Abstract
Recent research has shown that concern about the apprehension and deportation of undocumented immigrants can affect how members of their households who are eligible for public benefits choose to participate in public programs. The extent to which this “chilling effect” broadly affects adults’ Medicaid enrollment nationally remains unclear, in part because of the difficulty of isolating undocumented immigrants in survey data. In this study we identified households that likely included undocumented immigrants and then examined whether gains in health care coverage due to the expansion of Medicaid eligibility under the Affordable Care Act (ACA) were dampened for eligible people living in households with mixed immigration status. We found no significant differences in coverage gains for people in mixed-relative to non-mixed-status households in expansion states. Coverage gains were significantly lower, however, for people in mixed-status households relative to those in non-mixed-status households in nonexpansion states. These findings suggest that household immigration status may have dampened the “woodwork effect,” whereby the ACA enhanced knowledge about program availability, in turn increasing Medicaid enrollment in nonexpansion states among people previously eligible for the program but not enrolled in it.
Background
In 2016, approximately 25 percent of the uninsured in the United States—6.7 million people—were eligible for, but not enrolled in, the Medicaid program.1 There are many reasons why people might not participate, despite being eligible: Enrollment may be impeded by disability, the length and complexity of the application process, logistical barriers, or stigma.2–6
The presence of a noncitizen in a household can also affect willingness to participate in Medicaid. A number of studies have found that Medicaid-eligible citizen children of noncitizens are significantly less likely to enroll in Medicaid, relative to similar children of citizens.7 These differences increase in the face of enhanced enforcement of immigration laws.8 In particular, immigration enforcement was found to be responsible for three-quarters of the 4.4-percentage-point drop in Medicaid enrollment evident for children of noncitizens during the period 1993–2000.9 In this context, enforcement of immigration laws “chills” Medicaid enrollment for otherwise eligible children who live in families with noncitizen parents, given the fear that applying for public benefits may expose a household to scrutiny from immigration law enforcement agencies.
In 2013, Immigration and Customs Enforcement (ICE) issued a memo clarifying that any information collected during the application process for Medicaid and the subsidized state insurance Marketplace coverage established by the Affordable Care Act (ACA) would be used only for determining eligibility and ensuring the efficient operation of the programs.10 The memo indicated that no personal details would be shared with ICE authorities for the purpose of immigration enforcement actions against either the applicant or members of their household.10 These assurances may have lessened concerns for some people who had been debating whether to obtain coverage and who lived in households that included undocumented immigrants. Nonetheless, such memos may be limited in their ability to dispel fear and alter enrollment behavior, depending on the extent to which people trust such governmental assertions; believe there is congruency among the federal, state, and local policy environments; and expect policies to be changed in the future.
The extent to which “chilling effects” broadly affect Medicaid enrollment nationally among adults remains unclear, in part because of the difficulty of specifically identifying undocumented immigrants—as opposed to noncitizens, who may be lawfully present— in survey data. In our analysis we identified households in survey data that likely included a person with undocumented immigration status. We then leveraged the expansion of Medicaid eligibility under the ACA as a quasi-experimental opportunity to test whether changes in coverage were associated with differential effects for otherwise eligible adults in households with at least one undocumented immigrant (households with mixed status), compared with adults in households with no undocumented immigrants (households without mixed status).
Study Data And Methods
Data Sources
Data on individuals came from the 2009–15 American Community Survey (ACS), as compiled in the University of Minnesota’s Integrated Public Use Microdata Series.11 The ACS is administered by the Census Bureau to residents of approximately 3.5 million housing units and group quarters each year, allowing for representative annual estimates of sociodemographic characteristics, health care coverage, migration, and other population features for all fifty states and the District of Columbia. We indicated that a respondent was enrolled in Medicaid if they answered affirmatively that they had “Medicaid, Medical Assistance, or any kind of government-assistance plan for those with low incomes or a disability.”12 We relied on data from the Henry J. Kaiser Family Foundation to identify when states implemented expansion of Medicaid eligibility under the ACA.13
Study Population
We limited our study sample to the low-income population most likely to be affected by the ACA Medicaid expansion. Thus, we excluded those ages eighteen and younger (who were generally eligible for Medicaid before the ACA if in low-income families) and those older than age sixty-four (who were usually eligible for Medicare). Given that our analysis required observing whether an ACS respondent lived with an undocumented person, we further restricted our sample to people with at least one other person in their household. The sample was also restricted to people with at least five years of residence in the United States whose health insurance unit income was less than or equal to 138 percent of the federal poverty level—the Medicaid eligibility threshold established by the ACA. We relied on the health insurance unit—rather than the family or household—as the unit of analysis to calculate income as a percentage of the poverty level to ensure that family composition closely mirrored that used by both public and private insurers for determination of eligibility. The health insurance unit is narrower than the Census Bureau definition of family or household and accounts for the dependent relationships that are considered in the context of insurance eligibility determinations. Additional details on the methodologies used to define ACS respondents’ health insurance units are available elsewhere.14,15
We identified mixed- and non-mixed-status households by first determining whether an ACS respondent was likely an undocumented immigrant using a “residual” methodology developed by George Borjas and used in previous work to estimate labor-force participation by undocumented workers: Mixed-status households included at least one likely undocumented respondent, whereas non-mixed-status households did not.16,17 Using this approach, we first classified foreign-born survey respondents as lawful immigrants if any one of several conditions held. For example, immigrants were deemed lawful if they had served in the military, worked in a field requiring occupational licensing, or received Supplemental Security Income (for the full set of criteria, see the online appendix).18 The residual of the population—all other foreign-born respondents— were deemed likely to have undocumented immigration status. This residual methodology, unlike some alternative approaches, was highly parsimonious and replicable because of its avoidance of cross-survey multiple imputation and reweighting.19 All of our analyses were restricted to people deemed likely to have legal residence in the United States and who were otherwise eligible for Medicaid, as indicated in their ACS responses.
Statistical Analysis
To examine whether living in a mixed-status household was associated with differential receipt of Medicaid coverage, we first conducted a triple-differences analysis: We compared the proportion of eligible people with Medicaid, before and after expansion of Medicaid eligibility, in states that expanded Medicaid eligibility relative to those that did not, for people living in mixed-status households relative to those living in non-mixed-status households. We used this approach to control for a number of unobserved trends in the receipt of Medicaid coverage that could bias estimates of coverage changes. It thus allowed for more credible analysis of the causal effect of living in a mixed-status household.
Second, given evidence that there were substantial gains in Medicaid coverage in nonexpansion states after implementation of the ACA—the so-called woodwork effect—we also conducted a trend analysis in which we compared trends in Medicaid coverage in nonexpansion states for eligible people in mixed- and non-mixed-status households before and after 2014, when most expansion states elected to implement their expansions of Medicaid eligibility.20
All analyses were conducted using linear probability models with survey weights and a robust set of individual-level controls, including sex, age, education, race/ethnicity (white, black, Hispanic, and other), health insurance unit income as a percentage of the poverty level, marital status, employment status, number of adults, number of children, whether the respondent primarily spoke Spanish, and whether the respondent had self-care difficulties. Models also included fixed effects for state and year, and standard errors were clustered at the state level. We conducted secondary analyses in which we limited the sample to lawfully present immigrants (noncitizens likely residing in the United States legally), given our hypothesis that those people would be particularly susceptible to “chilling effects” because they did not have the additional legal protections of citizenship.
To determine the validity of our comparison groups and robustness of our results, we conducted a common trends test for the triple-differences analysis, comparing trends in our outcome of interest before implementation of the primary ACA insurance provisions in 2014 (appendix exhibit A1).18 We also repeated the primary Medicaid analysis after excluding four states that expanded Medicaid eligibility before the implementation of the ACA (appendix exhibit A2).18
An Institutional Review Board at Yale University deemed this study exempt from review. For additional details on the statistical analysis, see the appendix.18
Limitations
This study had several important limitations. First, our ability to identify mixed-status households using survey data was imperfect: While the residual methodology allowed us to determine with a high likelihood that a given ACS respondent was undocumented, we could not do so with certainty. The Borjas algorithm we used is similar to residual methodologies developed by the Department of Homeland Security and by Robert Warren and Jeffrey Passel to estimate the size of the undocumented population. Prior work has demonstrated that these residual approaches yield estimates of immigration status that closely mirror those based on self-reported survey data.21,22 While Homeland Security adjusts its estimates to account for an assumed 10 percent undercount of the undocumented population, and the Warren-Passel approach relies on probabilistic modeling to match the department’s estimates, the Borjas algorithm we used here is implemented at the individual level and does not rely on reweighting. On average over the study period, our annual estimates of the undocumented proportion of the US population using the Borjas algorithm were within 0.3 percentage points of official estimates published by the Department of Homeland Security and the Pew Research Center23(appendix exhibit A3).18 Using the 2012-13 pooled Annual Social and Economic Supplement files from the Current Population Survey, Pew has estimated that approximately 5.4 percent of people ages 20–64 in the United States were undocumented; our analysis using the ACS data yielded an estimate of 5.49 percent.17 The two estimates differed by approximately 170,000 people. Importantly, our approach and the information available in the ACS did not allow us to distinguish between a person gaining temporary relief from deportation granted by the Deferred Action for Childhood Arrivals (DACA) program and one who was likely undocumented. However, individuals in either category would have been excluded from our analysis given our sample restrictions.
Second, the analysis of trends in Medicaid coverage in nonexpansion states lacked a relevant control group. While all analyses included a robust set of individual-level control variables, this examination of the association between household immigration status and insurance coverage could be biased by the presence of other contemporaneous changes in the policy environment that remained unaddressed in model specifications. For example, changes occurring within state Medicaid program enrollment and renewal regulations might not be completely captured by our use of state fixed effects, though we found that many of these policies were stable within states over the study period.24
Third, given limitations in the wording of the ACS questionnaire, respondents coded as receiving Medicaid may have alternatively received “Medical Assistance” or other “government-assistance” coverage. As a result, a small number of respondents who received government-subsidized coverage via the state insurance Marketplaces may thus have been included in this study as receiving Medicaid.25 In all cases, we attempted to limit our analysis to the population of adults most likely to be eligible for and affected by Medicaid expansion: respondents ages 18–64 with at least five years of residence in the United States with a health insurance unit income of 138 percent of poverty or lower.
Fourth, while our health insurance unit was similar to the tax-filing unit used for determination of Medicaid eligibility, it might not perfectly capture the relevant household structure in all cases. In addition, although health insurance unit income as a percentage of the poverty level broadly reflects a tax-filing unit’s modified adjusted gross income—the income figure used in determining eligibility for Medicaid—we could not calculate this number precisely because of insufficient information in the ACS on payments and income sources.
Study Results
In both expansion and nonexpansion states, low-income people living in mixed-status households were more likely to be Hispanic, Spanish speakers, and noncitizens, compared to people living in households that were non-mixed status (exhibit 1). People in mixed-status households also had lower educational attainment: In expansion states, for example, 71.7 percent of Medicaid-eligible people in mixed-status households had completed at least high school, compared with 84.6 percent of those in non-mixed-status households.
Exhibit 1.
Characteristics of the study population
| Nonexpansion states | Expansion states | |||
|---|---|---|---|---|
| Non-mixed-status households (n = 1,067,281) |
Mixed-status households (n = 24,256) |
Non-mixed-status households (n = 1,503,683) |
Mixed-status households (n = 60,321) |
|
| Female | 54.8% | 53.5% | 53.6% | 55.0% |
| Age range (years) | ||||
| Younger than 25 | 36.7% | 45.9% | 38.7% | 44.0% |
| 25–50 | 45.0 | 40.8 | 43.6 | 40.6 |
| 50–64 | 18.3 | 13.3 | 17.6 | 15.4 |
| Race/ethnicity | ||||
| Black | 25.1% | 11.0% | 14.6% | 5.8% |
| Hispanic | 15.1 | 64.7 | 19.7 | 66.2 |
| Spanish speaker | 12.1 | 63.1 | 14.6 | 63.5 |
| Noncitizen | 3.0 | 20.3 | 5.0 | 28.0 |
| Education | ||||
| Less than high school | 16.9% | 27.4% | 15.4% | 28.3% |
| High school graduate | 45.5 | 37.9 | 43.4 | 36.3 |
| At least some college | 28.8 | 26.3 | 29.9 | 26.1 |
| College or more | 8.8 | 8.4 | 11.3 | 9.3 |
| Mean number in HIU of: | ||||
| Adults | 1.2 | 1.2 | 1.2 | 1.2 |
| Children | 0.7 | 0.7 | 0.6 | 0.6 |
| Mean HIU income as percentage of FPL | 58.4 | 57.0 | 56.9 | 54.3 |
| Married | 24.3% | 28.5% | 22.5% | 26.9% |
| Employed | 45.1% | 52.0% | 44.1% | 47.8% |
| Difficulty with self-care | 3.7% | 1.8% | 3.4% | 1.9% |
| Medicaida | 23.2% | 17.8% | 34.7% | 36.1% |
SOURCE Authors’ analysis of data for 2009–15 from the American Community Survey and the Henry J. Kaiser Family Foundation. NOTES The sample included survey respondents ages 18–64 with health insurance unit income less than or equal to 138 percent of the federal poverty level, at least five years of residence in the United States, and at least one other person in their household. Mixed-status households are those in which at least one member was determined to likely have undocumented immigration status. Expansion states are those that expanded eligibility for Medicaid. HIU is respondent’s health insurance unit. FPL is federal poverty level.
Respondents who indicated receiving “Medicaid, Medical Assistance, or any kind of government-assistance plan for those with low incomes or a disability.”
In the period 2009–15, the proportion of people in expansion states with Medicaid coverage was similar whether those people were in mixed- or non-mixed-status households, and the proportions for both types of households increased in 2014 with the implementation of relevant provisions of the ACA (exhibit 2). In 2009, 33.1 percent (95% confidence interval: 31.8, 34.5) of low-income people in mixed-status households living in expansion states were enrolled in Medicaid, compared with 30.3 percent (95% CI: 30.0, 30.5) of people in non-mixed-status households. In 2015, these proportions had increased to 46.3 percent (95% CI: 45.1, 47.6) and 45.7 percent (95% CI: 45.4, 45.9), respectively.
Exhibit 2. Percentages of people with Medicaid coverage, by state Medicaid expansion and household immigration status, 2009–15.
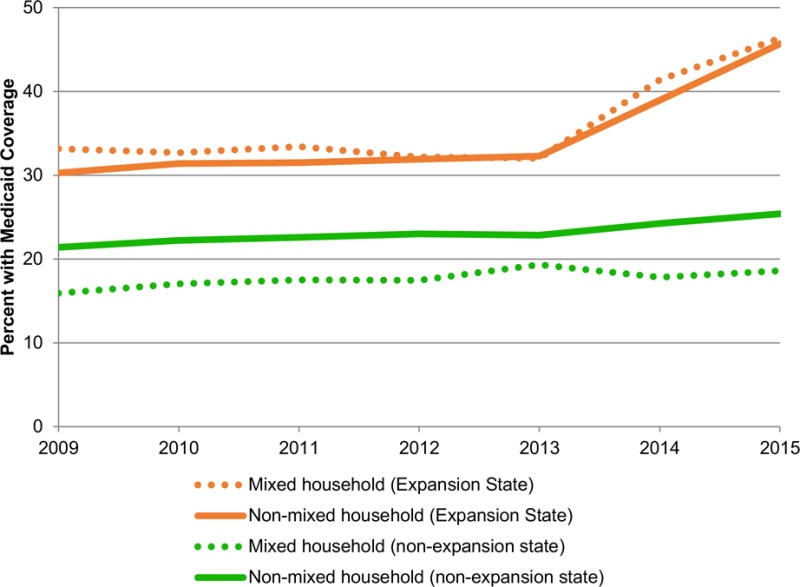
SOURCE Authors’ analysis of data for 2009–15 from the American Community Survey and the Henry J. Kaiser Family Foundation. NOTES The sample, mixed-status households, expansion states, and Medicaid coverage are defined in the notes to exhibit 1.
In comparison, people in nonexpansion states in mixed-status households were significantly less likely to be enrolled in Medicaid than those in non-mixed-status households across all years in the study period (exhibit 2). For example, in 2009, 15.9 percent (95% CI: 14.3, 17.5) of people in mixed-status households were enrolled in Medicaid, compared with 21.4 percent (95% CI: 21.1, 21.7) of those in non-mixed-status households.
The triple-differences analysis indicated that state expansions of Medicaid eligibility under the ACA were not associated with significant changes in Medicaid coverage for people in mixed-status households, relative to those in non-mixed-status households: During 2014–15, Medicaid expansion was associated with a nonsignificant 1.7-percentage-point differential change in Medicaid coverage (exhibit 3, model 1). In nonexpansion states, however, the trend analysis demonstrated that the 2014 change in Medicaid enrollment for people in mixed-status households was 1.7 percentage points (95% CI: −2.87, −0.42) less than it was for people in non-mixed-status households—a significant differential change that increased to 3.1 percentage points (95% CI: −4.10, −1.99) in 2015 (exhibit 3, model 2, and appendix exhibit A4).17 In all analyses, Medicaid expansion was not associated with significant changes in coverage for people in mixed- relative to those in non-mixed-status households when the samples were restricted to lawfully present immigrants. While the magnitude of the potential “chilling effect” became larger in the analysis for nonexpansion states restricted to lawfully present immigrants, the smaller sample size inflated confidence intervals to such a degree that we were unable to rule out the possibility of no effect.
Exhibit 3.
Relationship between state Medicaid expansion status and respondent Medicaid coverage, by household immigration status, 2009–15
| Full sample | Lawfully present immigrants | |||
|---|---|---|---|---|
| Change | 95% CI | Change | 95% CI | |
| Model 1 | ||||
| 2014–15 | 1.69 | [−0.10, 3.49] | −0.37 | [−5.37, 4.62] |
| 2014 | 1.34 | [−0.35, 3.03] | −0.70 | [−7.52, 6.13] |
| 2015 | 2.09 | [−0.65, 4.83] | 0.22 | [−4.41, 4.86] |
| Model 2 | ||||
| 2014 | −1.65** | [−2.87, -0.42] | −5.23 | [−11.84, 1.38] |
| 2015 | −3.05**** | [−4.10, -1.99] | −5.75* | [−11.73, 0.22] |
SOURCE Authors’ analysis of data for 2009–15 from the American Community Survey and the Henry J. Kaiser Family Foundation. NOTES The sample, mixed-status households, and Medicaid coverage are defined in the notes to exhibit 1. The lawfully present immigrant sample was further restricted to survey respondents who indicated they were noncitizens, but who were unlikely to be undocumented. In model 1, changes are percentage-point differences in the proportion of respondents with Medicaid coverage before and after expansion of eligibility for Medicaid, in expansion states relative to nonexpansion states, for people in mixed-status households relative to those in non-mixed-status households. In model 2, changes are percentage-point differences in the proportion of respondents in nonexpansion states with Medicaid coverage before and after expansion of Medicaid eligibility, for people in mixed-status households relative to those in non-mixed-status households. All analyses were conducted using linear probability models with survey weights and controls; details are in the text. CI is confidence interval.
p<0.10
p < 0.05
p < 0.01
p < 0.001.
Discussion
In states that expanded Medicaid eligibility under the ACA, we found that people in mixed-status households experienced increases in Medicaid enrollment that were statistically indistinguishable from the increases experienced by people in non-mixed-status households. Medicaid coverage gains for people in mixed- versus those in non-mixed-status households, however, were significantly different in nonexpansion states.
To apply for Medicaid, people must provide detailed data on household composition and income. When using the HealthCare.gov website to obtain coverage, for example, people may in some cases be prompted to provide the Social Security numbers and incomes of nonapplicant household members.26 People living in households that include undocumented immigrants might be concerned about providing this information for several reasons.27 First, if a nonapplicant family member does not have a Social Security number, an applicant may be worried that leaving the field blank (even when the number is not required) could implicitly signal undocumented immigration status. Second, otherwise eligible applicants could be hesitant to continue with the application process if they are aware that they are providing questionable personal information for a family member: While many undocumented people do have a Social Security number (often to pay taxes on wages), evidence suggests that as many as 1.8 million of those numbers may be fake or stolen.28 In both scenarios, people may be concerned that applying for coverage could have legal implications or expose family members to action by immigration enforcement agencies. It is worth noting that such fears are not entirely unwarranted: In North Carolina, for example, medical records at a county health department were used to help prosecute an undocumented person who had used a stolen Social Security number to obtain work.29
Evidence of “chilling effects” on Medicaid enrollment for a specific set of states highlights the important role of the policy context in mediating take-up of public benefits. Governments in nonexpansion states were broadly more likely to take legislative actions that enhanced enforcement of immigration laws, restricted immigrant access to public services, or placed additional administrative burdens on immigrants applying for public benefits, as reflected in scores on the Immigrant Climate Index30 (a database of city, county, and state regulations started in 2005 that ranks the regulations’ impact on immigrants). Our findings for nonexpansion states may be partially attributable to the history of these legislative actions, where concerns about sharing information with government entities could be amplified for people eligible for Medicaid and living in mixed-status households. People in such households in these states may also face greater difficulties accessing useful information on Medicaid eligibility or enrollment procedures, relative to people in non-mixed-status households. Given evidence that insurance enrollment increases access to health care services, reduces out-of-pocket spending, and improves self-reported health, depressed take-up of public health insurance among a subset of otherwise eligible people may introduce disparities in health outcomes and dampen labor-market productivity.31–33
Evidence that Medicaid expansion did not result in differential coverage gains for people in mixed-status households in expansion states may be related to the history of enrollment efforts in those states. Genevieve Kenney and coauthors found that Medicaid participation rates among eligible parents were significantly higher in almost all expansion states relative to nonexpansion states.34 It could be that these states, in addition to having more immigrant-friendly climates, are also more effective at ensuring take-up of insurance for everyone.
A 2012 report by the Office of the Assistant Secretary for Planning and Evaluation in the Department of Health and Human Services highlighted the many barriers faced by immigrants in accessing public services.27 While these obstacles are greater for noncitizens, particularly undocumented ones, they may also affect households of undocumented people as a whole. Common barriers included the complexity of the application process and eligibility rules; confusion about application requirements, including the need for proof of citizenship and Social Security numbers; and lack of access to supporting documentation. Language was deemed to be a particularly significant barrier, with many program administrators identifying a need for additional bilingual staff members and informational materials. The researchers found that “fears of mistreatment and deportation” consistently affected the likelihood of public program enrollment, with people concerned that application efforts would expose undocumented family members to immigration enforcement proceedings or would qualify them as “public charges,” a Department of Justice designation that could disqualify them from being eligible for improved immigration status. These concerns were heightened in states with more aggressive enforcement of immigration laws or with articles in the press that articulated a more explicit anti-immigrant sentiment.27 In some states, for example, local law enforcement directly participated in federal immigration enforcement efforts, including the implementation of biometric scanning to confirm identification and immigration status in local jail systems.27
These barriers suggest that some of the evidence of differential coverage gains for people in mixed- versus non-mixed-status households may be attributable to the local immigrant climate, information clarity and availability, or both. Local, state, and federal policy makers can likely improve the take-up of public health insurance among eligible people in mixed-status households by more explicitly communicating whether immigration status information provided in the application for Medicaid would be transmitted to and shared with federal authorities. Additional investment in bilingual assisters and informational materials and outreach to trusted community organizations such as churches have been identified as promising interventions for boosting enrollment among these populations.35,36 It remains unclear, however, to what extent enhanced investment in informational efforts may fully counter any “chilling effects” arising from environments in which immigration laws are more aggressively enforced, or where the climate is less welcoming to noncitizens. Additional research is needed, particularly in light of significant changes in the immigration policy environment in 2017–18.37
Conclusion
The ACA’s expansion of Medicaid eligibility broadly increased coverage for people living in households both with and without members whose immigration status is undocumented, but gains in Medicaid coverage were dampened among people in mixed-status households in states that did not elect to expand Medicaid eligibility. This finding provides suggestive evidence that immigration status dampened the woodwork effect, whereby state Medicaid expansions increased enrollment in nonexpansion states among people otherwise eligible for, but previously not enrolled in, Medicaid. Additional investment in targeted information and outreach campaigns for eligible people in mixed-status households may be warranted, in part to clarify the relationship between public benefit application processes and the transmission of immigration status data to federal authorities.
Supplementary Material
Acknowledgments
The authors acknowledge support from the Agency for Healthcare Research and Quality to Yale University (Grant No. T32 HS017589). William Schpero also acknowledges support from the National Institute on Aging to the National Bureau of Economic Research (Grant No. T32 AG000186).
Footnotes
An earlier version of this article was presented at the AcademyHealth Annual Research Meeting, June 27, 2017, in New Orleans, Louisiana, as well as the Association for Public Policy Analysis and Management Fall Research Conference, November 2, 2017, in Chicago, Illinois.
Notes
- 1.Garfield R, Damico A, Foutz J, Cox C, Claxton G, Levitt L. Estimates of eligibility for ACA coverage among the uninsured in 2016 [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; [last updated 2017 Oct 25; cited 2018 Jan 8]. Available from: https://www.kff.org/uninsured/issue-brief/estimates-of-eligibility-for-aca-coverage-among-the-uninsured-in-2016-october-2017-update/ [Google Scholar]
- 2.Stuber JP, Maloy KA, Rosenbaum S, Jones KC. Beyond stigma: what barriers actually affect the decisions of low-income families to enroll in Medicaid? [Internet] Washington (DC): George Washington UniversitySchool of Public Health and Health Services; 2000. Jul, [cited 2018 Jan 8]. (Issue Brief). Available from: http://publichealth.gwu.edu/departments/healthpolicy/CHPR/downloads/beyond_stigma_no3.pdf. [Google Scholar]
- 3.Iezzoni LI, Killeen MB, O’Day BL. Rural residents with disabilities confront substantial barriers to obtaining primary care. Health Serv Res. 2006;41(4 Pt 1):1258–75. doi: 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stuber J, Kronebusch K. Stigma and other determinants of participation in TANF and Medicaid. J Policy Anal Manage. 2004;23(3):509–30. doi: 10.1002/pam.20024. [DOI] [PubMed] [Google Scholar]
- 5.Moffitt R. An economic model of welfare stigma. Am Econ Rev. 1983;73(5):1023–35. [Google Scholar]
- 6.Sommers B, Kronick R, Finegold K, Po R, Schwartz K, Glied S. Understanding participation rates in Medicaid: implications for the Affordable Care Act [Internet] Washington (DC): Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; 2012. Mar 16, [cited 2018 Jan 8]. (ASPE Issue Brief). Available from: https://aspe.hhs.gov/system/files/pdf/76411/ib.pdf. [Google Scholar]
- 7.Acevedo-Garcia D, Stone LC. State variation in health insurance coverage for U.S. citizen children of immigrants. Health Aff (Millwood) 2008;27(2):434–46. doi: 10.1377/hlthaff.27.2.434. [DOI] [PubMed] [Google Scholar]
- 8.Vargas ED. Immigration enforcement and mixed-status families: the effects of risk of deportation on Medicaid use. Child Youth Serv Rev. 2015;57:83–9. doi: 10.1016/j.childyouth.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Watson T. Inside the refrigerator: immigration enforcement and chilling effects in Medicaid participation. Am Econ J Econ Policy. 2014;6(3):313–38. [Google Scholar]
- 10.Immigration and Customs Enforcement. Clarification of existing practices related to certain health care information [Internet] Washington (DC): ICE; 2013. Oct 25, [cited 2018 Jan 8]. Available from: https://www.ice.gov/doclib/ero-outreach/pdf/ice-aca-memo.pdf. [Google Scholar]
- 11.Ruggles S, Genadek K, Goeken R, Grover J, Sobek M. Integrated Public Use Microdata Series: Version 6.0 [home page on the Internet] Minneapolis (MN): University of Minnesota Minnesota Population Center; [cited 2018 Jan 8]. Available from: https://usa.ipums.org/usa-action/variables/group. [Google Scholar]
- 12.Ruggles S, Genadek K, Goeken R, Grover J, Sobek M. Integrated Public Use Microdata Series Questionnaire Text [Internet] Minneapolis (MN): University of Minnesota Minnesota Population Center; [cited 2018 Jan 8]. Available from: https://usa.ipums.org/usa-action/variables/HINSCAID#questionnaire_text_section. [Google Scholar]
- 13.Henry J, Kaiser Family Foundation . Status of state action on the Medicaid expansion decision [Internet] Menlo Park (CA): KFF; 2017. Nov 8, [cited 2018 Jan 8]. Available from: http://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. [Google Scholar]
- 14.State Health Access Data Assistance Center. Defining “family” for studies of health insurance coverage [Internet] Minneapolis (MN): University of Minnesota, SHADAC; 2012. Mar, [cited 2018 Jan 8]. (Issue Brief No. 27) Available from: http://www.shadac.org/sites/default/files/publications/SHADAC_Brief27.pdf. [Google Scholar]
- 15.State Health Access Data Assistance Center. Using SHADAC Health Insurance Unit (HIU) and Federal Poverty Guideline (FPG) microdata variables [Internet] Minneapolis (MN): University of Minnesota, SHADAC; 2013. Nov, [cited 2018 Jan 8]. Available from: http://www.shadac.org/sites/default/files/Old_files/shadac/publications/SHADAC_hiu_fpg_variables_IPUMS.pdf. [Google Scholar]
- 16.Borjas GJ. The earnings of undocumented immigrants [Internet] Cambridge (MA): National Bureau of Economic Research; 2017. Mar, [cited 2018 Jan 8]. (NBER Working Paper No. 23236) [Google Scholar]
- 17.Borjas GJ. The labor supply of undocumented immigrants. Labour Econ. 2017;46:1–13. [Google Scholar]
- 18.To access the Appendix, click on the Details tab of the article online.
- 19.Van Hook J, Bachmeier JD, Coffman DL, Harel O. Can we spin straw into gold? An evaluation of immigrant legal status imputation approaches. Demography. 2015;52(1):329–54. doi: 10.1007/s13524-014-0358-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frean M, Gruber J, Sommers BD. Disentangling the ACA’s coverage effects—lessons for policymakers. N Engl J Med. 2016;375(17):1605–8. doi: 10.1056/NEJMp1609016. [DOI] [PubMed] [Google Scholar]
- 21.Heer DM, Passel JF. Comparison of two methods for estimating the number of undocumented Mexican adults in Los Angeles County. Int Migr Rev. 1987;21(4):1446–73. [PubMed] [Google Scholar]
- 22.Baker B, Rytina N. Estimates of the unauthorized immigrant population residing in the United States: January 2012 [Internet] Washington (DC): Department of Homeland Security, Office of Immigration Statistics; 2013. Mar, [cited 2018 Jan 8 ]. Available from: https://www.dhs.gov/sites/default/files/publications/UnauthorizedImmigrantPopulationEstimatesintheUSJanuary2012_0.pdf. [Google Scholar]
- 23.Passel JS, Cohn D. Overall number of US unauthorized immigrants holds steady since 2009 [Internet] Washington (DC): Pew Research Center; 2016. Sep 20, [cited 2018 Jan 8 ]. Available from: http://www.pewhispanic.org/2016/09/20/overall-number-of-u-s-unauthorized-immigrants-holds-steady-since-2009/ [Google Scholar]
- 24.Brooks T, Wagnerman K, Artiga S, Cornachione E, Ubri P. Medicaid and CHIP eligibility, enrollment, renewal, and cost sharing policies as of January 2017 findings from a 50-state survey [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; 2017. Jan 12, [2018 Jan 8 ]. Available from: https://www.kff.org/medicaid/report/medicaid-and-chip-eligibility-enrollment-renewal-and-cost-sharing-policies-as-of-january-2017-findings-from-a-50-state-survey/ [Google Scholar]
- 25.Boudreaux M, Call K, Turner J, Fried B. Estimates of direct purchase from the ACS and Medicaid misreporting: is there a link? [Internet] Minneapolis (MN): State Health Access Data Assistance Center; 2014. May, [cited 2018 Jan 8]. (Brief No. 38) Available from: http://www.shadac.org/sites/default/files/publications/SHADACBrief38_DirectPurchase_Web.pdf. [Google Scholar]
- 26.Gonzales S. Overview of immigrant eligibility policies and application processes for health insurance affordability programs [Internet] Washington (DC): Center for Budget and Policy Priorities; 2015. Nov 19, [cited 2017 Dec 26]. Available from: http://ccf.georgetown.edu/wp-content/uploads/2015/11/20151124_Beyond_Basics_Open_Enrollment_3_Immigrant-Eligibility-And-App-Process.pdf. [Google Scholar]
- 27.Perreira KM, Crosnoe R, Fortuny K, Pedroza J, Ulvestad K, Weiland C, et al. Barriers to immigrants’ access to health and human services programs [Internet] Washington (DC): Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; 2012. May, [cited 2018 Jan 8]. (ASPE Issue Brief). Available from: https://aspe.hhs.gov/system/files/pdf/76471/rb.pdf. [Google Scholar]
- 28.Goss S, Wade A, Skirvin JP, Morris M, Bye KM, Huston D. Effects of unauthorized immigration on the actuarial status of the Social Security Trust Funds [Internet] Baltimore (MD): Social Security Administration, Office of the Chief Actuary; 2013. Apr, [cited 2018 Jan 8]. (Actuarial Note No. 151) Available from: https://www.ssa.gov/oact/NOTES/pdf_notes/note151.pdf. [Google Scholar]
- 29.Collins K. Illegal aliens may fear to seek care: doctors worry about public health. McClatchy - Tribune Business News. 2008 Aug 18; [cited 2018 Jan 8]. Available from: https://search.proquest.com/docview/464438537?accountid=15172.
- 30.Pham H, Van PH. The Immigrant Climate Index (ICI) [Internet] Waco (TX): Baylor University; 2017. [cited 2018 Jan 8]. Available from: http://business.baylor.edu/van_pham/ICI/ici.html. [Google Scholar]
- 31.Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947–56. doi: 10.1056/NEJMsa1612890. [DOI] [PubMed] [Google Scholar]
- 32.Aizer A. Advertising, Medicaid, and child health. Providence (RI): Brown University, Department of Economics; 2003. Got health? (Working Paper No. 2003-20) [Google Scholar]
- 33.Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, et al. The Oregon experiment—effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–22. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kenney GM, Haley JM, Pan CW, Lynch V, Buettgens M. A look at early ACA implementation: state and national Medicaid patterns for adults in 2014 [Internet] Washington (DC): Urban Institute; 2016. Sep 8, [cited 2018 Jan 8]. Available from: https://www.urban.org/research/publication/look-early-aca-implementation-state-and-national-medicaid-patterns-adults-2014. [Google Scholar]
- 35.Aizer A. Low take-up in Medicaid: does outreach matter and for whom? Am Econ Rev. 2003;93(2):238–41. [Google Scholar]
- 36.Artiga S, Rudowitz R, Tolbert J. Outreach and enrollment strategies for reaching the Medicaid eligible but uninsured population [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; 2016. Mar 2, [cited 2018 Jan 8]. Available from: http://www.kff.org/medicaid/issue-brief/outreach-and-enrollment-strategies-for-reaching-the-medicaid-eligible-but-uninsured-population/ [Google Scholar]
- 37.Page KR, Polk S. Chilling effect? Post-election health care use by undocumented and mixed-status families. N Engl J Med. 2017;376(12):e20. doi: 10.1056/NEJMp1700829. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


