Abstract
Background
Maternal morbidity and mortality is still a major public health issue in low- and middle-income countries such as Cambodia. Improving access to antenatal care (ANC) services for pregnant women has been widely recognized as one of the most effective means of reducing maternal mortality and morbidity. As such, this study examined the barriers for pregnant women living in rural, agricultural villages to accessing ANC based on data collected in the Ratanakiri province, one of the least developed provinces in Cambodia, using a combination of a community-based cross-sectional survey and a geographic information system (GIS).
Methods
A community-based cross-sectional survey was conducted among 377 mothers with children under the age of two living in 62 villages in the Ratanakiri province, Cambodia, in December 2015. Face-to-face interviews were conducted to ask mothers about their ANC service use, knowledge of ANC, barriers to accessing health facilities, and complications they experienced during the most recent pregnancy. At the same time, GIS data were also collected using a Global Positioning System (GPS) to accurately measure actual travel distance of pregnant women to access health facilities and to examine geographical and environmental barriers in greater detail.
Results
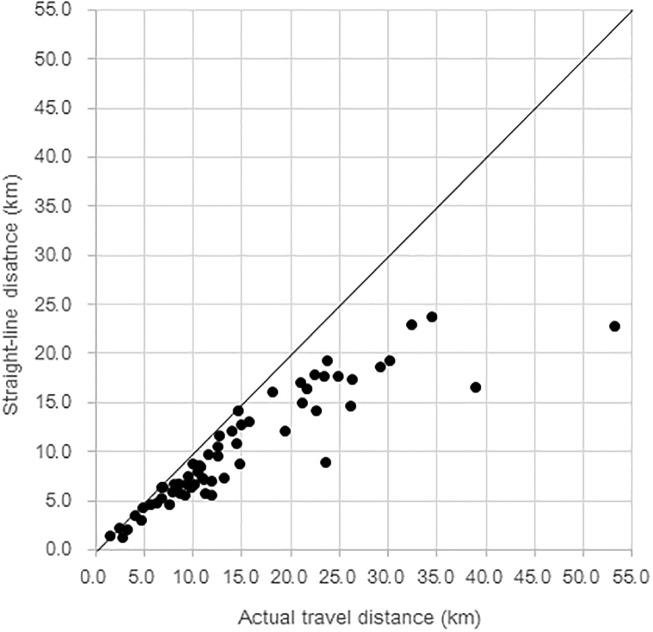
Only a third of the mothers met the recommendations made by the World Health Organization (WHO) of receiving ANC four times or more (achieved ANC4+), and a quarter of the mothers had never received ANC during their most recent pregnancy. Factors positively associated with achieving ANC4+ were mother’s secondary or higher education (adjusted odds ratio [AOR] = 5.50, 95% confidence interval [CI]: 1.74, 17.37), being aware that receiving ANC is recommended (AOR = 2.74, 95% CI: 1.25, 6.00), and knowledge about the recommended frequency for ANC (AOR = 2.26, 95% CI: 7.22). Actual travel distance was negatively associated with achieving ANC4+. Mothers who had to travel 10.0–14.9 km were 68% less likely (AOR = 0.32, 95% CI: 0.10, 0.99), and those who had to travel 15.0 km or longer were 79% less likely (AOR = 0.21, 95% CI: 0.07, 0.62) to have achieved ANC 4+, both compared to those who travelled 5.0 km or less. While most previous studies have used a straight-line to measure distance traveled, this study much more accurately measured the actual distance traveled by using a GIS. As a result, there was a statistically significant discrepancy between actual travel distance and straight-line distance.
Conclusions
This study revealed promoting factors and barriers for ANC use among pregnant women living in remote, agricultural villages in Cambodia. Furthermore, this study highlights the importance of measuring travel distances accurately to ensure that targeted interventions for ANC are not misguided by straight-line distances. The methodology used in this study can be applied widely to other developing countries, especially in remote areas with limited road networks where there may be a large discrepancy between actual and straight-line distances.
Introduction
Maternal morbidity and mortality is still a serious public health issue in low- and middle-income countries, even though there has been remarkable progress in improving maternal health since the Millennium Development Goals (MDGs) were adopted in 2000. An estimated 303,000 women died because of complication of pregnancy and childbirth in 2015, most of which occurred in rural, resource-limited settings in developing countries [1–3]. Lack of access to local health care services, including antenatal care (ANC) services for pregnant women, has been consistently reported as one of the key obstacles to reduce maternal mortality and morbidity [4,5].
The continuum of care (CoC) in maternal, neonatal, and child health (MNCH) has gained much attention as a means to reduce the burden of maternal deaths, neonatal deaths, and deaths among children under five, especially in low- and middle-income countries [6]. Enabling pregnant women to continuously receive ANC, skilled birth attendance at delivery, and postnatal care (PNC) are reported to have a significant positive impact on overall MNCH indicators [7]. In particular, receiving ANC has been shown to be one of, if not the best, indicator of positive pregnancy outcomes, significantly contributing to the reduction of maternal morbidity and mortality [5,8]. ANC are used to identify pregnancy risks and provide care for pregnant women who might be susceptible to a wide variety of potentially fatal conditions such as HIV, malaria, tuberculosis, anemia, and malnutrition [5,9,10]. Additionally, receiving ANC has been found to increase subsequent use of maternal and child health services, especially skilled birth attendance [11,12]. The World Health Organization (WHO) recommends that pregnant women receive ANC at least four times, comprising of tetanus toxoid vaccination, screening of infections, and identification of danger signs of pregnancy complications [13].
However, access to ANC is quite limited in most developing countries, and ANC use is often reported to be low [5]. Variety of barriers to access ANC have been reported in several previous studies [5,8,14–19]: sociocultural and psychological barriers included customs of keeping pregnancy a secret, reliance on traditional/alternative antenatal practices, influence of family members, and reluctance caused by poor attitudes of medical staff [20–25]. ANC use can also be hindered by a lack of knowledge about ANC and benefits of attendance as well as unawareness of health facilities that provide ANC [23,26]. Costs were also reported to be significant barriers: direct costs include medical care fees and transportation fees, while indirect costs include time off work and waiting times at clinic [17,27,28]. Additionally, several studies pointed out that the distance to the health facilities is one of the major barriers that were raised by the majority of pregnant women in resource-limited settings, especially in rural, agricultural villages [8,15,18,19].
Despite the importance of distance to health facilities, only a few studies have accurately measured the actual travel distance between the villages where pregnant women live and the nearest health center where they can receive ANC. Most previous studies have used straight-line distances (Euclidean distances) as a proxy for actual travel distance [29] or relied on distance information obtained from respondents [18,19]. In rural areas with limited infrastructure and road systems, it is quite common that the actual travel distance is much longer than the straight-line distance. Using straight-line distances have been considered inaccurate, because it ignores geographical/environmental barriers such as rivers, mountains, road types, and road undulation [30,31]. Although straight-line distance can be measured easily on a map, relying on this data can result in grossly underestimating the burden put on pregnant women to access ANC. Additionally, respondents’ answers regarding distance to the nearest health facility can be unreliable and may vary even if they live in the same village. As lack of access has been established as a barrier to women receiving ANC, any intervention targeting these women needs to accurately take into account the actual travel distance and geographical/environmental obstacles they may have to face during their travels. To this end, we focused on accurately measuring the travel distance using a geographic information system (GIS) [31].
Cambodia is one of the Southeast Asian countries that has been suffering from low utilization of maternal and child health services as well as high maternal and child mortality. In 2015, Cambodia had the third highest rates for neonatal mortality (15 per 1,000 live births), under-five mortality (29 per 1,000 live births), and maternal mortality (161 per 100,000 live births) in Southeast Asia (regional average: 13 per 1,000, 27 per 1,000, and 110 per 100,000 live births, respectively) [32]. A recent study in Cambodia demonstrated that as many as 40% of Cambodian women did not receive all three MNCH services (namely ANC), delivery with skilled-birth attendance, and PNC in 2010 [11].
As observed in many developing countries, there is substantial regional variation in the use of maternal and child health services in Cambodia. In the Ratanakiri province, consisting mainly of rural, agricultural villages with the lowest socioeconomic standards and limited infrastructure in the country, the percentage of pregnant women and mothers who received three kinds of MNCH services was only 24% compared to 96% in Phnom Penh in 2010 [11]. Additionally, in the same Ratanakiri province, the Demographic Health Survey (DHS) conducted in 2014 found that less than half (48.4%) of the 76 pregnant women were reported to have received ANC four times or more, which percentage was much lower than that in Phnom Penh (88.0%) [33].
Despite the serious situation, few studies have examined the barriers for pregnant women to receiving ANC in rural Cambodia. Moreover, no previous studies have accurately measured actual travel distance and examined geographical/environmental obstacles for pregnant women to reach health facilities that provide ANC.
This study, therefore, aims to 1) describe the current situation of ANC use among pregnant women living in rural, agricultural villages in the Ratanakiri province, Cambodia, and to 2) examine barriers to accessing ANC, using data from a community-based cross-sectional survey and a GIS. Based on the results of this study, factors associated with ANC use, barriers to access ANC, and the importance of measuring distance accurately for developing strategies to increase ANC are discussed.
Methods
Study site
This study was conducted as a baseline survey for an intervention study, which is currently carried out to integrate community-based malaria control and MNCH services in the Ratanakiri province, Cambodia. Ratanakiri province is one of the least developed provinces, with low health standards and socioeconomic status, in the country [33]. It is located in the north-eastern part of the country and shares its borders with Lao People’s Democratic Republic (PDR) and Vietnam. Residents, including 13 ethnic minority groups, generally live in villages of 20–60 families and mainly engage in subsistence shifting agriculture, rice farming, and plantation of rubber, cashew, and cassava.
Multi-stage sampling was conducted to select study villages. First, 12 out of 27 health centers in Ratanakiri, which cover villages where village malaria workers (VMW) reside and work on malaria control for their villagers, were chosen (VMW villages). Out of the 12 health centers, seven were selected based on accessibility throughout the year: Andaung Meas, Chomrom Bay Sruk, Kachanh, Lumphat, Ochum, Oyadav, and Taveng. Out of 73 VMW villages under the seven health centers, ten villages under the Ochum health center were excluded due to difficulty of access during the rainy season, and one village under the Andaung Meas health center was excluded because of the absence of eligible interviewees at the time of the survey. As a result, 62 VMW villages were selected for the study.
Data collection
Survey data
Data were collected from December 23 to 30, 2015, through interviews with mothers with children under two living in the selected VMW villages in the Ratanakiri province. To conduct face-to-face interviews, a semi-structured questionnaire was developed. The majority of the questions were drawn from three questionnaires: 1) Cambodia Demographic Health Survey 2014 [33], 2) questionnaires that we have already used in Cambodia for our previous studies on VMWs and mothers with children under five [34–36], and 3) a questionnaire that we used for the Ghana EMBRACE Implementation Research Project in collaboration with Ghana Health Services [7,37]. Specifically, the questionnaire contained questions regarding the following: a) mothers’ and their families’ socio-demographic characteristics; b) history of receiving MNCH services (frequency and timing of receiving ANC, delivery with SBA, PNC); c) history of malaria infection and testing during pregnancy (frequency, timing, through MNCH services or not); d) barriers to accessing health facilities; e) health-related behavior of mothers for themselves and their children under two (bednet use, breastfeeding, complementary feeding, treatment seeking behavior, etc.); f) mothers’ complications during pregnancy and childbirth (anemia, bleeding, etc.); g) children’s complications (fever, difficult breathing, etc.); and h) history of infectious diseases (malaria, diarrhea, and pneumonia, etc.). The questionnaire was first developed in English, translated into Khmer by Cambodian health experts, and then double-checked by other Khmer health experts to make sure that the translation was accurate.
Seventeen surveyors were hired to visit each survey participant’s residence and to conduct face-to-face interviews. Prior to the interview, experts from the National Center for Parasitology, Entomology, and Malaria Control, Cambodia (CNM) and lead researchers conducted a one-day training for the surveyors to explain the details of the questionnaire and how to conduct the interviews.
Surveyors were divided into four groups and visited 62 study villages within eight days. (Each survey team visited 14–17 villages in total.) In each study village, surveyors visited residences of mothers with children under two based on the information provided by VMWs. We recruited all mothers with children under two, who were available at the time of the survey. If mothers were absent, a second attempt was made within the same day. Those who were absent during the second visit and who were physically or mentally unable to provide informed consent were excluded from the study. There were no mothers who refused to participate in the study. A total of 388 mothers were interviewed. During the interview, surveyors asked mothers to show them maternal health record book and confirmed the accuracy of mothers’ report about the number and timing of ANC visits. Out of the 388 mothers interviewed, 11 were excluded from analysis because of missing data.
GPS data collection and analysis
Simultaneously with the survey, GPS data were collected to exactly measure actual travel distance between 62 villages and their nearest health center. Four GPS data collectors were hired and actually traveled from the center of each village to its nearest health center as taught by VMWs and/or study participants living in the village. Village center was designated as the starting point of the travel because households are clustered around the village center, where a meeting place or an open space with a well locates. Drivers traveled with with Holux m-241, a wireless GPS logger, which was set to record GPS data, including latitude, longitude, altitude, and time, every five seconds during each trip. Data were first entered into Excel 2016 through Holux exTour for Logger v2.1 software, and then into Arc Map 10.4, which was used to calculate actual travel distance between each village and its nearest health center. In addition, straight-line distance was also calculated using the same software, Arc Map 10.4, to compare with actual travel distance. Means of transportation and obstacles that mothers faced during their travel were asked in the face-to-face interview.
Data management, statistical analysis, and ethical considerations
All survey data were coded, entered into data analysis software with actual travel distance data and straight-line distance data, and then double-checked by the authors to ensure accuracy. Descriptive analysis was conducted to describe sociodemographic characteristics, ANC service use, knowledge of ANC, presence of complications during pregnancy, and perceived barriers to receiving ANC among mothers who attended ANC four times or more (ANC4+ achievers) and those who received ANC three times or less or not at all (non-achievers). Mothers were assigned to socio-economic status quartiles based on household assets and housing characteristics determined by principal component analysis [36,38].
To identify determinants of achievements in receiving ANC four times or more, two multiple logistic regression analyses were performed: one with actual travel distance and the other with straight-line distance. By doing so, we aimed to detect discrepancies or inconsistencies between the two distance measures, if any. In each analysis, the following independent variables were included: age, education, husband’s education, wealth quartiles, ethnicity, number of children, presence of health issues during pregnancy, experience of stillbirth and/or child loss, the nearest health center, and knowledge about ANC (if ANC is recommended even without any health issues, and recommended times of ANC). Out of the other sociodemographic characteristics, literacy was excluded from the regression analysis because of multicollinearity with education (r = 0.89). Marital status and occupation were excluded because of the small sub-group sample sizes (too few mothers who were not married and who were not farmers). Child age and child gender were also excluded because they are irrelevant to ANC use during the pregnancy.
A variety of perceived barriers to accessing health center among ANC4+ achievers and non-achievers are summarized with descriptive statistics. In the questionnaire, twenty-seven possible perceived barriers that mothers could have felt when accessing or trying to access ANC were asked with four choices: yes, to some extent, no, and don’t know. Possible perceived barriers asked in the questionnaire were selected based on previous studies: a financial barrier, a transportation barrier, seven geographical/environmental barriers, eight health-related barriers, six facility-related barriers, and five family-related barriers [5,15,39]. Those who answered “yes” and “to some extent” were classified as those who perceived the barrier. Open-ended questions were also asked if mothers felt any other barriers, but all answers overlapped with one of the given 27 barriers.
Data analysis was done using STATA version 14. Informed consent was obtained from all study participants before the interview. The study protocol, consent forms, and survey questionnaires were approved by the National Ethics Committee for Health Research, the Ministry of Health, Cambodia (368 NECHR), the Research Ethics Committee of Tokyo University of Agriculture and Technology (28–45), and the Research Ethics Committee of the University of Tokyo (11030).
Results
A total of 377 mothers with children under two living in 62 villages in the Ratanakiri province, Cambodia were included in the analysis for this study. Their sociodemographic characteristics are described in Table 1. Approximately half (50.9%) of the mothers were in their twenties, and about a fourth (23.7%) were in their thirties. Most mothers were married (97.6%). Two thirds (66.6%) of the mothers had no school education at all. Two thirds (68.2%) responded that they were illiterate, and only 5.3% were confident about their ability to read. Their husbands were slightly better educated than their wives, but about 45% had no school education. Most of the mothers (91.3%) were farmers. In addition to mothers who belonged to the Khmer group, which is the largest ethnic group in Cambodia, there were ten other ethnic minority groups represented in this study. Of these, three groups comprised about two-thirds of the study population (Thompoun 23.4%, Charay 20.2%, and Kreung 15.4%).
Table 1. Sociodemographic characteristics of ANC4+ achievers and non-achievers (Total n = 377 in 62 villages).
| Characteristics | Overall (n = 377) | Achievers (n = 123) | Non-achievers (n = 254) | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-value | |
| Age | |||||||
| <20 | 80 | 21.2 | 24 | 19.5 | 56 | 22.0 | 0.055 |
| 20–29 | 192 | 50.9 | 71 | 57.7 | 121 | 47.6 | |
| 30–39 | 89 | 23.7 | 27 | 22.0 | 62 | 24.4 | |
| 40+ | 16 | 4.2 | 1 | 0.8 | 15 | 5.9 | |
| Marital status (Married) | 368 | 97.6 | 122 | 99.2 | 246 | 96.9 | 0.540 |
| Education | |||||||
| None | 251 | 66.6 | 59 | 48.0 | 192 | 75.6 | <0.001 |
| Primary (1–6 years) | 98 | 26.0 | 46 | 37.4 | 52 | 20.5 | |
| ≧Secondary (≧7 years) | 28 | 7.4 | 18 | 14.6 | 10 | 3.9 | |
| Literacy | |||||||
| Cannot read at all | 257 | 68.2 | 65 | 52.8 | 192 | 75.6 | <0.001 |
| Able to read only part | 100 | 26.5 | 45 | 36.6 | 55 | 21.7 | |
| Able to read whole | 20 | 5.3 | 13 | 10.6 | 7 | 2.8 | |
| Husband’s education | |||||||
| None | 170 | 45.1 | 34 | 27.6 | 136 | 53.5 | <0.001 |
| Primary (1–6 years) | 137 | 36.3 | 56 | 45.5 | 81 | 31.9 | |
| ≧Secondary (≧7 years) | 70 | 18.6 | 33 | 26.8 | 37 | 14.6 | |
| Couple’s education | |||||||
| None | 177 | 46.9 | 38 | 30.9 | 139 | 54.7 | <0.001 |
| ≧Primary (≧1 year) | 200 | 53.1 | 85 | 69.1 | 115 | 45.3 | |
| Occupation (farmer) | 344 | 91.3 | 108 | 87.8 | 236 | 92.9 | 0.100 |
| Wealth quartiles | 0.312 | ||||||
| Low | 95 | 25.2 | 26 | 21.1 | 69 | 27.2 | |
| Lower middle | 94 | 24.9 | 28 | 22.8 | 66 | 26.0 | |
| Upper middle | 94 | 24.9 | 32 | 26.0 | 62 | 24.4 | |
| High | 94 | 24.9 | 37 | 30.1 | 57 | 22.4 | |
| Ethnicity | |||||||
| Khmer | 42 | 11.2 | 27 | 22.0 | 15 | 5.9 | <0.001 |
| Thompoun | 88 | 23.4 | 25 | 20.3 | 63 | 24.8 | |
| Charay | 76 | 20.2 | 20 | 16.3 | 56 | 22.0 | |
| Kreung | 58 | 15.4 | 19 | 15.4 | 39 | 15.4 | |
| Other | 113 | 29.8 | 32 | 26.0 | 81 | 31.9 | |
| Number of children | |||||||
| 1 | 140 | 37.2 | 45 | 36.6 | 95 | 37.4 | 0.152 |
| 2 | 112 | 29.7 | 45 | 36.6 | 67 | 26.4 | |
| 3–4 | 99 | 26.2 | 27 | 22.0 | 72 | 28.3 | |
| 5+ | 26 | 6.9 | 6 | 4.9 | 20 | 7.9 | |
| Child age (month) | |||||||
| 0–5 | 141 | 37.4 | 96 | 78.0 | 45 | 17.7 | 0.190 |
| 6–11 | 96 | 25.5 | 59 | 48.0 | 37 | 14.6 | |
| 12–17 | 73 | 19.3 | 56 | 45.5 | 17 | 6.7 | |
| 18–23 | 67 | 17.8 | 43 | 35.0 | 24 | 9.4 | |
| Sex of the child (female) | 181 | 48.0 | 64 | 52.0 | 117 | 46.1 | 0.274 |
| Experience of stillbirth (Yes) | 42 | 11.1 | 14 | 11.4 | 28 | 11.0 | 0.917 |
| Experience of child loss* (Yes) | 49 | 13.0 | 16 | 13.0 | 33 | 13.0 | 0.997 |
| Health center | |||||||
| Oyadav (17 villages) | 93 | 24.7 | 18 | 14.6 | 75 | 29.5 | 0.006 |
| Lumphat (8) | 75 | 19.9 | 31 | 25.2 | 44 | 17.3 | |
| Andaung Meas (10) | 64 | 17.0 | 27 | 22.0 | 37 | 14.6 | |
| Ochum (10) | 50 | 13.2 | 15 | 12.2 | 35 | 13.8 | |
| Taveng (8) | 38 | 10.1 | 16 | 13.0 | 22 | 8.7 | |
| Chomrom Bey Sruk (3) | 29 | 7.7 | 5 | 4.1 | 24 | 9.4 | |
| Kachanh (6) | 28 | 7.4 | 11 | 8.9 | 17 | 6.7 | |
| Actual travel distance to health center (km) | |||||||
| < 5.0 | 42 | 11.1 | 18 | 14.6 | 24 | 9.4 | 0.001 |
| 5.0–9.9 | 98 | 26.0 | 44 | 35.8 | 54 | 21.3 | |
| 10.0–14.9 | 132 | 35.0 | 41 | 33.3 | 91 | 35.8 | |
| 15.0 + | 105 | 27.9 | 20 | 16.3 | 85 | 33.5 | |
| Straight-line distance to health center (km) | |||||||
| < 5.0 | 67 | 17.8 | 33 | 26.8 | 34 | 13.4 | 0.003 |
| 5.0–9.9 | 162 | 43.0 | 53 | 43.1 | 109 | 42.9 | |
| 10.0–14.9 | 75 | 19.9 | 22 | 17.9 | 53 | 20.9 | |
| 15.0 + | 73 | 19.3 | 15 | 12.2 | 58 | 22.8 | |
* Experience of child loss: Mother had lost a child/children after delivery.
About a third (37.2%) of the mothers had one child. Child age (months) varied, but about a third (37.4%) belonged to the youngest age group, 0–5 months. About half (48.0%) of the children were female. Approximately a tenth (11.1%) of the mothers had experienced stillbirth, and 13.0% had lost children in the past.
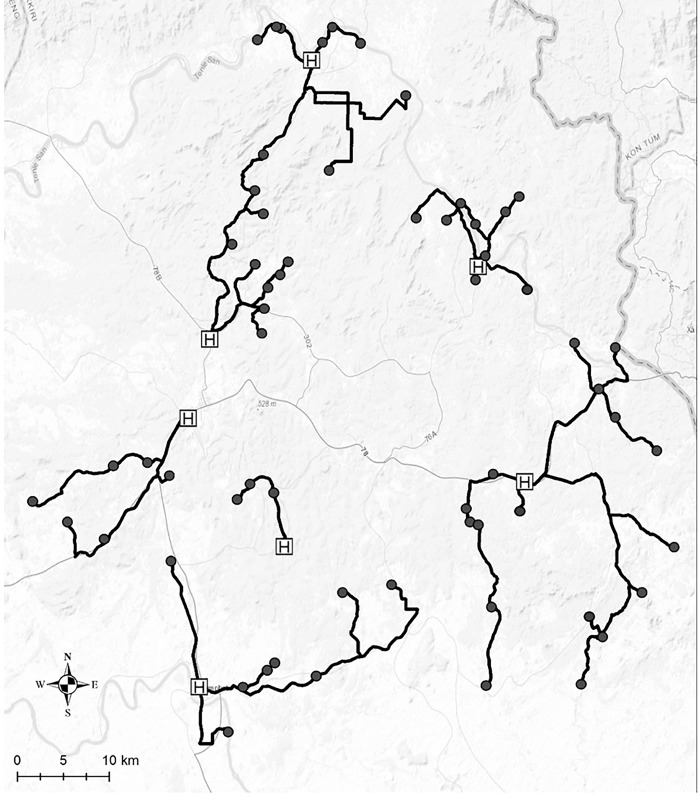
Actual travel distance between each of the 62 villages and the nearest health center was measured using the GIS and compared with straight-line distance measured on a map. A striking discrepancy was found between data gained by the two distance measures (Fig 1). Depending on the village, difference between actual travel distance and straight-line distance ranged from 3.0 m to 30.2 km. For all villages, actual travel distance measured using GPS was longer than the straight-line distance (median difference = 2.83km, mean difference = 4.48 km, SD = 5.19). The mean of the actual travel distance between 62 villages and their nearest health centers (14.71 km, SD = 9.84) was significantly longer than the mean of the straight-line distance (10.23 km, SD = 5.75) (t = 6.79, df = 61, p<0.001). As shown in Fig 2, pregnant women living in the majority of villages had to make a detour from the straight-line path because of insufficient road networks and environmental barriers such as forests and rivers.
Fig 1. Discrepancy between actual travel distance and straight-line distance from 62 villages to their nearest health centers in Ratanakiri province.
Fig 2. Map of study site in Ratanakiri province with actual travel route from 62 villages to their nearest health centers.
Black circle: village, black line: actual travel route from each village to its nearest health center, H: health center (Sources: Esri, HERE, DeLorme, Intermap, increment P Corp., GEBCO USGS, FAO, NPS, NRCAN, GeoBase, IGN, Kadaster NL, Ordnance Survey, Esri Japan, METI Esri China (Hong Kong), swisstopo, MapmyIndia, OpenStreetMap contributors, and the GIS User Community).
The distances the mothers had to travel are distributed very differently between actual and straight-line distances (chi-square test p<0.001) (Table 1). According to the actual travel distance, 11.1% of the mothers were found to have lived in villages where the distance to the nearest health center was shorter than 5.0 km. About a fourth (26.0%) lived in villages with a distance between 5.0 km and 9.9 km, 35.0% between 10.0 km and 14.9 km, and 27.9% belonged to the farthest group of 15 km or longer. However, based on the straight-line distance, nearly half (43%) of the mothers were found to have lived in villages 5.0–9.9 km away, and only 19.9% and 19.3% were found to have lived in villages of 10.0–14.9 km away and 15.0 km or farther from the nearest health center, respectively.
Similarly, the two distance measures showed totally different distributions of ANC4+ and non-achievers. Actual travel distance showed that the majority (71.3%) of the non-achievers lived in villages 10.0 km or farther from the nearest health center. On the other hand, the straight-line distance showed less than half (43.7%) lived in villages 10.0 km or farther, while nearly the other half (42.9%) lived in villages 5.0–9.9 km away from the nearest health center. These findings clearly show that straight-line distances are misleading because they convey the impression that the study population as a whole and ANC non-achievers live closer to the nearest health center than in reality.
Frequency of ANC use, knowledge of ANC, contents of health education received at ANC, and experience of health issues during pregnancy are summarized in Table 2. Only about a third (32.6%) of the mothers had received ANC four times or more as recommended by the WHO [40]. About a quarter (24.1%) of the mothers never received ANC during their most recent pregnancy. Most (92.7%) of the mothers, who had been to the nearest health center to receive ANC, took a motorcycle, which was owned by their family or someone in their village. The majority of mothers (71.9%) were aware that receiving ANC is recommended regardless of the presence of health problems. However, only about a third (31.3%) of them knew that pregnant women are recommended to receive ANC at least four times. Only 13.5% of the mothers were aware of one or more of the danger signs during pregnancy such as severe headache, vaginal bleeding, and vaginal secretion. Most mothers reported that they received ANC because they were willing to get a checkup (55.9%) or they were worried about their pregnancy (25.5%) or health (9.8%).
Table 2. ANC utilization and knowledge among ANC4+ achievers and non-achievers.
| Overall | Achievers | Non-achievers | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-value | |
| ANC visit (times) | (n = 377) | (n = 123) | (n = 254) | ||||
| 0 | 91 | 24.1 | 0 | 0 | 91 | 35.8 | |
| 1 | 41 | 10.9 | 0 | 0 | 41 | 16.1 | |
| 2 | 48 | 12.7 | 0 | 0 | 48 | 18.9 | |
| 3 | 74 | 19.6 | 0 | 0 | 74 | 29.1 | |
| 4 or more | 123 | 32.6 | 123 | 100 | 0 | 0 | |
| Transportation to ANC (n = 286) | (n = 286) | (n = 123) | (n = 163) | ||||
| Motorcycle | 265 | 92.7 | 114 | 92.7 | 151 | 92.6 | 0.340 |
| Taxi | 4 | 1.4 | 1 | 0.8 | 3 | 1.8 | |
| On foot | 3 | 1.1 | 0 | 0.0 | 3 | 1.8 | |
| Other (bicycle, boat etc.) | 14 | 4.9 | 8 | 6.5 | 6 | 3.7 | |
| Knowledge | |||||||
| ANC is recommended regardless of the presence of complications | 271 | 71.9 | 111 | 90.2 | 160 | 63.0 | <0.001 |
| Recommended times of ANC (4 or more) | 118 | 31.3 | 68 | 55.3 | 50 | 19.7 | <0.001 |
| Danger sign during pregnancy (correct) | 51 | 13.5 | 28 | 22.8 | 23 | 9.1 | <0.001 |
| Major reason why received ANC | (n = 286) | (n = 123) | (n = 163) | ||||
| Wanted to get a checkup | 160 | 55.9 | 71 | 57.7 | 89 | 54.6 | 0.419 |
| Worried about pregnancy | 73 | 25.5 | 32 | 26.0 | 41 | 25.2 | |
| Worried about health problem | 28 | 9.8 | 11 | 8.9 | 17 | 10.4 | |
| Health workers’ advice | 1 | 0.3 | 0 | 0.0 | 1 | 0.6 | |
| Family’s suggestion | 5 | 1.7 | 0 | 0.0 | 5 | 3.1 | |
| Other | 19 | 6.6 | 9 | 7.3 | 10 | 6.1 | |
| Knowledge gained at ANC (Multiple choice) | (n = 286) | (n = 123) | (n = 163) | ||||
| Recommended place of delivery | 222 | 77.6 | 104 | 84.6 | 118 | 72.4 | 0.015 |
| Recommended timing and frequency of ANC | 167 | 58.4 | 77 | 62.6 | 90 | 55.2 | 0.210 |
| Early initiation and exclusively breastfeeding | 142 | 49.7 | 65 | 52.8 | 77 | 47.2 | 0.348 |
| Danger signs during pregnancy | 138 | 48.3 | 63 | 51.2 | 75 | 46.0 | 0.383 |
| Nutrition of pregnant women | 132 | 46.2 | 61 | 49.6 | 71 | 43.6 | 0.311 |
| Items to prepare before delivery | 125 | 43.7 | 65 | 52.8 | 60 | 36.8 | 0.007 |
| Family planning | 109 | 38.1 | 61 | 49.6 | 48 | 29.4 | 0.001 |
| How to prevent malaria | 84 | 29.4 | 39 | 31.7 | 45 | 27.6 | 0.451 |
| Arrange transportation to go to HC for delivery | 62 | 21.7 | 34 | 27.6 | 28 | 17.2 | 0.033 |
| Presence of health issues during pregnancy | (n = 377) | (n = 123) | (n = 254) | ||||
| 126 | 33.4 | 43 | 35.0 | 83 | 32.7 | 0.660 | |
| Kinds of health issues during pregnancy (Multiple choice) | (n = 377) | (n = 123) | (n = 254) | ||||
| severe headache | 88 | 23.3 | 30 | 24.4 | 58 | 22.8 | 0.738 |
| Fits | 79 | 21.0 | 27 | 22.0 | 52 | 20.5 | 0.741 |
| Fever | 73 | 19.4 | 26 | 21.1 | 47 | 18.5 | 0.544 |
| severe abdominal pain | 60 | 15.9 | 18 | 14.6 | 42 | 16.5 | 0.636 |
| fast/difficult breathing | 27 | 7.2 | 10 | 8.1 | 17 | 6.7 | 0.612 |
| vaginal bleeding | 4 | 1.1 | 2 | 1.6 | 2 | 0.8 | 0.598 |
| Received care to treat health issues | (n = 126) | (n = 43) | (n = 83) | ||||
| 74 | 58.7 | 29 | 67.4 | 45 | 54.2 | 0.134 | |
Overall, higher percentages of achievers correctly answered each and every knowledge item compared to non-achievers. Significantly higher percentages of achievers learned about the recommended place of delivery (84.6% vs 72.4%, p = 0.015), items to prepare before delivery (52.8% vs 36.8%, p = 0.007), family planning (49.6% vs 29.4%, p = 0.001), and the necessity of arranging transportation to go to HC for delivery (27.6% vs 17.2%, p = 0.033).
About a third (33.4%) of the mothers reported that they had experienced one or more health issues (complications) during pregnancy. The complications included severe headache (23.3%), fits (21.0%), fever (19.4%), severe abdominal pain (15.9%), fast/difficult breathing (7.2%), and vaginal bleeding (1.1%). A higher percentage of mothers who achieved ANC4+ received care for the complications compared to non-achievers, but the difference was not statistically significant (67.4% vs 54.2%, p = 0.134).
Factors associated with achieving ANC4+ were examined by multiple logistic regression analysis (Table 3). Two models were run, one with actual distance data and the other with straight-line distance data. In both models, significant promoting factors for achieving ANC4+ were mother’s educational background and knowledge about ANC, while the only preventing factor was distance to the nearest health center where pregnant women can receive ANC. According to the model using actual travel distance, mothers with secondary or higher education were about five times more likely to have achieved ANC4+ during their most recent pregnancy (AOR = 5.50, 95%CI: 1.74, 17.37). Mothers who were aware that ANC is recommended for pregnant women even without any health issues were about three times more likely to have achieved ANC4+ (AOR = 2.74, 95%CI: 1.25, 6.00), and those who knew the recommended times for ANC were about four times more likely to have achieved ANC4+ (AOR = 2.26, 95%CI: 7.22). Mothers who had to travel 10.0–14.9km to get to the nearest health center were about 70% less likely to have achieved ANC4+ (AOR = 0.32, 95%CI: 0.10, 0.99), and those who had to travel 15.0 km or longer were about 80% less likely to have achieved ANC 4+ (AOR = 0.21, 95%CI: 0.07, 0.62) compared to those who lived in villages with actual travel distance of 5.0 km or less.
Table 3. Factors associated with achieving ANC4+ (n = 377).
| Univariate | Multiple logistic regression with actual travel distance | Multiple logistic regression with straight-line distance | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | AOR | 95%CI | AOR | 95%CI | ||||
| Age | |||||||||
| <20 | 1 | 1 | 1 | ||||||
| 20–29 | 1.37 | 0.78 | 2.40 | 1.00 | 0.46 | 2.22 | 0.98 | 0.45 | 2.15 |
| 30–39 | 0.85 | 0.45 | 1.62 | 0.73 | 0.26 | 2.00 | 0.76 | 0.28 | 2.06 |
| Education | |||||||||
| None | 1 | 1 | 1 | ||||||
| Primary (1–6 years) | 2.88 | 1.76 | 4.71** | 1.70 | 0.84 | 3.41 | 1.73 | 0.86 | 3.50 |
| ≧Secondary (≧7 years) | 5.86 | 2.56 | 13.38** | 5.50 | 1.74 | 17.37** | 5.08 | 1.63 | 15.82* |
| Husband’s education | |||||||||
| None | 1 | 1 | 1 | ||||||
| Primary (1–6 years) | 2.77 | 1.67 | 4.59 | 1.69 | 0.86 | 3.32 | 1.64 | 0.83 | 3.24 |
| ≧Secondary (≧7 years) | 3.57 | 1.96 | 6.51 | 1.58 | 0.66 | 3.75 | 1.47 | 0.61 | 3.53 |
| Wealth quartiles | |||||||||
| Low | 1 | 1 | 1 | ||||||
| Lower middle | 1.13 | 0.60 | 2.12 | 1.08 | 0.49 | 2.35 | 1.01 | 0.47 | 2.18 |
| Upper middle | 1.37 | 0.74 | 2.55 | 1.73 | 0.80 | 3.76 | 1.70 | 0.79 | 3.68 |
| High | 1.72 | 0.93 | 3.18 | 1.28 | 0.57 | 2.90 | 1.26 | 0.57 | 2.82 |
| Ethnicity | |||||||||
| Khmer | 1 | 1 | 1 | ||||||
| Thompoun | 0.22 | 0.10 | 0.48** | 0.52 | 0.16 | 1.72 | 0.60 | 0.19 | 1.94 |
| Charay | 0.20 | 0.08 | 0.45** | 0.50 | 0.13 | 1.94 | 0.47 | 0.13 | 1.80 |
| Kreung | 0.27 | 0.12 | 0.62** | 1.07 | 0.30 | 3.80 | 1.17 | 0.32 | 4.25 |
| Other | 0.22 | 0.10 | 0.47** | 0.39 | 0.13 | 1.20 | 0.38 | 0.12 | 1.16 |
| Number of children | |||||||||
| 1 | 1 | 1 | 1 | ||||||
| 2 | 1.42 | 0.85 | 2.38 | 2.05 | 0.97 | 4.35 | 2.02 | 0.96 | 4.27 |
| 3–4 | 0.79 | 0.45 | 1.40 | 0.96 | 0.38 | 2.42 | 0.91 | 0.37 | 2.28 |
| 5+ | 0.63 | 0.24 | 1.69 | 1.20 | 0.31 | 4.74 | 1.13 | 0.29 | 4.44 |
| Presence of danger sign during pregnancy | |||||||||
| Not present | 1 | 1 | 1 | ||||||
| Present | 1.11 | 0.70 | 1.74 | 1.17 | 0.66 | 2.10 | 1.22 | 0.68 | 2.18 |
| Experience of stillbirth and/or child loss | |||||||||
| No | 1 | 1 | 1 | ||||||
| Yes | 0.87 | 0.48 | 1.58 | 1.14 | 0.52 | 2.53 | 1.06 | 0.48 | 2.33 |
| Health center | |||||||||
| Oyadav | 1 | 1 | 1 | ||||||
| Lumphat | 2.94 | 1.47 | 5.85** | 2.21 | 0.59 | 8.23 | 1.84 | 0.53 | 6.32 |
| Andaung Meas | 3.04 | 1.49 | 6.21** | 1.94 | 0.74 | 5.11 | 2.13 | 0.82 | 5.57 |
| Ochum | 1.79 | 0.81 | 3.95 | 0.73 | 0.17 | 3.10 | 0.72 | 0.18 | 2.89 |
| Taveng | 3.03 | 1.33 | 6.91** | 2.27 | 0.68 | 7.54 | 2.48 | 0.77 | 8.00 |
| Chomrom Bey Sruk | 0.87 | 0.29 | 2.59 | 0.54 | 0.11 | 2.78 | 0.48 | 0.98 | 2.38 |
| Kachanh | 2.67 | 1.08 | 6.74* | 1.16 | 0.28 | 4.77 | 1.13 | 0.27 | 4.80 |
| Actual travel distance to health center (km) | |||||||||
| < 5.0 | 1 | 1 | |||||||
| 5.0–9.9 | 1.09 | 0.52 | 2.25 | 0.66 | 0.22 | 1.97 | |||
| 10.0–14.9 | 0.60 | 0.29 | 1.23 | 0.32 | 0.10 | 0.99* | |||
| 15.0 + | 0.31 | 0.14 | 0.69** | 0.21 | 0.07 | 0.62** | |||
| Straight-line distance to health center (km) | |||||||||
| < 5.0 | 1 | 1 | |||||||
| 5.0–9.9 | 0.50 | 0.28 | 0.90* | 0.46 | 0.19 | 1.08 | |||
| 10.0–14.9 | 0.43 | 0.21 | 0.85* | 0.28 | 0.10 | 0.79* | |||
| 15.0 + | 0.27 | 0.13 | 0.56** | 0.23 | 0.08 | 0.64** | |||
| Knowledge: ANC is recommended | |||||||||
| No | 1 | 1 | 1 | ||||||
| Yes | 5.43 | 2.84 | 10.34** | 2.74 | 1.25 | 6.00* | 2.82 | 1.28 | 6.23* |
| Knowledge: Recommended times of ANC | |||||||||
| Wrong | 1 | 1 | 1 | ||||||
| Correct (four or more) | 5.04 | 3.15 | 8.08** | 4.04 | 2.26 | 7.22** | 4.07 | 2.28 | 7.29** |
*p<0.05
**p<0.01
Details of perceived barriers that mothers felt in accessing the nearest health center to receive ANC during their most recent pregnancy were compared between ANC 4+ achievers and non-achievers (Table 4). A significantly higher percentage of non-achievers perceived financial barriers compared to achievers (77.6% vs 56.9%, p<0.001). In addition, distance and undulation of the road to the nearest health center were geographical/environmental barriers that were perceived by a significantly higher percentage of non-achievers compared to achievers (85.4% vs 77.2%, p = 0.048; 70.1% vs 58.5%, p = 0.026). Abdominal pain, being unaware of where to receive ANC, and having no one to accompany one were also important barriers that were perceived by a significantly higher percentage of non-achievers compared to achievers (46.5% vs 35.8%, p = 0.049; 13.0% vs 4.9%, p = 0.015; 25.2% vs 9.8%, p<0.001). All raw research data and codes for variables are shown in S1, S2 and S3 Files.
Table 4. Perceived barriers to access health center among ANC4+ achievers and non-achievers.
| Perceived barrier | Overall (n = 377) | Achievers (n = 123) | Non-achievers (n = 254) | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-value | |
| Financial barrier | |||||||
| No money | 300 | 79.6 | 91 | 74.0 | 209 | 82.3 | 0.061 |
| Transportation barrier | |||||||
| No transportation | 267 | 70.8 | 70 | 56.9 | 197 | 77.6 | <0.001 |
| Geographical/Environmental barrier | |||||||
| Too far | 312 | 82.8 | 95 | 77.2 | 217 | 85.4 | 0.048 |
| Bumpy road | 267 | 70.8 | 81 | 65.9 | 186 | 73.2 | 0.140 |
| Dust | 266 | 70.6 | 85 | 69.1 | 181 | 71.3 | 0.667 |
| Undulation of the road | 250 | 66.3 | 72 | 58.5 | 178 | 70.1 | 0.026 |
| Rain | 216 | 57.3 | 66 | 53.7 | 150 | 59.1 | 0.321 |
| Forest/bush | 89 | 23.6 | 25 | 20.4 | 64 | 25.2 | 0.296 |
| Flood | 63 | 16.7 | 22 | 17.5 | 41 | 16.1 | 0.670 |
| Health-related barrier | |||||||
| Fetal movement | 248 | 65.8 | 76 | 61.8 | 172 | 67.7 | 0.255 |
| Felt tired | 245 | 65.0 | 75 | 61.0 | 170 | 66.9 | 0.256 |
| Headache | 218 | 57.8 | 64 | 52.0 | 154 | 60.6 | 0.279 |
| Vomiting | 203 | 53.8 | 66 | 53.7 | 137 | 53.9 | 0.959 |
| Abdominal pain | 162 | 43.0 | 44 | 35.8 | 118 | 46.5 | 0.049 |
| Blurry vision | 122 | 32.4 | 37 | 30.1 | 85 | 33.5 | 0.510 |
| Edema | 94 | 24.9 | 24 | 19.5 | 70 | 27.6 | 0.090 |
| Vaginal bleeding | 13 | 3.4 | 4 | 3.3 | 9 | 3.5 | 0.574 |
| Facility-related barrier | |||||||
| Long waiting time | 175 | 46.4 | 64 | 52.0 | 111 | 43.7 | 0.128 |
| Inconvenient service hour | 131 | 34.7 | 48 | 39.0 | 83 | 32.7 | 0.225 |
| Not wanting to be scolded | 91 | 24.1 | 27 | 22.0 | 64 | 25.2 | 0.490 |
| Afraid to go | 90 | 23.9 | 19 | 15.4 | 71 | 28.0 | 0.008 |
| Good service not available | 46 | 12.2 | 10 | 8.1 | 36 | 14.2 | 0.093 |
| Didn’t know where to go | 39 | 10.3 | 6 | 4.9 | 33 | 13.0 | 0.015 |
| No female doctor | 29 | 7.7 | 5 | 4.1 | 24 | 9.4 | 0.066 |
| Family-related barrier | |||||||
| Difficult to leave elder children (achiever = 78, non-achiever = 159) | 77 | 32.5 | 23 | 29.5 | 54 | 34.0 | 0.489 |
| No one can accompany | 76 | 20.2 | 12 | 9.8 | 64 | 25.2 | <0.001 |
| No support from husband | 57 | 15.1 | 14 | 11.4 | 43 | 16.9 | 0.159 |
| No support from mother-in-law | 39 | 10.3 | 13 | 10.6 | 26 | 10.2 | 0.921 |
Discussion
This study revealed the limited use of ANC and barriers for pregnant women living in rural, agricultural villages to accessing ANC in the Ratanakiri province, Cambodia. Only a third of the mothers had received ANC four times or more and a quarter of the mothers had never received ANC during their most recent pregnancy. Factors associated with achieving ANC4+ were mother’s educational background, knowledge about ANC, and actual travel distance to the nearest health facility. As for perceived barriers, compared to ANC4+ achievers, a significantly higher percentage of non-achievers perceived to have financial barriers, geographical/environmental barriers (actual travel distance and undulation of the road), as well as health-related (abdominal pain), facility-related (don’t know where to go), and family-related (no one could accompany the mother) barriers. Furthermore, the mothers’ lack of knowledge was quite evident. Although about a third of the mothers had experienced complications during their pregnancy, only one out of seven were aware of the danger signs during pregnancy.
ANC use was limited with only a third (32.6%) of the mothers having received ANC four times or more during their most recent pregnancy. This is much lower than the figure (48.4%) obtained by the DHS in Cambodia conducted in 2014 [33], as well as those reported by recent studies conducted in other developing countries, such as 86% on average from three locations in Ghana [41] and 46% in Rwanda [16]. Together with the fact that a fourth of the pregnant women had never received ANC, this study highlighted the urgent need to increase ANC among this population.
Despite the large discrepancy in reported ANC use, many of our results were consistent with other similar studies, assuring the validity of our findings. For example, mothers’ higher educational background and better knowledge about ANC were promoting factors for receiving ANC four times or more. Several previous studies have demonstrated that women’s education was positively associated with their health service use [8,18,39]. In addition, our study revealed that knowledge of recommended frequency of ANC is crucial for achieving ANC4+. Even though the majority of the mothers knew that receiving ANC is recommended, only a third of them were aware of the recommended frequency. Those who had this knowledge were four-times more likely to have achieved ANC4+. To effectively increase ANC use, this information needs to reach pregnant women ideally at the first ANC.
Also, similar to previous studies, we found that travel distance is negatively associated with achieving ANC4+. Previous studies have pointed out that distance could be a significant barrier for health service use. A qualitative study conducted in another rural province, Kampong Cham, in Cambodia demonstrated that distance to the health facility, poor road conditions, and inadequate transportation were common obstacles raised by reproductive age women to use health services [15]. Karra et al. reported that even relatively small distances from health facilities were associated with child mortality, and that reducing travel distances and travel times is likely to increase the use of health services and reduce neonatal mortality [42]. The negative effect of distance on health service use needs to be considered to develop an effective strategy to increase ANC and other maternal and child health service use.
Although travel distance has been established by others and confirmed in this study as a barrier to health service use, this study additionally elucidates the importance of measuring actual travel distance accurately in remote areas with limited road networks. Many previous studies that included distance as a factor for health service utilization, only used straight-line distance as a proxy for actual travel distance [29]. However, straight-line distance gotten simply by connecting two points on a map is often inaccurate as it ignores geographical/environmental barriers that might affect actual travel distance [30]. This is especially true in many of the developing countries where the pregnant women must make numerous detours to avoid any number of geographical/environmental barriers, such as forests, rivers, undulation of roads, etc. The importance of distinguishing between actual and straight-line distance was confirmed by our findings, as we found a statistically significant difference in distribution between straight-line distance and actual travel distance among ANC4+ achievers and non-achievers. Obviously, such a finding does not alter the known association between travel distance and ANC use, as evident by the results of the two multiple logistic regression models (with straight-line distance or actual distance) consistently showing that living in villages 10.0 km or farther from the nearest health center being negatively associated with achieving ANC4+. However, using actual travel distance, we found that a great majority of the ANC4+ non-achievers lived in villages that require trips of 10.0 km or longer to get to the nearest health center. Specifically, actual travel distance showed that more than two thirds of the ANC4+ non-achievers lived in villages 10.0 km or farther away, while straight-line distance showed that less than half of the non-achievers lived 10.0 km or farther away. Therefore, relying on straight-line distance creates the risk of misunderstanding the target population most in need of future intervention programs to assist in accessing ANC. Further, using actual distance may better account for the amount of effort and time it takes for a person to reach the nearest health facility, with the rationale that the longer actual distance is indicative of the fact that detours are being taken to avoid the many barriers that the person may encounter. Measuring actual travel distance using GPS logger is not time consuming (only one-way travel from a village to its nearest health center) and does not require access to governmental records or expensive equipment/facility. Data collection and analysis only require a handheld GPS and common software packages to accomplish accurate location of each travel path [43]. For future research that aims to analyze access to health services, especially in remote areas with limited road networks and geographical/environmental barriers, a GIS is recommended as a simple and cost-effective tool to measure distance accurately.
In addition to distance, other barriers to access ANC need to be considered when developing strategies or local health policies to raise health service use. Compared to ANC4+ achievers, a significantly higher percentage of non-achievers claimed undulation of the road, financial constraints, abdominal pain, being unaware of where to receive ANC, and having no one to accompany them as barriers when trying to access ANC. While most of these barriers have been described in several previous studies [5,15,17], undulation of the road has never been focused on as a barrier for pregnant women to access ANC. In addition to long-distance travel by motorcycle, undulation of the road can put pregnant women at risk of road accident, which can result in adverse fetal outcomes [44,45]. Future intervention programs and strategies to raise ANC use by pregnant women need to incorporate safety measures for travel. In addition, to tackle the above-mentioned barriers as a whole, it is highly recommended that community-based maternal health services and outreach programs tailored to the local context be conducted, especially in remote and resource-limited settings.
Findings from this study should be considered in the context of some limitations. First, mothers with children under two were asked about events during their most recent pregnancy, which might have introduced recall bias. Second, because interview data collected in this study were self-reported by mothers, there was a possibility of courtesy bias. To minimize these biases, data were confirmed with a maternal health record book whenever available, and interviews were conducted by experienced and trained interviewers with on-site supervision.
Despite these limitations, this is a pioneering study to examine barriers to accessing ANC, combining a community-based cross-sectional survey and a GIS. This study revealed factors associated with ANC use by pregnant women living in remote, agricultural villages in Cambodia. Furthermore, this study highlights the importance of measuring actual travel distance accurately to examine barriers to access health facilities and to properly select target populations for future interventions. The findings and methodology of this study will contribute to the development and implementation of an effective community-based intervention program to increase ANC use in Cambodia as well as in other developing countries, especially in remote areas with limited road networks.
Supporting information
(XLSX)
(XLSX)
(XLSX)
Acknowledgments
We heartily thank all the mothers who participated in this study as well as all the experts of National Center for Parasitology, Entomology and Malaria Control, National Maternal and Child Health Center, Ratanakiri Provincial Health Department, health centers, and Village Malaria Workers who made this study possible. This work was supported by JSPS KAKENHI Grant Number JP15H05284.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by JSPS KAKENHI Grant Number JP15H05284. (Japan Society for the Promotion of Science: http://www.jsps.go.jp/english/index.html) The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bustreo F, Say L, Koblinsky M, Pullum TW, Temmerman M, Pablos-Méndez A. Ending preventable maternal deaths: the time is now. Lancet Glob Health. 2013. October;1(4):e176–7. doi: 10.1016/S2214-109X(13)70059-7 Epub 2013 Aug 19. [DOI] [PubMed] [Google Scholar]
- 2.WHO. Trends in Maternal Mortality: 1990 to 2015: Estimates by WHO, UNICEF, UNFPA, World Bank, and the United Nations Population Division. Geneva: WHO. 2015
- 3.Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016. January 30;387(10017):462–74. doi: 10.1016/S0140-6736(15)00838-7 Epub 2015 Nov 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campbell OM, Graham WJ; Lancet Maternal Survival Series steering group. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006. October 7;368(9543):1284–99. Review. doi: 10.1016/S0140-6736(06)69381-1 [DOI] [PubMed] [Google Scholar]
- 5.Finlayson K, Downe S. Why do women not use antenatal services in low- and middle-income countries? A meta-synthesis of qualitative studies. PLoS Med. 2013;10(1):e1001373 doi: 10.1371/journal.pmed.1001373 Epub 2013 Jan 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007. October 13;370(9595):1358–69. Review. doi: 10.1016/S0140-6736(07)61578-5 [DOI] [PubMed] [Google Scholar]
- 7.Kikuchi K, Ansah EK, Okawa S, Enuameh Y, Yasuoka J, Nanishi K, et al. Effective Linkages of Continuum of Care for Improving Neonatal, Perinatal, and Maternal Mortality: A Systematic Review and Meta-Analysis. PLoS One. 2015. September 30;10(9):e0139288 doi: 10.1371/journal.pone.0139288 eCollection 2015. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore N, Blouin B, Razuri H, Casapia M, Gyorkos TW. Determinants of first trimester attendance at antenatal care clinics in the Amazon region of Peru: A case-control study. PLoS One. 2017. February 16;12(2):e0171136 doi: 10.1371/journal.pone.0171136 eCollection 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ronsmans C, Graham WJ; Lancet Maternal Survival Series steering group. Maternal mortality: who, when, where, and why. Lancet. 2006. September 30;368(9542):1189–200. Review. doi: 10.1016/S0140-6736(06)69380-X [DOI] [PubMed] [Google Scholar]
- 10.Carroli G, Rooney C, Villar J. How effective is antenatal care in preventing maternal mortality and serious morbidity? An overview of the evidence. Paediatr Perinat Epidemiol. 2001. January;15 Suppl 1:1–42. Review. [DOI] [PubMed] [Google Scholar]
- 11.Wang W, Hong R. Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth. 2015. March 19;15:62 doi: 10.1186/s12884-015-0497-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adjiwanou V, Legrand T. Does antenatal care matter in the use of skilled birth attendance in rural Africa: a multi-country analysis. Soc Sci Med. 2013. June;86:26–34. doi: 10.1016/j.socscimed.2013.02.047 Epub 2013 Mar 14. [DOI] [PubMed] [Google Scholar]
- 13.WHO Global Health Observatory (GHO), Antenatal care situation and trends, Geneva: WHO. 2011
- 14.Simkhada B, Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008. February;61(3):244–60. doi: 10.1111/j.1365-2648.2007.04532.x Review. [DOI] [PubMed] [Google Scholar]
- 15.Matsuoka S, Aiga H, Rasmey LC, Rathavy T, Okitsu A. Perceived barriers to utilization of maternal health services in rural Cambodia. Health Policy. 2010. May;95(2–3):255–63. doi: 10.1016/j.healthpol.2009.12.011 Epub 2010 Jan 13. [DOI] [PubMed] [Google Scholar]
- 16.Rurangirwa AA, Mogren I, Nyirazinyoye L, Ntaganira J, Krantz G. Determinants of poor utilization of antenatal care services among recently delivered women in Rwanda; a population based study. BMC Pregnancy Childbirth. 2017. May 15;17(1):142 doi: 10.1186/s12884-017-1328-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mason L, Dellicour S, Ter Kuile F, Ouma P, Phillips-Howard P, Were F, et al. Barriers and facilitators to antenatal and delivery care in western Kenya: a qualitative study. BMC Pregnancy Childbirth. 2015. February 13;15:26 doi: 10.1186/s12884-015-0453-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kisuule I, Kaye DK, Najjuka F, Ssematimba SK, Arinda A, Nakitende G, et al. Timing and reasons for coming late for the first antenatal care visit by pregnant women at Mulago hospital, Kampala Uganda. BMC Pregnancy Childbirth. 2013. May 25;13:121 doi: 10.1186/1471-2393-13-121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andrew EV, Pell C, Angwin A, Auwun A, Daniels J, Mueller I, et al. Factors affecting attendance at and timing of formal antenatal care: results from a qualitative study in Madang, Papua New Guinea. PLoS One. 2014. May 19;9(5):e93025 doi: 10.1371/journal.pone.0093025 eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myer L, Harrison A. Why do women seek antenatal care late? Perspectives from rural South Africa. J Midwifery Womens Health. 2003. Jul-Aug;48(4):268–72. [DOI] [PubMed] [Google Scholar]
- 21.Mrisho M, Obrist B, Schellenberg JA, Haws RA, Mushi AK, Mshinda H, et al. The use of antenatal and postnatal care: perspectives and experiences of women and health care providers in rural southern Tanzania. BMC Pregnancy Childbirth. 2009. March 4;9:10 doi: 10.1186/1471-2393-9-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atuyambe L, Mirembe F, Annika J, Kirumira EK, Faxelid E. Seeking safety and empathy: adolescent health seeking behavior during pregnancy and early motherhood in central Uganda. J Adolesc. 2009. August;32(4):781–96. doi: 10.1016/j.adolescence.2008.10.012 Epub 2008 Dec 2. [DOI] [PubMed] [Google Scholar]
- 23.Tinoco-Ojanguren R, Glantz NM, Martinez-Hernandez I, Ovando-Meza I. Risk screening, emergency care, and lay concepts of complications during pregnancy in Chiapas, Mexico. Soc Sci Med. 2008. March;66(5):1057–69. doi: 10.1016/j.socscimed.2007.11.006 Epub 2008 Jan 9. [DOI] [PubMed] [Google Scholar]
- 24.Mubyazi GM, Bloch P, Magnussen P, Olsen ØE, Byskov J, Hansen KS, Bygbjerg IC. Women’s experiences and views about costs of seeking malaria chemoprevention and other antenatal services: a qualitative study from two districts in rural Tanzania. Malar J. 2010. February 17;9:54 doi: 10.1186/1475-2875-9-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kabakian-Khasholian T, Campbell O, Shediac-Rizkallah M, Ghorayeb F. Women’s experiences of maternity care: satisfaction or passivity? Soc Sci Med. 2000. July;51(1):103–13. [DOI] [PubMed] [Google Scholar]
- 26.Choudhury N, Ahmed SM. Maternal care practices among the ultra poor households in rural Bangladesh: a qualitative exploratory study. BMC Pregnancy Childbirth. 2011. March 1;11:15 doi: 10.1186/1471-2393-11-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abrahams N, Jewkes R, Mvo Z. Health care-seeking practices of pregnant women and the role of the midwife in Cape Town, South Africa. J Midwifery Womens Health. 2001. Jul-Aug;46(4):240–7. [DOI] [PubMed] [Google Scholar]
- 28.Titaley CR, Dibley MJ, Roberts CL. Factors associated with underutilization of antenatal care services in Indonesia: results of Indonesia Demographic and Health Survey 2002/2003 and 2007. BMC Public Health. 2010. August 16;10:485 doi: 10.1186/1471-2458-10-485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cudnik MT, Yao J, Zive D, Newgard C, Murray AT. Surrogate markers of transport distance for out-of-hospital cardiac arrest patients. Prehosp Emerg Care. 2012. Apr-Jun;16(2):266–72. doi: 10.3109/10903127.2011.615009 Epub 2011 Sep 27. [DOI] [PubMed] [Google Scholar]
- 30.Martin D, Jordan H, Roderick P. Taking the bus: incorporating public transport timetable data into healthcare accessibility modelling. Environment and Planning A. 2008; 40:2510–2525. doi: 10.1068/a4024 [Google Scholar]
- 31.Yao J, Murray AT, Agadjanian V. A geographical perspective on access to sexual and reproductive health care for women in rural Africa. Soc Sci Med. 2013. November;96:60–8. doi: 10.1016/j.socscimed.2013.07.025 Epub 2013 Aug 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ADB. Key indicators for Asia and the Pacific 2016. Manila: Asia Development Bank. 2016. https://www.adb.org/publications/key-indicators-asia-and-pacific-2016
- 33.National Institute of Statistics, Cambodia, Directorate General for Health, Cambodia, and ICF International. 2015. Cambodia Demographic and Health Survey 2014. Phnom Penh, Cambodia: National Institute of Statistics, Cambodia, Directorate General for Health, Cambodia, and ICF International. http://dhsprogram.com/pubs/pdf/FR312/FR312.pdf.
- 34.Yasuoka J, Poudel KC, Poudel-Tandukar K, Nguon C, Ly P, Socheat D, Jimba M. Assessing the quality of service of village malaria workers to strengthen community-based malaria control in Cambodia. Malar J. 2010. April 23;9:109 doi: 10.1186/1475-2875-9-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yasuoka J, Poudel KC, Ly P, Nguon C, Socheat D, Jimba M. Scale-up of community-based malaria control can be achieved without degrading community health workers’ service quality: the Village Malaria Worker project in Cambodia. Malar J. 2012. January 4;11:4 doi: 10.1186/1475-2875-11-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hasegawa A, Yasuoka J, Ly P, Nguon C, Jimba M. Integrating child health services into malaria control services of village malaria workers in remote Cambodia: service utilization and knowledge of malaria management of caregivers. Malar J. 2013. August 23;12:292 doi: 10.1186/1475-2875-12-292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okawa S, Ansah EK, Nanishi K, Enuameh Y, Shibanuma A, Kikuchi K, et al. High Incidence of Neonatal Danger Signs and Its Implications for Postnatal Care in Ghana: A Cross-Sectional Study. PLoS One. 2015. June 19;10(6):e0130712 doi: 10.1371/journal.pone.0130712 eCollection 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vyas S, Kumaranayake L: Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006. November;21(6):459–68. Epub 2006 Oct 9. doi: 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- 39.Khanam R, Creanga AA, Koffi AK, Mitra DK, Mahmud A, Begum N, et al. Patterns and Determinants of Care-Seeking for Antepartum and Intrapartum Complications in Rural Bangladesh: Results from a Cohort Study. PLoS One. 2016. December 20;11(12):e0167814 doi: 10.1371/journal.pone.0167814 eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.WHO: WHO mmendations on antenatal care for a positive pregnancy experience. Geneva: WHO; 2016 [PubMed] [Google Scholar]
- 41.Yeji F, Shibanuma A, Oduro A, Debpuur C, Kikuchi K, Owusu-Agei S, et al. Continuum of Care in a Maternal, Newborn and Child Health Program in Ghana: Low Completion Rate and Multiple Obstacle Factors. PLoS One. 2015. December 9;10(12):e0142849 doi: 10.1371/journal.pone.0142849 eCollection 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Karra M, Fink G, Canning D. Facility distance and child mortality: a multi-country study of health facility access, service utilization, and child health outcomes. Int J Epidemiol. 2016. May 16 [Epub ahead of print] doi: 10.1093/ije/dyw062 [DOI] [PubMed] [Google Scholar]
- 43.Wampler PJ, Rediske RR, Molla AR. Using ArcMap, Google Earth, and Global Positioning Systems to select and locate random households in rural Haiti. Int J Health Geogr. 2013. January 18;12:3 doi: 10.1186/1476-072X-12-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Auriault F, Thollon L, Pérès J, Behr M. Adverse fetal outcome in road accidents: Injury mechanism study and injury criteria development in a pregnant woman finite element model. Accid Anal Prev. 2016. December;97:96–102. doi: 10.1016/j.aap.2016.08.026 Epub 2016 Sep 2. [DOI] [PubMed] [Google Scholar]
- 45.Redelmeier DA, Naqib F, Thiruchelvam D, R Barrett JF. Redelmeier DA, Naqib F, Thiruchelvam D, R Barrett JF. Motor vehicle crashes during pregnancy and cerebral palsy during infancy: a longitudinal cohort analysis. BMJ Open. 2016. September 20;6(9):e011972 doi: 10.1136/bmjopen-2016-011972 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.