Abstract
Objectives
Many factors influence the likelihood of suicide attempts or deaths in persons with bipolar disorder. One key aim of the International Society for Bipolar Disorders Task Force on Suicide was to summarize the available literature on the presence and magnitude of effect of these factors.
Methods
A systematic review of studies published from 1 January 1980 to 30 May 2014 identified using keywords ‘bipolar disorder’ and ‘suicide attempts or suicide’. This specific paper examined all reports on factors putatively associated with suicide attempts or suicide deaths in bipolar disorder samples. Factors were subcategorized into: (1) sociodemographics, (2) clinical characteristics of bipolar disorder, (3) comorbidities, and (4) other clinical variables.
Results
We identified 141 studies that examined how 20 specific factors influenced the likelihood of suicide attempts or deaths. While the level of evidence and degree of confluence varied across factors, there was at least one study that found an effect for each of the following factors: sex, age, race, marital status, religious affiliation, age of illness onset, duration of illness, bipolar disorder subtype, polarity of first episode, polarity of current/recent episode, predominant polarity, mood episode characteristics, psychosis, psychiatric comorbidity, personality characteristics, sexual dysfunction, first-degree family history of suicide or mood disorders, past suicide attempts, early life trauma, and psychosocial precipitants.
Conclusion
There is a wealth of data on factors that influence the likelihood of suicide attempts and suicide deaths in people with bipolar disorder. Given the heterogeneity of study samples and designs, further research is needed to replicate and determine the magnitude of effect of most of these factors. This approach can ultimately lead to enhanced risk stratification for patients with bipolar disorder.
Keywords: Bipolar disorder, suicide, suicide attempts
Introduction
There are many different paths that can lead to a suicide attempt or death in a person with bipolar disorder (BD). Efforts to better understand and prevent suicidal behavior must therefore utilize the breadth of all available knowledge (Brown et al., 2000; Gonda et al., 2012; Mann et al., 2005; Zisook et al., 2013), with a special emphasis on diagnosis-specific information (Foster, 2013; Gonda et al., 2012). While aspects of risk of suicide attempts and deaths among people with BD undoubtedly partially overlap with suicide attempts or deaths in general, a robust, diagnosis-specific literature has accumulated in the past several decades.
In order to improve the understanding of suicide attempts and suicide in people with BD, the International Society for Bipolar Disorders (ISBD) launched a special task force with the goal of summarizing the rapidly expanding literature in this area. As described in paper I in this issue, the ISBD Task Force on Suicide in BD focused on four key areas of review, one of which was identifying factors associated with greater likelihood of suicide attempts or suicide in people with BD.
A number of excellent reviews of this area have been published over the years (Baethge and Cassidy, 2013; Gonda et al., 2012; Hawton et al., 2005b; Malhi et al., 2013; Mathews et al., 2013; Pompili et al., 2013; Yerevanian and Choi, 2013), and our ISBD task force also separately conducted a series of meta-analyses on 10 specific correlates of suicide attempt and deaths for which there was sufficient data to analyze using this method (Schaffer et al., 2014a). The meta-analysis paper employed specific criteria for study and variable selection based on eligibility for meta-analysis. This current article focuses on the more expansive search for all variables that have been examined for influence on likelihood of suicide attempts or death in BD samples, including newer data that were not addressed in earlier reviews of this topic.
Methods
Details of the ISBD task force methodology are outlined in paper I of this series. Briefly, we completed a systematic review of articles on BD and suicide attempts or suicides published between 1 January 1980 and 30 May 2014. A total of 141 papers related to the specific topic of factors were associated with suicide attempts or deaths.
Results
Table 1 provides a summary of the list of factors that have been associated with suicide attempts or suicide deaths in BD.
Table 1.
Summary of main factors associateda with suicide attempts and suicide deaths in BD.
| Variables | Increased likelihood of suicide attempts in BD | Increased likelihood of suicide deaths in BD |
|---|---|---|
| Sociodemographics | ||
| Sex | Female | Male |
| Females have higher SMR | ||
| Age | Younger | No clear effect |
| Older age—higher lethality attempts | Older age—higher ratio of deaths/attempts | |
| Race | Minorities—specific to youth only | |
| Marital status | Single, divorced, single parents | |
| Religious affiliation | Discordant results | |
|
| ||
| Characteristics of BD | ||
| Age of illness onset | Younger age | |
| Duration of illness | Discordant results | |
| Polarity of first episode | Depression | |
| Mixed symptoms | ||
| Mania—more violent attempts | ||
| Predominant polarity | Depressive | |
| Polarity of current episode | Depressive episodes | Depressive episodes |
| Mixed states | Mixed states | |
| Manic states with psychotic features | ||
| Other mood episode characteristics | Mixed features | Hopelessness |
| Greater number and severity of episodes/rapid cycling | Psychomotor agitation | |
| Anxiety | ||
| Atypical features | ||
| Suicidal ideation | ||
| Psychosis at any time | Discordant results | No effect |
| BD subtype | No clear effect | No clear effect |
|
| ||
| Comorbidities | ||
| Psychiatric comorbidity | Substance use disorder | Substance use disorder—no clear effect |
| Cigarette smoking | Anxiety disorder | |
| Coffee intake | ||
| Anxiety disorder | ||
| Obesity or high BMI | ||
| Eating disorder | ||
| Personality disorders and characteristics | Personality disorders—including borderline or cluster B PD in particular | |
| Aggression or irritability | ||
| Impulsivity (discordant results) | ||
|
| ||
| Other clinical variables | ||
| First-degree family history | Mood disorders | Mood disorders |
| BD | BD | |
| Suicide | Suicide | |
| Prior suicide attempts | Presence | Presence |
| Early life trauma | Childhood abuse | |
| Higher early life stress | ||
| Psychosocial precipitants | Interpersonal problems | Present within a week prior to death |
| Occupational problems | ||
| Bereavement | ||
| Sexual dysfunction | Presence | |
SMR: standardized mortality ratio; BD: bipolar disorder; BMI: body mass index; PD: personality disorder.
Discordant results were identified if studies produced opposite results for a particular variable.
Based on findings in at least one study. The data quality to support the findings varies to a considerable degree. See text of manuscript for full descriptions.
Sociodemographic factors
Sex
There is highly consistent evidence that women with BD are significantly more likely than men with BD to attempt suicide (Antypa et al., 2013; Bellivier et al., 2011; Bronisch et al., 2005; Dilsaver et al., 2005; Engstrom et al., 2004; Simon et al., 2007a; Tidemalm et al., 2014; Tsai et al., 1999; Undurraga et al., 2012). This is seen across epidemiological and clinical samples, as well as among different age groups. For example, Dilsaver et al. (2005) reported a nearly 3 times greater risk of suicide attempts among adolescent girls as compared to adolescent boys with BD (Dilsaver et al., 2005). Women are reported to be significantly less likely to attempt suicide by violent methods (Perroud et al., 2007).
The sex-based differences in risk of death by suicide are more nuanced. While men with BD clearly have significantly higher absolute rates of suicide deaths (Clements et al., 2013; Hoyer et al., 2000; Ilgen et al., 2010; Nordentoft et al., 2011; Schaffer et al., 2014b; Simon et al., 2007a; Weeke and Vaeth, 1986), in a meta-analyses of 28 studies, Tondo et al. (2003) reported a numerical, but not statistically significant higher standardized mortality rate (SMR) for women. The higher SMR for women reflects greater relative increase in risk for women with BD vs without BD, as compared to men with BD vs without BD. In a more recent study, Ilgen et al. (2010) also reported adjusted hazard ratios (HRs) for suicide death to be higher in female US veterans (HR = 6.33) compared to male veterans (HR = 2.98). Recent data from the Swedish national registry similarly identified a numerically higher SMR for suicide in women with BD than men with BD (SMR = 16.98 and SMR = 11.98, respectively) although the sex differences were no longer apparent when controlling for other sociodemographics and substance use disorders (Crump et al., 2013). While higher SMRs in women with BD may not be significant in all studies, the consistent findings suggest that the impact of the illness on risk of suicide is greater in women than in men, and that this effect appears to be stronger in BD as compared to other psychiatric diagnoses (Clements et al., 2013; Schaffer et al., 2014b). Greater help-seeking behavior leading to higher representation of women with BD may also potentially impact SMR rates, but this is difficult to determine from available data.
Age
Studies examining the relationship between age and suicide attempts in BD have found that attempters are significantly younger than non-attempters (Antypa et al., 2013; Neves et al., 2009; Pawlak et al., 2013; Ryu et al., 2010). Ryu et al. (2010) further stratified these results within age groups, with the highest retrospectively reported lifetime suicide attempt rate being in the 20–29 year age group (42.9%) followed by the 30–39 year age group (25%) and the 40+ year age group (23.2%), but the lowest rate was in the 10–19 year age group (8.9%). In a large epidemiological sample, young women with BD had a much higher ratio of suicide attempts/suicide deaths (85:1) compared to men over the age of 45 years (5:1) (Simon et al., 2007a). Oquendo et al. (2009) also reported an association between older age and higher lethality of suicide attempt. There is no age difference found in likelihood of violent or non-violent attempts (Neves et al., 2009).
There are inconsistent results with regard to age and risk of suicide death in BD. Ösby et al. (2001) reported a higher SMR among younger patients (less than 30 years) in their sample of 15,386 BD patients, while an even larger Health Maintenance Organization (HMO) sample of 32,360 BD suicides (Simon et al., 2007a) did not find any significant difference across age groups, with HRs vs subjects age 30–44 years (the reference group) being 0.63 for 18- to 29-year-olds, 0.85 for 45- to 64-year-olds and 1.34 for those 65 or older. In a Canadian sample of suicide deaths, those with BD were significantly younger at the time of death compared to non-BD suicides (43.3 years vs 47.1 years) (Schaffer et al., 2014b).
Youth
In a systematic review of studies involving youth with BD (mean age = 14.4 years), a pooled frequency of 21.3% lifetime history of suicide attempt was reported, with a 14.7% rate of suicide attempt in prospective studies with a mean 3.5 years duration (Hauser et al., 2013). While an exhaustive review of suicidal behavior among youth with BD is beyond the scope of this paper and has been reviewed elsewhere (Halfon et al., 2013), there are several key studies that reported data on this issue. Among youth with BD, a number of factors have been associated with increased likelihood of suicide attempts: illness onset after the age of 12 years (Bani-Fatemi et al., 2013), mixed states (Bani-Fatemi et al., 2013; Berutti et al., 2014), severity of depressive symptoms at intake (Bani-Fatemi et al., 2013; Berutti et al., 2014), comorbid attention deficit hyperactivity disorder (ADHD) (Hauser et al., 2013), comorbid panic disorder (Bani-Fatemi et al., 2013), comorbid substance use (Bani-Fatemi et al., 2013), history of psychosis (Bani-Fatemi et al., 2013), history of physical and/or sexual abuse (Bani-Fatemi et al., 2013), history of non-suicidal self-harm behaviors (Bani-Fatemi et al., 2013), family history of suicide or depression (Bani-Fatemi et al., 2013) and poorer family functioning, even after controlling for the severity of the BD illness (Berutti et al., 2014). Classification of youth with BD as being irritable-only, elated-only or both irritable and elated within the Course and Outcomes of Bipolar Youth (COBY) prospective cohort study did not reveal any differences in risk of suicide attempt (Hunt et al., 2013).
In a prospective study of 405 adolescents with BD, Goldstein et al. (2012) found BD I to be associated with higher rates of lifetime suicide attempt than BD not otherwise specified (NOS), with no difference between BD I and II, while Algorta et al. (2011) found no differences between BD subtypes. This latter study also demonstrated that minority youth (defined as Hispanic or African American) had higher rates of lifetime suicide attempts, while the Goldstein et al. (2012) study found no differences in terms of race or socioeconomic status.
Studies have reported higher risk of attempting suicide in BD girls compared to boys (Bani-Fatemi et al., 2013; Dilsaver et al., 2005; Goldstein et al., 2012), but this is not a consistent finding (Berutti et al., 2014).
In the only study focused on suicide death in children or youth with BD, Brent et al. (1993a) reported on 67 BD suicide deaths compared to matched controls and found mixed states (odds ratio [OR] = 9.0) and comorbid substance abuse disorders (OR = 17.0) to each be significantly associated with higher risk of death by suicide.
Race/ethnicity
Only one study in the United States addressed BD suicide deaths by race/ethnicity. Non-Hispanic whites who died by suicide had a significantly higher rate of BD diagnosis (6.1%), as compared to non-Hispanic blacks (2.6%), Hispanics (2.3%) and others (1.6%) (Karch et al., 2006). In a Toronto study, ethnicity did not influence risk of suicide attempts in patients with BD (Bani-Fatemi et al., 2013).
Marital/family status
Three clinical BD studies reported that those who were single or divorced had a significantly higher rate of lifetime suicide attempt (Azorin et al., 2009; Leverich et al., 2003; Shabani et al., 2013). Furthermore, single parents had significantly higher rates of suicide attempts than those who were married or cohabitating with children, and this was evident for both mothers and fathers (Leverich et al., 2003).
Religious affiliation
In an elegant study of BD subjects and their religious affiliation, Dervic et al. (2011) reported a significantly lower rate of lifetime suicide attempt among the 149 patients with religious affiliation compared to the 49 patients without (63.1% vs 80.4%), and showed that moral or religious objections to suicide appear to mediate the effects of religious affiliation on suicidal behavior. In contrast, high religious involvement was associated with greater likelihood of suicide attempt in a mixed unipolar–bipolar spectrum sample (Azorin et al., 2013b).
Altitude of residence
In a novel study using data from 16 US states, a significantly higher mean altitude of residence was present among BD suicide victims compared to suicide victims with other psychiatric diagnoses (Huber et al., 2014), with the authors speculating on a possible role of mitochondrial dysfunction as a contributor to suicidal behavior in BD.
Clinical characteristics of BD
Age of onset of BD
There is highly consistent evidence that earlier age of illness onset is associated with an increased likelihood of suicide attempts (Antypa et al., 2013; Azorin et al., 2009; Azorin et al., 2013a; Coryell et al., 2013; Dalton et al., 2003; Dennehy et al., 2011; Engstrom et al., 2004; Goldberg et al., 1998; Grunebaum et al., 2006; Leverich et al., 2003; Parmentier et al., 2012; Perroud et al., 2007; Ryu et al., 2010; Sanchez-Gistau et al., 2009; Song et al., 2012; Suominen et al., 2009; Tidemalm et al., 2014). One challenge in interpreting this finding is that frequencies rather than rates of suicide attempts were reported; therefore, the potential artifact of a longer duration of illness for subjects with an earlier age of onset was not generally accounted for. Age of onset was defined in a heterogeneous way throughout the literature, including age at which either depressive or manic symptoms or episodes began, age of first hospitalization, or a categorical definition of age of onset prior to a specific cut-off. Using an arbitrary cut-off of a mean age of onset above or below age 24 years, 6/16 studies had a mean age of onset of >24 years among suicide attempters, and 10/16 had a mean age of onset of >24 years among non-attempters.
We could not identify any data on the association between age of illness onset and suicide death, a glaring gap in the literature.
Duration of illness
Several studies reported that subjects with suicide attempts had a significantly longer duration of illness (Azorin et al., 2008; Bellivier et al., 2011; Michaelis et al., 2004; Roy-Byrne et al., 1988), with two exceptions that reported a significantly shorter duration of illness in prospective (Valtonen et al., 2006) and retrospective (Manchia et al., 2013) samples of suicide attempters. Roy-Byrne et al. (1988) controlled for age, and found that the positive correlation between suicide attempt and duration of illness persisted in both men and women. They also reported a positive correlation between duration of illness and higher lethality of attempt.
One study reported that suicide deaths among people diagnosed with BD most commonly occurred after >5 years of illness duration (71.4% of cases), and that this was significantly different than suicide deaths among other psychiatric diagnoses (50.3% of cases) (Clements et al., 2013).
Polarity of first mood episode and predominant polarity
Depressive polarity of first mood episode has been consistently associated with a lifetime history of suicide attempts (Azorin et al., 2009; Bellivier et al., 2011; Finseth et al., 2012; Ryu et al., 2010; Sanchez-Gistau et al., 2009; Undurraga et al., 2012; Valtonen et al., 2006) and a higher number of suicide attempts (Chaudhury et al., 2007; Neves et al., 2009). The effect of mixed symptoms during the first illness episode has not been well studied, with the exception being a cohort study of 1090 BD patients which found that among suicide attempters whose first episode was mania, the episode was more likely to be characterized by coexisting depressive symptoms (Azorin et al., 2010). Patients with a first episode of mania have been reported to be significantly more likely to attempt suicide by violent means as compared to patients with a first episode of depression (Neves et al., 2009). There were no studies of the relationship between polarity of first episode and suicide deaths.
The presence of a depressive predominant polarity has been consistently associated with greater likelihood of lifetime suicide attempts than a manic predominant polarity (Baldessarini et al., 2012; Carvalho et al., 2014; Colom et al., 2006; Popovic et al., 2014).
Polarity of episode at the time of suicide attempt or death
Both depressive and mixed states have been associated with a greater likelihood of suicide attempt, in the range of 18–62 fold and 27–74 fold higher rates, respectively, compared to pure mania (Dalton et al., 2003; Dilsaver et al., 1994; Liu et al., 1996; Tondo et al., 1999; Valtonen et al., 2008). Suicide attempts during a pure manic episode are quite rare, accounting for 0–3% of all suicide attempts in people with BD (Dalton et al., 2003; Keks et al., 2009; Liu et al., 1996; Valtonen et al., 2008).
Patients presenting in a mixed state, or who have a lifetime history of exclusively mixed episodes, also carry a higher risk of lifetime suicide attempt (Azorin et al., 2009; Goldberg et al., 1998; Gonzalez-Pinto et al., 2011). For instance, Pacchiarotti et al. (2011) found that patients with an illness course of elevated mood states characterized by only mixed episodes had a higher lifetime risk of suicide attempt (60%) compared to subjects with a combination of mixed and pure manic episodes (28%), and subjects with pure mania only (17%). Gonzalez-Pinto et al. (2011) reported the results of a 10-year follow-up study of 120 BD patients, in which 29.5% of subjects presenting with an index mixed episode attempted suicide, compared to 13.0% of subjects who presented with a non-mixed episode. The Jorvi Bipolar Study found that although mixed states may represent an equal or even higher risk period compared to depression, depressive states are a much larger component of the course of illness in BD, and therefore are linked with the greatest absolute number of suicide attempts. Of the subjects with suicide attempts documented during the period of follow-up, 74% occurred during a major depressive episode (MDE), 6% during a full mixed episode and 13% during a depressive-mixed period. The incidence of suicide attempts in the BD group during periods of subthreshold depression, full major depression and mixed/depressive mixed was 87.1, 410.7 and 878.0 per 1000 patient-years, respectively (Holma et al., 2014; Valtonen et al., 2008).
Only 0–1% of suicide attempts occur during periods of euthymia (Dalton et al., 2003; Valtonen et al., 2008).
In a Finnish study of 28 suicide deaths in BD, 78% occurred during a MDE, 11% during a mixed episode and 11% during or soon after a manic episode with psychotic features (Isometsä et al., 1994). In a more recent study by Hoyer et al. (2009) of 30 BD suicide deaths, 27 occurred during a MDE and 3 during a manic episode.
Other characteristics of mood episodes
The number of lifetime manic or depressive episodes or a history of rapid cycling have also been correlated with likelihood of a suicide attempt (Fagiolini et al., 2004; Oquendo et al., 2000; Song et al., 2012; Undurraga et al., 2012). In a Brazilian sample of BD outpatients assessed at a mean age of 41 years, suicide attempters had experienced a mean of 12 manic/hypomanic episodes and 8 depressive episodes compared to 6 manic/hypomanic episodes and 3 depressive episodes in the non-attempter group (Malloy-Diniz et al., 2009). Oquendo et al. (2000) reported that the association between greater number of depressive episodes and suicide attempt in an inpatient BD sample remained significant even when intensity of current depressive symptoms was controlled for.
Not surprisingly, patients who present with increased severity of depressive symptoms (Fagiolini et al., 2004; Hantouche et al., 2010; Michaelis et al., 2004), hopelessness (Acosta et al., 2012; Valtonen et al., 2007) or suicidal ideation (Allen et al., 2005; Azorin et al., 2009; Grunebaum et al., 2006; Roy-Byrne et al., 1988; Umamaheswari et al., 2014) carry an increased lifetime risk of suicide attempts. One study reported that BD suicide attempters were more likely to present with atypical depressive features (Sanchez-Gistau et al., 2009). Among 35 people with BD who died by suicide, 81% expressed hopelessness and 54% experienced psychomotor agitation during the last illness phase prior to death (Keks et al., 2009).
Psychosis
The presence of psychotic symptoms at any point during the BD illness has not been correlated with likelihood of a suicide attempt (Bellivier et al., 2011; Dennehy et al., 2011; Finseth et al., 2012; Gazalle et al., 2007; Gold-berg et al., 1998; Malloy-Diniz et al., 2009; Ryu et al., 2010; Valtonen et al., 2006), with one exception being a Korean sample (Song et al., 2012). In a refined analysis, Azorin et al. (2009) reported a lower mean psychosis score during the index manic episode among suicide attempters compared to non-attempters with BD. Psychotic BD has also not been associated with risk of suicide deaths (Black et al., 1988; Dennehy et al., 2011; Tondo et al., 2007; Tsai et al., 2002). Keks et al. (2009) found a relatively high rate of lifetime psychosis (63%) among BD suicide decedents, but there was no comparison group. In a more detailed examination, Tsai et al. (2002) reported no overall difference in the presence of psychosis at illness onset between 41 BD suicide decedents and 41 living controls (58.6% vs 68.3%, respectively); however, mood-incongruent psychosis at onset of illness was significantly less common among those who died by suicide compared to controls (39.0% vs 61.0%).
BD subtype
A large number of studies have compared the rates of suicide attempt between BD I and BD II, and the results suggest no clear effect of illness subtype. Some studies report higher rates among those with BD II (Holma et al., 2014; Ryu et al., 2010; Song et al., 2012; Tondo et al., 1999), others have found higher rates in BD I (Antypa et al., 2013; Bega et al., 2012; Joyce et al., 2010), but most report no significant difference (Chen et al., 2014; Dalton et al., 2003; Dennehy et al., 2011; Engstrom et al., 2004; Finseth et al., 2012; Galfalvy et al., 2006; Grunebaum et al., 2006; Hantouche et al., 2010; Leverich et al., 2003; Perroud et al., 2007; Sanchez-Gistau et al., 2009; Simon et al., 2007b; Valtonen et al., 2006). No apparent methodological factors were identified which could account for these different findings.
Phase of illness across both subtypes has also been studied. Tondo et al. (1999) reported suicide attempts in BD II being associated with depression only, as compared to BD I in which attempts occurred during both mixed states and depression. In a more recent study, Holma et al. (2014) found numerically higher incidence rates of suicide attempts in BD II vs BD I across all phases of illness, but the results were not significantly different.
The association between BD subtype and suicide deaths was examined in a large study of patients hospitalized in a private Italian hospital. Among 1765 BD patients seen in follow-up, suicide occurred in 2.8% of BD I patients and 4.2% of BD II patients, a non-significant difference (Sani et al., 2011). No studies were identified which reported on suicide deaths among people with bipolar spectrum disorder.
Comorbidities
Substance use
The large majority of studies on substance use report higher rates of suicide attempts among BD subjects with lifetime or current substance use disorders (Azorin et al., 2009; Dalton et al., 2003; Finseth et al., 2012; Gazalle et al., 2007; Goldberg et al., 1998; Grunebaum et al., 2006; Leverich et al., 2003; Malloy-Diniz et al., 2009; Nery et al., 2014; Oquendo et al., 2010; Perroud et al., 2007; Potash et al., 2000; Sanchez-Gistau et al., 2009; Simon et al., 2007a; Simon et al., 2007b; Sublette et al., 2009; Swann et al., 2005; Tondo et al., 1999; Valtonen et al., 2006). For instance, Simon et al. (2007a) reported that a past-year diagnosis of a substance use disorder was significantly associated with suicide attempts leading to hospitalization (HR = 2.53) and suicide attempts not leading to hospitalization (HR = 2.86) among over 32,000 BD subjects. Studies that separately examined alcohol and other substances generally found both types of use to be associated with suicide attempts (Bellivier et al., 2011; Gazalle et al., 2007; Moor et al., 2012); however, there were exceptions with Oquendo et al. (2010) finding that only alcohol use disorders were associated with suicide attempts among BD subjects in the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) sample, and Sublette et al. (2009) reporting only drug abuse being significantly independently associated with suicide attempts in a clinical BD sample, while the higher rates of suicide attempts among those with alcohol use disorders was primarily mediated by higher levels of aggression. Two recent studies with partially overlapping samples reported significant association between recent cannabis use and lifetime suicide attempt (Aas et al., 2013; Kvitland et al., 2014); however, several other studies failed to show a consistent correlation (Bellivier et al., 2000; Cassidy, 2011; Parmentier et al., 2012; Tondo et al., 1999). On the other hand, current or lifetime cigarette smoking has been consistently associated with suicide attempts in BD (Baethge et al., 2009; Ostacher et al., 2006, 2009). For instance, analysis of United States epidemiological data found a higher lifetime history of suicide attempt among current smokers even when controlling for other factors (OR = 1.35) (Baek et al., 2013). There is also some evidence of a dose effect, with further increased risk correlated with more cigarettes per day (Antypa et al., 2013; Baethge et al., 2009). This same study also identified a dose relationship between amount of coffee intake per day and risk of suicide attempts (Baethge et al., 2009).
Several large studies found no significant association between any substance use disorder and risk of death by suicide in BD (Cassidy, 2011; Nordentoft et al., 2011; Simon et al., 2007a; Tsai et al., 2002) although the Nordentoft study reported a substantial numerical increased incidence rate in men. The exception is data from Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD), in which 75% of subjects who died by suicide has a substance use disorder history as compared to 29.8% among those who had no prospective suicide events (Dennehy et al., 2011).
Anxiety
Most studies report that the presence of a comorbid anxiety disorder or anxiety symptoms increases the likelihood of suicide attempts in individuals with BD (Baldassano, 2006; Gazalle et al., 2007; Malloy-Diniz et al., 2009; Moor et al., 2012; Perroud et al., 2007; Sala et al., 2012; Sanchez-Gistau et al., 2009; Simon et al., 2007a; Thibodeau et al., 2013). Simon et al. (2007b) reported a significant increase in likelihood of a lifetime suicide attempt among patients with a lifetime anxiety disorder (46.7% vs 24.4%), with the association remaining significant when controlling for age, sex and substance use, but not age of illness onset. Other studies controlling for confounders yielded mixed results. While two studies replicated the independent association between anxiety disorder comorbidity and suicide attempt rates (Sala et al., 2012; Simon et al., 2007a), others did not (Leverich et al., 2003; Marangell et al., 2006; Neves et al., 2009). The diverse definition of anxiety in these studies is worth noting, including lifetime or recent anxiety symptoms, and inclusion of all or only some anxiety disorders.
A number of studies examined specific anxiety disorders in BD patients. Generalized anxiety disorder (GAD) has been found to be more common among attempters (Azorin et al., 2009; Malloy-Diniz et al., 2009; Neves et al., 2009; Perroud et al., 2007), and four studies reported higher rates of social phobia (Baldassano, 2006; Gazalle et al., 2007; Perroud et al., 2007; Simon et al., 2007b), with only one large French study not replicating this association (Azorin et al., 2009) although rates of social phobia were low in this study. Panic disorder has been consistently associated with suicide attempts across five studies (Azorin et al., 2009; Baldassano, 2006; Moor et al., 2012; Neves et al., 2009; Simon et al., 2007b), with one report of 72.2% of BD patients with panic disorder attempting suicide, and 60.3% with any anxiety disorder, compared to 22.1% of those without any anxiety disorder (Baldassano, 2006). Results for agoraphobia were contradictory, with Perroud et al. (2007) finding agoraphobia to be significantly associated with suicide attempts in BD patients while in a much larger cohort study, Azorin et al. (2009) could not find a similar association. In a clinical sample of 500 BD patients, there were significantly more attempters among those with comorbid obsessive-compulsive disorder (OCD) (Baldassano, 2006); however, again the Azorin et al. (2009) report did not replicate this. Finally, one study found that BD patients with posttraumatic stress disorder (PTSD) comorbidity were more likely to have a history of suicide attempt (Baldassano, 2006).
Simon et al. (2007a) reported a significantly increased risk of suicide deaths (age and sex adjusted HR = 1.81) among those with a comorbid anxiety disorder, which was not seen with a substance use comorbidity. No other studies examined this specific association.
Weight and metabolic parameters
Higher mean body mass index has been reported among BD patients with a lifetime suicide attempt than those without (30.2 vs 27.9) (Fagiolini et al., 2004). In a subsequent analysis of the same dataset, metabolic syndrome, and in particular the abdominal obesity criteria were also associated with higher rates of suicide attempt (Aas et al., 2013). In a large Brazilian outpatient sample, obesity was significantly associated with a history of suicide attempt (Gomes et al., 2010). There was no available data on weight or metabolic parameters and suicide deaths in BD.
Eating disorders
Four studies have identified associations between an eating disorder and suicide attempt in patients with BD. A New Zealand sample of 100 BD patients aged 15–36 reported a significant association between lifetime history of any eating disorder and risk of suicide attempt (OR = 3.7) (Moor et al., 2012). The presence of an eating disorder was also significantly prospectively associated with higher rates of suicide attempt (OR = 1.85) (Tidemalm et al., 2014). Rates of suicide attempt history were significantly higher in a United States sample of BD patients with comorbid binge eating disorder (McElroy et al., 2013). Data from patients with purging type bulimia nervosa identified significantly higher rates of suicide attempt among patients with comorbid BD (Favaro et al., 2008). Goldstein et al. (2013) also reported higher rates of lifetime suicide attempt among obese BD subjects compared to non-obese BD subjects in the NESARC sample.
Personality disorders and traits
The impact of personality disorders and various personality traits on risk of suicide attempts among those with BD has been extensively studied. There is consistent evidence that the presence of any personality disorder (Moor et al., 2012; Tidemalm et al., 2014; Undurraga et al., 2012; Valtonen et al., 2006), and specifically cluster B or borderline personality disorder are associated with higher risk of suicide attempts (Apfelbaum et al., 2013; Galfalvy et al., 2006; Garno et al., 2005; Joyce et al., 2010; Malloy-Diniz et al., 2009; Moor et al., 2012; Sanchez-Gistau et al., 2009). In a recent US study, BD and borderline personality disorder were found to have independent and additive effects on whether a prior suicide attempt had been made (Zimmerman et al., 2013). Very little has been reported on other personality clusters or disorders. Romero et al. (2007) did report higher rates of cluster C personality disorders among BD patients with a family history of suicide as compared to those with no family history.
With regard to personality traits, a number of studies reported higher scores on tests of aggression and hostility among those with BD who attempt suicide (Azorin et al., 2009; Chaudhury et al., 2007; Grunebaum et al., 2006; Michaelis et al., 2004; Rocca et al., 2010; Sher et al., 2006). The findings on effect of impulsivity are more complex, with contradictory reports of higher (Azorin et al., 2009; Storosum et al., 2005; Swann et al., 2005) or lower (Gilbert et al., 2011) impulsivity traits being associated with suicide attempts, or no effect being found (Perroud et al., 2011). Impulsivity and hostility have also been found to be correlated with each other among BD patients with a history of suicide attempt, but not correlated among patients with no history of suicide attempt (Michaelis et al., 2004). Higher impulsivity has been associated with increased medical severity of suicide attempt in one BD clinical sample (Swann et al., 2005), but with lower lethality of attempts in another sample (Gilbert et al., 2011). A recent review of impulsivity in BD only identified a weak independent link with suicidal intent or acts (Watkins and Meyer, 2013).
Other personality traits or characteristics such as extreme attributional style (Stange et al., 2014), lower social skills (Rocca et al., 2010) or self-directedness (Sarisoy et al., 2012) and cyclothymic temperament (Azorin et al., 2009; Pompili et al., 2012) have similarly been significantly associated with suicide attempts in BD samples.
Other clinical variables
Family history of suicide or mood disorders
There is fairly consistent evidence that a first-degree family history of suicide significantly increases the likelihood of suicide attempt in patients with BD (Antypa et al., 2013; Antypa and Serretti, 2014; Cassidy, 2011; Dalton et al., 2003; Dennehy et al., 2011; Engstrom et al., 2004; Finseth et al., 2012; Galfalvy et al., 2006; Guillaume et al., 2010; Hantouche et al., 2010; Leverich et al., 2003; Parmentier et al., 2012; Sanchez-Gistau et al., 2009; Valtonen et al., 2006). Romero et al. (2007) reported that among a large BD clinical sample, a family history of suicide was associated with significantly higher rates of lifetime suicide attempt (52% vs 26%), with an independent OR of 2.80. A comparable OR of 2.45 was reported in a combined Canadian-Italian clinical study, with further data showing that a significantly higher risk of suicidal behavior remained present when extended to a second-degree or third-degree family history of suicidal behavior (OR = 1.5) (Manchia et al., 2013). The effect of family history of suicidality appears to be additive to a history of childhood abuse, as demonstrated by Carballo et al. (2008) who found that the presence of both factors was associated with an earlier age of first suicide attempt, and greater number of lifetime attempts.
First-degree family history of suicide has also been strongly associated with suicide deaths in BD samples in a small number of studies (Dennehy et al., 2011; Sani et al., 2011; Tondo et al., 2007; Tsai et al., 2002).
A family history of mood disorders and more specifically BD has been reported more commonly among BD patients who attempt or die by suicide (Antypa and Serretti, 2014; Berutti et al., 2014; Brent et al., 1993b; Manchia et al., 2013; Sanchez-Gistau et al., 2009), but not in all studies (Tidemalm et al., 2014). For instance, Brent et al. (1993b) identified higher rates of bipolar spectrum in family members (OR = 4.9) among those with BD who died by suicide.
Prior suicide attempts
There is consistent evidence that past suicide attempts are significantly associated with increased risk of future suicide attempts and deaths in BD (Aizenberg et al., 2006; Guillaume et al., 2010; Michaelis et al., 2003; Tsai et al., 2002; Valtonen et al., 2006), with an analysis of STEP-BD data finding it to be the strongest predictor of a prospectively identified suicide event (OR = 3.86) (Antypa et al., 2013). A large national Finnish study of suicides post-hospitalization for BD found that intra-episodic suicide attempt was a significant predictor of suicide death after hospitalization for bipolar depression (HR = 8.05) or mixed episodes (HR = 11.1) (Isometsä et al., 2014). In a Swedish prospective cohort study of 6086 BD subjects, past suicide attempt was significantly associated with suicide attempt during follow-up among both men (OR = 3.93) and women (OR = 4.24) (Tidemalm et al., 2014). Schaffer et al. (2014b) reported higher rates of past suicide attempts among suicide completers with BD compared to those without BD (47.1% vs 25.8%). In terms of lethality, a higher lethality first attempt has been associated with a decreased likelihood of making a second attempt (Michaelis et al., 2003). In a large prospective clinical sample, Valtonen et al. (2006) reported that suicide attempt before the index mood episode or during the index mood episode were each significantly associated with greater risk of future suicide attempts.
Early life trauma
There is evidence that childhood abuse or early life stress is positively associated with suicide attempts in BD (Erten et al., 2014; Maniglio, 2013). In a clinical sample of 166 BD patients, 40% reported childhood physical or sexual abuse, which was significantly associated with an increased rate of suicide attempts (Carballo et al., 2008). Among 587 patients with BD, emotional abuse and sexual abuse were each found to be independently associated with history of suicide attempt (Etain et al., 2013). Additional analysis revealed that childhood abuse and cannabis abuse have significant additive effects, with over 80% of subjects with both childhood abuse and cannabis use making a suicide attempt (Aas et al., 2013). Benedetti et al. (2011) also reported that patients with BD who had attempted suicide identified higher levels of early life stress.
Psychosocial precipitants
Social stressors have been prospectively associated with increased likelihood of suicide attempts among men and women with BD (Tidemalm et al., 2014). Tsai et al. (1999) identified interpersonal and occupational problems to be more common among attempters in their clinical sample of 101 BD patients. In a larger sample of 648 BD patients, a greater number of suicide attempters had experienced the death of an important other in the 12 months preceding the onset of their illness (Leverich et al., 2003). Rates of employment/financial or recent medical stressors were lower in a comparison of BD suicides to non-BD suicides (Schaffer et al., 2014b). Finally, Isometsä (2005) found that 40% of recent stressful life events occurred within the week prior to suicide death, and speculated that these events may have been dependent on the persons own behavior, possibly linked to manic or mixed presentations.
Sexual dysfunction
In a clinical sample of 60 BD patients, sexual dysfunction characterized by impaired desire or difficulty with excitement or orgasm was significantly associated with a lifetime history of suicide attempt (Dell’Osso et al., 2009) although whether this effect is mediated by a global decline in interest is not clear.
Discussion
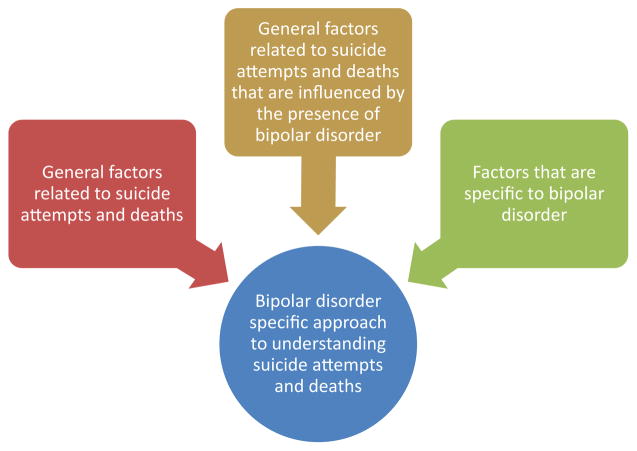
This systematic review identified a wealth of data on factors associated with suicide attempts and suicide deaths specific to BD samples. Such data can support the utilization of a diagnosis-specific approach to better understanding of suicide attempts and suicide in BD. A diagnosis-specific approach seeks to incorporate three types of information (schematic Figure 1): (1) knowledge on suicide and suicide attempts in general; (2) knowledge on general factors that are influenced by the presence of BD (e.g. relative difference of suicide risk in women with BD compared to women without BD) and (3) knowledge on factors that are specific to the diagnosis of BD (e.g. polarity of most recent mood episode). The historical paucity of data on suicide attempts and suicide specific to BD has given way to a more robust and growing literature from which a diagnosis-specific approach can be informed. There is also a track record of this being accomplished in the area of schizophrenia, for which a diagnosis-specific approach to suicide has been widely accepted (De Hert et al., 2001; Hawton et al., 2005a; Hunt et al., 2006; Reutfors et al., 2009; Siris, 2001).
Figure 1.
Schematic of ISBD Suicide Task Force proposed diagnostic-specific approach to understanding suicide attempts and deaths in bipolar disorder.
Table 1 lists the main demographic and clinical factors that have been associated with suicide attempts or suicide in BD. While the data quality and robustness across factors are not uniform, this list provides a starting point for further research in this area, highlighting the need for further replication and determination of independence and magnitude of effects. For instance, many factors likely covary with others (e.g. duration of illness with age; predominant polarity with polarity of first episode and most recent episode); therefore, while interactions between factors were highlighted when present in the literature, most studies did not address this. One aspect of this has already been undertaken by our ISBD Task Force through publication of a series of meta-analyses on correlates of suicide attempts and suicide in BD (Schaffer et al., 2014a). Variables that were found to be significantly associated with suicide attempts included female sex, younger age of illness onset, depressive polarity of first illness episode, depressive polarity of current or more recent episode, comorbid anxiety disorder, comorbid substance use disorder, comorbid cluster B/borderline personality disorder and first-degree family history of suicide. Variables that were found to be significantly associated with suicide deaths in BD included male sex and first-degree family history of suicide. However, not all variables have enough data to permit meta-analysis, so researchers conducting work in this area are encouraged to collect and report on as many of the listed factors as possible. Examination of numerous factors within each study will also permit for greater clarity as to the presence of collinearity or interactions across variables, and will facilitate transitioning toward standardization of risk assessments that are of great interest to researchers and clinicians (Bernert et al., 2014). A recent study on BD suicides (n = 170) identified the presence of five separate clusters or subgroups of BD suicide decedents based on a number of sociodemographic and clinical factors reviewed above; further replication is required to determine the validity and reliability of these subgroups (Schaffer et al., 2014b).
Several important limitations should be considered when interpreting the results of this review. First, as with any review of the literature, reporting bias must be considered, with negative associations less likely to be published. This is further impacted by the fact that for some studies the BD subjects only constituted a portion of the entire sample, and negative results may therefore not be highlighted in the publication. Second, methodological heterogeneity, differences in sample characteristics across countries and treatment settings, and a limited number of studies in many areas make the implicit or explicit conclusions tenuous at best; therefore, many findings should be considered hypothesis-generating and meant to stir further study and clinical reflection rather than firm evidence-based conclusions. Third, the complex relationship between numerous factors that likely contribute to most suicide attempts or deaths could not be adequately examined in our review, as most available data do not include any detailed examination of interactions. Furthermore, some identified factors such as marital status, early trauma, personality characteristics and other may be confounded by the diagnosis of BD. Fourth, the timing and nature of the association between suicide attempts and certain clinical variables (e.g. anxiety, substance use) could not be adequately determined, as the history of suicide attempt may have predated the comorbidity. Finally, as noted in paper I, the majority of data come from North America, Europe and East Asia, and other regions need to be more represented in the literature in order to understand the generalizability of findings, however it is worthwhile noting that many factors seem to be consistent across regions.
Conclusion
At this stage, we conclude that there are sufficient data to support incorporation of diagnosis-specific findings when seeking to better understand suicide attempts and suicide in BD. Integration of general information on suicide along with BD-specific data on non-specific and illness-specific factors can provide for a strong framework for future work.
We recommend a number of steps be taken to further develop the required research base from which evidence-based interventions can be developed. These include: (1) future studies of suicide attempts or suicide deaths in BD should include as many of the variables discussed in this article as possible. This will allow for replication of findings, and build sufficient data to begin exploration of the relationships between factors; (2) there are a number of putatively important variables that still need to be directly studied in BD, including but not limited to rural vs urban status, and sexual orientation; (3) prospective cohort studies in BD should include measures of suicide risk and outcomes; (4) the impact of environmental factors (e.g. seasons, weather, latitude, lithium water levels, toxins) on suicide attempts and suicide risk in BD is an area of importance that requires further study and (5) particular attention should be given to developing BD studies of suicide risk and potential interventions in countries or world regions from which data is lacking.
Acknowledgments
The authors wish to thank the International Society for Bipolar Disorders executive and staff who assisted with the organization of the task force, and the students and researchers who assisted with the literature review and provided statistical work (Jessika Lenchyshyn BSc McMaster University; Randy Rovinski MSc, University of Toronto). Partial findings were presented during symposia at the 16th Annual Conference of the International Society for Bipolar Disorders.
Funding
Partial support for this project was provided by the Brenda Smith Bipolar Disorder Research Fund, Sunnybrook Health Sciences Centre, University of Toronto.
Footnotes
Declaration of interest
Dr Schaffer has in the past received speakers’ bureau honoraria, advisory panel funding, and/or research grants from Bristol-Myers Squibb, Eli Lilly Canada, Lundbeck Canada, Otsuka, Pfizer Canada and Sunovion. Dr Isometsä has no financial disclosures to report. Dr Azorin has received research support and has acted as consultant and/or served on a speaker’s bureau for Bristol-Myers Squibb, Janssen, Lilly, Lundbeck, Roche and Sanofi-Aventis. Dr Cassidy has no financial disclosures to report. Dr Goldstein has received research support from NIMH, NIDA, NICHD, The Pittsburgh Foundation and Royalties from Guilford Press. Dr Rihmer has in the past received speakers’ bureau honoraria, advisory board funding or travel support from AstraZeneca, Janssen, Lundbeck, Lilly, Servier-EGIS, Richer and TEVA-Biogal. Dr Sinyor has received grant support from the American Foundation for Suicide Prevention, Physicians’ Services Incorporated (PSI) Foundation and the Brenda Smith Bipolar Disorder Research Fund. Dr Tondo has received funding from private donors to Aretaeus Association and to McLean Hospital. Dr Moreno has received grant support or served as a speaker for Abbott, Aché, Lundbeck, EMS and Eurofarma. Dr Turecki has no financial disclosures to report. Ms Reis has no financial disclosures to report. Dr Kessing has within the preceding 3 years been a consultant for Lundbeck and AstraZeneca. Dr. Ha has no financial disclosures to report. Dr Weizman has no financial disclosures to report. Dr Beautrais has no financial disclosures to report. Dr Chou has no financial disclosures to report. Dr Diazgranados has no financial disclosures to report. Dr Levitt has received research grants from Janssen Ortho, AstraZeneca, Great West Life Insurance and Eli Lilly Canada and has acted as a consultant for Janssen Ortho. Dr Zarate is listed as a coinventor on a patent application for the use of ketamine and its metabolites in major depression. He has assigned his rights in the patent to the United States government but will share a percentage of any royalties that may be received by the government. Dr Yatham has been a member of advisory boards and/or received research grants and/or been a speaker for AstraZeneca, DSP, Janssen, Lilly, GSK, Bristol-Myers Squibb, Lundbeck, Novartis, Servier, Sunovion and Pfizer.
References
- Aas M, Etain B, Bellivier F, et al. Additive effects of childhood abuse and cannabis abuse on clinical expressions of bipolar disorders. Psychological Medicine. 2013;44:1653–1662. doi: 10.1017/S0033291713002316. [DOI] [PubMed] [Google Scholar]
- Acosta FJ, Vega D, Torralba L, et al. Hopelessness and suicidal risk in bipolar disorder. A study in clinically nonsyndromal patients. Comprehensive Psychiatry. 2012;53:1103–1109. doi: 10.1016/j.comppsych.2012.03.013. [DOI] [PubMed] [Google Scholar]
- Aizenberg D, Olmer A, Barak Y. Suicide attempts amongst elderly bipolar patients. Journal of Affective Disorders. 2006;91:91–94. doi: 10.1016/j.jad.2005.12.013. [DOI] [PubMed] [Google Scholar]
- Algorta GP, Youngstrom EA, Frazier TW, et al. Suicidality in pediatric bipolar disorder: Predictor or outcome of family processes and mixed mood presentation? Bipolar Disorders. 2011;13:76–86. doi: 10.1111/j.1399-5618.2010.00886.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen MH, Chessick CA, Miklowitz DJ, et al. Contributors to suicidal ideation among bipolar patients with and without a history of suicide attempts. Suicide and Life-Threatening Behavior. 2005;35:671–680. doi: 10.1521/suli.2005.35.6.671. [DOI] [PubMed] [Google Scholar]
- Antypa N, Serretti A. Family history of a mood disorder indicates a more severe bipolar disorder. Journal of Affective Disorders. 2014;156:178–186. doi: 10.1016/j.jad.2013.12.013. [DOI] [PubMed] [Google Scholar]
- Antypa N, Antonioli M, Serretti A. Clinical, psychological and environmental predictors of prospective suicide events in patients with bipolar disorder. Journal of Psychiatric Research. 2013;47:1800–1808. doi: 10.1016/j.jpsychires.2013.08.005. [DOI] [PubMed] [Google Scholar]
- Apfelbaum S, Regalado P, Herman L, et al. Comorbidity between bipolar disorder and cluster B personality disorders as indicator of affective dysregulation and clinical severity. Actas Españolas de Psiquiatría. 2013;41:269–278. [PubMed] [Google Scholar]
- Azorin JM, Bellivier F, Kaladjian A, et al. Characteristics and profiles of bipolar I patients according to age-at-onset: Findings from an admixture analysis. Journal of Affective Disorders. 2013a;150:993–1000. doi: 10.1016/j.jad.2013.05.026. [DOI] [PubMed] [Google Scholar]
- Azorin JM, Kaladjian A, Adida M, et al. Toward the delineation of mania subtypes in the French National EPIMAN-II Mille Cohort. Comparisons with prior cluster analytic investigations. European Archives of Psychiatry and Clinical Neuroscience. 2008;258:497–504. doi: 10.1007/s00406-008-0823-x. [DOI] [PubMed] [Google Scholar]
- Azorin JM, Kaladjian A, Adida M, et al. Risk factors associated with lifetime suicide attempts in bipolar I patients: Findings from a French National Cohort. Comprehensive Psychiatry. 2009;50:115–120. doi: 10.1016/j.comppsych.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Azorin JM, Kaladjian A, Besnier N, et al. Suicidal behaviour in a French Cohort of major depressive patients: Characteristics of attempters and nonattempters. Journal of Affective Disorders. 2010;123:87–94. doi: 10.1016/j.jad.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Azorin JM, Kaladjian A, Fakra E, et al. Religious involvement in major depression: Protective or risky behavior? The relevance of bipolar spectrum. Journal of Affective Disorders. 2013b;150:753–759. doi: 10.1016/j.jad.2013.02.034. [DOI] [PubMed] [Google Scholar]
- Baek JH, Eisner LR, Nierenberg AA. Smoking and suicidality in subjects with bipolar disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Depress Anxiety. 2013;30:982–990. doi: 10.1002/da.22107. [DOI] [PubMed] [Google Scholar]
- Baethge C, Cassidy F. Fighting on the side of life: A special issue on suicide in bipolar disorder. Bipolar Disorders. 2013;15:453–456. doi: 10.1111/bdi.12097. [DOI] [PubMed] [Google Scholar]
- Baethge C, Tondo L, Lepri B, et al. Coffee and cigarette use: Association with suicidal acts in 352 Sardinian bipolar disorder patients. Bipolar Disorders. 2009;11:494–503. doi: 10.1111/j.1399-5618.2009.00727.x. [DOI] [PubMed] [Google Scholar]
- Baldassano CF. Illness course, comorbidity, gender, and suicidality in patients with bipolar disorder. The Journal of Clinical Psychiatry. 2006;67(Suppl 11):8–11. [PubMed] [Google Scholar]
- Baldessarini RJ, Salvatore P, Khalsa HM, et al. Episode cycles with increasing recurrences in first-episode bipolar-I disorder patients. Journal of Affective Disorders. 2012;136:149–154. doi: 10.1016/j.jad.2011.08.037. [DOI] [PubMed] [Google Scholar]
- Bani-Fatemi A, Polsinelli G, Kennedy JL, et al. Ethnicity and suicide attempt: Analysis in bipolar disorder and schizophrenia. BMC Psychiatry. 2013;13:252. doi: 10.1186/1471-244X-13-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bega S, Schaffer A, Goldstein B, et al. Differentiating between bipolar disorder types I and II: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Journal of Affective Disorders. 2012;138:46–53. doi: 10.1016/j.jad.2011.12.032. [DOI] [PubMed] [Google Scholar]
- Bellivier F, Szoke A, Henry C, et al. Possible association between serotonin transporter gene polymorphism and violent suicidal behavior in mood disorders. Biological Psychiatry. 2000;48:319–322. doi: 10.1016/s0006-3223(00)00891-x. [DOI] [PubMed] [Google Scholar]
- Bellivier F, Yon L, Luquiens A, et al. Suicidal attempts in bipolar disorder: Results from an observational study (EMBLEM) Bipolar Disorders. 2011;13:377–386. doi: 10.1111/j.1399-5618.2011.00926.x. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Radaelli D, Poletti S, et al. Opposite effects of suicidality and lithium on gray matter volumes in bipolar depression. Journal of Affective Disorders. 2011;135:139–147. doi: 10.1016/j.jad.2011.07.006. [DOI] [PubMed] [Google Scholar]
- Bernert RA, Hom MA, Roberts LW. A review of multidisciplinary clinical practice guidelines in suicide prevention: Toward an emerging standard in suicide risk assessment and management, training and practice. Academic Psychiatry. 2014;38:585–592. doi: 10.1007/s40596-014-0180-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berutti M, Nery FG, Sato R, et al. Association between family history of mood disorders and clinical characteristics of bipolar disorder: Results from the Brazilian bipolar research network. Journal of Affective Disorders. 2014;161:104–108. doi: 10.1016/j.jad.2014.02.045. [DOI] [PubMed] [Google Scholar]
- Black DW, Winokur G, Nasrallah A. Effect of psychosis on suicide risk in 1,593 patients with unipolar and bipolar affective disorders. The American Journal of Psychiatry. 1988;145:849–852. doi: 10.1176/ajp.145.7.849. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, et al. Psychiatric risk factors for adolescent suicide: A case-control study. Journal of the American Academy of Child and Adolescent Psychiatry. 1993a;32:521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, et al. The validity of diagnoses obtained through the psychological autopsy procedure in adolescent suicide victims: Use of family history. Acta Psychiatrica Scandinavica. 1993b;87:118–122. doi: 10.1111/j.1600-0447.1993.tb03341.x. [DOI] [PubMed] [Google Scholar]
- Bronisch T, Schwender L, Hofler M, et al. Mania, hypomania, and suicidality: Findings from a prospective community study. Archives of Suicide Research. 2005;9:267–278. doi: 10.1080/13811110590929460. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, et al. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- Carballo JJ, Harkavy-Friedman J, Burke AK, et al. Family history of suicidal behavior and early traumatic experiences: Additive effect on suicidality and course of bipolar illness? Journal of Affective Disorders. 2008;109:57–63. doi: 10.1016/j.jad.2007.12.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho AF, McIntyre RS, Dimelis D, et al. Predominant polarity as a course specifier for bipolar disorder: A systematic review. Journal of Affective Disorders. 2014;163C:56–64. doi: 10.1016/j.jad.2014.03.035. [DOI] [PubMed] [Google Scholar]
- Cassidy F. Risk factors of attempted suicide in bipolar disorder. Suicide and Life-Threatening Behavior. 2011;41:6–11. doi: 10.1111/j.1943-278X.2010.00007.x. [DOI] [PubMed] [Google Scholar]
- Chaudhury SR, Grunebaum MF, Galfalvy HC, et al. Does first episode polarity predict risk for suicide attempt in bipolar disorder? Journal of Affective Disorders. 2007;104:245–250. doi: 10.1016/j.jad.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Liu YH, Zheng QW, et al. Suicide risk in major affective disorder: Results from a national survey in China. Journal of Affective Disorders. 2014;155:174–179. doi: 10.1016/j.jad.2013.10.046. [DOI] [PubMed] [Google Scholar]
- Clements C, Morriss R, Jones S, et al. Suicide in bipolar disorder in a national English sample, 1996–2009: Frequency, trends and characteristics. Psychological Medicine. 2013;43:2593–2602. doi: 10.1017/S0033291713000329. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Daban C, et al. Clinical and therapeutic implications of predominant polarity in bipolar disorder. Journal of Affective Disorders. 2006;93:13–17. doi: 10.1016/j.jad.2006.01.032. [DOI] [PubMed] [Google Scholar]
- Coryell W, Fiedorowicz J, Leon AC, et al. Age of onset and the prospectively observed course of illness in bipolar disorder. Journal of Affective Disorders. 2013;146:34–38. doi: 10.1016/j.jad.2012.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crump C, Sundquist K, Winkleby MA, et al. Comorbidities and mortality in bipolar disorder: A Swedish national cohort study. JAMA Psychiatry. 2013;70:931–939. doi: 10.1001/jamapsychiatry.2013.1394. [DOI] [PubMed] [Google Scholar]
- Dalton EJ, Cate-Carter TD, Mundo E, et al. Suicide risk in bipolar patients: The role of comorbid substance use disorders. Bipolar Disorders. 2003;5:58–61. doi: 10.1034/j.1399-5618.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- De Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: A long-term follow-up study. Schizophrenia Research. 2001;47:127–134. doi: 10.1016/s0920-9964(00)00003-7. [DOI] [PubMed] [Google Scholar]
- Dell’Osso L, Carmassi C, Carlini M, et al. Sexual dysfunctions and suicidality in patients with bipolar disorder and unipolar depression. The Journal of Sexual Medicine. 2009;6:3063–3070. doi: 10.1111/j.1743-6109.2009.01455.x. [DOI] [PubMed] [Google Scholar]
- Dennehy EB, Marangell LB, Allen MH, et al. Suicide and suicide attempts in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) Journal of Affective Disorders. 2011;133:423–427. doi: 10.1016/j.jad.2011.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dervic K, Carballo JJ, Baca-Garcia E, et al. Moral or religious objections to suicide may protect against suicidal behavior in bipolar disorder. The Journal of Clinical Psychiatry. 2011;72:1390–1396. doi: 10.4088/JCP.09m05910gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilsaver SC, Benazzi F, Rihmer Z, et al. Gender, suicidality and bipolar mixed states in adolescents. Journal of Affective Disorders. 2005;87:11–16. doi: 10.1016/j.jad.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Dilsaver SC, Chen YW, Swann AC, et al. Suicidality in patients with pure and depressive mania. The American Journal of Psychiatry. 1994;151:1312–1315. doi: 10.1176/ajp.151.9.1312. [DOI] [PubMed] [Google Scholar]
- Engstrom C, Brandstrom S, Sigvardsson S, et al. Bipolar disorder. III: Harm avoidance a risk factor for suicide attempts. Bipolar Disorders. 2004;6:130–138. doi: 10.1111/j.1399-5618.2004.00101.x. [DOI] [PubMed] [Google Scholar]
- Erten E, Funda Uney A, Saatcioglu O, et al. Effects of childhood trauma and clinical features on determining quality of life in patients with bipolar I disorder. Journal of Affective Disorders. 2014;162:107–113. doi: 10.1016/j.jad.2014.03.046. [DOI] [PubMed] [Google Scholar]
- Etain B, Aas M, Andreassen OA, et al. Childhood trauma is associated with severe clinical characteristics of bipolar disorders. The Journal of Clinical Psychiatry. 2013;74:991–998. doi: 10.4088/JCP.13m08353. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Kupfer DJ, Rucci P, et al. Suicide attempts and ideation in patients with bipolar I disorder. The Journal of Clinical Psychiatry. 2004;65:509–514. doi: 10.4088/jcp.v65n0409. [DOI] [PubMed] [Google Scholar]
- Favaro A, Santonastaso P, Monteleone P, et al. Self-injurious behavior and attempted suicide in purging bulimia nervosa: Associations with psychiatric comorbidity. Journal of Affective Disorders. 2008;105:285–289. doi: 10.1016/j.jad.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Finseth PI, Morken G, Andreassen OA, et al. Risk factors related to lifetime suicide attempts in acutely admitted bipolar disorder inpatients. Bipolar Disorders. 2012;14:727–734. doi: 10.1111/bdi.12004. [DOI] [PubMed] [Google Scholar]
- Foster TJ. Suicide prevention as a prerequisite for recovery from severe mental illness. International Journal of Psychiatry in Medicine. 2013;46:15–25. doi: 10.2190/PM.46.1.b. [DOI] [PubMed] [Google Scholar]
- Galfalvy H, Oquendo MA, Carballo JJ, et al. Clinical predictors of suicidal acts after major depression in bipolar disorder: A prospective study. Bipolar Disorders. 2006;8:586–595. doi: 10.1111/j.1399-5618.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- Garno JL, Goldberg JF, Ramirez PM, et al. Bipolar disorder with comorbid cluster B personality disorder features: Impact on suicidality. The Journal of Clinical Psychiatry. 2005;66:339–345. doi: 10.4088/jcp.v66n0310. [DOI] [PubMed] [Google Scholar]
- Gazalle FK, Hallal PC, Tramontina J, et al. Polypharmacy and suicide attempts in bipolar disorder. Revista Brasileira de Psiquiatria. 2007;29:35–38. [PubMed] [Google Scholar]
- Gilbert AM, Garno JL, Braga RJ, et al. Clinical and cognitive correlates of suicide attempts in bipolar disorder: Is suicide predictable? The Journal of Clinical Psychiatry. 2011;72:1027–1033. doi: 10.4088/JCP.10m06410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg JF, Garno JL, Leon AC, et al. Association of recurrent suicidal ideation with nonremission from acute mixed mania. The American Journal of Psychiatry. 1998;155:1753–1755. doi: 10.1176/ajp.155.12.1753. [DOI] [PubMed] [Google Scholar]
- Goldstein BI, Liu SM, Schaffer A, et al. Obesity and the three-year longitudinal course of bipolar disorder. Bipolar Disorders. 2013;15:284–293. doi: 10.1111/bdi.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Ha W, Axelson DA, et al. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Archives of General Psychiatry. 2012;69:1113–1122. doi: 10.1001/archgenpsychiatry.2012.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes FA, Kauer-Sant’Anna M, Magalhaes PV, et al. Obesity is associated with previous suicide attempts in bipolar disorder. Acta Neuropsychiatrica. 2010;22:63–67. doi: 10.1111/j.1601-5215.2010.00452.x. [DOI] [PubMed] [Google Scholar]
- Gonda X, Pompili M, Serafini G, et al. Suicidal behavior in bipolar disorder: Epidemiology, characteristics and major risk factors. Journal of Affective Disorders. 2012;143:16–26. doi: 10.1016/j.jad.2012.04.041. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Pinto A, Barbeito S, Alonso M, et al. Poor long-term prognosis in mixed bipolar patients: 10-year outcomes in the Vitoria prospective naturalistic study in Spain. The Journal of Clinical Psychiatry. 2011;72:671–676. doi: 10.4088/JCP.09m05483yel. [DOI] [PubMed] [Google Scholar]
- Grunebaum MF, Ramsay SR, Galfalvy HC, et al. Correlates of suicide attempt history in bipolar disorder: A stress-diathesis perspective. Bipolar Disorders. 2006;8:551–557. doi: 10.1111/j.1399-5618.2006.00304.x. [DOI] [PubMed] [Google Scholar]
- Guillaume S, Jaussent I, Jollant F, et al. Suicide attempt characteristics may orientate toward a bipolar disorder in attempters with recurrent depression. Journal of Affective Disorders. 2010;122:53–59. doi: 10.1016/j.jad.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Halfon N, Labelle R, Cohen D, et al. Juvenile bipolar disorder and suicidality: A review of the last 10 years of literature. European Child & Adolescent Psychiatry. 2013;22:139–151. doi: 10.1007/s00787-012-0328-z. [DOI] [PubMed] [Google Scholar]
- Hantouche E, Angst J, Azorin JM. Explained factors of suicide attempts in major depression. Journal of Affective Disorders. 2010;127:305–308. doi: 10.1016/j.jad.2010.04.032. [DOI] [PubMed] [Google Scholar]
- Hauser M, Galling B, Correll CU. Suicidal ideation and suicide attempts in children and adolescents with bipolar disorder: A systematic review of prevalence and incidence rates, correlates, and targeted interventions. Bipolar Disorders. 2013;15:507–523. doi: 10.1111/bdi.12094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, et al. Schizophrenia and suicide: Systematic review of risk factors. The British Journal of Psychiatry. 2005a;187:9–20. doi: 10.1192/bjp.187.1.9. [DOI] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, et al. Suicide and attempted suicide in bipolar disorder: A systematic review of risk factors. The Journal of Clinical Psychiatry. 2005b;66:693–704. doi: 10.4088/jcp.v66n0604. [DOI] [PubMed] [Google Scholar]
- Holma KM, Haukka J, Suominen K, et al. Differences in incidence of suicide attempts between bipolar I and II disorders and major depressive disorder. Bipolar Disorders. 2014;16:652–661. doi: 10.1111/bdi.12195. [DOI] [PubMed] [Google Scholar]
- Hoyer EH, Licht RW, Mortensen PB. Risk factors of suicide in inpatients and recently discharged patients with affective disorders. A case-control study. European Psychiatry. 2009;24:317–321. doi: 10.1016/j.eurpsy.2008.03.011. [DOI] [PubMed] [Google Scholar]
- Hoyer EH, Mortensen PB, Olesen AV. Mortality and causes of death in a total national sample of patients with affective disorders admitted for the first time between 1973 and 1993. The British Journal of Psychiatry. 2000;176:76–82. doi: 10.1192/bjp.176.1.76. [DOI] [PubMed] [Google Scholar]
- Huber RS, Coon H, Kim N, et al. Altitude is a risk factor for completed suicide in bipolar disorder. Medical Hypotheses. 2014;82:377–381. doi: 10.1016/j.mehy.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt IM, Kapur N, Windfuhr K, et al. Suicide in schizophrenia: Findings from a national clinical survey. Journal of Psychiatric Practice. 2006;12:139–147. doi: 10.1097/00131746-200605000-00002. [DOI] [PubMed] [Google Scholar]
- Hunt JI, Case BG, Birmaher B, et al. Irritability and elation in a large bipolar youth sample: Relative symptom severity and clinical outcomes over 4 years. The Journal of Clinical Psychiatry. 2013;74:e110–e117. doi: 10.4088/JCP.12m07874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, Bohnert AS, Ignacio RV, et al. Psychiatric diagnoses and risk of suicide in veterans. Archives of General Psychiatry. 2010;67:1152–1158. doi: 10.1001/archgenpsychiatry.2010.129. [DOI] [PubMed] [Google Scholar]
- Isometsä E. Suicide in bipolar I disorder in Finland: Psychological autopsy findings from the National Suicide Prevention Project in Finland. Archives of Suicide Research. 2005;9:251–260. doi: 10.1080/13811110590929442. [DOI] [PubMed] [Google Scholar]
- Isometsä E, Sund R, Pirkola S. Post-discharge suicides of inpatients with bipolar disorder in Finland. Bipolar Disorders. 2014;16:867–874. doi: 10.1111/bdi.12237. [DOI] [PubMed] [Google Scholar]
- Isometsä ET, Henriksson MM, Aro HM, et al. Suicide in bipolar disorder in Finland. The American Journal of Psychiatry. 1994;151:1020–1024. doi: 10.1176/ajp.151.7.1020. [DOI] [PubMed] [Google Scholar]
- Joyce PR, Light KJ, Rowe SL, et al. Self-mutilation and suicide attempts: Relationships to bipolar disorder, borderline personality disorder, temperament and character. Australian and New Zealand Journal of Psychiatry. 2010;44:250–257. doi: 10.3109/00048670903487159. [DOI] [PubMed] [Google Scholar]
- Karch DL, Barker L, Strine TW. Race/ethnicity, substance abuse, and mental illness among suicide victims in 13 US states: 2004 data from the National Violent Death Reporting System. Injury Prevention. 2006;12(Suppl 2):ii22–ii27. doi: 10.1136/ip.2006.013557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keks NA, Hill C, Sundram S, et al. Evaluation of treatment in 35 cases of bipolar suicide. Australian and New Zealand Journal of Psychiatry. 2009;43:503–508. doi: 10.1080/00048670902873680. [DOI] [PubMed] [Google Scholar]
- Kvitland LR, Melle I, Aminoff SR, et al. Cannabis use in first-treatment bipolar I disorder: Relations to clinical characteristics. Early Intervention in Psychiatry. 2014 doi: 10.1111/eip.12138. Epub ahead of print 17 April. [DOI] [PubMed] [Google Scholar]
- Leverich GS, Altshuler LL, Frye MA, et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. The Journal of Clinical Psychiatry. 2003;64:506–515. doi: 10.4088/jcp.v64n0503. [DOI] [PubMed] [Google Scholar]
- Liu CY, Bai YM, Yang YY, et al. Suicide and parasuicide in psychiatric inpatients: Ten years experience at a general hospital in Taiwan. Psychological Reports. 1996;79:683–690. doi: 10.2466/pr0.1996.79.2.683. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Crow S, Biernacka JM, et al. Clinical phenotype of bipolar disorder with comorbid binge eating disorder. Journal of Affective Disorders. 2013;150:981–986. doi: 10.1016/j.jad.2013.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi GS, Bargh DM, Kuiper S, et al. Modeling bipolar disorder suicidality. Bipolar Disorders. 2013;15:559–574. doi: 10.1111/bdi.12093. [DOI] [PubMed] [Google Scholar]
- Malloy-Diniz LF, Neves FS, Abrantes SS, et al. Suicide behavior and neuropsychological assessment of type I bipolar patients. Journal of Affective Disorders. 2009;112:231–236. doi: 10.1016/j.jad.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Manchia M, Hajek T, O’Donovan C, et al. Genetic risk of suicidal behavior in bipolar spectrum disorder: Analysis of 737 pedigrees. Bipolar Disorders. 2013;15:496–506. doi: 10.1111/bdi.12088. [DOI] [PubMed] [Google Scholar]
- Maniglio R. The impact of child sexual abuse on the course of bipolar disorder: A systematic review. Bipolar Disorders. 2013;15:341–358. doi: 10.1111/bdi.12050. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: A systematic review. Journal of the American Medical Association. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- Marangell LB, Bauer MS, Dennehy EB, et al. Prospective predictors of suicide and suicide attempts in 1,556 patients with bipolar disorders followed for up to 2 years. Bipolar Disorders. 2006;8:566–575. doi: 10.1111/j.1399-5618.2006.00369.x. [DOI] [PubMed] [Google Scholar]
- Mathews DC, Richards EM, Niciu MJ, et al. Neurobiological aspects of suicide and suicide attempts in bipolar disorder. Translational Neuroscience. 2013;4:203–216. doi: 10.2478/s13380-013-0120-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaelis BH, Goldberg JF, Davis GP, et al. Dimensions of impulsivity and aggression associated with suicide attempts among bipolar patients: A preliminary study. Suicide and Life-Threatening Behavior. 2004;34:172–176. doi: 10.1521/suli.34.2.172.32783. [DOI] [PubMed] [Google Scholar]
- Michaelis BH, Goldberg JF, Singer TM, et al. Characteristics of first suicide attempts in single versus multiple suicide attempters with bipolar disorder. Comprehensive Psychiatry. 2003;44:15–20. doi: 10.1053/comp.2003.50004. [DOI] [PubMed] [Google Scholar]
- Moor S, Crowe M, Luty S, et al. Effects of comorbidity and early age of onset in young people with bipolar disorder on self harming behaviour and suicide attempts. Journal of Affective Disorders. 2012;136:1212–1215. doi: 10.1016/j.jad.2011.10.018. [DOI] [PubMed] [Google Scholar]
- Nery FG, Miranda-Scippa A, Nery-Fernandes F, et al. Prevalence and clinical correlates of alcohol use disorders among bipolar disorder patients: Results from the Brazilian Bipolar Research Network. Comprehensive Psychiatry. 2014;55:1116–1121. doi: 10.1016/j.comppsych.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Neves FS, Malloy-Diniz LF, Correa H. Suicidal behavior in bipolar disorder: What is the influence of psychiatric comorbidities? The Journal of Clinical Psychiatry. 2009;70:13–18. doi: 10.4088/jcp.08m04037. [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Archives of General Psychiatry. 2011;68:1058–1064. doi: 10.1001/archgenpsychiatry.2011.113. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Carballo JJ, Rajouria N, et al. Are high-lethality suicide attempters with bipolar disorder a distinct phenotype? Archives of Suicide Research. 2009;13:247–256. doi: 10.1080/13811110903044385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Currier D, Liu SM, et al. Increased risk for suicidal behavior in comorbid bipolar disorder and alcohol use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) The Journal of Clinical Psychiatry. 2010;71:902–909. doi: 10.4088/JCP.09m05198gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Waternaux C, Brodsky B, et al. Suicidal behavior in bipolar mood disorder: Clinical characteristics of attempters and nonattempters. Journal of Affective Disorders. 2000;59:107–117. doi: 10.1016/s0165-0327(99)00129-9. [DOI] [PubMed] [Google Scholar]
- Ösby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Archives of General Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- Ostacher MJ, Lebeau RT, Perlis RH, et al. Cigarette smoking is associated with suicidality in bipolar disorder. Bipolar Disorders. 2009;11:766–771. doi: 10.1111/j.1399-5618.2009.00744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostacher MJ, Nierenberg AA, Perlis RH, et al. The relationship between smoking and suicidal behavior, comorbidity, and course of illness in bipolar disorder. The Journal of Clinical Psychiatry. 2006;67:1907–1911. doi: 10.4088/jcp.v67n1210. [DOI] [PubMed] [Google Scholar]
- Pacchiarotti I, Mazzarini L, Kotzalidis GD, et al. Mania and depression. Mixed, not stirred. Journal of Affective Disorders. 2011;133:105–113. doi: 10.1016/j.jad.2011.03.037. [DOI] [PubMed] [Google Scholar]
- Parmentier C, Etain B, Yon L, et al. Clinical and dimensional characteristics of euthymic bipolar patients with or without suicidal behavior. European Psychiatry. 2012;27:570–576. doi: 10.1016/j.eurpsy.2011.05.005. [DOI] [PubMed] [Google Scholar]
- Pawlak J, Dmitrzak-Weglarz M, Skibinska M, et al. Suicide attempts and clinical risk factors in patients with bipolar and unipolar affective disorders. General Hospital Psychiatry. 2013;35:427–432. doi: 10.1016/j.genhosppsych.2013.03.014. [DOI] [PubMed] [Google Scholar]
- Perroud N, Baud P, Mouthon D, et al. Impulsivity, aggression and suicidal behavior in unipolar and bipolar disorders. Journal of Affective Disorders. 2011;134:112–118. doi: 10.1016/j.jad.2011.05.048. [DOI] [PubMed] [Google Scholar]
- Perroud N, Baud P, Preisig M, et al. Social phobia is associated with suicide attempt history in bipolar inpatients. Bipolar Disorders. 2007;9:713–721. doi: 10.1111/j.1399-5618.2007.00471.x. [DOI] [PubMed] [Google Scholar]
- Pompili M, Gonda X, Serafini G, et al. Epidemiology of suicide in bipolar disorders: A systematic review of the literature. Bipolar Disorders. 2013;15:457–490. doi: 10.1111/bdi.12087. [DOI] [PubMed] [Google Scholar]
- Pompili M, Rihmer Z, Akiskal H, et al. Temperaments mediate suicide risk and psychopathology among patients with bipolar disorders. Comprehensive Psychiatry. 2012;53:280–285. doi: 10.1016/j.comppsych.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Popovic D, Torrent C, Goikolea JM, et al. Clinical implications of predominant polarity and the polarity index in bipolar disorder: A naturalistic study. Acta Psychiatrica Scandinavica. 2014;129:366–374. doi: 10.1111/acps.12179. [DOI] [PubMed] [Google Scholar]
- Potash JB, Kane HS, Chiu YF, et al. Attempted suicide and alcoholism in bipolar disorder: Clinical and familial relationships. The American Journal of Psychiatry. 2000;157:2048–2050. doi: 10.1176/appi.ajp.157.12.2048. [DOI] [PubMed] [Google Scholar]
- Reutfors J, Brandt L, Jonsson EG, et al. Risk factors for suicide in schizophrenia: Findings from a Swedish population-based case-control study. Schizophrenia Research. 2009;108:231–237. doi: 10.1016/j.schres.2008.12.023. [DOI] [PubMed] [Google Scholar]
- Rocca CC, Gerchmann L, Abreu LN, et al. Lifetime history of suicide attempts is associated with poorer social skills in patients with bipolar disorder type I. Revista Brasileira de Psiquiatria. 2010;32:200–201. doi: 10.1590/s1516-44462010000200021. [DOI] [PubMed] [Google Scholar]
- Romero S, Colom F, Iosif AM, et al. Relevance of family history of suicide in the long-term outcome of bipolar disorders. The Journal of Clinical Psychiatry. 2007;68:1517–1521. doi: 10.4088/jcp.v68n1007. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Post RM, Hambrick DD, et al. Suicide and course of illness in major affective disorder. Journal of Affective Disorders. 1988;15:1–8. doi: 10.1016/0165-0327(88)90002-x. [DOI] [PubMed] [Google Scholar]
- Ryu V, Jon DI, Cho HS, et al. Initial depressive episodes affect the risk of suicide attempts in Korean patients with bipolar disorder. Yonsei Medical Journal. 2010;51:641–647. doi: 10.3349/ymj.2010.51.5.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sala R, Goldstein BI, Morcillo C, et al. Course of comorbid anxiety disorders among adults with bipolar disorder in the U.S. population. Journal of Psychiatric Research. 2012;46:865–872. doi: 10.1016/j.jpsychires.2012.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Gistau V, Colom F, Mane A, et al. Atypical depression is associated with suicide attempt in bipolar disorder. Acta Psychiatrica Scandinavica. 2009;120:30–36. doi: 10.1111/j.1600-0447.2008.01341.x. [DOI] [PubMed] [Google Scholar]
- Sani G, Tondo L, Koukopoulos A, et al. Suicide in a large population of former psychiatric inpatients. Psychiatry and Clinical Neurosciences. 2011;65:286–295. doi: 10.1111/j.1440-1819.2011.02205.x. [DOI] [PubMed] [Google Scholar]
- Sarisoy G, Kacar OF, Pazvantoglu O, et al. Temperament and character traits in patients with bipolar disorder and associations with attempted suicide. Comprehensive Psychiatry. 2012;53:1096–1102. doi: 10.1016/j.comppsych.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Schaffer A, Isometsa ET, Tondo L, et al. International Society for Bipolar Disorders Task Force on Suicide: Meta-analyses and meta-regression of correlates of suicide attempts and suicide deaths in bipolar disorder. Bipolar Disorders. 2014a;17:1–16. doi: 10.1111/bdi.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaffer A, Sinyor M, Reis C, et al. Suicide in bipolar disorder: Characteristics and subgroups. Bipolar Disorders. 2014b;16:732–740. doi: 10.1111/bdi.12219. [DOI] [PubMed] [Google Scholar]
- Shabani A, Teimurinejad S, Kokar S, et al. Suicide risk factors in Iranian patients with bipolar disorder: A 21-month follow-up from BDPF study. Iranian Journal of Psychiatry and Behavioral Sciences. 2013;7:16–23. [PMC free article] [PubMed] [Google Scholar]
- Sher L, Carballo JJ, Grunebaum MF, et al. A prospective study of the association of cerebrospinal fluid monoamine metabolite levels with lethality of suicide attempts in patients with bipolar disorder. Bipolar Disorders. 2006;8:543–550. doi: 10.1111/j.1399-5618.2006.00319.x. [DOI] [PubMed] [Google Scholar]
- Simon GE, Hunkeler E, Fireman B, et al. Risk of suicide attempt and suicide death in patients treated for bipolar disorder. Bipolar Disorders. 2007a;9:526–530. doi: 10.1111/j.1399-5618.2007.00408.x. [DOI] [PubMed] [Google Scholar]
- Simon NM, Zalta AK, Otto MW, et al. The association of comorbid anxiety disorders with suicide attempts and suicidal ideation in outpatients with bipolar disorder. Journal of Psychiatric Research. 2007b;41:255–264. doi: 10.1016/j.jpsychires.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Siris SG. Suicide and schizophrenia. Journal of Psychopharmacology. 2001;15:127–135. doi: 10.1177/026988110101500209. [DOI] [PubMed] [Google Scholar]
- Song JY, Yu HY, Kim SH, et al. Assessment of risk factors related to suicide attempts in patients with bipolar disorder. The Journal of Nervous and Mental Disease. 2012;200:978–984. doi: 10.1097/NMD.0b013e3182718a07. [DOI] [PubMed] [Google Scholar]
- Stange JP, Sylvia LG, da Silva Magalhaes PV, et al. Extreme attributions predict suicidal ideation and suicide attempts in bipolar disorder: Prospective data from STEP-BD. World Psychiatry. 2014;13:95–96. doi: 10.1002/wps.20093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storosum JG, Wohlfarth T, Gispende Wied CC, et al. Suicide risk in placebo-controlled trials of treatment for acute manic episode and prevention of manic-depressive episode. The American Journal of Psychiatry. 2005;162:799–802. doi: 10.1176/appi.ajp.162.4.799. [DOI] [PubMed] [Google Scholar]
- Sublette ME, Carballo JJ, Moreno C, et al. Substance use disorders and suicide attempts in bipolar subtypes. Journal of Psychiatric Research. 2009;43:230–238. doi: 10.1016/j.jpsychires.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suominen K, Mantere O, Valtonen H, et al. Gender differences in bipolar disorder type I and II. Acta Psychiatrica Scandinavica. 2009;120:464–473. doi: 10.1111/j.1600-0447.2009.01407.x. (with additional written communication from Isometsa E) [DOI] [PubMed] [Google Scholar]
- Swann AC, Dougherty DM, Pazzaglia PJ, et al. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. The American Journal of Psychiatry. 2005;162:1680–1687. doi: 10.1176/appi.ajp.162.9.1680. [DOI] [PubMed] [Google Scholar]
- Thibodeau MA, Welch PG, Sareen J, et al. Anxiety disorders are independently associated with suicide ideation and attempts: Propensity score matching in two epidemiological samples. Depress Anxiety. 2013;30:947–954. doi: 10.1002/da.22203. [DOI] [PubMed] [Google Scholar]
- Tidemalm D, Haglund A, Karanti A, et al. Attempted suicide in bipolar disorder: Risk factors in a cohort of 6086 patients. PLoS ONE. 2014;9:e94097. doi: 10.1371/journal.pone.0094097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tondo L, Baldessarini RJ, Hennen J, et al. Suicide attempts in major affective disorder patients with comorbid substance use disorders. The Journal of Clinical Psychiatry. 1999;60(Suppl 2):63–69. discussion 75–66, 113–116. [PubMed] [Google Scholar]
- Tondo L, Isacsson G, Baldessarini R. Suicidal behaviour in bipolar disorder: Risk and prevention. CNS Drugs. 2003;17:491–511. doi: 10.2165/00023210-200317070-00003. [DOI] [PubMed] [Google Scholar]
- Tondo L, Lepri B, Baldessarini RJ. Suicidal risks among 2826 Sardinian major affective disorder patients. Acta Psychiatrica Scandinavica. 2007;116:419–428. doi: 10.1111/j.1600-0447.2007.01066.x. (with additional written communication from Tondo L) [DOI] [PubMed] [Google Scholar]
- Tsai SY, Kuo CJ, Chen CC, et al. Risk factors for completed suicide in bipolar disorder. The Journal of Clinical Psychiatry. 2002;63:469–476. doi: 10.4088/jcp.v63n0602. [DOI] [PubMed] [Google Scholar]
- Tsai SY, Lee JC, Chen CC. Characteristics and psychosocial problems of patients with bipolar disorder at high risk for suicide attempt. Journal of Affective Disorders. 1999;52:145–152. doi: 10.1016/s0165-0327(98)00066-4. [DOI] [PubMed] [Google Scholar]
- Umamaheswari V, Avasthi A, Grover S. Risk factors for suicidal ideations in patients with bipolar disorder. Bipolar Disorders. 2014;16:642–651. doi: 10.1111/bdi.12179. [DOI] [PubMed] [Google Scholar]
- Undurraga J, Baldessarini RJ, Valenti M, et al. Suicidal risk factors in bipolar I and II disorder patients. The Journal of Clinical Psychiatry. 2012;73:778–782. doi: 10.4088/JCP.11m07041. [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Haukka J, et al. Differences in incidence of suicide attempts during phases of bipolar I and II disorders. Bipolar Disorders. 2008;10:588–596. doi: 10.1111/j.1399-5618.2007.00553.x. [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Mantere O, et al. Prospective study of risk factors for attempted suicide among patients with bipolar disorder. Bipolar Disorders. 2006;8:576–585. doi: 10.1111/j.1399-5618.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Mantere O, et al. Suicidal behaviour during different phases of bipolar disorder. Journal of Affective Disorders. 2007;97:101–107. doi: 10.1016/j.jad.2006.05.033. [DOI] [PubMed] [Google Scholar]
- Watkins HB, Meyer TD. Is there an empirical link between impulsivity and suicidality in bipolar disorders? A review of the current literature and the potential psychological implicatio ns of the relationship. Bipolar Disorders. 2013;15:542–558. doi: 10.1111/bdi.12090. [DOI] [PubMed] [Google Scholar]
- Weeke A, Vaeth M. Excess mortality of bipolar and unipolar manic-depressive patients. Journal of Affective Disorders. 1986;11:227–234. doi: 10.1016/0165-0327(86)90074-1. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Choi YM. Impact of psychotropic drugs on suicide and suicidal behaviors. Bipolar Disorders. 2013;15:594–621. doi: 10.1111/bdi.12098. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Martinez J, Young D, et al. Comorbid bipolar disorder and borderline personality disorder and history of suicide attempts. Journal of Personality Disorders. 2013;28:358–364. doi: 10.1521/pedi_2013_27_122. [DOI] [PubMed] [Google Scholar]
- Zisook S, Anzia J, Atri A, et al. Teaching evidence- based approaches to suicide risk assessment and prevention that enhance psychiatric training. Comprehensive Psychiatry. 2013;54:201–208. doi: 10.1016/j.comppsych.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]