Abstract
Objective:
A non-invasive diagnostic technique for abdominal adhesions is not currently available. Capture of abdominal motion due to respiration in cine-MRI has shown promise, but is difficult to interpret. This article explores the value of a complimentary diagnostic aid to facilitate the non-invasive detection of abdominal adhesions using cine-MRI.
Method:
An image processing technique was developed to quantify the amount of sliding that occurs between the organs of the abdomen and the abdominal wall in sagittal cine-MRI slices. The technique produces a “sheargram” which depicts the amount of sliding which has occurred over 1–3 respiratory cycles. A retrospective cohort of 52 patients, scanned for suspected adhesions, made 281 cine-MRI sagittal slices available for processing. The resulting sheargrams were reported by two operators and compared with expert clinical judgment of the cine-MRI scans.
Results:
The sheargram matched clinical judgment in 84% of all sagittal slices and 93–96% of positive adhesions were identified on the sheargram. The sheargram displayed a slight skew towards sensitivity over specificity, with a high positive adhesion detection rate but at the expense of false positives.
Conclusion:
Good correlation between sheargram and absence/presence of inferred adhesions indicates quantification of sliding motion has potential to aid adhesion detection in cine-MRI.
Advances in knowledge:
This is the first attempt to clinically evaluate a novel image processing technique quantifying the sliding motion of the abdominal contents against the abdominal wall. The results of this pilot study reveal its potential as a diagnostic aid for detection of abdominal adhesions.
INTRODUCTION
Abdominal adhesions are formations of fibrous tissue that develop between abdominal structures in response to tissue damage. They are a major cause of morbidity and place a substantial burden on healthcare worldwide having been reported to cost $1.3bn annually in the USA (in 1994) and ~€60 mil per year in Sweden.1–3 Diagnosis of adhesions remains a challenge, with explorative laparoscopic surgery the primary diagnostic tool. Surgery itself is widely regarded to be the leading cause of adhesions and a non-invasive diagnostic technique could be of significant benefit.4,5
Cine-MRI is a dynamic imaging modality that can capture motion of the abdominal contents. Cine-MRI has shown potential for adhesion detection with two studies indicating sensitivities of at least 93% when compared with gold standard surgical confirmation.6,7 Their detection relies on examination of movement of the abdominal contents with respiratory motion, also called “visceral slide”. The radiologist qualitatively examines this motion for regions where displacement appears reduced or hindered—potentially linking them to the presence of adhesions. Movement examination remains a time consuming challenge and a diagnostic aid may be of benefit, particularly for less experienced radiologists in training.8
We have previously described an image processing technique to aid abdominal wall adhesion detection in cine-MRI.9 The principal output of the technique is a “sheargram”, depicting the cumulative amount of sliding which occurs along the abdominal wall. The technique was trialled on synthetic data and a preliminary set of clinical images. Tests confirmed the ability of the sheargram to accurately measure shear and showed that a drop in shear could correspond to surgically confirmed adhesions.9 This article further explores clinical application of the technique through a pilot study. Correlation of the sheargram with clinical judgment is used as a metric to clarify its potential as an indicator for adhesive pathology.
METHOD
The sheargram
The movement of the diaphragm during respiration induces an inferior–superior displacement of the abdominal contents which is captured on cine-MRI. Simultaneously the abdominal wall exhibits a different, anteroposterior mode of motion. The disconnect between the motion of the two structures creates a movement discontinuity along the interface between the abdominal contents and abdominal wall. In the healthy, the abdominal contents slide unimpeded at the discontinuity but where adhesive pathology exists, sliding is inhibited.
The sheargram technique quantifies the amount of sliding at the interface between the abdominal wall and abdominal contents. First, the images are segmented to create two new sets of images: frames containing only the abdominal contents and frames with the abdominal contents removed. Image registration is then used to track the movement of objects in each of the two regions independently. Using the quantified displacement information generated by the image registration, the shear at the sliding interface between the two regions can be calculated. Shear is used as a quantifiable analogue for sliding. The output of the technique is a “sheargram” depicting the cumulative amount of sliding which has occurred over the entire dynamic imaging sequence. A region of reduced shear on the sheargram is expected to correlate with a structure adhered to the abdominal wall: this principle is investigated in this paper via a pilot study.
Pilot study
A cohort of 52 patients were randomly selected from a retrospective pool of 106 patients who had a dynamic MRI for undiagnosed abdominal pain with suspected adhesions. The MRI scans were undertaken on a 1.5 T Siemens Avanto scanner. The cine-MRI scanning protocol is similar to that previously described by Leinemann et al: it is a true-FISP, with echo and relaxation times of 1.53 and 3.66 ms, flip angle of 60°, a matrix size of 192 × 256, slice thickness of 5 mm, 0.4 s per frame and 30 frames per imaged slice.6,9 Patients were positioned supine and instructed to bear down and breathe deeply to induce suitable superior–inferior movement of the abdominal organs. No patient preparation or contrast was used. Typically, five sagittal slices were acquired at the midline, left/right paramedian and left/right lateral at the ascending/descending colon. The 52 patients contained 281 unique dynamic sagittal slices.
The quality of the dynamic images is dependent on the amount of respiratory motion generated by the patient. Small amounts of respiratory motion induce less movement of the abdominal contents, less shear at the abdominal wall and are therefore difficult to interpret. Each slice was graded as high and low quality data, based on the amount of respiratory motion. For example, a dynamic sagittal slice which contained less than one full respiratory cycle was deemed to be low quality. We excluded low quality slices from this pilot study because we sought proof of principle. This removed potential complications introduced by unsuitable data for a clearer assessment of the correlation of the reduced shear in the sheargram to adhesions identified on the cine-MRI. Approximately 50% (141/281) sagittal slices (from 37 patients) were judged to be of high quality and processed.
Two operators reported on all 141 sheargrams: one a technical expert in the image processing technique, the other a consultant radiologist with experience in cine-MRI reporting for adhesion diagnosis. Prior to commencing the pilot study, the radiologist was trained in sheargram interpretation using a training dataset of 10 sheargrams accompanied by their cine-MRI videos. Both reporters came to an independent judgment on whether the sheargram contained a reduction of shear which could correspond to an adhesion. The reporting procedure allowed the reporters three options in their judgment of the sheargram:
“Yes”, there is a significant reduction in shear inferring an adhesion is present
“No”, the sheargram depicts a normal shear pattern inferring no adhesions
“Equivocal”, the sheargram shows a reduction in shear but it is not clear whether it is sufficient to infer the presence of an adhesion
The radiologist examined each of the cine-MR image sequences after reviewing the sheargram to confirm the presence of an adhesion in that slice. This reporting procedure emulated how sheargrams might be used clinically. The same scoring system was used (“yes”, “no” or “equivocal”) for the radiologist’s examination of the cine-MRI. The original diagnostic reports of the cine-MRIs were also available for comparison.
Analysis primarily compared sheargram interpretation with the radiologist’s clinical examination of the cine-MRI. The level of correlation was adjudicated based on percentage agreement between the two. The cohort size ensured statistical significance in correspondence between sheargram and radiologist examination if correlation exceeded 63% (to a p value of <0.01). The study therefore permitted evaluation of whether the sheargram produced results that were representative of the actual shear occurring in the images and whether this corresponded to clinically indicated adhesive pathology.
RESULTS
Figure 1 shows four example sheargrams: two with inferred adhesions and two healthy slices. The sheargrams display a coloured band overlaid on the MRI image, which depicts the amount of shear: red indicating high shear, blue—low shear. The sharp reductions in shear observed in Figure 1a,b correspond to areas with inferred adhesions, as marked by the white arrows. The lack of a sharp shear reduction in Figure 1c,d should indicate smooth sliding and an absence of adhesions.
Figure 1.

Two examples where the sheargram correctly correlated with positively inferred adhesions (a and b) and two healthy sheargrams which correctly correlated with an absence of adhesions (c and d). White arrows and lines annotate location and extent of each adhesion.
The primary goal of the analysis was to correlate sheargram interpretation with expert clinical opinion of the cine-MRI. The scoring system (“yes”, “no”, “equivocal”) creates nine possible combinations for comparison, summarised in Table 1.
Table 1.
The nine categories used to classify agreement between sheargram and clinical decision
| Classification number | Adhesion inferred on cine-MRI? | Adhesion identified on sheargram? | Broad agreement classification |
| 1 | Yes | Yes | Agreement (true positives/negatives) |
| 2 | No | No | |
| 3 | Equivocal | Equivocal | |
| 4 | Equivocal | Yes | Partial agreement |
| 5 | Equivocal | No | |
| 6 | Yes | Equivocal | |
| 7 | No | Equivocal | |
| 8 | No | Yes | Disagreement (false positives/negatives) |
| 9 | Yes | No |
Broader groupings of agreement, partial agreement and disagreement are also indicated.
The classification system described in Table 1 formed the basis for assessing correlation between sheargram and clinical decision of the cine-MRI. The greyed out categories shown in Table 1 were not used in subsequent results and analysis. These are cases where the radiologist made an equivocal clinical decision on the cine-MRI and therefore the presence of an adhesion is ambiguous and unknown. These cases do not present a definitive answer for the sheargram result to be compared against. There was only one sagittal slice where an equivocal cine-MRI judgment was made, leaving 140 sagittal slices remaining for comparison with the sheargram.
The nine different agreement classifications can be collated to form three broad classification categories, as shown in Table 1. Figure 2 plots the number of sagittal slices in each of the broad classification categories to provide a coarse overview of the correlation.
Figure 2.
Number of sheargrams which agree/disagree with clinical decision on adhesions in the cine-MRI (broad classification).
Figure 2 shows a strong correlation between the interpretation of the sheargram and clinical opinion. 82 and 78% of sheargrams, judged by the radiologist and technical expert, respectively, agreed with the clinical judgment on the presence of adhesions; 11 and 10% of cases disagreed.
A breakdown of the correlation for each of the possible combinations in Table 1 is presented in Figure 3. For clarification, true positives, true negatives, false positives and false negatives in this study refer to the comparison of the sheargram interpretation with adhesions identified by the radiologist on the cine-MRI, i.e. a “true positive” refers to a reduction in shear on the sheargram that correctly correlates to an inferred adhesion on the cine-MRI.
Figure 3.
Correlation between the sheargram and clinically inferred adhesions on the cine-MRI for each of the two reporters represented as pie charts and 2 × 2 contingency tables. The numbers on the charts are the number of sagittal slices (total sagittal slices = 140).
In the pie charts, the green-shaded segments highlight the true positives and true negatives, the red segments the false positives and false negatives and the yellow portions are partial agreements. The contingency tables in Figure 3 exclude all equivocal cases to permit an estimate of sensitivity and specificity. The sensitivity was 96% for the radiologist and 90% for the technical expert. The vast majority of slices without adhesions were also correctly identified on the sheargram, with the specificity approaching 90% (87% for the radiologist and 88% for the technical expert) when excluding all equivocal sheargram judgments.
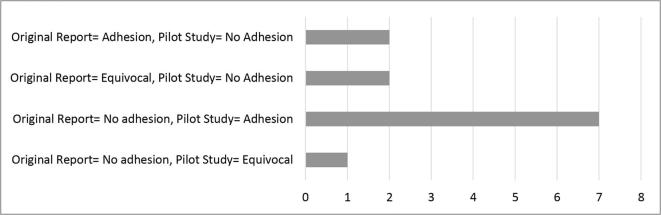
The original diagnostic cine-MRI reports were also available for interrogation. The original report was produced by the same radiologist that participated in this pilot study. Comparison between the original report and the clinical decision made during this pilot study reveals 12 cases where the radiologist changed their opinion after reviewing the sheargram. The changes are summarised in Figure 4.
Figure 4.
The 12 changes made between the original cine-MRI report and the radiologist's clinical decision in the pilot study.
The majority of changes involved re-designation from negative to positive presence of adhesions. The identification of these additional adhesions were all paired with a positive or equivocal sheargram, potentially indicating its influence on clinical decisions.
DISCUSSION
We have previously presented a technique to quantify the sliding motion of the abdominal contents against the abdominal wall and tested its ability to measure sliding.9 With this pilot study, we aim to verify the potential clinical usefulness of the sheargram to aid detection of abdominal wall adhesions. The primary metric for assessment was how well the interpretation of the sheargram matched clinical interpretation of the cine-MRI.
Sheargram correlation with cine-MRI
Good agreement between sheargram and clinical judgment is indicated in Figures 2 and 3. The combination of complete and partial agreements accounted for 89 and 90% of cases for the radiologist and technical expert, respectively. Calculation of a conclusive figure for the level of agreement depends on the interpretation of an “equivocal” sheargram. Notably, an equivocal reduction in shear on a sheargram still draws the attention of the reporter to that specific location. Consequently, there is justification that an equivocal judgment is more aligned to a positive sheargram than a negative. Applying this justification and reclassifying “equivocal” sheargrams as a positive “yes ”, results in the following figures:
Overall agreement: The sheargram correctly correlated with clinical opinion in 84% of cases for both reporters. This comfortably exceeded the 63% agreement required for statistical significance (i.e. p value < 0.01).
Detection of positive adhesions: Sensitivities of 96% (26/27) and 93% (25/27) were recorded for the radiologist and technical expert, respectively.
Identification of healthy cases: The proportion of healthy sagittal slices that correctly correlated with negative sheargrams is given by a specificity of 81% for both reporters.
The high percentage of adhesions correctly identified on the sheargram and the lower percentage of agreement for negative cases highlight a skew towards sensitivity over specificity. There were 14 and 12 false positives compared with 1 and 2 false negatives for the radiologist and technical expert, respectively (Figure 3). The intention of the sheargram is for it to become a diagnostic aid; designed to alert the radiologist to suspicious areas with possible adhesions. Therefore, a high sensitivity is favoured as it is preferable to draw the attention of the reporter to suspected adhesions subsequently deemed to be healthy, rather than miss adhesions.
The analysis has assumed each slice is independent; however, some slices belong to the same patient and potentially demonstrate correlation with one another. Considering multiple slices within each patient: 63% of patients had agreement between sheargram and cine-MRI in all slices; 34% had one disagreement and 3% had two disagreements. The spread of disagreement between sheargram and expert opinion was shared across the patient cohort rather than concentrated in particular patients and implies that two slices belonging to the same patient are no more likely to both lead to a disagreement than two slices from different patients. Consequently, it was appropriate to treat the sagittal slices as independent entities.
The evidence presented supports the premise that the sheargram produces a shear profile representative of the sliding that occurs along the abdominal wall and that a reduction in quantified shear correlates to adhesive pathology.
Where did it fail?
There was a single sheargram which produced a healthy shear profile (judged by both reporters) in which an adhesion was identified on the cine-MRI resulting in a false negative. This case is shown in Figure 5a. The technical expert recorded a second false negative, shown in Figure 5b.
Figure 5.

The two false negative sheargram examples from the pilot study.
At the area of the adhesion in Figure 5a there was considerable lateral movement through the imaging plane. The adhered bowel loop was only visible in approximately half of the 30-frame dynamic image sequence. Substantial movement occurring through the imaging plane at the sliding interface is interpreted as displacement by the image registration algorithm and culminates in anomalous shear. The case in Figure 5b can be explained by a difference in sheargram interpretation. The technical expert noted that the reduction in shear in the lower abdomen, although significant, was in the absence of structure adjacent to the abdominal wall and was therefore discounted. The radiologist documented bowel close enough to the abdominal wall to contribute to shear and an adhesion to the pelvic floor and therefore reported a positive adhesion.
Changes in clinical opinion
The radiologist originally reported the cine-MRI scans at least 5 months prior to undertaking this pilot study. This ensured that the radiologist was not influenced by recent memory. Alterations between the original report and this pilot study have greater pertinence as inter-operator variability is negated.
The majority, 10/12, of the alterations shown in Figure 4 aligned with the judgment made on the sheargram. This insinuates the sheargram influenced the interpretation of the cine-MRI. The two remaining sagittal slices were from the same patient and the radiologist’s sheargram interpretation matched the original report. The technical expert made an “equivocal” judgment on these two sheargrams implying it was a challenging scan to interpret. There were seven alterations in opinion from “no adhesion” (on the original report) to a positive adhesion, potentially resulting in identification of new adhesions previously missed. However, these potential additional adhesions cannot be confirmed without surgery. The evidence suggests the sheargram had the capability to inform adhesion identification to the abdominal wall. However, it should be stressed that the radiologist did not review the transaxial slices in this pilot study which were available when constructing the original report. This difference could also account for some of the changes in clinical opinion.
Limitations
This paper acknowledges that the gold standard diagnostic method for abdominal adhesion diagnosis is explorative surgery, not cine-MRI. However, in the absence of surgical confirmation, comparison of the sheargram to cine-MRI serves as a practical alternative and permitted a much larger patient cohort to be evaluated. Moreover, a recent in-house assessment confirmed a low false positive rate of cine-MRI when compared with surgical confirmation of identified adhesions: providing circumstantial evidence for the sheargram’s correlation with surgery. However, confirming the interpretation of the sheargram and cine-MRI to surgical findings remains a necessity to determine the true diagnostic usefulness of the technique.
Despite the demonstrated link between a drop in shear and inferred presence of adhesions, the true clinical benefit of the technique has yet to be determined. There is a disconnect between detecting adhesions and determining their contribution to clinical presentation. However, non-invasive detection would provide the clinician with additional information with which to make a more informed decision on diagnosis and surgical intervention.
Exclusion criteria ensured that only images of high quality would be evaluated. We argue that this is appropriate for this proof of principle exercise, permitting analysis on real but suitable data. This should be taken into consideration when interpreting the results. Only 50% of the data was considered as “high quality”. Patient compliance was the primary source of poorer quality data and this invites an opportunity to refine the scanning protocol. Over 90% of the poor quality data could be attributed to a lack of respiratory motion that induced insufficient displacement of the abdominal contents. Trials are underway to investigate the training of participants (via an instructional video) to improve breathing during image acquisition, complemented by simplified instructions. The reliability of the sheargram on lower quality data also needs to be ascertained.
Although the sheargram is produced from a quantitative parameter, interpretation of the sheargram itself introduces subjectivity. The two reporters in this pilot study were from differing backgrounds and therefore provide a good indication of the inter-operator variability in sheargram interpretation. 85% (120/141) of sheargram interpretations between the two reporters agreed, 13% (19/141) partially agreed and 1.4% (2/141) disagreed. The notable number of partial agreements can be ascribed to the technical expert reporting more equivocally due to a lack of experience in diagnostic decision-making. 76% of the partial agreements were related to an observed drop in shear in the lower abdomen. A gradual reduction in shear at the lower extremities of the abdomen is often observed in healthy individuals. This can lead to a sometimes ambiguous judgment on whether the reduction is significant and sharp enough to be abnormal or whether it is gradual and mild enough to be normal. The partial agreements are less concerning than the two cases where a complete disagreement was recorded. One of the two cases where a complete sheargram disagreement was recorded is shown in Figure 5b, while the other can be accounted for by a difference in clinical experience. Greater objectivity would benefit the technique but a more automated process would require considerable effort to implement. Arguably, the variability between the two reporters can be considered acceptable.
The false negative case in Figure 5a resulting from out-of-plane motion highlights a fundamental problem with imaging a three-dimensional (3D) object in a two-dimensional plane. Progression to 3D pseudo-dynamic imaging to capture a complete view of movement within the entire abdomen is being considered. Successful implementation of 3D imaging would also permit movement analysis of structures deeper within the abdominal cavity rather than being limited to its perimeter, as in the current two-dimensional implementation.
CONCLUSION
Our sheargram technique for measuring the sliding motion of the abdominal contents against the abdominal wall in cine-MRI has already been described. This pilot study confirms the sheargram is capable of matching areas of reduced shear to inferred adhesive pathology identified by expert clinical judgment on cine-MRI. A subset of approximately 50% of the most suitable data was selected from a total of 281 sagittal slices from a cohort of 52 patients. The sheargram matched the final clinical cine-MRI adjudication in 84% of cases and at least 93% of all located adhesions were identified on the sheargram. Arguably, the sheargram influenced decision-making since changes in the radiologist’s opinion were observed between the original report and the pilot study after examination of the sheargram. Identification of seven potentially new adhesions were made, with all seven matching interpretation of the sheargram. However, poor patient compliance indicates the need to simplify the breathing procedure and provide clearer instructions along with clarification of the minimum amount of respiratory motion required.
The evidence presented has indicated that visceral slide quantification presented in a sheargram can be a diagnostic aid for cine-MRI interpretation. This interim study has provided confidence that the technique deserves further development and a more thorough clinical trial is warranted.
FUNDING
The Bardhan Research and Education Trust of Rotherham.
ACKNOWLEDGEMENTS
The authors would like to thank the Bardhan Research and Education Trust of Rotherham (BRET) for supporting this research and Dr Paul Spencer for his input leading up to this work.
Contributor Information
David Randall, Email: drandall1@sheffield.ac.uk.
Frank Joosten, Email: fjoosten@rijnstate.nl.
Richard Peter Ten Broek, Email: richard.tenbroek@radboudumc.nl.
Richard Gillott, Email: richard.gillott@rothgen.nhs.uk.
Karna Dev Bardhan, Email: Bardhan.sec@rothgen.nhs.uk.
Chema Strik, Email: chema.strik@radboudumc.nl.
Wiesje Prins, Email: wprins@rijnstate.nl.
Harry van Goor, Email: harry.vangoor@radboudumc.nl.
John Wesley Fenner, Email: j.w.fenner@sheffield.ac.uk.
REFERENCES
- 1.ten Broek RP, Issa Y, van Santbrink EJ, Bouvy ND, Kruitwagen RF, Jeekel J, et al. Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ 2013; 347: f5588. doi: 10.1136/bmj.f5588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tingstedt B, Isaksson J, Andersson R. Long-term follow-up and cost analysis following surgery for small bowel obstruction caused by intra-abdominal adhesions. Br J Surg 2007; 94: 743–8. doi: 10.1002/bjs.5634 [DOI] [PubMed] [Google Scholar]
- 3.Ray NF, Denton WG, Thamer M, Henderson SC, Perry S. Abdominal adhesiolysis: inpatient care and expenditures in the United States in 1994. J Am Coll Surg 1998; 186: 1–9. doi: 10.1016/S1072-7515(97)00127-0 [DOI] [PubMed] [Google Scholar]
- 4.Brüggmann D, Tchartchian G, Wallwiener M, Münstedt K, Tinneberg HR, Hackethal A. Intra-abdominal adhesions: definition, origin, significance in surgical practice, and treatment options. Dtsch Arztebl Int 2010; 107: 769–75. doi: 10.3238/arztebl.2010.0769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dubuisson J, Botchorishvili R, Perrette S, Bourdel N, Jardon K, Rabischong B, et al. Incidence of intraabdominal adhesions in a continuous series of 1000 laparoscopic procedures. Am J Obstet Gynecol 2010; 203: 111.e1–111.e3. doi: 10.1016/j.ajog.2010.03.031 [DOI] [PubMed] [Google Scholar]
- 6.Lienemann A, Sprenger D, Steitz HO, Korell M, Reiser M. Detection and mapping of intraabdominal adhesions by using functional cine MR imaging: preliminary results. Radiology 2000; 217: 421–5. doi: 10.1148/radiology.217.2.r00oc23421 [DOI] [PubMed] [Google Scholar]
- 7.Lang RA, Buhmann S, Hopman A, Steitz HO, Lienemann A, Reiser MF, et al. Cine-MRI detection of intraabdominal adhesions: correlation with intraoperative findings in 89 consecutive cases. Surg Endosc 2008; 22: 2455–61. doi: 10.1007/s00464-008-9763-9 [DOI] [PubMed] [Google Scholar]
- 8.Fenner J, Wright B, Emberey J, Spencer P, Gillott R, Summers A, et al. Towards radiological diagnosis of abdominal adhesions based on motion signatures derived from sequences of cine-MRI images. Phys Med 2014; 30: 437–47. doi: 10.1016/j.ejmp.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 9.Randall D, Fenner J, Gillott R, ten Broek R, Strik C, Spencer P, et al. A novel diagnostic aid for detection of intra-abdominal adhesions to the anterior abdominal wall using dynamic magnetic resonance imaging. Gastroenterol Res Pract 2016; 2016: 1–6. doi: 10.1155/2016/2523768 [DOI] [PMC free article] [PubMed] [Google Scholar]