded five clinical case reports, two studies using a time series experimental design, and four group studies that ranged in experimental rigor from a design described as case-controlled (Murray et al. 2015) to the Randomized Controlled Trials (RCT) (Russell et al. 2013; Vause et al. 2015; Wolters et al. 2016). While the clinical case studies (Elliott and Fitzsimons 2014; Farrell et al. 2016; Lehmkuhl et al. 2008; Nadeau et al. 2013; Reaven and Hepburn 2003) offered data on the promising applications of an intervention and allow for an examination of the details of the intervention approach, they did not include design elements for external and internal validity or a determination of treatment efficacy.
In contrast, both single subject experimental designs (Neil et al. 2017; Vause et al. 2014) had high treatment fidelity as trained naïve observers completed treatment implementation checks via watching video recordings and reached 100% inter-observer agreement. Out of the four group studies, all included measures for ensuring treatment fidelity, except Murray et al. (2015), which acknowledged it as a limitation. In the RCT by Vause et al. (2015), therapists also collected observational probe data to check reliability on parent ratings of targeted behaviors and reached 86% agreement with parents' Likert-type scale ratings. In the RCT by Russell et al. (2013), evaluators blind to treatment conducted symptom ratings assessment prior to commencing treatment, at post-treatment, and at 1, 3, 6, and 12-month follow-up to identify if the treatment effects were random or due to clinical improvement. In the other RCT by Wolters et al. (2016), two naïve raters evaluated 25% of the session reports and reached 99% agreement. Of the four group studies, two had a control group (Murray et al. 2015; Russell et al. 2013) while the other two had a waitlist or treatment as usual (TAU) (Vause et al. 2015; Wolters et al. 2016).
Treatment Outcomes
Various measures were utilized to evaluate treatment effects across studies. The most common measures included the Children's Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) (Scahill et al. 1997), the Autism Diagnostic Interview-Revised (ADI-R) (Lord et al. 1994), self-generated ratings, parent OCB rating scale, and treatment satisfaction report. Some other measures included the Child Behavior Checklist (CBCL; Achenbach and Rescorla 2001), the Children's Global Assessment Scale (CGAS; Shaffer et al. 1983), the Repetitive Behavior Scale-Revised (RBS-R; Bodfish et al. 1999), and the Anxiety Disorder Interview Schedule for DSM-IV – Child and Parent Version (ADIS-C/P; Silverman and Albano 1996). Except in a case study by Elliott and Fitzsimons (2014), pre- and post-treatment assessments were conducted in all studies. Overall, there were significant reductions in OCD symptoms in scores of all checklists and in some, even decreases of OCBs to zero levels (Farrell et al. 2016; Nadeau et al. 2013; Neil et al. 2017), and high treatment satisfaction. In the case-controlled study, however, Murray et al. (2015) found that as compared to OCD + NoASD group, OCD + ASD group had a significantly smaller decrease in symptoms over treatment (38.31% vs. 48.20%) and lower remission rates at post treatment (9% vs. 46%). In addition, in the RCT by Russell et al. (2013), there were no statistically significant differences in treatment effects between CBT group and Anxiety Management group. Wolters et al. (2016) examined whether OCD severity and ASD symptoms were predictive of the effect of CBT treatment and found that neither baseline severity nor autistic symptoms were predictive.
Except for the Murray et al. (2015) study, all studies administered follow-up measures to identify it treatment gains were sustained. Follow-up measures were conducted in a varying period of time, ranging from 2 sessions (Elliott and Fitzsimons 2014) to 20 month (Neil et al. 2017). Across all studies, treatment gains were maintained with little to no changes except the single subject experimental design by Vause et al. (2014), where the OCD symptoms were reduced but resurfaced for the female participant due to some triggers. In Fb-CBT studies (Neil et al. 2017; Vause et al. 2014, 2015), functional behavioral assessment and parent training were the pivotal accompaniments of CBT, which resulted in near to zero level OCBs, high treatment satisfaction, and maintained treatment gains in as far as 20 month follow-up. Parental involvement was one of the major modifications incorporated across all studies; however, only five of the studies (Farrell et al. 2016; Nadeau et al. 2013; Neil et al. 2017; Vause et al. 2014, 2015) also included parent training within therapy or as a separate session, during which they learned about treatment protocols and had training on how to manage OCD demands.
Although ERP is the core phase of CBT treatment, there are a few other phases that are incorporated with varying degrees of intensity, including psychoeducation, cognitive restructuring, fear hierarchy development, and relapse prevention. A few of the studies (Elliott and Fitzsimons 2014; Farrell et al. 2016; Lehmkuhl et al. 2008; Reaven and Hepburn 2003) had a reduced focus on cognitive restructuring and an earlier introduction of ERP due to the participant(s)' difficulty in identifying and reflecting on specific obsessions. In terms of relative treatment effects of these phases, Vause et al. (2014, 2015) studies found that psychoeducation/mapping alone did not show a treatment effect; changes were observed only after ERP, functional behavioral assessment, and positive reinforcement were introduced.
Discussion
This review identified 11 studies that evaluated the effectiveness of CBT treatment for individuals with ASD and OCD. Overall, the small number of research reports with very few studies that demonstrate experimental control limits our ability to make conclusions about the efficacy of CBT for OCD in this population. However, all studies reported promising results with regard to effectiveness of the use of CBT when modified to meet the unique needs of the individuals with ASD and the review included two RCTs (Vause et al. 2015; Wolters et al. 2016) that provided rigorous evidence of the effectiveness of CBT for reducing the symptoms of OCD in individuals with ASD.
The modifications employed were not standard across the studies (see summary in Table 2). The most common ones included parental involvement, visual cues, incorporation of child interests, personalized metaphors and coping statements, and self-monitoring. Given the high comorbidity of ASD in individuals with OCD and vice versa, there is a pressing need to offer individuals with ASD and OCD effective treatment approaches. There is a need for additional rigorous research that can contribute to the development of an enhanced CBT protocol with modifications that would meet the individualized and idiosyncratic needs of individuals with ASD. This might eliminate the ambiguity around what modifications to employ in the intervention package and facilitate the intervention delivery both for the therapist and the participants.
All of the participants in this review were able to benefit from the CBT treatment; however, it is noteworthy that they all had high-functioning autism and IQ > 69. Vause et al. (2015) warranted their exclusion of individuals on the lower end of the spectrum suggesting that higher functioning individuals, who are verbally fluent and have an IQ > 69, may be at greater risk for having anxiety disorders, including OCD, in comparison to individuals who are lower functioning (Gadow et al. 2005; Gillott et al. 2001), whereas the other studies presented no rationale for the exclusion. Farrell et al. (2016) stated that although CBT treatment has growing support for treating OCD symptoms in the context of high-functioning autism, preliminary findings suggest that modified CBT may also be effective in reducing repetitive behaviors (RBs) in the context of ASD and co-occurring intellectual disability (Boyd et al. 2013). Thus, efforts for optimizing the efficacy of CBT treatment should be expanded to also address individuals with fewer verbal and cognitive skills.
Another prominent feature about the participants is that except in Russell et al. (2013) study, they were youth with ages ranging from 7 to 18 years. There might be a selection bias here due to the fact that youth population is relatively easier to recruit and work with and early intervention is acknowledged to be more efficacious. Future studies should seek to examine the effectiveness of CBT with the adult population since both ASD and OCD are pervasive disorders and affect the aging population in multiple domains.
Limitations
The findings of this literature review should be interpreted with reference to a number of limitations. First, since CBT treatment for individuals with only ASD and OCD is a relatively nascent field of inquiry, research on this field is scarce. For the sake of including as many research studies as possible, methodological rigor was not an exclusion criterion. In this review, we included studies that offered descriptive data (e.g., five case studies) and those with more rigorous designs with experimental control. Only two of the group studies (Murray et al. 2015; Russell et al. 2013) had comparison to an active treatment condition, while the others incorporated either a waitlist or TAU (Vause et al. 2015; Wolters et al. 2016). Second, there was a wide variation of techniques (i.e., behavioral, skills-based, cognitive) employed in CBT treatment across studies, which rendered the analysis of intervention delivery difficult. The heterogeneity across components of CBT and their delivery had a threat to internal validity, not allowing a conclusive finding with regard to what treatment modality was the most effective. Third, although studies that included pharmacological treatment were excluded from the review, in a few studies (Reaven and Hepburn 2003; Murray et al. 2015), medication was started during CBT treatment, which blurs the finding that observed improvements were the result of CBT alone. Finally, the outcome measures incorporated as pre/post-test in the reviewed studies included self-report and parent-report data. Self –report data had relatively poor reliability while parent-report data were susceptible to observer drift. Behavior scales or checklists rated by the participants or parents were not as rigorous as those rated by the therapists in terms of treatment fidelity.
Future Research and Practice
This review yielded 11 studies that examined the potential of CBT as an effective treatment approach for ASD and OCD. Given the number of individuals with ASD that are affected by comorbid OCD, there is a critical need to expand the research base of evidence-based practices that can provide effective treatments. There is also a need to examine the predictors of treatment effect. CBT studies to date have focused primarily on intervention delivery and treatment outcomes. While the nature and process of CBT are significant to determine the treatment efficacy, some other factors might also moderate or mediate treatment outcomes. Wolters et al. (2016) found that neither baseline OCD severity nor ASD symptoms were predictive of treatment effect. However, this finding alone is not sufficient to generalize. Future studies might also examine the predictors of remission and relapse. Almost all of the studies included follow-up data to reveal maintenance of gains over a period of time. Although all concluded that treatment gains were sustained, none of the studies described the factors that possibly helped remission. It could be hypothesized that lack of parental accommodation, continued affective education, homework compliance, and positive reinforcement might help remission and prevent relapse. Future research is needed to examine the validity of these factors and increase the sustainability of treatment gains.
Three of the studies (Neil et al. 2017; Vause et al. 2014, 2015) found that some of the treatment phases (e.g., ERP, Cognitive Training (CT), Functional Behavioral Assessment and Intervention (FBAI) were more effective than the others (e.g., psychoeducation and mapping). Although ERP has been reported as the active ingredient in reducing OCBs (Lehmkuhl et al. 2008; March and Mulle 1998), it is not known whether ERP alone would yield in the same results. Component analysis studies are needed to examine the relative efficacy of treatment phases so that, if applicable, more focus is placed on more effective phases to optimize treatment outcomes. Relatedly, future research should include the component of FBAI in the CBT treatment since emerging research supports the use of function-based components (Kuhn et al. 2009; Rodriguez et al. 2012). This innovation may help not only identify some other possible functions of OCBs such as social attention, access to a tangible item, escape from task, and automatic reinforcement (Feldman et al. 2002; Hanley et al. 2003) but also bring about a more comprehensive treatment protocol that may result in quicker treatment response and higher remission rates.
The studies we reviewed were varied in the types of intervention delivery methods, including group CBT, family CBT, and individual CBT. Only Neil et al. (2017) referred to the efficacy of individual CBT over group CBT. In future research, it will be important to examine the relationship between how intervention is delivered and the treatment outcomes. In addition, the outcome measures used in the studies were limited to measures of symptom severity. While changes in symptom severity are clearly the most important proximal outcomes for treatment, future studies might also examine measures related to lifestyle outcomes that might occur as symptoms are reduced. Those outcomes might include effects of treatment on social and communication skills, access to community activities, friendship development, and family quality of life.
Parental involvement was a core aspect of CBT treatment across the studies. In other pediatric applications of CBT for anxiety or OCD, the involvement of the family has led to more robust outcomes (Sofronoff et al. 2005; Storch et al. 2007). However, not all studies clearly explained the role of parents in intervention, nor did they examine it as a predictor of treatment success. Future research is needed to clarify how and evaluate to what extent parent involvement plays an active role in terms of the treatment success.
Conclusion
This is the first review to examine the existing studies on the efficacy of the CBT treatment for individuals with ASD and OCD only. The results suggest that participants clinically benefited from the interventions as indicated by reduced symptom severity scores on both self- and parent-report questionnaires and clinician-administered measures of OCBs. However, in order to meet the unique needs of the individuals and maximize treatment outcomes, CBT needs to be enhanced with modifications such as increased structure in the sessions, visual aids and cues, and considerable parental involvement. Given the high comorbidity of ASD and OCD, continued rigorous research on this promising approach for treatment is needed.
Acknowledgments
Funding: Preparation of this article was supported, in part, by funding from the National Institutes of Health. Treatment of Anxiety in Autism. 1R01HD080096-01A1.
Footnotes
Compliance with Ethical Standards: Ethical Approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent: No informed consent was required for this article.
Conflict of Interest: All authors declare that they have no conflict of interest.
References
- Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant assessment. Burlington: ASEBA; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text rev) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed) Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- Autism and Developmental Disabilities Monitoring Network Surveillance. Principal Investigators. Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR. 2010;63(2):1–21. 2014. [PubMed] [Google Scholar]
- Bird G, Cook R. Mixed emotions: The contribution of alexithymia to the emotional symptoms of autism. Translational Psychiatry. 2013;3(7):e285. doi: 10.1038/tp.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodfish JW, Symons F, Lewis M. The repetitive behavior scale: Test manual. Morganton: Western Carolina Center Research Reports; 1999. [Google Scholar]
- Boyd BA, Woodard CR, Bodfish JW. Feasibility of exposure response prevention to treat repetitive behaviors of children with autism and an intellectual disability: A brief report. Autism. 2013;17:196–204. doi: 10.1177/1362361311414066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlgren S, Sandberg AD, Hjelmquist E. The non-specificity of theory of mind deficits: Evidence from children with communicative disabilities. European Journal of Cognitive Psychology. 2003;15:129–155. doi: 10.1080/09541440303601. [DOI] [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: The early start Denver model. Pediatrics. 2010;125(1):e17–e23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott SJ, Fitzsimons L. Modified CBT for treatment of OCD in a 7-year-old boy with ASD—A case report. Journal of Child and Adolescent Psychiatric Nursing. 2014;27:156–159. doi: 10.1111/jcap.12081. [DOI] [PubMed] [Google Scholar]
- Farrell LJ, James SC, Maddox BB, Griffiths D, White S. Clinical Handbook of Obsessive-Compulsive and Related Disorders. Switzerland: Springer International Publishing; 2016. Treatment of comorbid obsessive-compulsive disorder in youth with ASD: The case of Max; pp. 337–355. [DOI] [Google Scholar]
- Feldman MA, Condillac RA, Tough S, Hunt S, Griffiths D. Effectiveness of community positive behavioral intervention for persons with developmental disabilities and severe behavior disorders. Behavior Therapy. 2002;33:377–398. doi: 10.1016/S0005-7894(02)80034-X. [DOI] [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162:151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Freeston MH, Ladouceur R. Exposure and response prevention for obsessive thoughts. Cognitive and Behavioral Practice. 1999;6:362–383. doi: 10.1016/S1077-7229(99)80056-X. [DOI] [Google Scholar]
- Gadow KD, Devincent CJ, Pomeroy J, Azizian A. Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism. 2005;9:392–415. doi: 10.1177/1362361305056079. [DOI] [PubMed] [Google Scholar]
- Gillott A, Furniss F, Walter A. Anxiety in high-functioning children with autism. Autism. 2001;5:277–286. doi: 10.1177/1362361301005003005. [DOI] [PubMed] [Google Scholar]
- Hanley GP, Iwata BA, McCord BE. Functional analysis of problem behavior: A review. Journal of Applied Behavior Analysis. 2003;36:147–185. doi: 10.1901/jaba.2003.36-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happé F, Frith U. The weak coherence account: Detail-focused cognitive style in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2006;36:5–25. doi: 10.1007/s10803-005-0039-0. [DOI] [PubMed] [Google Scholar]
- Joshi G, Petty C, Wozniak J, Henin A, Fried R, Galdo M, et al. The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: A large comparative study of a psychiatrically referred population. Journal of Autism and Developmental Disorders. 2010;40:1361–1370. doi: 10.1007/s10803-010-0996-9. [DOI] [PubMed] [Google Scholar]
- Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: A comparative study. Journal of Autism and Developmental Disorders. 2013;43:1314–1325. doi: 10.1007/s10803-012-1679-5. [DOI] [PubMed] [Google Scholar]
- Kasari C. Assessing change in early intervention programs for children with autism. Journal of Autism and Developmental Disorders. 2002;32:447–461. doi: 10.1023/A:1020546006971. [DOI] [PubMed] [Google Scholar]
- Kuhn DE, Hardesty SL, Sweeney NM. Assessment and treatment of excessive straightening and destructive behavior in an adolescent diagnosed with autism. Journal of Applied Behavior Analysis. 2009;42:355–360. doi: 10.1901/jaba.2009.42-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang R, Regester A, Lauderdale S, Ashbaugh K, Haring A. Treatment of anxiety in autism spectrum disorders using cognitive behaviour therapy: A systematic review. Developmental Neurorehabilitation. 2010;13:53–63. doi: 10.3109/17518420903236288. [DOI] [PubMed] [Google Scholar]
- Lehmkuhl HD, Storch EA, Bodfish JW, Geffken GR. Brief report: Exposure and response prevention for obsessive compulsive disorder in a 12-year-old with autism. Journal of Autism and Developmental Disorders. 2008;38:977–981. doi: 10.1007/s10803-007-0457-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S. Autism diagnostic observation schedule (ADOS) manual. Los Angeles: Western Psychological Services; 1999. [Google Scholar]
- March JS, Mulle K. OCD in children and adolescents: A cognitive-behavioral treatment manual. New York: Guilford Press; 1998. [Google Scholar]
- March JS, Franklin M, Nelson A, Foa E. Cognitive-behavioral psychotherapy for pediatric obsessive-compulsive disorder. Journal of Clinical Child Psychology. 2001;30:8–18. doi: 10.1207/S15374424JCCP3001_3. [DOI] [PubMed] [Google Scholar]
- Matson JL, Nebel-Schwalm MS. Comorbid psychopathology with autism spectrum disorder in children: An overview. Research in Developmental Disabilities. 2007;28:341–352. doi: 10.1016/j.ridd.2005.12.004. [DOI] [PubMed] [Google Scholar]
- McGuire JF, Piacentini J, Lewin AB, Brennan EA, Murphy TK, Storch EA. A meta-analysis of cognitive behavior therapy and medication for child obsessive-compulsive disorder: Moderators of treatment efficacy, response, and remission. Depression and Anxiety. 2015;32:580–593. doi: 10.1002/da.22389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier SM, Petersen L, Schendel DE, Mattheisen M, Mortensen PB, Mors O. Obsessive-compulsive disorder and autism Spectrum disorders: Longitudinal and offspring risk. PloS One. 2015;10:1–12. doi: 10.1371/journal.pone.0141703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray K, Jassi A, Mataix-Cols D, Barrow F, Krebs G. Outcomes of cognitive behavior therapy for obsessive–compulsive disorder in young people with and without autism spectrum disorders: A case controlled study. Psychiatry Research. 2015;228:8–13. doi: 10.1016/j.psychres.2015.03.012. [DOI] [PubMed] [Google Scholar]
- Nadeau JM, Arnold EB, Storch EA, Lewin AB. Family cognitive-behavioral treatment for a child with autism and comorbid obsessive compulsive disorder. Clinical Case Studies. 2013;13:22–36. doi: 10.1177/1534650113504488. [DOI] [Google Scholar]
- Neil N, Sturmey P. Assessment and treatment of obsessions and compulsions in individuals with autism spectrum disorders: A systematic review. Review Journal of Autism and Developmental Disorders. 2014;1:62–79. doi: 10.1007/s40489-013-0006-1. [DOI] [Google Scholar]
- Neil N, Vause T, Yates H, Feldman M. Effects of group functional behavior-based cognitive behavioral therapy for obsessive-compulsive behavior in a youth with autism spectrum disorder. Journal of Child and Family Behavior Therapy. 2017 doi: 10.1007/s10803-018-3772-x. in press. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Langley AK. Cognitive-behavioral therapy for children who have obsessive-compulsive disorder. Journal of Clinical Psychology. 2004;60:1181–1194. doi: 10.1002/jclp.20082. [DOI] [PubMed] [Google Scholar]
- Ponniah K, Magiati I, Hollon SD. An update on the efficacy of psychological treatments for obsessive–compulsive disorder in adults. Journal of Obsessive-compulsive and Related Disorders. 2013;2:207–218. doi: 10.1016/j.jocrd.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaven J, Hepburn S. Cognitive-behavioral treatment of obsessive-compulsive disorder in a child with Asperger syndrome a case report. Autism. 2003;7:145–164. doi: 10.1177/1362361303007002003. [DOI] [PubMed] [Google Scholar]
- Reaven JA, Blakeley-Smith A, Nichols S, Dasari M, Flanigan E, Hepburn S. Cognitive-behavioral group treatment for anxiety symptoms in children with high-functioning autism spectrum disorders a pilot study. Focus on Autism and Other Developmental Disabilities. 2009;24:27–37. doi: 10.1177/1088357608327666. [DOI] [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K, Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: A randomized trial. Journal of Child Psychology and Psychiatry. 2012;53:410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez NM, Thompson RH, Schlichenmeyer K, Stocco CS. Functional analysis and treatment of arranging and ordering by individuals with an autism spectrum disorder. Journal of Applied Behavior Analysis. 2012;45:1–22. doi: 10.1901/jaba.2012.45-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell AJ, Jassi A, Fullana MA, Mack H, Johnston K, Heyman I, Mataix-Cols D. Cognitive behavior therapy for comorbid obsessive-compulsive disorder in high-functioning autism Spectrum disorders: A randomized controlled trial. Depression and Anxiety. 2013;30:697–708. doi: 10.1002/da.22053. [DOI] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, et al. Children's Yale-Brown obsessive compulsive scale: Reliability and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Scattone D, Mong M. Cognitive behavior therapy in the treatment of anxiety for adolescents and adults with autism spectrum disorders. Psychology in the Schools. 2013;50:923–935. doi: 10.1002/pits.21717. [DOI] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A children's global assessment scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety disorders interview schedule for DSM-IV: Child interview schedule. San Antonio: Graywind Publications; 1996. [Google Scholar]
- Simpson HB, Foa EB, Liebowitz MR, Ledley DR, Huppert JD, Cahill S, et al. A randomized, controlled trial of cognitive-behavioral therapy for augmenting pharma-cotherapy in obsessive-compulsive disorder. American Journal of Psychiatry. 2008;165:621–630. doi: 10.1176/appi.ajp.2007.07091440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. A randomized controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry. 2005;46:1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Mann G, Duke D, Munson M, et al. Family-based cognitive behavioral therapy for pediatric obsessive-compulsive disorder: Comparison of intensive and weekly approaches. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:469–478. doi: 10.1097/chi.0b013e31803062e7. [DOI] [PubMed] [Google Scholar]
- Storch EA, Arnold EB, Lewin AB, Nadeau JM, Jones AM, De Nadai AS, et al. The effect of cognitive-behavioral therapy versus treatment as usual for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:132–142. doi: 10.1016/j.jaac.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Storch EA, Lewin AB, Collier AB, Arnold E, De Nadai AS, Dane BF, et al. A randomized controlled trial of cognitive-behavioral therapy versus treatment as usual for adolescents with autism spectrum disorders and comorbid anxiety. Depression and Anxiety. 2015;32:174–181. doi: 10.1002/da.22332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsakanikos E, Costello H, Holt G, Bouras N, Sturmey P, Newton T. Psychopathology in adults with autism and intellectual disability. Journal of Autism and Developmental Disorders. 2006;36:1123–1129. doi: 10.1007/s10803-006-0149-3. [DOI] [PubMed] [Google Scholar]
- Vause T, Hoekstra S, Feldman M. Evaluation of individual function-based cognitive-behavioural therapy for obsessive compulsive behaviour in children with autism spectrum disorder. Journal on Developmental Disabilities. 2014;20(3):30–41. [Google Scholar]
- Vause T, Neil N, Jaksic H, Jackiewicz G, Feldman M. Preliminary randomized trial of function-based cognitive-behavioral therapy to treat obsessive compulsive behavior in children with autism spectrum disorder. Focus on Autism and Other Developmental Disabilities. 2015:1–11. doi: 10.1177/1088357615588517. [DOI] [PubMed] [Google Scholar]
- White SW, Ollendick T, Scahill L, Oswald D, Albano AM. Preliminary efficacy of a cognitive-behavioral treatment program for anxious youth with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009a;39:1652–1662. doi: 10.1007/s10803-009-0801-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009b;29:216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Albano AM, Johnson CR, Kasari C, Ollendick T, Klin A, et al. Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism. Clinical Child and Family Psychology Review. 2010;13:77–90. doi: 10.1007/s10567-009-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolters LH, de Haan E, Hogendoorn SM, Boer F, Prins PJ. Severe pediatric obsessive compulsive disorder and co-morbid autistic symptoms: Effectiveness of cognitive behavioral therapy. Journal of Obsessive-Compulsive and Related Disorders. 2016;10:69–77. doi: 10.1016/j.jocrd.2016.06.002. [DOI] [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of Child Psychology and Psychiatry. 2009;50:224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Ehrenreich-May J, Alessandri M, Fujii C, Renno P, Laugeson E, et al. Cognitive behavioral therapy for early adolescents with autism spectrum disorders and clinical anxiety: A randomized, controlled trial. Behavior Therapy. 2015;46:7–19. doi: 10.1016/j.beth.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]