Abstract
Objective
We sought to characterize the circumstances, orientations, and impact locations of falls in community-dwelling, ambulatory, older women.
Methods
For this longitudinal, observational study, 125 community-dwelling women age ≥ 65 years were recruited. Over 12-months of follow-up, fall details were recorded using twice-monthly questionnaires.
Results
More than half (59%) of participants fell, with 30% of participants falling more than once (fall rate=1.3 falls per person-year). Slips (22%) and trips (33%) accounted for the majority of falls. Approximately 44% of falls were forward in direction, while backward falls accounted for 41 % of falls. About a third of all falls were reported to have lateral (sideways) motion. Subjects reported taking a protective step in response to 82% of forward falls and 37% of backward falls. Of falls reporting lateral motion, a protective step was attempted in 70% of accounts. Common impact locations included the hip/pelvis (47% of falls) and the hand/wrist (27%). Backwards falls were most commonly reported with slips and when changing direction, and increased the risk of hip/pelvis impact (OR=12.6; 95% CI: 4.7-33.8). Forward falls were most commonly reported with trips and while hurrying, and increased the risk of impact to the hand/wrist (OR=2.6; 95% CI: 1.2-5.9).
Conclusion
Falls in older ambulatory women occur more frequently than previously reported, with the fall circumstance and direction dictating impact to common fracture locations. Stepping was a common protective recovery strategy and that may serve as an appropriate focus of interventions to reduce falls in this high risk population.
Keywords: Trips, Slips, Injury, Fracture, Balance, SAFER
Graphical abstract

1. Introduction
Unintentional falls account for nearly 1.7 million nonfatal injuries in older women each year, resulting in an injury rate (6,631 per 100,000) that is 56% higher than that of men (Centers for Disease Control and Prevention, 2015). An understanding of fall circumstances, orientations, and impact locations may assist with identifying interventions that reduce injury in this high-risk population.
Both extrinsic and intrinsic causal factors account for notable proportions of falls in older women (Aoyagi et al., 1998; Luukinen, Koski, Hiltunen, & Kivelä, 1994). The concurrent activity (Berg, Alessio, Mills, & Tong, 1997; Bleijlevens et al., 2010; Duckham et al., 2013; Niino, Tsuzuku, Ando, & Shimokata, 2000; Painter, Elliott, & Hudson, 2009; Yasumura, Haga, & Niino, 1996), time of day (Aoyagi et al., 1998; Berg et al., 1997; Campbell et al., 1990; Luukinen, Koski, Honkanen, & Kivela, 1995; Niino et al., 2000) time of year (Aoyagi et al., 1998; Berg et al., 1997), and fall location (Aoyagi et al., 1998; Berg et al., 1997; Li et al., 2006) have been reported in separate studies. However, these circumstances have not been recorded comprehensively within a single study.
It is well understood how the fall direction (e.g. backward falls or falls to the side) and impact locations (e.g. the hip or hand) alter the risk of hip or wrist fracture (Greenspan, Myers, Maitland, Resnick, & Hayes, 1994; Palvanen et al., 2000; Parkkari et al., 1999; Schwartz, Kelsey, Sidney, & Grisso, 1998). What is not known, however, is the frequency of and circumstances that lead to high-risk fall mechanics in community-dwelling older women. Previous video-surveillance studies in long-term care facilities can guide our initial expectations. In one study, nearly 40% of observed falls involved a hip impact, with forward or sideways falls having 4-8 times greater odds of hip impact compared to backward falls or falls straight downward (Yang, Mackey, Liu-Ambrose, Feldman, & Robinovitch, 2016). In the same study, dependent activities of daily living performance and cognitive impairment were each associated with 60% greater odds of hip impact. In another study, 37% of falls had an impact to the head, with forward falls associated with a nearly three-fold increase in the odds of head impact compared to backwards falls (Schonnop et al., 2013). Approximately 64-74% of falls in these two studies had an impact to the hand, which subsequently had no influence on the odds of head impact (Schonnop et al., 2013; Yang et al., 2016). However, we anticipate that the fall direction and impact frequency may be different in a community-dwelling cohort with greater physical and cognitive function.
The purpose of this longitudinal, observational study was to characterize the circumstances, orientations, and impact locations of falls in community-dwelling, ambulatory, older women. Our findings will add insight to our understanding of fall risk in this population, which may, in turn, justify new intervention targets to reduce falls and fall-related injury.
2. Materials and Methods
2.1 Study Participants
As part of our Study Assessing Fall Epidemiology and Risk (SAFER), we recruited 125 community-dwelling, ambulatory women age ≥ 65 years, representing approximately 25 women per 5-year age strata (65-69 years: n=27, 70-74 years: n=26, 75-79 years: n=26, 80-84 years: n=25, 85+ years: n=21). On average, participants were overweight, but active, having few chronic comorbidites and high balance confidence (Table 1). All participants reported the ability to walk a city block without a gait aid (e.g. cane, walker). Women who had a lower extremity joint replacement within a year prior to participation were excluded. The inclusion criteria related to mobility and joint replacement were in place so that participants could feasibly and safely participate in other aspects of the SAFER study, including assessments of gait, balance, and strength. Participants were also to take part in a study involving bone density measurements, thus women on the osteoporosis drug teriparatide or denosumab were excluded. Participants had no previous diagnosis of dementia, were cognitively intact, and able to provide informed consent. This study was approved by the Mayo Clinic Institutional Review Board. All participants provided written informed consent.
Table 1. Baseline characteristics of the 125 ambulatory, community-dwelling women age ≥65 years.
| Baseline Characteristics | Mean ± SD, Median (IQR), or N (%) |
|---|---|
|
| |
| Age (years) | 77.1 ± 7.5 |
|
| |
| BMI (kg/m2) | 27.2 ± 5.0 |
|
| |
| Charlson Comorbidity Index* (0-33) | 1.0 (0, 2.0) |
|
| |
| Physical Activity Estimates (kcal/week)** | 27333 ± 6442 |
|
| |
| ABC Score (%)*** | 87.1 ± 12.6 |
|
| |
| Yes (%) | |
|
| |
| Any falls last 12 months | 47 (32%0 |
|
| |
| Use a cane or walker | 4 (3%) |
|
| |
| Alcohol intake: | |
| None | 38 (30.4%) |
| 1-6 drinks/week | 73 (58.4%) |
| ≥ 7 drinks/week | 14 (11.2%) |
|
| |
| Smoking status | |
| Current | 1 (0.8%) |
| Former | 40 (32.0%) |
| Never | 84 (67.2%) |
|
| |
| Thyroid supplements | 34 (27.2%) |
|
| |
| Diuretics | 45 (36,0%) |
|
| |
| Anti-seizure medications | 2 (1.6%) |
|
| |
| Corticosteroids | 3 (2.4%) |
|
| |
| Anti-depressants | 25 (20.2%) |
|
| |
| Narcotics | 3 (2.4%) |
Index of diseases within five years of baseline, weighted for disease severity (Charlson, Pompei, Ales, & MacKenzie, 1987; Deyo, Cherkin, & Ciol, 1992; Quan et al., 2005)
Caloric expenditure estimates, for physical activity status, were based on body weight, duration of activity and published MET values (Ainsworth et al., 1993).
Activities-Specific Balance Confidence scale (Powell & Myers, 1995)
2.2 Assessment of Incident Falls
Over one year of follow-up, twice-monthly questionnaires were completed by participants to detail falls occurring in a half-month period (Appendix A). The definition of a fall and list of fall circumstances were advanced from previous studies and recommendations (Bleijlevens et al., 2010; Lamb et al., 2005). Figures used in questionnaires to represent fall direction and orientations were modified from a previous study (Palvanen et al., 2000). A description of the fall direction, step response, and arm placement for each figure was provided to all participants as a separate document (Appendix B). Upon enrollment in the study, a research team member reviewed the questionnaire with the participant to ensure that she understood each question and image. Questionnaires were returned to the study team by mail, regardless of whether a fall had occurred. Blank mailers and postage-paid envelopes were distributed to participants on a quarterly basis. Should a fall-questionnaire not be received for two consecutive periods (i.e. one month), a reminder letter was sent to the participant. If still no response, study staff called the participant and fall information was recorded over the phone, when necessary.
2.3 Statistical Analyses
The median time to fall was estimated using the Kaplan-Meier method. Fall circumstances, orientations, and impact locations were summarized using percentages, calculated from non-missing values where indicated. Generalized estimating equations, which accounted for multiple falls in the same participants, were used to calculate odds ratios (OR) and 95% confidence intervals (95% CI) to determine if the fall direction (Figure 2) or mechanism (e.g. slip or trip) affected the risk of fall impact to different anatomical regions. All models were unadjusted. Statistics were calculated using SAS version 9.4 (SAS Institute, NC, USA).
Figure 2. Fall Orientations and Impacts.
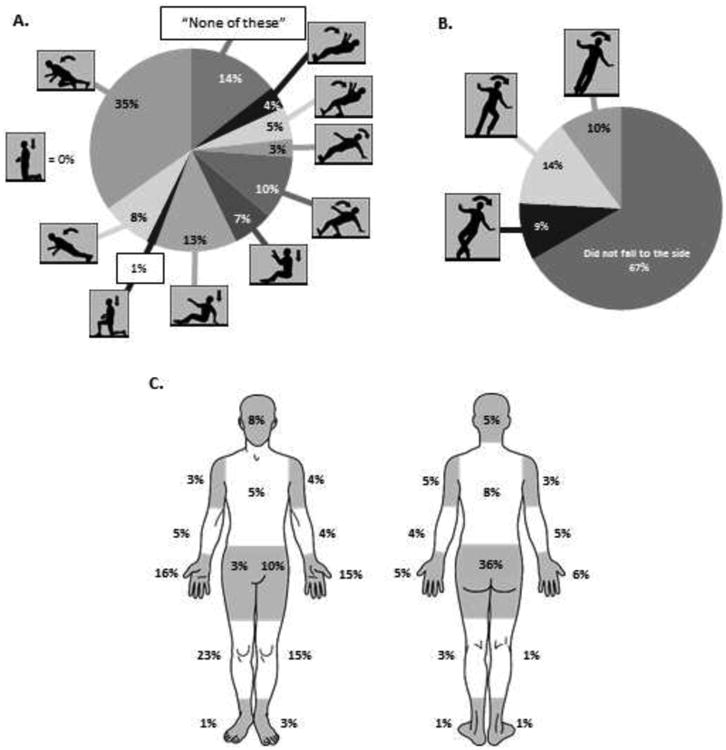
A. Body orientations of falls reported in the forwards or backwards direction (20 fall records did not report this information, leaving blank responses, so percentages are based on n=138 falls). Forward falls were identified from the four leftmost orientations, and backward falls were identified as the remaining six figures. B. Body orientations of falls also reporting lateral (sideways) motion (32 fall records did not report this information, leaving blank responses, so percentages are based on n=126 falls). C. Sites of fall impact, with 87 falls recording more than one impact location (12 fall records did not indicate an impact region, leaving blank answers, so percentages are based on n=146 falls). Note that fall impacts were sometimes reported on the front and back of the same region, or impacts may have been reported to both the left and right analogous regions. Therefore, the sum of percentages in a specific region (e.g. 42% for the hand/wrist) will not equal the results presented in the text (e.g. 27% of falls had a hand/wrist impact).
3. Results
In total, 2917 out of 2993 (97.5%) fall mailers were returned or recorded via phone. The majority of participants (70%) returned all mailers (number of returned mailers: median=24, interquartile range [IQR]=23-24, range=14-24). Thirty eight reminder letters were sent to 32 participants (1-3 letters per participant). Ten reminder phone calls were made to seven participants (1-2 calls per participant). One participant missed nine consecutive mailers after she was diagnosed with cancer, and an additional participant missed 10 mailers at the end of the collection period due to unknown reasons. Two participants passed away during the fall-tracking period, with one death due to cancer and one cause of death not available to the investigators.
3.1 Incidence of Falls
The majority of participants fell, often more than once. Seven fall records that did not directly answer the question pertaining to if a fall occurred, but contained other answers detailing a fall, were included as falls in our analyses. Over 124.6 person-years of follow-up, 74 participants (59%) fell at least once, with 38 (30%) falling more than once. A total of 158 falls were recorded, resulting in a rate of 1.3 falls per person-year. The median number of falls per participant was 1 (IQR: 0-2, range: 0-10 falls per participant). The median time to first fall was four months (IQR=1.5-8; range: 0.5-12 months). Of 151 records with the available information, 128 falls (85%) were on the “floor, ground, or lower level”, 13 falls (9%) were onto “an object (e.g. furniture)” and 10 falls (7%) were “against a wall or railing”. When considering only falls to the “floor, ground or lower level”, 68 participants (54%) fell at a rate of 1.1 falls per person-year.
3.2 Circumstances of Falls
Falls typically occurred during waking hours around the home (Figure 1). At home, nearly an equal number of falls occurred outdoors (n=43) as indoors (n=44). Away from the home, more falls occurred outdoors (n=35) than indoors (n=23). Falls occurred across all seasons, with the lowest number in the Spring (Spring=26, Summer=49, Autumn=41, Winter=42).
Figure 1. The percentage of all falls (n=158) experienced under certain contexts in 125 ambulatory, community-dwelling women age ≥ 65 years.
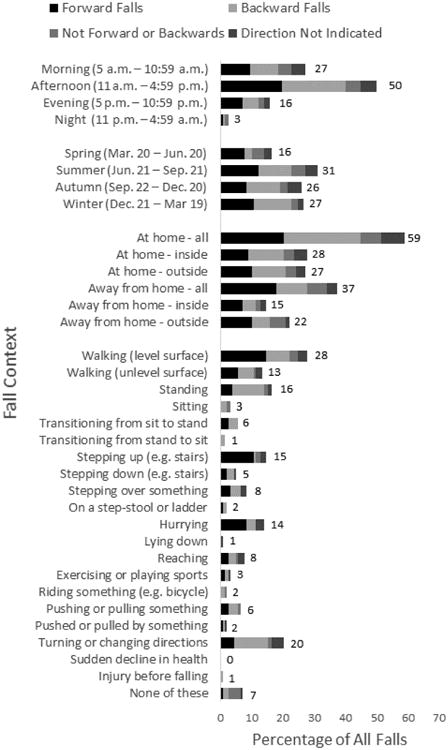
Forward falls, backward falls, falls in neither direction, and falls in which such directions were not reported are distinguished by different shades of gray. Seven fall records did not indicate a time of day. Six fall records did not indicate if it was at home or away from home (four of which were outside, two of which also did not indicate indoor/outdoor status). Six at-home fall records and one away-from-home fall record did not indicate if the fall was outside or not. Five fall records did not indicate any concurrent activity.
Nearly half of all falls occurred during some form of gait, with stairs, hurrying, or a change in direction being common circumstances (Figure 1). Forward falls were frequently noted while hurrying (13/22 falls while hurrying) and stepping up a level (17/23 falls while stepping up). Turning or changing direction commonly resulted in a backwards fall (17/32 falls while turning). Approximately half of all falls were associated with either a slip (n=34) or a trip (n=52), as reported by stepping onto a slippery surface or having an obstacle block the foot, respectively (Table 2). Four falls were associated with both hazards. Of all slip-related falls, 24 (71%) were reported in the winter. There were only 9 falls in 7 women associated with dizziness, loss of consciousness, alcohol/medication, a sudden decline in health, or injury before the fall.
Table 2. The direction-specific contexts and characteristics of recorded falls among 125 ambulatory, community-dwelling women age ≥65 years.
| Fall Direction | All Falls (n=158) | Forward Falls (n=61) | Backward Falls (n=57) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Age at fall (years) (mean ± SD) | 78.3 ± 7.7, | 78.7 ± 8.3, | 78.9 ± 7.6, | ||||||
| Question | Yes | No | No Response | Yes | No | No Response | Yes | No | No Response |
| Did you step onto a slippery | 34 (22%) | 108 (68%) | 16 (10%) | 10 (16%) | 48 (79%) | 3 (5%) | 19 (33%) | 32 (56%) | 6 (11%) |
| Did an object, such as a curb, rug or power cord block your foot? (i.e. you tripped) | 52 (33%) | 98 (62%) | 8 (5%) | 28 (46%) | 31 (51%) | 2 (3%) | 11 (19%) | 42 (74%) | 4 (7%) |
| Did you experience an unexpected drop in the floor or ground level? | 40 (25%) | 108 (68%) | 10 (6%) | 14 (23%) | 42 (69%) | 5 (8%) | 16 (28%) | 38 (67%) | 3 (5%) |
| Did you try to stop your fall by grabbing something (e.g. a hand rail)? | 33 (21%) | 108 (68%) | 17* (11%) | 16 (26%) | 42 (69%) | 3* (5%) | 9 (16%) | 41 (72%) | 7* (12%) |
| Were you wearing corrective glasses or lenses when you fell?** | 123 (78%) | 33 (21%) | 2 (1%) | 50 (82%) | 11 (18%) | 0 | 43 (75%) | 14 (25%) | 0 |
| Was it dark where you fell? | 14 (9%) | 141 (89%) | 3 (2%) | 5 (8%) | 56 (92%) | 0 | 7 (12%) | 49 (86%) | 1 (2%) |
| Were you injured as a result of the fall? | 40 (25%) | 115 (73%) | 3 (2%) | 20 (33%) | 41 (67%) | 0 | 11 (19%) | 45 (79%) | 1 (2%) |
If yes…
|
15 (38%) | 25 (62%) | 0 | 7 (35%) | 13 (65%) | 0 | 5 (45%) | 6 (55%) | 0 |
|
9 (23%) | 31 (78%) | 0 | 5 (25%) | 15 (75%) | 0 | 2 (18%) | 9 (82%) | 0 |
|
9 (23%) | 30 (75%) | 1 (3%) | 5 (25%) | 14 (70%) | 1 (5%) | 2 (18%) | 9 (82%) | 0 |
|
3 (8%) | 37 (93%) | 0 | 3 (15%) | 17 (85%) | 0 | 0 | 11 (100%) | 0 |
Includes responses of “I don't know”.
140 of158 responded that they regularly wore corrective lenses. 18 people (including 4 forward fallers, 7 backward fallers) who regularly wear glasses or corrective lenses fell when not wearing glasses or lenses. One person who does not regularly wear glasses or lenses fell when wearing glasses or lenses.
3.3 Fall Orientations and Impact Locations
Of the 158 reported falls, 20 did not identify whether the fall was in the forward or backward direction, as defined by questionnaire images (Figure 2A). Forward falls, including falls onto a knee, accounted for 44% (n=61/138) of fall-orientation reports (Figure 2A). Of these forward falls, 47% were induced by a trip. Of the 52 reported trips, 54% were associated with a forward fall. During 82% (n=50) of forward falls, a recovery step was reported. One third of forward falls resulted in injury, with 25% of injuries leading to an emergency department visit (Table 2).
Backward falls, including downward falls onto the buttocks, accounted for 41% (n=57) of fall-orientation reports (Figure 2A). Of these falls, 33% were induced by a slip. Of the 34 reported slips, 56% were associated with a backward fall. During 37% (n=21) of backward falls, a recovery step was attempted. In 63% (n=36) of backward falls, a fall orientation was reported demonstrating that a hand was placed as to take the impact of the fall. However, only 14% (n=8) of backward falls reported hand impact. One-fifth of backward falls resulted in self-reported injury, of which 45% lead to an emergency department visit (Table 2).
A fall to the side could be reported in conjunction with a forward or backwards orientation (Figure 2A and 2B, Appendix A). Of the 40 falls reported with sideways motion, 10 had concurrent forward orientations, 12 had concurrent backward orientations, and 18 were not associated with either orientations. There were 32 records that did not indicate whether there was sideways motion with the fall, and 6 records indicated that they “did not know” if such motion occurred (Figure 2B). A stepping response was reported in 70% of falls with sideways motion, with a side-step being more common (n=17) than a cross-over step (n=11). Approximately 31% (n=16) of trips and 18% (n=6) of slip-induced falls were reported with sideways motion.
Fall impacts to the hand/wrist, knee, and hip/pelvis, as determined by reported impact locations (Figure 2C), were common. There were 12 fall records which did not indicate the site of impact. Of the 146 falls with information available, 87 listed more than one impact site. Nearly half of falls with impact records (47%, n=69) indicated impact to the hip/pelvis. One quarter (27%, n=40) of falls with impact records included an impact to the hand/wrist. A similar proportion (29%, n=42) were associated with an impact to the knee. Impacts to the head (12%, n=18), shoulder (12%, n=18) or elbow (16%, n=23) were also common.
The direction of the fall dictated the risk of impacting common fracture locations (Figure 3). A backward fall increased the odds of an impact to the hip/pelvis (OR=12.60, 95% CI: 4.69, 33.82) and torso (OR=3.70, 95%CI: 1.39, 9.83). A forward fall increased the risk of impact to the knee (OR=9.29, 95%CI: 3.88, 22.25) and hand/wrist (OR=2.63, 95%CI: 1.18, 5.89). A fall with sideways motion, regardless of whether also in the forward or backward direction, increased the odds of impact to the shoulder (OR=4.01, 95%CI: 1.17, 13.77) and elbow (OR=2.74, 95%CI: 1.13, 6.67). Although fall direction altered the risk of impact location, the mechanism of the fall (i.e. a trip or a slip) did not do so (Figure 3).
Figure 3. Odds ratios and 95% confidence intervals of fall impact locations as a function of the fall direction or disturbance type.
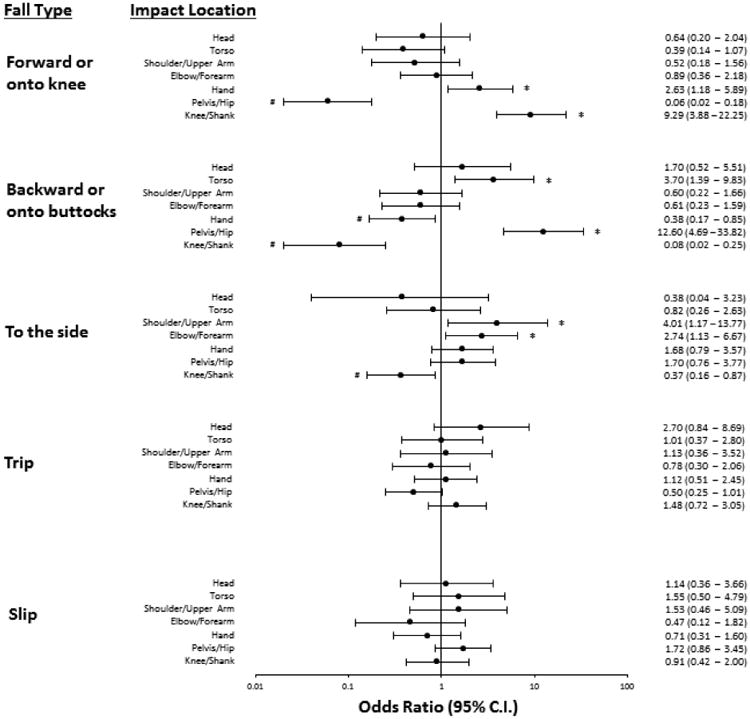
Odds ratios are displayed on a log10 scale. Confidence intervals above 1 are denoted with an *. Confidence intervals below 1 are denoted with a #.
One quarter of falls resulted in self-reported injury, with nearly 38% of those injuries leading to medical attention (Table 2). Of the nine fractures recorded in this study, four occurred to the nose and/or facial bones (three forward falls, one backward fall), two were self-reported to be of the proximal “arm” and/or “shoulder” (both forward falls, one with lateral motion), one was of the calcaneus (a fall off the side of a stair-case), one occurred at the sacrum (a backward fall from an ice-related slip), and one was of the pelvis (no direction reported, unexpected drop in floor due to a missed step).
4. Discussion
Despite being an ambulatory cohort of women, the proportion who fell (59%) and the fall incidence (1.3 falls per person-year) were amongst the highest reported in the literature (34%–62% and 0.28–0.78 falls per person-year, respectively) (Berg et al., 1997; Campbell et al., 1990; Davis, Ross, Nevitt, & Wasnich, 1997; Freiberger & Menz, 2006; Hill, Schwarz, Flicker, & Carroll, 1999; Luukinen et al., 1994, 1995; Maki, Holliday, & Topper, 1994; O'loughlin, Robitaille, Boivin, & Suissa, 1993; Rapp et al., 2014). Semimonthly contact with participants may have elicited more fall records than less frequent contact. Some previous studies required weekly (Maki et al., 1994) or biweekly (Berg et al., 1997) reports of falls. However, other studies had participants return reports on a monthly basis (Campbell et al., 1990; Freiberger & Menz, 2006; Hill et al., 1999; O'loughlin et al., 1993) or less frequently (Davis et al., 1997; Luukinen et al., 1994; Rapp et al., 2014). Given the potential benefit of our frequent fall-tracking methods, along with the high adherence (97.5%) to returning fall reports, we believe the present results accurately represent the fall risk in our cohort of community-dwelling, ambulatory, older women.
For community-dwelling older adults, common activities reported during a fall include walking (21-64% of falls), hurrying or running (4-12%), turning (7%), getting up from a chair (3-12%), and ascending (3-7%) or descending (7-9%) stairs (Berg et al., 1997; Bleijlevens et al., 2010; Duckham et al., 2013; Niino et al., 2000; Painter et al., 2009; Yasumura et al., 1996). In a study of video-recorded falls in long-term care, 42% of falls occurred during walking, 13% while turning, and 9% transitioning from sitting to standing (Robinovitch et al., 2013). Compared to these previous studies, we observed similar results associated with walking (42%), sit-to-stand (6%), and stepping down (5%). However, we observed more falls associated with turning (20%) and stepping up (15%). Falls while turning are of note, as more than half of such falls were backwards, a direction associated with hip/pelvic impact. As observed in previous studies (Berg et al., 1997; Campbell et al., 1990; Luukinen et al., 1995; Niino et al., 2000) most falls occurred at typically awake hours. We observed similar proportions of indoor (42%) and outdoor (52%) falls as that of previous studies (30-45% indoors, 28-56% outdoors) (Aoyagi et al., 1998; Berg et al., 1997; Li et al., 2006).
For older women, prior studies have suggested that extrinsic factors, such as trips, slips, or collisions, account for more fall-related injuries (44 – 69% of fall injuries, 67% of femur fractures) than intrinsic factors such as loss of consciousness or balance disorders (25 – 33% of fall injuries, 23% of femur fractures) (Clark, 1968; Morfitt, 1983; Yasumura et al., 1996). The percentage of falls induced by a trip (33%) was amongst the highest reported in the literature (3-40%), and the proportion induced by a slip (22%) exceeded previous reports (3-17%) (Aoyagi et al., 1998; Berg et al., 1997; Lord, Ward, Williams, & Anstey, 1993; Luukinen et al., 1994; Robinovitch et al., 2013). These results are alarming, as 21-42% and 19-28% of injurious falls are due to a trip or slip, respectively (Morfitt, 1983; Yasumura et al., 1996). Unlike previous studies that associated intrinsic factors with 56% of falls in women (Aoyagi et al., 1998), we found only 6% of falls in our cohort were attributed to intrinsic factors of dizziness, loss of consciousness, alcohol/medication, a sudden decline in health, or injury before the fall. This percentage is closer to the 11% of video-recorded falls due to collapse or loss of consciousness in long-term care (Robinovitch et al., 2013). Our questionnaire did not account for more continual underlying intrinsic factors such as a balance disorder or lower extremity weakness. Admittedly, our questionnaire emphasized the biomechanical and environmental fall circumstances. Given the low incidence of intrinsically-caused falls compared to previous studies, we may not have sensitively captured the influence of physiological factors.
Given that almost half of falls recorded an impact to the hip or pelvis, a figure slightly higher than the 40% observed in long-term care facilities (Yang et al., 2016), it is not surprising that nearly all hip fractures (98%) are due to a fall (Parkkari et al., 1999). Of all fall directions, only backward falls increased the risk of impact to the hip or pelvis in this study (OR = 12.6). This observation is in direct contrast with results from long-term care facilities, which reported that initially-directed forward and sideways falls, not backwards falls, increased the odds of hip impact (Yang et al., 2016). These discrepancies may be due to between-study differences. We did not distinguish the hip from the pelvis, so backward falls may be more associated with impact to the sacrum or pelvis, and not necessarily the proximal femur. Furthermore, we did not distinguish initial from final fall orientations. Previous video records of falls in long-term care facilities determined that 36% of falls had different initial and landing configurations, such as a lateral fall in which a person rotated to land backwards (Yang et al., 2016). In such cases, we do not know if our figures represented initial or final fall orientations. Additionally, between-study differences in the participants' functional or cognitive capacity, or the concurrent use of mobility aids, may influence how fall direction dictates the risk of hip impact.
Protective arm movements have been suggested to reduce the likelihood of hip fracture (Greenspan et al., 1994; Palvanen et al., 2000; Parkkari et al., 1999; Schwartz et al., 1998), although not necessarily the likelihood of hip impact (Yang et al., 2016). Given that 37% (n=36) of backward falls with reported body orientations in our study did not report hand placement to take the fall impact, and only 14% of all backward falls reported any hand impact, our data suggest that protective arm movements are not frequently used in response to a backward fall. Falls with a sideways orientation were more likely to have an impact to the elbow, so protective arm placements during a lateral fall may be a common strategy to reduce the magnitude of hip/pelvis impact, but at the cost of potential injury, including fracture, near the elbow. In general, we observed far fewer hand impacts (27% of falls) compared to video-based studies in long-term care (74%) (Schonnop et al., 2013) or laboratory studies of young adults (98%) (Feldman & Robinovitch, 2007).
Fall-recovery training in which external perturbations necessitate a stepping response to arrest the fall is of increasing interest (Rosenblatt, Marone, & Grabiner, 2013) and our results would support such a research focus. The common recovery strategy of a stepping response was more prevalent in our study of ambulatory women from the community (63% of falls) than previous reports from video recordings in a senior center (45%) (Holliday, Fernie, Gryfe, & Griggs, 1990) or long-term care facilities (49%) (Yang et al., 2016). In the latter study by Yang et al, stepping doubled the odds of hip impact (Yang et al., 2016), These findings coupled with the fact that failed stepping-responses were so prevalent in our study, would suggest that it is important to not only train the initiation of a stepping response, but also modify step placement and body rotation as to improve the efficacy of such a stepping response in preventing a fall or fall injury. Addressing intrinsic fall-risk factors should continue to be part of clinical interventions to reduce falls. However, the high observed incidence of trips and slips warrants a specific focus on the avoidance of and recovery from these extrinsic causes. To our knowledge, our study is the first to report that cross-over steps, as a response to a fall, were attempted in the free-living environment. As with laboratory-based studies of fall-recovery (Maki, Edmondstone, & McIlroy, 2000), side steps were the more common response to a lateral fall. Given that about one fourth of falls had an attempted lateral stepping response (Figure 2B), the correct selection and execution of a lateral stepping strategy warrants investigation as an intervention target to prevent falls.
While the present study does not specifically evaluate the validity of our fall-tracking methods, self-reported injuries were consistent with recorded impact locations. Previous studies have corroborated reported impact locations with hematoma locations and witness accounts (Palvanen et al., 2000; Parkkari et al., 1999). A previous study determined that 50% of falls for residents in long-term facilities had discrepancies between self-reports and video surveillance (Yang, Feldman, Leung, Scott, & Robinovitch, 2015). We suspect, however, that fall recall was more accurate for our community-dwelling cohort. We acknowledge that the validity and reliability of our specific questionnaire have not been quantified. Previous studies validated fall orientation images during in-person interviews of people who sustained fall injury (Palvanen et al., 2000). We have adapted these images for our study. By translating this approach to mailed questionnaires and non-injurious falls, we may be placing the validity of the measure at risk. That said, among our participants who sustained injuries from a fall, their impact locations marked on questionnaires were consistent with the injuries sustained in their medical records. Future work will be needed to validate this approach with witness accounts, as video surveillance is not feasible in the ambulatory setting. Reliability could be determined by asking participants to repeat the questionnaire a second time, although recollection accuracy may be diminished with time.
Limitations of this study include a relatively small sample size of participants that excluded men. The high incidence of falls and fall-related impacts to the hip, head, and upper extremities observed in this study warrants further investigation with a larger sample. Women have a markedly higher rate of non-fatal fall injury compared to men (Centers for Disease Control and Prevention, 2015). Although evidence suggests older women may also have a higher incidence of falls (Aoyagi et al., 1998; Blake et al., 1988; Davis et al., 1997; De Rekeneire et al., 2003; Hill et al., 1999; Luukinen et al., 1994; Painter et al., 2009; Rapp et al., 2014; S Yasumura et al., 1994), we do not know if sex influences the likelihood of reporting a fall. Therefore, the implications from this study may not be directly applicable to older men.
5. Conclusions
In summary, this study demonstrated a higher incidence of falls for community-dwelling older women than has been previously reported. Trips, slips, and falls to the side were frequently observed, and impacts to the hip/pelvis and hand/wrist were common. Forward falls were associated with trips, climbing up steps and hurrying. Backward falls were associated with slips or changing directions. A forward fall increased the risk of hand/wrist impact, and a backwards fall increased the odds of impact to the hip/pelvis. Stepping response was frequently attempted in order to arrest the fall, and may be a natural response that can be further trained in order to prevent falls. Our comprehensive findings on fall circumstances, orientations, and impact locations provide insights that may further guide assessments and interventions to reduce fall-related injuries.
Highlights.
Over one year, 59% of older women fell, resulting in 1.3 falls per person-year.
The majority of falls were associated with a trip (33%) or slip (22%).
Falls were 44% forward and 41 % backward, with 33% concurrently or solely sideways.
Compensatory steps were often a response to forward (82%) and sideways (70%) falls.
Impacts to the hip/pelvis (47% of falls) and hand/wrist (27%) were common.
Acknowledgments
We thank Louise McCready, R.N. for study coordination and Diana Hansen for data collection and processing.
Funding: This work was supported by National Institutes of Health [grant numbers R01AR027065 to SK/SA, T32HD07447 to J. R. Basford, NIH UL1TR000135 to SK]. The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Appendix A


The above questionnaire (front and back) was returned twice monthly by participants. Study staff filled out the “Subject” and “Date” (i.e. 15-day period) information for a series of questionnaires, which was distributed to participants on a quarterly basis.
Appendix B


The “Fall Figure Guide” was provided to all participants at the beginning of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Montoye HJ, Sallis JF, Paffenbarger RS. Compendium of physical activities: classification of energy costs of human physical activities. Medicine and Science in Sports and Exercise. 1993;25(1):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- Aoyagi K, Ross PD, Davis JW, Wasnich RD, Hayashi T, Takemoto TII. Falls among community-dwelling elderly in Japan. Journal of Bone and Mineral Research. 1998;13(9):1468–1474. doi: 10.1359/jbmr.1998.13.9.1468. [DOI] [PubMed] [Google Scholar]
- Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age and Ageing. 1997;26(4):261–268. doi: 10.1093/ageing/26.4.261. [DOI] [PubMed] [Google Scholar]
- Blake AJ, Morgan K, Bendall MJ, Dallosso H, Ebrahim SBJ, Arie THD, et al. Bassey EJ. Falls by elderly people at home: Prevalence and associated factors. Age and Ageing. 1988;17(6):365–372. doi: 10.1093/ageing/17.6.365. [DOI] [PubMed] [Google Scholar]
- Bleijlevens MHC, Diederiks JPM, Hendriks MRC, van Haastregt JCM, Crebolder HFJM, van Eijk JTM. Relationship between location and activity in injurious falls: an exploratory study. BMC Geriatrics. 2010;10(1):40. doi: 10.1186/1471-2318-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age and Ageing. 1990;19(2):136–141. doi: 10.1093/ageing/19.2.136. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention N. C. for I. P. and C. Web-based Injury Statistics Query and Reporting System (WISQARS) 2017 Retrieved from http://www.cdc.gov/injury/wisqars/
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Clark AN. Factors in fracture of the female femur. A clinical study of the environmental, physical, medical and preventive aspects of this injury. Gerontologia Clinica. 1968;10(5):257–270. doi: 10.1159/000245191. [DOI] [PubMed] [Google Scholar]
- Davis JW, Ross PD, Nevitt MC, Wasnich RD. Incidence rates of falls among Japanese men and women living in Hawaii. Journal of Clinical Epidemiology. 1997;50(5):589–594. doi: 10.1016/s0895-4356(96)00430-1. [DOI] [PubMed] [Google Scholar]
- De Rekeneire N, Visser M, Peila R, Nevitt MC, Cauley JA, Tylavsky FA, Harris TB. Is a fall just a fall: Correlates of falling in healthy older persons. The health, aging and body composition study. Journal of the American Geriatrics Society. 2003;51(6):841–846. doi: 10.1046/j.1365-2389.2003.51267.x. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Duckham RL, Procter-Gray E, Hannan MT, Leveille SG, Lipsitz LA, Li W. Sex differences in circumstances and consequences of outdoor and indoor falls in older adults in the MOBILIZE Boston cohort study. BMC Geriatrics. 2013;13(1):133. doi: 10.1186/1471-2318-13-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman F, Robinovitch SN. Reducing hip fracture risk during sideways falls: Evidence in young adults of the protective effects of impact to the hands and stepping. Journal of Biomechanics. 2007;40(12):2612–2618. doi: 10.1016/j.jbiomech.2007.01.019. [DOI] [PubMed] [Google Scholar]
- Freiberger E, Menz HB. Characteristics of falls in physically active community-dwelling older people: Findings from the “Standfest im Alter” study. Zeitschrift Fur Gerontologie Und Geriatrie. 2006;39(4):261–267. doi: 10.1007/s00391-006-0394-2. [DOI] [PubMed] [Google Scholar]
- Greenspan SL, Myers ER, Maitland La, Resnick NM, Hayes WC. Fall severity and bone mineral density as risk factors for hip fracture in ambulatory elderly. Journal of the American Medical Association. 1994;271(2):128–133. [PubMed] [Google Scholar]
- Hill K, Schwarz J, Flicker L, Carroll S. Falls among healthy, community-dwelling, older women: A prospective study of frequency, circumstances, consequences and prediction accuracy. Australian and New Zealand Journal of Public Health. 1999;23(1):41–48. doi: 10.1111/j.1467-842x.1999.tb01203.x. [DOI] [PubMed] [Google Scholar]
- Holliday PJ, Fernie GR, Gryfe CI, Griggs GT. Video recording of spontaneous falls of the elderly. ASTM Special Technical Publication. 1990:7–16. [Google Scholar]
- Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, Jørstad‐ Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: The Prevention of Falls Network Europe consensus. Journal of the American Geriatrics Society. 2005;53(9):1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- Li W, Keegan THM, Sternfeld B, Sidney S, Quesenberry CP, Jr, Kelsey JL, et al. Kelsey JL. Outdoor falls among middle-aged and older adults: A neglected public health problem. American Journal of Public Health. 2006;96(7):1192–1200. doi: 10.2105/AJPH.2005.083055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord SR, Ward JA, Williams P, Anstey KJ. An epidemiological study of falls in older community-dwelling women: The Randwick falls and fractures study. Australian Journal of Public Health. 1993;17(3):240–245. doi: 10.1111/j.1753-6405.1993.tb00143.x. [DOI] [PubMed] [Google Scholar]
- Luukinen H, Koski K, Hiltunen L, Kivelä SL. Incidence rate of falls in an aged population in Northern Finland. Journal of Clinical Epidemiology. 1994;47(8):843–850. doi: 10.1016/0895-4356(94)90187-2. [DOI] [PubMed] [Google Scholar]
- Luukinen H, Koski K, Honkanen R, Kivela SL. Incidence of injury-causing falls among older adults by place of residence: A population-based study. Journal of the American Geriatrics Society. 1995;43(8):871–876. doi: 10.1111/j.1532-5415.1995.tb05529.x. [DOI] [PubMed] [Google Scholar]
- Maki BE, Edmondstone MA, McIlroy WE. Age-related differences in laterally directed compensatory stepping behavior. Journals of Gerontology - Series A Biological Sciences and Medical Sciences. 2000;55(5):M270–M277. doi: 10.1093/gerona/55.5.m270. [DOI] [PubMed] [Google Scholar]
- Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. Journal of Gerontology. 1994;49(2):M72–84. doi: 10.1093/geronj/49.2.m72. [DOI] [PubMed] [Google Scholar]
- Morfitt JM. Falls in old people at home: Intrinsic versus environmental factors in causation. Public Health. 1983;97(2):115–120. doi: 10.1016/s0033-3506(83)80008-0. [DOI] [PubMed] [Google Scholar]
- Niino N, Tsuzuku S, Ando F, Shimokata H. Frequencies and circumstances of falls in the national institute for longevity sciences, longitudinal study of aging (NILS-LSA) Journal of Epidemiology. 2000;10(1 SUPPL):S90–S94. doi: 10.2188/jea.10.1sup_90. [DOI] [PubMed] [Google Scholar]
- O'loughlin JL, Robitaille Y, Boivin JFF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. American Journal of Epidemiology. 1993;137(3):342–354. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- Painter JA, Elliott SJ, Hudson S. Falls in community-dwelling adults aged 50 Years and older : Prevalence and contributing factors. Journal of Allied Health. 2009;38(4):201–207. [PubMed] [Google Scholar]
- Palvanen M, Kannus P, Parkkari J, Pitkäjärvi T, Pasanen M, Vuori I, et al. Järvinen M. The injury mechanisms of osteoporotic upper extremity fractures among older adults: A controlled study of 287 consecutive patients and their 108 controls. Osteoporosis International. 2000;11(10):822–831. doi: 10.1007/s001980070040. [DOI] [PubMed] [Google Scholar]
- Parkkari J, Kannus P, Palvanen M, Natri A, Vainio J, Aho H, et al. Järvinen M. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: A prospective controlled hip fracture study with 206 consecutive patients. Calcified Tissue International. 1999;65(3):183–187. doi: 10.1007/s002239900679. [DOI] [PubMed] [Google Scholar]
- Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. The Journals of gerontology Series A, Biological Sciences and Medical Sciences. 1995;50A(1):M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Ghali Wa. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- Rapp K, Freiberger E, Todd C, Klenk J, Becker C, Denkinger M, Fuchs J. Fall incidence in Germany: Results of two population-based studies, and comparison of retrospective and prospective falls data collection methods. BMC Geriatrics. 2014;14(1):1–8. doi: 10.1186/1471-2318-14-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, Loughi M. Video capture of the circumstances of falls in elderly people residing in long-term care: An observational study. The Lancet. 2013;381(9860):28. doi: 10.1016/S0140-6736(12)61263-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip-related falls by community-dwelling adults: A prospective study. Journal of the American Geriatrics Society. 2013;61(9):1629–1631. doi: 10.1111/jgs.12428. [DOI] [PubMed] [Google Scholar]
- Schonnop R, Yang Y, Feldman F, Robinson E, Loughin M, Robinovitch SN. Prevalence of and factors associated with head impact during falls in older adults in long-term care. CMAJ : Canadian Medical Association Journal = Journal de l'Association Medicale Canadienne. 2013;185(17) doi: 10.1503/cmaj.130498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz AV, Kelsey JL, Sidney S, Grisso JA. Characteristics of falls and risk of hip fracture in elderly men. Osteoporosis International. 1998;8(3):240–246. doi: 10.1007/s001980050060. [DOI] [PubMed] [Google Scholar]
- Yang Y, Feldman F, Leung PM, Scott V, Robinovitch SN. Agreement between video footage and fall incident reports on the circumstances of falls in long-term care. Journal of the American Medical Directors Association. 2015;16(5):388–394. doi: 10.1016/j.jamda.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Yang Y, Mackey DC, Liu-Ambrose T, Feldman F, Robinovitch SN. Risk factors for hip impact during real-life falls captured on video in long-term care. Osteoporosis International. 2016;27(2):537–547. doi: 10.1007/s00198-015-3268-x. [DOI] [PubMed] [Google Scholar]
- Yasumura S, Haga H, Nagai H, Suzuki T, Amano H, Shibata H. Rate of falls and the correlates among elderly people living in an urban community in Japan. Age and Ageing. 1994;23(4):323–327. doi: 10.1093/ageing/23.4.323. [DOI] [PubMed] [Google Scholar]
- Yasumura S, Haga H, Niino N. Circumstances of injurious falls leading to medical care among elderly people living in a rural community. 1996 doi: 10.1016/0167-4943(96)00711-x. [DOI] [PubMed] [Google Scholar]


